Professional Documents
Culture Documents
Lower Respi Raymond Serrano PDF
Lower Respi Raymond Serrano PDF
Uploaded by
Noelle Grace Ulep Baroman0 ratings0% found this document useful (0 votes)
18 views9 pagesOriginal Title
Lower-Respi-Raymond-Serrano.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
18 views9 pagesLower Respi Raymond Serrano PDF
Lower Respi Raymond Serrano PDF
Uploaded by
Noelle Grace Ulep BaromanCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 9
CASE NO. 119
RAYMOND SERRANO
SESSION I
TUTOR GUIDE:
1 First 1 hour
Give Chief Complaints of Raymond Serrano. Let students extract the medical
history and physical examination findings. Do not give information unless
asked for.
2 Next 45 minutes
Let the students formulate their hypotheses and let them identify and prioritize
learning issues,
2 Last 15 minutes
Processing and feedback
LEARNING ISSUES:
Anatomy of the lower respiratory tract
Physiology of breathing
Mechanism of transport of blood gases
Causes of dyspnea
CASE NO. 119
RAYMOND SERRANO
SESSION I
Chief Complaints: high-grade fever, chills and difficulty of breathing.
Case Scenario:
Raymond Serrano, an 11-year old male child. residing at San Miguel Village, is admitted to
the Mercy Community Hospital for the chief complaints of high-grade fever. chills and difficulty of
breathing.
About a day prior to admission, his teacher, at the Living Spring Academy, noticed that he
was feverish, with a runny nose, dry, hacking cough and teary eyes. He was brought to the school
linic at recess time and was told to increase his fluid intake. rest. and take paracetamol for fever and
vitamin C-rich beverages. The next day, although the cough gersisted, the runny nose and teary eyes
cleared up, and Raymond felt well enough to return to schocl. By midmoming, however, his fever
retumed, ranging from 39-40°C, his cough worsened and he seemed to be in respiratory distress as
‘manifested by his rapid respiration and cyanosis around the mouth. He also started shaking violently
‘and complained that he felt cold, despite his high temperature. The alarmed teachers called his
parents who fetched him from school and brought him directly to the hospital for admission,
Raymond is the only child of Elaine, 36. a high-school teacher in MSU-IIT, and Jude, 37, an
‘engineer employed by Global Steel Corporation. According to his parents, this is Raymond's first
hospitalization as he had never been seriously lil except for the usual cough and colds. Immunization
is complete, including boosters. Developmental milestones were normal for his age. He is a fith-
grader at the Living Spring Academy and an average student.
PHYSICAL EXAMINATION:
General Survey: Anxious, tachypneic, restless. well nourished, well developed, febrile child
Vital signs: 8P= 90/60 mm Hg Weight = 35 kg
HR= 110/min Height = 138 om
R= 60/min 40.5°C
HEENT:
+ Normocephatic
No conjunctival injections
With flaring of the alae nasi
Very red throat
Enlarged and red tonsils
Neck: (+) cervical lymphadenopathy both sides of the neck
Chest and Lungs:
‘© Symmetrical, with intercostal and retrosternal retractions
+ (#) duliness, right lower lobe
+ Diminished vocal and tactile fremitus on the right lower lobe
60
+ Diminished breath sounds with fine crackles on the right lower lobe
Heart:
* Tachycardic
+ No murmurs heard
Abdomen:
«Slightly globular
+) right lower quadrant pain
+ Diminished to absent bowel sounds
= No organomegaly
Extremities: wer extremities
Equal palpable pulses both upoer
Genitalia:
+ Normal circumcised, male extemal gen’
+ Both testes descended and palpable
(For submission during the next tutorial)
4. Let the students write the mecicai ristory and PE findings of the case.
2. Let them write their pmary
rationale for considering these 4
sion and differential diagnoses, including their
'Ses and for ruling them out.
3. Let them include pian
Allow them to suggest dia
using the P(ersonal) treatment guidelines.
lures they may want to request.
CASE NO. 119
RAYMOND SERRANO
SESSION II
TUTOR GUIDE:
1. First 1 hour and 15 minutes.
Let the students present the case history and give their primary impressions and
differential diagnoses. Answer the tasks and discuss the learning issues identified in the
previous session
2. Next 30 minutes
Give the case scenario. Compare the Preatment of the students with the treatment
plan in the scenario.
Identify new leaming issues
3 Last 15 minutes
Processing and feedback
LEARNING ISSUES:
1. Community-acquired pneumonia
Common causes according to 2
Pathophysiology
Clinical manifestations
Diagnostic tests
Complications
2. Current guidelines in the management of CAP in adults and pediatric age group
2
CASE NO. 119
RAYMOND SERRANO
SESSION II
CASE SCENARIO
Raymond was admitted with the following orders: (What are the reasons for admission?
What are the current guidelines in the treatment of pneumonia?)
Non-pharmacologic treatment:
+ Vital signs every 4 hours
‘+ Tepid sponge bath for temper
+ Increase intake of oral fluids
Pharmacologic treatment:
+ Paracetamol 325 mg (Tempra; + tablet every 4 hours
+ Cefuroxime Na (Zinacef) 250 mg 2 vials slow IV ANST q 8 hrs (Do you agree
with the choice of antibiotic? Are there other drugs that you can use?)
+ Oxygen inhalation at 2 Limin
‘+ IVF: 40.3 NaCl at 73 mlnr (Compute for the IV rate)
Laboratory request:
= Complete biood count
+ Blood cutture
+ Urinalysis
+ Chest X-ray (PA and
TASK: Give the rationale for the above orders.
“What results do you expect to receive?
63
CASE NO. 119
RAYMOND SERRANO
SESSION Ill
TUTOR GUIDE:
1. First 1 hour
Answer the tasks and discuss the learning issues identified in the previous session
2. Next 45 minutes.
Give the case scenario. Discuss the laboratory results
Identify new leaming issues
3. Last 15 minutes
Processing and feedback
64
CASE NO. 119
RAYMOND SERRANO
‘SESSION III
All the laboratory results, except for the blood culture, came in two hours later.
Complete Blood Cou
Hemoglobin = 140 g/t
Hematocrit = 0.40
Red blood cell 3
White blood cells = 48 x 10°71
Polymorphonuctears
Lymphocytes = 0.19
Eosinophils = 0.01
Platelets= 229 x 10°/1
Urinalysis:
Color - straw Sp. Gravity - 1.020
Transparency - clear Albumin ~ ()
pH-6.5 Sugar - ¢)
Microscopic:
Pus cells - 0-t/hpf
RBC - 0
Epithelial cells -none
Casts - none
Bacteria - none
Chest X-ray (PA, Lateral) : Consolidation in the right lower lobe
TASK1: Interpret the laboratory results. How will these affect your management?
By the second hospital day, Raymond seemed to be feeling better. Physical examination
revealed that he was still febrile (38.5°C), and his heart rate was 92/min. and respiratory rate was
45/min. However, examination of the lungs revealed an increase in fremitus on the right lower lobe
and disappearance of the rales. (How would you now assess your patient?)
Later that aftemoon, the blood culture results arrived
st
Blood culture (24 hours}
-ptococcus pneumoniae
TASK2: ‘What is your plan of management now?
65
CASE NO. 119
RAYMOND SERRANO
SESSION IV
TUTOR GUIDE:
1. First 1 hour
Answer the tasks and discuss the leaming issues identified in the previous session
2, Next 45 minutes
Give the case scenario,
Identify new leaming issues
3. Last 15 minutes
Processing and feedback
CASE NO. 119
RAYMOND SERRANO
SESSION IV
CASE SCENARIO:
All of the medications were continued. By the third hospital day, Raymond's fever has
subsided, and his respiratory difficulty lessened, although there was still flaring of the alae nasi. RR
was 30/min and HR was 85/min. (Assess Raymond’s condition. What is your plan of
management now?)
Oxygen inhalation and the IV fluids were discontinued and the patient was shifled to
cefuroxime axetil 500 mg 1 capsule 3 x a day. His cough loosened and he was putting out large
amounts of mucus, some of which were blood-tinged. By the 5" hospital day, Raymond was afebrile
and was not in respiratory distress .He was discharged with instructions to go back to his doctor for
check-up after 3 days.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- EthnolecrepooooorttpdfDocument61 pagesEthnolecrepooooorttpdfNoelle Grace Ulep BaromanNo ratings yet
- Labor: Williams 25th EditionDocument27 pagesLabor: Williams 25th EditionNoelle Grace Ulep BaromanNo ratings yet
- Set BDocument2 pagesSet BNoelle Grace Ulep BaromanNo ratings yet
- Partograph For MoodleDocument37 pagesPartograph For MoodleNoelle Grace Ulep BaromanNo ratings yet
- C19 Pregnant WomenDocument27 pagesC19 Pregnant WomenNoelle Grace Ulep BaromanNo ratings yet
- Scanned With CamscannerDocument54 pagesScanned With CamscannerNoelle Grace Ulep BaromanNo ratings yet
- Death: Andrew M Marcella, MD, DPBS, FPCS, FPSGSDocument19 pagesDeath: Andrew M Marcella, MD, DPBS, FPCS, FPSGSNoelle Grace Ulep BaromanNo ratings yet
- Medico-Legal Investigation of Death: Andrew M Marcella, MD, DPBS, FPCS, FPSGSDocument27 pagesMedico-Legal Investigation of Death: Andrew M Marcella, MD, DPBS, FPCS, FPSGSNoelle Grace Ulep BaromanNo ratings yet
- DM Management TherapiesDocument16 pagesDM Management TherapiesNoelle Grace Ulep BaromanNo ratings yet
- Sex Crimes: Forensic MedicineDocument39 pagesSex Crimes: Forensic MedicineNoelle Grace Ulep Baroman100% (1)
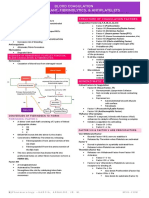
- Blood Coagulation Anticoagulant, Fibrinolytics, & AntiplateletsDocument19 pagesBlood Coagulation Anticoagulant, Fibrinolytics, & AntiplateletsNoelle Grace Ulep BaromanNo ratings yet
- Causes of Chest DiscomfortDocument8 pagesCauses of Chest DiscomfortNoelle Grace Ulep BaromanNo ratings yet
- Anxiety Disorders Intro2Document18 pagesAnxiety Disorders Intro2Noelle Grace Ulep BaromanNo ratings yet
- Cardiovascular Physical TherapyDocument41 pagesCardiovascular Physical TherapyNoelle Grace Ulep BaromanNo ratings yet
- Ch12 HeartDocument130 pagesCh12 HeartNoelle Grace Ulep BaromanNo ratings yet
- Trauma-And Stressor - Related DisordersDocument24 pagesTrauma-And Stressor - Related DisordersNoelle Grace Ulep BaromanNo ratings yet
- Schizophrenia Spectrum and Other Psychotic DisordersDocument31 pagesSchizophrenia Spectrum and Other Psychotic DisordersNoelle Grace Ulep BaromanNo ratings yet
- Dissociative DisordersDocument29 pagesDissociative DisordersNoelle Grace Ulep BaromanNo ratings yet
- AortaDocument1 pageAortaNoelle Grace Ulep BaromanNo ratings yet
- Somatoform Disorders and Factitious Disorders: DSM-1V-TRDocument33 pagesSomatoform Disorders and Factitious Disorders: DSM-1V-TRNoelle Grace Ulep Baroman100% (1)
- Intro To Clinical PsychiatryDocument26 pagesIntro To Clinical PsychiatryNoelle Grace Ulep Baroman100% (1)