Professional Documents
Culture Documents
Azole-Resistant What You Need To Know: Aspergillus Fumigatus
Uploaded by
Paula GeorgianaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Azole-Resistant What You Need To Know: Aspergillus Fumigatus
Uploaded by
Paula GeorgianaCopyright:
Available Formats
Clinical CMN
Stay Current...
Microbiology
N e w s l e t t e r
Stay Informed.
Vol. 42, No. 1 Azole-Resistant Aspergillus fumigatus:
January 1, 2020
www.cmnewsletter.com What You Need To Know
In ThIS ISSue Shawn R. Lockhart, Karlyn Beer, and Mitsuru Toda, Mycotic Diseases Branch, Centers for Disease
Control and Prevention, Atlanta, Georgia
1 Azole-Resistant Aspergillus
fumigatus: What You Need Abstract
To Know Aspergillosis is one of the most common fungal infections. The predominant cause of aspergillosis is
6 Salmonella enterica the species Aspergillus fumigatus. There have been increasing reports of A. fumigatus isolates that are
Serotype Typhi Soft Tissue resistant to azole antifungals. The predominant causes of this resistance are environmentally acquired
Infection Following Direct mutations in the target gene, CYP51A, known as TR 34/L98H and TR 46/Y121F/T289A. They consist
Inoculation: a Rare Route of of a tandem repeat in the promoter region (TR) and one or two amino acid changes in the protein
Transmission sequence, respectively. Unfortunately, the capacity in the United States for mold antifungal suscepti-
A case report bility testing is limited, so the extent of azole resistance in clinical practice is largely unknown. This
review discusses the causes and implications of azole-resistant A. fumigatus and the role that antifungal
susceptibility testing might play in its identification.
Note to Authors Introduction patients with hematologic malignancy. The mor-
Please note that CMN will tality rate associated with invasive aspergillosis is
no longer be accepting case Anyone who has processed respiratory specimens dependent upon the patient population, but in a
reports for publication in in a clinical microbiology laboratory is familiar recent study of 960 patients with various under-
the newsletter. with the white-bordered, felt-like mold colonies lying conditions, the 12-week mortality was 35%
of various colors that are typical of Aspergillus [3]. Aspergillus isolates, especially A. fumigatus,
(Fig. 1 and 2). Aspergillus species are ubiquitous that are resistant to medical azole treatment are
in the environment, and airborne conidia can be associated with treatment failure and increased
found both indoors and outdoors. Perhaps due to mortality. In a study comparing 90-day mortal-
their ubiquitous nature, Aspergillus species are the ity among 196 patients with voriconazole-sus-
most frequently encountered molds from respi- ceptible and voriconazole-resistant A. fumigatus
ratory specimens and one of the most frequent infections, 90-day mortality was 25% higher for
causes of invasive mold infections [1]. Although those with a resistant infection [4].
there are more than 250 species of Aspergillus,
four species cause almost 90% of all human
Susceptibility Testing of Aspergillus
Aspergillus infections: A. fumigatus, A. flavus, A.
Corresponding author: terreus, and A. niger. The most common species Susceptibility testing of molds is not common in
Shawn R. Lockhart,
encountered in clinical practice is A. fumigatus, the United States, even though the Clinical and
Ph.D.,
D(ABMM), F(AAM), Mycotic
responsible for over half of aspergillosis cases in Laboratory Standards Institute (CLSI) has devel-
Diseases Branch, Centers for the United States [2]. It can cause several types oped a standard for mold antifungal susceptibil-
Disease Control and Prevention, of disease, including asthma, allergic broncho- ity testing (AFST) [5]. No automated systems or
1600 Clifton Rd., Mailstop G- pulmonary aspergillosis, chronic obstructive custom kits are available for susceptibility testing
11, Atlanta, GA 30333. Tel.: pulmonary aspergillosis, and invasive pulmo- of molds, so many laboratories develop AFST
404-639-2569. E-mail: nary aspergillosis, of which the last can lead to individually. Most laboratories that have validated
gyi2@cdc.gov disseminated disease. Aspergillosis is the most mold AFST use either standard broth microdi-
0196-4399/©2020 Elsevier Inc. common cause of invasive mold infections among lution or gradient diffusion strips (such as Etest)
All rights reserved
Clinical Microbiology Newsletter 42:1,2020 | ©2020 Elsevier 1
Figure 1. Colonies of A. fumigatus growing on Sabouraud dextrose Figure 2. Micrograph of A. fumigatus stained with lactophenol cotton
agar. Colonies are typically green with a white border, turning slate blue. Conidial heads are columnar and occur only on the upper portion
grey with age. of the vesicle; uniseriate with a phialide that produces chains of
smooth globose conidia.
[6]. While broth microdilution is the standard, good correlation is though few Aspergillus breakpoints exist, this does not mean there
achieved between gradient diffusion strips and broth microdilution are no other interpretive criteria. Both EUCAST and CLSI have
for itraconazole, voriconazole, and amphotericin B (Fig. 3) [7,8]. developed epidemiological cutoff values (ECVs or ECOFFs) for
Gradient diffusion strips are generally easier to implement in labo- a number of Aspergillus species and antifungal combinations [14]
ratories without experience performing susceptibility testing. In (http://www.eucast.org/mic_distributions_and_ecoffs/). While
addition to these two methodologies, another recently developed an ECV is not a breakpoint, it does help to determine whether
assay uses a 4-well azole agar plate with RPMI agar in wells con- an isolate is wild type (has an MIC value that is consistent with a
taining itraconazole (4 µg/ml), voriconazole (2 µg/ml), posacon- normal distribution and no resistance mutations) or non-wild type
azole (0.5 µg/ml), and no drug [9,10]. The plate is inoculated with
a known concentration of Aspergillus conidia and then monitored
for growth. Growth in any of the wells containing azoles indi-
cates the possibility of resistance and that the isolate should be
investigated further. The European Committee on Antimicrobial
Susceptibility Testing (EUCAST) recently adopted a standard for
the use of these plates for Aspergillus susceptibility testing [11].
One of the commonly cited reasons for not validating mold
susceptibility testing is that interpretive criteria have not been
established to qualify the results. Although 0.008 µg/ml is usually
interpreted as susceptible and 16 µg/ml is usually interpreted as
resistant, what about MIC values in the middle, such as 0.5, 1, or
2 µg/ml? EUCAST established breakpoints for some of the azole
antifungals and amphotericin B against Aspergillus species in 2012
[12, 13]. However, these breakpoints are valid only when using
the EUCAST method of AFST. Fortunately, CLSI approved its
first breakpoint for a mold at the 26 January 2019 meeting of the
Antifungal Susceptibility Testing Subcommittee. The breakpoint
for susceptibility of A. fumigatus against voriconazole is ≤0.5 µg/
ml, and the breakpoint for resistance is ≥2 µg/ml. CLSI does not Figure 3. Etests showing a voriconazole-susceptible (left) and an
have breakpoints for other Aspergillus species or other molds. Even itraconazole-resistant (right) A. fumigatus isolate.
2 Clinical Microbiology Newsletter 42:1,2020 | ©2020 Elsevier
(likely to have a mutation that confers resistance). For a bug-drug that are used in agriculture rather than from exposure to azoles
combination where it is generally known that the drug is effica- during treatment or prophylaxis in patients [21,22].
cious for treatment, like Aspergillus and the newer azoles, ECVs
Since the initial discovery in the Netherlands in 1998, A. fumiga-
may be used to determine whether an isolate has acquired muta-
tus isolates with TR 34/L98H have been identified in Asia, Africa,
tions and is therefore not wild type. This designation is challeng-
Australia, South America, and North America [23]. In addition,
ing, though, because there are few clinical data to inform as to the
a second set of mutations, TR 46/Y121F/T289A (TR 46), has been
interpretive value of these MICs. Thus, it is unknown whether an
identified. Like TR34, TR46 is associated with the use of azole fun-
MIC result that falls outside the ECV range would be predictive
gicides in agriculture [13,14,23,24].
of treatment failure [15].
To determine whether and to what extent these fungicide-associ-
Azole Resistance in A. fumigatus ated resistant isolates are present in the United States, the Cen-
ters for Disease Control and Prevention (CDC) conducted passive
The prevalence of azole resistance in A. fumigatus has been
surveillance for azole-resistant A. fumigatus in the United States.
increasing for more than a decade [16-18]. The most frequently
Of the >1,000 A. fumigatus isolates collected from 22 states during
encountered resistance mutations are those that occur in the
2011 to 2013, none contained the TR 34 or TR 46 mutation [25].
14-α-demethylase gene, CYP51A, a component of the ergosterol
The first U.S. isolates with either TR 34 or TR 46 were identified
synthesis pathway and the target of the azole antifungals. This
from a national reference laboratory that retrospectively exam-
gene is orthologous to ERG11, the gene target of azoles in Candida
ined all isolates collected during 2001 to 2014. In that collec-
species. Multiple amino acid substitutions that lead to azole resis-
tion, they found that 26 isolates had elevated MIC values to more
tance have been identified in the Cyp51A protein. These mutations
than one azole. One isolate from 2008 and one from 2014, both
generally occur in isolates from patients that have received long-
from Pennsylvania, contained the TR 34 mutation [26]. In addi-
term azole therapy or prophylaxis. Depending on the mutation,
tion, two isolates with the TR 46 mutation, one from Arizona in
they can confer resistance to either a single azole, multiple azoles,
2008 and one from an unknown location in 2012, were identified
or all the azoles (Table 1). To confound matters, approximately
[26]. Another report, published in 2016, identified a patient from
30% of isolates that show in vitro azole resistance do not have an
Michigan who had an isolate containing the TR 46 mutation [27].
identifiable resistance mechanism [17]. It is thought that efflux
In 2015, CDC reinitiated passive surveillance for azole-resistant
pumps play a role in resistance in these isolates [19]. While the
A. fumigatus. During 2015 to 2017, five additional isolates with the
incidence of azole-resistant A. fumigatus is increasing globally, it
is not yet common in patients in the United States [20]. TR34 mutation were identified, two from Pennsylvania, two from
Virginia, and one from California, although these positive results
Resistance can develop under selection pressure from azoles, and represented only 0.3% of all of the isolates tested [20]. These iso-
this can happen inside the human body when a patient is on long- lates and two others with TR 34 mutations were identified among
term azole therapy or in the environment, where A. fumigatus is 7 patients, of whom 3 died and 4 had not been previously treated
exposed by chance to azoles used for other purposes. A study by with azole medication [28]. Patients had no epidemiologic links,
Snelders and colleagues in 2008 initially identified a trend toward suggesting a variety of different sources contributed to their A.
increasing azole resistance in A. fumigatus isolates in the Neth- fumigatus specimens.
erlands [17]. The most frequent cause of resistance was a pair of
mutations found in the 14-α-demethylase gene (CYP51A) called Role of Agricultural Azoles in A. fumigatus Resistance
TR 34 /L98H (TR 34 ). The mutations consist of a tandem 34-bp Certain agricultural azole fungicides, including difenoconazole,
repeat in the promoter region of the gene that leads to increased tebuconazole, and propiconazole, are structurally similar to medi-
gene expression (TR 34) and an amino acid change from lysine to cal azoles, such as itraconazole, voriconazole, and posaconazole
histidine at amino acid 98 (L98H) that hinders the binding of [29]. Azole fungicides are used in agriculture (crop protection
azoles to the target. A worrisome aspect of the TR 34 mutation is from fungal diseases and promotion of increased crop yields) and
that it is believed to be derived from the use of azole fungicides in other applications, such as preservation of wood and other
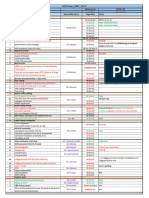
Table 1. The most common mutations in CYP51A that lead to azole resistance in A. fumigatus
Mutation Found in patients Found in nature Primary resistancea
TR34/L98H Yes Yes Itraconazole/posaconazole
TR46/Y121F/T289A Yes Yes Voriconazole
G54E/R/V Yes Yes Itraconazole/posaconazole
G138C/S Yes No Itraconazole/posaconazole
M220I/R/K/V Yes Yes Itraconazole/posaconazole/voriconazole
G448S No No Voriconazole
a Some isolates with these mutations are pan-azole resistant, but further work needs to be done to decipher other contributing mutations within the same isolate.
Clinical Microbiology Newsletter 42:1,2020 | ©2020 Elsevier 3
materials [30]. Of the many classes of agricultural fungicides, Implications for Clinicians
azoles represent the largest fungicide class in agricultural and hor- Although azole-resistant A. fumigatus has been infrequently
ticultural use. In the Netherlands, the total volume of fungicides reported in the United States to date, these reports likely rep-
used has not changed dramatically over time, but the proportion resent an underestimate of the number of patients with resistant
of azole fungicide use doubled between 1995 and 2007 [22]. In the isolates. A. fumigatus infection and colonization are not report-
United States, azole fungicides are commonly used on wheat, corn, able conditions in any state and are not nationally notifiable to
the CDC, meaning that no formal reporting requirement exists.
and soybeans, three of the major crops produced in this country
Perhaps as a result, clinicians are largely unaware of resistant A.
in metric tons. The estimated usage of azoles in this country also
fumigatus and its added risk of treatment failure and death, espe-
increased dramatically from 2006 to 2015 [31].
cially among patients with invasive aspergillosis [4]. A retrospec-
In addition to clinical isolates, A. fumigatus isolates with TR34 and tive cohort study in the Netherlands showed 21% higher mortality
TR 46 mutations have been found in the environment, including in patients with voriconazole-resistant invasive aspergillosis than
in patients’ homes and back yards, in flower bulb waste and wood in patients infected with voriconazole-susceptible isolates [41].
Unfortunately, the problem of azole-resistant A. fumigatus is still
chips, in hospital gardens, and even in air samples from hospitals
not widely recognized. In a 2018 survey of 709 infectious disease
[24,32-35]. They have also been found in sealed tulip bulbs in
physicians, over half were unfamiliar with the concept of azole-
Ireland that were imported from the Netherlands, where azole
resistant A. fumigatus and only 62% reported having access to
resistance in A. fumigatus has become common [35]. While all the antifungal susceptibility testing [42]. Together, limited awareness
environmental A. fumigatus isolates with TR 34 and TR 46 muta- and lack of reporting mechanisms point to a strong need for vigi-
tions were identified outside the United States, the conundrum lance among front-line clinicians treating susceptible patients, even
remained that no one in the United States had actually looked in those without prior azole treatment. Clinicians and laboratories
the environment for these mutations. To see if A. fumigatus isolates interested in participating in CDC’s voluntary passive surveillance
associated with the use of agricultural azoles could be identified program are invited to submit all A. fumigatus isolates; more infor-
in the United States, isolates were collected from crop debris on mation and submission instructions are available online (lhttps://
www.cdc.gov/fungal/aspergillus-resistance.html) .
a farm in Georgia that had been treated with tebuconazole and
propiconazole. Of the 200 isolates collected, 20 contained the TR34 Summary
mutation and none contained the TR 46 mutation [36]. This single Azole-resistant A. fumigatus is present in the United States in
finding may not be representative of the rest of the United States, patients and in the environment. Many factors, including increas-
but with the increasing use of agricultural azoles throughout the ing use of agricultural azoles, medical prophylaxis, and long-term
country, it indicates potential for increasing incidence, similar to treatment of patients, and the growing number of patients sus-
what has been seen in Europe. ceptible to fungal infections may contribute to the potential for
increasing azole-resistant A. fumigatus prevalence in the United
new Antifungals States, as it has in parts of Europe. The solution is not a simple
Medical azoles are the first-line therapy for invasive aspergillo- one, but two important steps clinical microbiologists can take are
vigilance and increased AFST capacity. Laboratories can con-
sis, and use of azole antifungal medications has improved patient
sider implementing susceptibility testing of isolates from patients
survival [37]. The Infectious Diseases Society of America rec-
thought to have a resistant infection or surveillance for azole-
ommends voriconazole as the primary treatment of choice for
resistant isolates using one of the protocols mentioned above.
most forms of Aspergillus infection; other azoles, as well as for-
The findings and conclusions in this article are those of the authors
mulations of amphotericin B, are also used [38]. Because some
and do not necessarily represent the official position of the Centers
A. fumigatus isolates with the TR 34 mutation are pan-resistant to
for Disease Control and Prevention.
the azoles, amphotericin B is left as the only proven treatment
option. However, other classes of mold-active antifungal agents References
with activity against Aspergillus are now in phase 2 clinical trials. [1] Sugui JA, Kwon-Chung KJ, Juvvadi PR, Latge JP, Steinbach WJ.
Olorofim (formerly F901318) is a mold-active antifungal that tar- Aspergillus fumigatus and related species. Cold Spring Harbor
Perspect Med 2014;5:a019786.
gets dihydroorotate dehydrogenase and inhibits pyrimidine bio-
[2] Patterson TF, Kirkpatrick WR, White M, Hiemenz JW, Wingard
synthesis [39]. A second mold-active compound in development JR, Dupont B, et al. Invasive aspergillosis. Disease spectrum, treat-
is fosmanogepix (formerly APX001A). This compound is a potent ment practices, and outcomes. I3 Aspergillus Study Group. Medicine
inhibitor of glycophosphatidylinositol biosynthesis [40]. Both com- 2000;79:250-60.
[3] Steinbach WJ, Marr KA, Anaissie EJ, Azie N, Quan SP, Meier-
pounds have very strong in vitro activity against multiple species
Kriesche HU, et al. Clinical epidemiology of 960 patients with
of Aspergillus. The results of phase 3 clinical trials will determine invasive aspergillosis from the PATH Alliance registry. J Infect
whether they join the current antifungal armamentarium. 2012;65:453-64.
4 Clinical Microbiology Newsletter 42:1,2020 | ©2020 Elsevier
[4] Lestrade PP, Bentvelsen RG, Schauwvlieghe AF, Schalekamp S, van [21] Snelders E, Huis In ‘t Veld RA, Rijs AJ, Kema GH, Melchers
der Velden WJ, Kuiper EJ, et al. Voriconazole resistance and mortal- WJ, Verweij PE. Possible environmental origin of resistance of
ity in invasive aspergillosis: a multicenter retrospective cohort study. Aspergillus fumigatus to medical triazoles. Appl Environ Microbiol
Clin Infect Dis 2019;68:1463-71. 2009;75:4053-7.
[5] CLSI. Reference method for broth dilution antifungal susceptibility [22] Verweij PE, Snelders E, Kema GH, Mellado E, Melchers WJ. Azole
testing of filamentous fungi, 3rd edition. Wayne, PA, USA: CLSI; resistance in Aspergillus fumigatus: a side-effect of environmental
2017. fungicide use? Lancet Infect Dis 2009;9:789-95.
[6] Bernal-Martinez L, Alastruey-Izquierdo A, Cuenca-Estrella M. [23] Resendiz Sharpe A, Lagrou K, Meis JF, Chowdhary A, Lockhart SR,
Diagnostics and susceptibility testing in Aspergillus. Future Microbiol Verweij PE. Triazole resistance surveillance in Aspergillus fumigatus.
2016;11:315-28. Med Mycol 2018;56:83-92.
[7] Meletiadis J, Mouton JW, Meis JF, Bouman BA, Verweij PE. Com- [24] van der Linden JW, Camps SM, Kampinga GA, Arends JP, Debets-
parison of the Etest and the Sensititre colorimetric methods with Ossenkopp YJ, Haas PJ, et al. Aspergillosis due to voriconazole highly
the NCCLS proposed standard for antifungal susceptibility testing resistant Aspergillus fumigatus and recovery of genetically related
of Aspergillus species. J Clin Microbiol 2002;40:2876-85. resistant isolates from domiciles. Clin Infect Dis 2013;57:513-20.
[8] Pfaller JB, Messer SA, Hollis RJ, Diekema DJ, Pfaller MA. In vitro [25] Pham CD, Reiss E, Hagen F, Meis JF, Lockhart SR. Passive surveil-
susceptibility testing of Aspergillus spp.: comparison of Etest and lance for azole-resistant Aspergillus fumigatus, United States, 2011-
reference microdilution methods for determining voriconazole and 2013. Emerg Infect Dis 2014;20:1498-503.
itraconazole MICs. J Clin Microbiol 2003;41:1126-9.
[26] Wiederhold NP, Gil VG, Gutierrez F, Lindner JR, Albataineh MT,
[9] Buil JB, van der Lee HAL, Rijs AJMM, Zoll J, Hovestadt JAMF, McCarthy DI, et al. First detection of TR34 L98H and TR46 Y121F
Melchers WJG, et al. Single-center evaluation of an agar-based T289A Cyp51 mutations in Aspergillus fumigatus isolates in the
screening for azole resistance in Aspergillus fumigatus by using VIP- United States. J Clin Microbiol 2016;54:168-71.
check. Antimicrob Agents Chemother 2017;61:e01250-17.
[27] Vazquez JA, Manavathu EK. Molecular characterization of a voricon-
[10] Arendrup MC, Verweij PE, Mouton JW, Lagrou K, Meletiadis J. azole-resistant, posaconazole-susceptible Aspergillus fumigatus isolate
Multicentre validation of 4-well azole agar plates as a screening in a lung transplant recipient in the United States. Antimicrob Agents
method for detection of clinically relevant azole-resistant Aspergillus Chemother 2016;60:1129-33.
fumigatus. J Antimicrob Chemother 2018;73:2274.
[28] Beer KD, Farnon EC, Jain S, Jamerson C, Lineberger S, Miller J, et al.
[11] Guinea J, Verweij PE, Meletiadis J, Mouton JW, Barchiesi F, Aren- Multidrug-resistant Aspergillus fumigatus carrying mutations linked
drup MC. How to: EUCAST recommendations on the screening to environmental fungicide exposure—three states, 2010-2017. Morb
procedure E.Def 10.1 for the detection of azole resistance in Asper- Mortal Wkly Rep 2018;67:1064-7.
gillus fumigatus isolates using four-well azole-containing agar plates.
[29] Snelders E, Camps SM, Karawajczyk A, Schaftenaar G, Kema
Clin Microbiol Infect 2019;25:681-7.
GH, van der Lee HA, et al. Triazole fungicides can induce cross-
[12] Hope W W , Cuenca-Estrella M , Lass-Florl C, Arendrup MC. resistance to medical triazoles in Aspergillus fumigatus. PLoS One
EUCAST technical note on voriconazole and Aspergillus spp. Clin 2012;7:e31801.
Microbiol Infect 2013;19:E278-80.
[30] Wise KA, Smith D, Freije A, Mueller DS, Kandel Y, Allen T,
[13] Arendrup MC, Cuenca-Estrella M , Lass-Florl C, Hope W W . et al. Meta-analysis of yield response of foliar fungicide-treated
EUCAST technical note on Aspergillus and amphotericin B, itracon- hybrid corn in the United States and Ontario, Canada. PLoS One
azole, and posaconazole. Clin Microbiol Infect 2012;18:E248-50. 2019;14:e0217510.
[14] CLSI. Epidemiological cutoff values for antifungal susceptibility [31] Centers for Disease Control and Prevention. Issues for addressing
testing. 2nd ed. supplement M59. Wayne, PA, USA: CLSI; 2018. antimicrobial resistance in the environment. Available from: https://
wellcome.ac.uk/sites/default/files/antimicrobial-resistance-environ-
[15] Lockhart SR, Ghannoum MA, Alexander BD. Establishment and use
ment-report.pdf [Accessed 10/5/2019]
of epidemiological cutoff values for molds and yeasts by use of the
Clinical and Laboratory Standards Institute M57 standard. J Clinic [32] Lavergne RA, Chouaki T, Hagen F, Toublanc B, Dupont H, Jouni-
Microbiol 2017;55:1262-8. eaux V, et al. Home environment as a source of life-threatening
azole-resistant Aspergillus fumigatus in immunocompromised patients.
[16] Heo ST, Tatara AM, Jimenez-Ortigosa C, Jiang Y, Lewis RE, Tarrand
Clin Infect Dis 2017;64:76-8.
J, et al. Changes in in vitro susceptibility patterns of Aspergillus to
triazoles and correlation with aspergillosis outcome in a tertiary care [33] Schoustra SE, Debets AJM, Rijs AJMM, Zhang J, Snelders E,
cancer center, 1999-2015. Clin Infect Dis 2017;65:216-25. Leendertse PC, et al. Environmental hotspots for azole resistance
selection of Aspergillus fumigatus, the Netherlands. Emerg Infect Dis
[17] Snelders E, van der Lee HA, Kuijpers J, Rijs AJ, Varga J, Samson
2019;25:1347-53.
RA, et al. Emergence of azole resistance in Aspergillus fumigatus and
spread of a single resistance mechanism. PLoS Med 2008;5:e219. [34] Chowdhary A, Sharma C, van den Boom M, Yntema JB, Hagen F,
Verweij PE, et al. Multi-azole-resistant Aspergillus fumigatus in the
[18] Abdolrasouli A, Petrou MA, Park H, Rhodes JL, Rawson TM, Moore
environment in Tanzania. J Antimicrob Chemother 2014;69:2979-83.
LSP, et al. Surveillance for azole-resistant Aspergillus fumigatus in a
centralized diagnostic mycology service, London, United Kingdom, [35] Dunne K, Hagen F, Pomeroy N, Meis JF, Rogers TR. intercountry
1998-2017. Front Microbiol 2018;9:2234. transfer of triazole-resistant Aspergillus fumigatus on plant bulbs. Clin
Infect Dis 2017;65:147-9.
[19] da Silva Ferreira ME, Capellaro JL, dos Reis Marques E, Malavazi I,
Perlin D, Park S, et al. In vitro evolution of itraconazole resistance [36] Hurst SF, Berkow EL, Stevenson KL, Litvintseva AP, Lockhart SR.
in Aspergillus fumigatus involves multiple mechanisms of resistance. Isolation of azole-resistant Aspergillus fumigatus from the envi-
Antimicrobial Agents Chemother 2004;48:4405-13. ronment in the south-eastern US A. J Antimicrob Chemother
2017;72:2443-6.
[20] Berkow EL, Nunnally NS, Bandea A, Kuykendall R, Beer K, Lock-
hart SR. Detection of TR34/L98H CYP51A mutation through pas- [37] Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE,
sive surveillance for azole-resistant Aspergillus fumigatus in the United Oestmann JW, et al. Voriconazole versus amphotericin B for primary
States from 2015 to 2017. Antimicrob Agents Chemother 2018;62. therapy of invasive aspergillosis. N Engl J Med 2002;347:408-15.
Clinical Microbiology Newsletter 42:1,2020 | ©2020 Elsevier 5
[38] Patterson TF, Thompson GR III, Denning DW, Fishman JA, Had- [41] van Paassen J, Russcher A, In ‘t Veld-van Wingerden AW, Verweij
ley S, Herbrecht R, et al. Practice guidelines for the diagnosis and PE, Kuijper EJ. Emerging aspergillosis by azole-resistant Aspergillus
management of aspergillosis: 2016 update by the Infectious Diseases fumigatus at an intensive care unit in the Netherlands, 2010 to 2013.
Society of America. Clin Infect Dis 2016;63:e1-e60. Euro Surveill 2016;21:30300.
[39] du Pré S, Beckmann N, Almeida MC, Sibley GEM, Law D, Brand [42] Walker TA, Lockhart SR, Beekmann SE, Polgreen PM, Santibanez
AC, et al. Effect of the novel antifungal drug F901318 (olorofim) S, Mody RK, et al. Recognition of azole-resistant Aspergillosis by
on growth and viability of Aspergillus fumigatus. Antimicrob Agents physicians specializing in infectious diseases, United States. Emerg
Chemother 2018;62:e00231-18. Infect Dis 2018;24:111-3.
[40] Zhao M, Lepak AJ, Marchillo K, Vanhecker J, Sanchez H, Ambrose
PG, et al. APX001 pharmacokinetic/pharmacodynamic target
determination against Aspergillus fumigatus in an in vivo model of
invasive pulmonary aspergillosis. Antimicrob Agents Chemother
2019;63:e02372-18.
6 Clinical Microbiology Newsletter 42:1,2020 | ©2020 Elsevier
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Fritz Springmeier InterviewDocument59 pagesFritz Springmeier InterviewCzink Tiberiu100% (4)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pattern, Price and Time - Using Gann TheoryDocument29 pagesPattern, Price and Time - Using Gann TheoryRohitOhri44% (9)
- Echofish JRC Jfc-180bbDocument4 pagesEchofish JRC Jfc-180bbJERINsmileNo ratings yet
- Arts - 9 - Quarter 3 Module 1Document4 pagesArts - 9 - Quarter 3 Module 1John Mark Prestoza100% (3)
- Hach - MWP (Plan Vs Actual) Status - 22 Oct-1Document1 pageHach - MWP (Plan Vs Actual) Status - 22 Oct-1ankit singhNo ratings yet
- Fungal Evolution: Diversity, Taxonomy and Phylogeny of The FungiDocument37 pagesFungal Evolution: Diversity, Taxonomy and Phylogeny of The FungiPaula GeorgianaNo ratings yet
- US Dollar Store Consumer BehaviourDocument10 pagesUS Dollar Store Consumer BehaviourTryden Royce D'SouzaNo ratings yet
- Bearing CapacityDocument4 pagesBearing CapacityahmedNo ratings yet
- Prog Copywriting Exercise 10Document3 pagesProg Copywriting Exercise 10azertyNo ratings yet
- Islamiyat O-Level Paper-1 Notes PDFDocument126 pagesIslamiyat O-Level Paper-1 Notes PDFddd80% (5)
- Gonzles Ramrez2016Document14 pagesGonzles Ramrez2016Paula GeorgianaNo ratings yet
- Gallium: Professional Paper 1802-HDocument48 pagesGallium: Professional Paper 1802-HPaula GeorgianaNo ratings yet
- Medical Applications and Toxicities of Gallium CompoundsDocument25 pagesMedical Applications and Toxicities of Gallium CompoundsPaula GeorgianaNo ratings yet
- PD2017 013 PDFDocument36 pagesPD2017 013 PDFChico Hermanu BrillianNo ratings yet
- Normalization ExercisesDocument2 pagesNormalization ExercisesAnh DiệuNo ratings yet
- Presentation On Modal Auxiliary VerbsDocument18 pagesPresentation On Modal Auxiliary VerbsAbdelhafid ZaimNo ratings yet
- CH 1 Cases - Mcqs CH 1 Cases - McqsDocument55 pagesCH 1 Cases - Mcqs CH 1 Cases - McqsChaudhary AdeelNo ratings yet
- Friday HeatsDocument29 pagesFriday HeatsTGrasley6273No ratings yet
- The Rook Volume XXIIIDocument40 pagesThe Rook Volume XXIIIThe RookNo ratings yet
- Capital Structure TheoriesDocument9 pagesCapital Structure TheoriesMahesh HadapadNo ratings yet
- 3.6-6kva Battery Cabinet: 1600Xp/1600Xpi SeriesDocument22 pages3.6-6kva Battery Cabinet: 1600Xp/1600Xpi SeriesIsraelNo ratings yet
- Organ TransplantationDocument36 pagesOrgan TransplantationAnonymous 4TUSi0SqNo ratings yet
- Human Rights RapDocument4 pagesHuman Rights Rapapi-264123803No ratings yet
- ED 305 Calvin College Lesson Planning FormDocument4 pagesED 305 Calvin College Lesson Planning Formapi-314250067No ratings yet
- Ece 250 Project PortfolioDocument7 pagesEce 250 Project Portfolioapi-511924847No ratings yet
- Clam Antivirus 0.100.0 User ManualDocument34 pagesClam Antivirus 0.100.0 User ManualJacobus SulastriNo ratings yet
- 13 Datasheet Chint Power Cps Sca5ktl-Psm1-EuDocument1 page13 Datasheet Chint Power Cps Sca5ktl-Psm1-EuMARCOS DANILO DE ALMEIDA LEITENo ratings yet
- Elite MindsDocument1 pageElite MindsShivaNo ratings yet
- Intelligent Platform Management Interface Firmware, Upgrade: Operational InstructionDocument23 pagesIntelligent Platform Management Interface Firmware, Upgrade: Operational InstructionLayth WaellNo ratings yet
- PMLS 2 Unit 9Document3 pagesPMLS 2 Unit 9Elyon Jirehel AlvarezNo ratings yet
- Please DocuSign Youssef ADMISSIONS FORM W ATDocument5 pagesPlease DocuSign Youssef ADMISSIONS FORM W ATyoussefkhalfaoui30No ratings yet
- Practice Paper 1 Class X Social Science Time 3 Hrs. M.M 80 General InstructionsDocument6 pagesPractice Paper 1 Class X Social Science Time 3 Hrs. M.M 80 General Instructionsvvs .b.s1453No ratings yet
- E8 Practice Test Second Term Grade 8 - 962023103557Document13 pagesE8 Practice Test Second Term Grade 8 - 962023103557Duy HoangNo ratings yet
- SSLD Stairways LowresDocument44 pagesSSLD Stairways LowresboyNo ratings yet