Professional Documents
Culture Documents
10 1002@bjs 11464 PDF
Uploaded by
Lourdes MollardOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 1002@bjs 11464 PDF
Uploaded by
Lourdes MollardCopyright:
Available Formats
Original article
Hepatocellular carcinoma tumour burden score to stratify
prognosis after resection
D. I. Tsilimigras1 , D. Moris1 , J. M. Hyer1 , F. Bagante1,4 , K. Sahara1 , A. Moro1 , A. Z. Paredes1 ,
R. Mehta1 , F. Ratti5 , H. P. Marques6 , S. Silva6 , O. Soubrane7 , V. Lam8 , G. A. Poultsides3 , I. Popescu10 ,
S. Alexandrescu10 , G. Martel11 , A. Workneh11 , A. Guglielmi4 , T. Hugh9 , L. Aldrighetti5 ,
I. Endo12 , K. Sasaki2 , A. Rodarte2 , F. N. Aucejo2 and T. M. Pawlik1
Departments of Surgery, 1 Ohio State University Wexner Medical Center, Columbus, and 2 Digestive Disease Institute, Cleveland Clinic, Cleveland,
Ohio, and 3 Stanford University, Stanford, California, USA, Departments of Surgery, 4 University of Verona, Verona, and 5 Ospedale San Raffaele, Milan,
Italy, 6 Department of Surgery, Curry Cabral Hospital, Lisbon, Portugal, 7 Department of Hepatobiliopancreatic Surgery, Assistance Publique – Hôpitaux
de Paris, Beaujon Hospital, Clichy, France, Departments of Surgery, 8 Westmead Hospital, and 9 University of Sydney, School of Medicine, Sydney, New
South Wales, Australia, 10 Department of Surgery, Fundeni Clinical Institute, Bucharest, Romania, 11 Department of Surgery, University of Ottawa,
Ottawa, Ontario, Canada, and 12 Yokohama City University School of Medicine, Yokohama, Japan
Correspondence to: Professor T. M. Pawlik, Department of Surgery, Ohio State University, Wexner Medical Center, 395 W 12th Avenue, Suite 670,
Columbus, Ohio 43210-1240, USA (e-mail: tim.pawlik@osumc.edu)
Background: Although the Barcelona Clinic Liver Cancer (BCLC) staging system has been largely
adopted in clinical practice, recent studies have emphasized the need for further refinement and
subclassification of this system.
Methods: Patients who underwent hepatectomy with curative intent for BCLC-0, -A or -B hepatocellular
carcinoma (HCC) between 2000 and 2017 were identified using a multi-institutional database. The
tumour burden score (TBS) was calculated, and overall survival (OS) was examined in relation to TBS
and BCLC stage.
Results: Among 1053 patients, 63 (6⋅0 per cent) had BCLC-0, 826 (78⋅4 per cent) BCLC-A and 164
(15⋅6 per cent) had BCLC-B HCC. OS worsened incrementally with higher TBS (5-year OS 77⋅9, 61
and 39 per cent for low, medium and high TBS respectively; P < 0⋅001). No differences in OS were
noted among patients with similar TBS, irrespective of BCLC stage (61⋅6 versus 58⋅9 per cent for
BCLC-A/medium TBS versus BCLC-B/medium TBS, P = 0⋅930; 45 versus 13 per cent for BCLC-A/high
TBS versus BCLC-B/high TBS, P = 0⋅175). Patients with BCLC-B HCC and a medium TBS had better
OS than those with BCLC-A disease and a high TBS (58⋅9 versus 45 per cent; P = 0⋅005). On multivariable
analysis, TBS remained associated with OS among patients with BCLC-A (medium TBS: hazard ratio
(HR) 2⋅07, 95 per cent c.i. 1⋅42 to 3⋅02, P < 0⋅001; high TBS: HR 4⋅05, 2⋅40 to 6⋅82, P < 0⋅001) and
BCLC-B (high TBS: HR 3⋅85, 2⋅03 to 7⋅30; P < 0⋅001) HCC. TBS could also stratify prognosis among
patients in an external validation cohort (5-year OS 79, 51⋅2 and 28 per cent for low, medium and high
TBS respectively; P = 0⋅010).
Conclusion: The prognosis of patients with HCC varied according to the BCLC stage but was largely
dependent on the TBS.
Paper accepted 15 November 2019
Published online in Wiley Online Library (www.bjs.co.uk). DOI: 10.1002/bjs.11464
Introduction of cancer-related death, with model-based simulations
forecasting a continued increase in the incidence of HCC
Hepatocellular carcinoma (HCC) is the most common until at least 20303,4 . Cancer staging is necessary as it
primary liver malignancy, with over 750 000 new cases helps define prognosis, as well as informs treatment
and a nearly equal number of cancer-related deaths each recommendations5,6 . Among the staging systems available,
year1,2 . In the USA, HCC is the fastest growing cause the Barcelona Clinic Liver Cancer (BCLC) system has
© 2020 BJS Society Ltd BJS
Published by John Wiley & Sons Ltd
D. I. Tsilimigras, D. Moris, J. M. Hyer, F. Bagante, K. Sahara, A. Moro et al.
been used widely in the West and has been endorsed by Hospital, Sydney, New South Wales, Australia; Stanford
the European Association for the Study of the Liver7 – 9 . University, Stanford, California, USA; Fundeni Clinical
According to the BCLC system, resection should be Institute, Bucharest, Romania; University of Ottawa,
offered only to patients with BCLC-0 and BCLC-A HCC, Ottawa, Ontario, Canada; and University of Sydney,
whereas those with more advanced disease (BCLC-B and School of Medicine, Sydney, New South Wales, Australia.
BCLC-C) are recommended to undergo other types of Follow-up data for patients who underwent HCC resec-
treatment, including transarterial chemoembolization tion were recorded in an international, multi-institutional
(TACE) and sorafenib8,9 . database. Patients with BCLC stages 0, A and B HCC8
The original BCLC system was refined in 2011, with were included in the final cohort. Patients who did not
single large HCCs (at least 5 cm) designated as BCLC-A undergo resection with curative intent (intent of resection
rather than BCLC-B10 . As such, single tumours of at least defined before operation), those with BCLC-C tumours
2 cm as well as two or three tumours smaller than 3 cm and patients with inadequate follow-up data were excluded
are currently considered as BCLC-A HCC8 . Neverthe- from the analysis. Patients who died within 90 days of
less, these criteria have been considered too vague, with operation (31, 2⋅9 per cent) were not excluded from the
studies11,12 showing heterogeneous outcomes after resec- analysis. The study was approved by the institutional
tion of HCC within the same stage. In addition, several review boards of all participating institutions.
investigators13 – 16 have recently advocated extending the
criteria for resection, acknowledging that certain patients Outcomes and variables of interest
with BCLC-B HCC may benefit more from surgery than
other locoregional therapies (TACE). The prognostic dis- The primary outcome was overall survival (OS), defined
crimination as well as the treatment allocation of the as the interval between the date of hepatectomy and the
revised BCLC classification have been questioned, empha- date of death or last follow-up. The secondary outcome was
sizing the need for refinement and further subclassification disease-free survival (DFS), defined as the interval between
of this system17 . the date of hepatectomy and the date of recurrence or
First proposed by Sasaki and colleagues18 , the tumour last follow-up. The primary independent variables were
burden score (TBS) incorporates both tumour number BCLC stage8 and TBS. Demographic and clinical data
and tumour size as continuous variables, and has been included: age, sex, ASA fitness grade, history of cirrhosis,
demonstrated to differentiate prognosis among patients hepatitis B virus (HBV) and hepatitis C virus (HCV) infec-
undergoing resection for colorectal liver metastases. To tion, α-fetoprotein (AFP) level, Child–Pugh grade, mini-
mally invasive surgery, extent of surgical resection (minor
date, no study has assessed the ability of TBS to predict
or major), tumour size and grade, pathological lymphovas-
outcomes among patients undergoing resection of HCC
cular invasion, liver capsule involvement, margin status (R0
of various BCLC stages. The objective of the present
or R1) and TBS.
study was to evaluate the impact of TBS in relation to
the prognosis of patients undergoing resection for HCC.
In addition, this study sought to examine whether TBS Definitions
could be used as a tool to stratify prognosis and identify Single tumours smaller than 2 cm were designated as
patients who may benefit the most from resection beyond BCLC-0; a single tumour of at least 2 cm, or two to three
(BCLC-B) the current BCLC resection criteria. nodules all smaller than 3 cm, as BCLC-A; and two to
three nodules of at least 3 cm, or four or more nodules, as
Methods BCLC-B8,19 . Tumour size was defined by the size of the
largest lesion if there were multiple nodules. Major hepate-
Patients who underwent resection of HCC with curative ctomy was defined as resection of three or more Couinaud
intent between 2000 and 2017 were identified from an segments20 . TBS was defined as the distance from the ori-
international multi-institutional database. Patients were gin of a Cartesian plane and comprised two variables18 :
treated at one of 11 participating institutions: Ohio State maximum tumour size (x-axis) and number of tumours
University Wexner Medical Center, Columbus, Ohio, (y-axis) so that TBS2 = (maximum tumour diameter)2 +
USA; Yokohama City University School of Medicine, (number of tumours)2 . For each patient, the maximum
Yokohama, Japan; University of Verona, Verona, Italy; tumour diameter and number of tumours were obtained
Ospedale San Raffaele, Milan, Italy; Curry Cabral Hos- from the final pathological report. Cut-off values of TBS
pital, Lisbon, Portugal; Assistance Publique – Hôpitaux were determined by X-tile, a bioinformatics tool produced
de Paris, Beaujon Hospital, Clichy, France; Westmead by Camp and colleagues21 .
© 2020 BJS Society Ltd www.bjs.co.uk BJS
Published by John Wiley & Sons Ltd
Tumour burden score for hepatocellular carcinoma
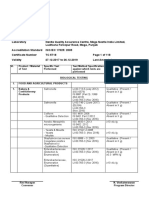
Table 1 Clinicopathological characteristics of the entire cohort
Total BCLC-0 BCLC-A BCLC-B
(n = 1053) (n = 63) (n = 826) (n = 164) P†
Age (years)* 67 (59–73) 64 (58–71) 67 (59–74) 68 (62–74) 0⋅012‡
≤ 65 444 (43⋅6) 30 (52) 362 (45⋅0) 52 (33⋅3)
> 65 575 (56⋅4) 28 (48) 443 (55⋅0) 104 (66⋅7)
Sex 0⋅184
M 789 (75⋅1) 44 (71) 613 (74⋅3) 132 (80⋅5)
F 262 (24⋅9) 18 (29) 212 (25⋅7) 32 (19⋅5)
ASA fitness grade 0⋅113
≤ II 578 (62⋅5) 40 (66) 435 (60⋅8) 103 (69⋅6)
> II 347 (37⋅5) 21 (34) 281 (39⋅2) 45 (30⋅4)
Cirrhosis 0⋅035
No 646 (61⋅5) 30 (48) 520 (63⋅2) 96 (58⋅5)
Yes 404 (38⋅5) 33 (52) 303 (36⋅8) 68 (41⋅5)
HBV infection 0⋅082
No 769 (73⋅9) 39 (63) 614 (75⋅2) 116 (71⋅6)
Yes 272 (26⋅1) 23 (37) 203 (24⋅8) 46 (28⋅4)
HCV infection 0⋅346
No 723 (69⋅4) 39 (62) 574 (70⋅3) 110 (67⋅9)
Yes 319 (30⋅6) 24 (38) 243 (29⋅7) 52 (32⋅1)
AFP (ng/ml) 0⋅018
≤ 400 725 (80⋅7) 52 (88) 564 (81⋅7) 109 (73⋅2)
> 400 173 (19⋅3) 7 (12) 126 (18⋅3) 40 (26⋅8)
Child–Pugh grade 0⋅620
A 704 (95⋅3) 47 (94) 534 (95⋅7) 123 (93⋅9)
B 35 (4⋅7) 3 (6) 24 (4⋅3) 8 (6⋅1)
Minimally invasive surgery < 0⋅001
No 792 (75⋅5) 29 (46) 621 (75⋅5) 142 (87⋅1)
Yes 257 (24⋅5) 34 (54) 202 (24⋅5) 21 (12⋅9)
Type of resection < 0⋅001
Minor 668 (65⋅4) 53 (87) 526 (65⋅7) 89 (55⋅6)
Major 354 (34⋅6) 8 (13) 275 (34⋅3) 71 (44⋅4)
Tumour size (cm)* 5⋅0 (3⋅0–8⋅5) 1⋅5 (1⋅2–1⋅7) 5⋅0 (3⋅2–8⋅5) 6⋅0 (4⋅3–9⋅0) < 0⋅001‡
Differentiation grade 0⋅243
Well/moderate 806 (80⋅2) 45 (78) 639 (81⋅3) 122 (75⋅8)
Poor/undifferentiated 199 (19⋅8) 13 (22) 147 (18⋅7) 39 (24⋅2)
Lymphovascular invasion < 0⋅001
No 560 (62⋅0) 50 (85) 439 (63⋅6) 71 (46⋅1)
Yes 343 (38⋅0) 9 (15) 251 (36⋅4) 83 (53⋅9)
Liver capsule involvement < 0⋅001
No 513 (67⋅8) 40 (87) 405 (69⋅0) 68 (54⋅8)
Yes 244 (32⋅2) 6 (13) 182 (31⋅0) 56 (45⋅2)
Margin status 0⋅024
R0 907 (88⋅6) 54 (93) 720 (89⋅4) 133 (82⋅6)
R1 117 (11⋅4) 4 (7) 85 (10⋅6) 28 (17⋅4)
Tumour burden score < 0⋅001
Low 269 (25⋅5) 63 (100) 206 (24⋅9) –
Medium 675 (64⋅1) – 535 (64⋅8) 140 (85⋅4)
High 109 (10⋅4) – 85 (10⋅3) 24 (14⋅6)
Values in parentheses are percentages unless indicated otherwise; *values are median (i.q.r.). Data were incomplete for some variables. BCLC, Barcelona
Clinic Liver Cancer; HBV, hepatitis B virus; HCV, hepatitis C virus; AFP, α-fetoprotein. †χ2 or Fisher’s exact test, except ‡Kruskal–Wallis one-way
ANOVA.
© 2020 BJS Society Ltd www.bjs.co.uk BJS
Published by John Wiley & Sons Ltd
D. I. Tsilimigras, D. Moris, J. M. Hyer, F. Bagante, K. Sahara, A. Moro et al.
Fig. 1 Kaplan–Meier survival curves for entire cohort by Barcelona Clinic Liver Cancer stage and tumour burden score
a Overall survival by BCLC stage b Overall survival by TBS
1·0 1·0
0·8 0·8
Overall survival
Overall survival
0·6 0·6
0·4 0·4
BCLC-0 Low TBS
BCLC-A Medium TBS
0·2 0·2
BCLC-B High TBS
0 12 24 36 48 60 0 12 24 36 48 60
Time after surgery (months) Time after surgery (months)
No. at risk No. at risk
BCLC-0 63 51 38 30 20 15 Low TBS 269 215 156 120 86 62
BCLC-A 826 628 464 337 232 171 Medium TBS 675 523 385 276 190 171
BCLC-B 164 122 77 57 39 24 High TBS 109 63 38 28 20 14
c Disease-free survival by TBS
1·0
0·8
Disease-free survival
0·6
0·4
Low TBS
0·2
Medium TBS
High TBS
0 12 24 36 48 60
Time after surgery (months)
No. at risk
Low TBS 269 182 112 79 47 32
Medium TBS 675 410 252 173 115 82
High TBS 109 43 21 17 12 10
a Overall survival by Barcelona Clinic Liver Cancer (BCLC) stage; b overall and c disease-free survival by tumour burden score (TBS). a P = 0⋅010,
b P < 0⋅001, c P < 0⋅001 (log rank test).
External validation cohort Statistical analysis
The ability of TBS to predict prognosis was subsequently Descriptive statistics for continuous and categorical
validated externally. Data from patients who underwent variables are presented as median (i.q.r.) and number
hepatectomy with curative intent for HCC between 2007 (percentage) respectively. Bivariable analyses comprised
and 2019 at Cleveland Clinic, Cleveland, Ohio, USA, Kruskal–Wallis one-way ANOVA for continuous variables
were analysed. The external validation cohort included and χ2 or Fisher’s exact test for categorical variables, as
patients who met the same inclusion criteria as those in the appropriate. Bivariable survival analyses were performed
multi-institutional cohort. The institutional review board using Kaplan–Meier curves and the log rank test. Vari-
approved the study. ables that were significant in bivariable Cox regression
© 2020 BJS Society Ltd www.bjs.co.uk BJS
Published by John Wiley & Sons Ltd
Tumour burden score for hepatocellular carcinoma
Fig. 2 Kaplan–Meier survival curves by tumour burden score for Barcelona Clinic Liver Cancer stages A and B separately
a Overall survival, BCLC-A b Overall survival, BCLC-B
1·0 1·0
0·8 0·8
Overall survival
Overall survival
0·6 0·6
0·4 0·4
Low TBS
Medium TBS
0·2 High TBS 0·2
0 12 24 36 48 60 0 12 24 36 48 60
Time after surgery (months) Time after surgery (months)
No. at risk No. at risk
Low TBS 206 164 118 90 66 47 Medium TBS 140 106 71 53 37 23
Medium TBS 535 417 314 223 153 111 High TBS 24 16 6 4 2 1
High TBS 85 47 32 24 18 13
c Disease-free survival, BCLC-A d Disease-free survival, BCLC-B
1·0 1·0
0·8 0·8
Disease-free survival
Disease-free survival
0·6 0·6
0·4 0·4
0·2 0·2
0 12 24 36 0 12 24 36
Time after surgery (months) Time after surgery (months)
No. at risk No. at risk
Low TBS 206 139 83 58 Medium TBS 140 76 42 26
Medium TBS 535 334 210 147 High TBS 24 8 2 1
High TBS 85 35 19 16
Overall survival for patients with a Barcelona Clinic Liver Cancer (BCLC) A and b BCLC-B tumours; and disease-free survival for patients with c BCLC-A
and d BCLC-B tumours by tumour burden score (TBS). a P < 0⋅001, b P < 0⋅001, c P = 0⋅008, d P = 0⋅043 (log rank test).
analysis (P < 0⋅050) were entered into a multivariable included in the final cohort. Overall, 63 patients (6⋅0 per
model, and backward step selection was used to eliminate cent) had BCLC-0, 826 (78⋅4 per cent) had BCLC-A
non-significant variables using P < 0⋅100. The level of and 164 (15⋅6 per cent) had BCLC-B HCC (Table 1).
statistical significance for all tests was set at α = 0⋅05. All Median age was 67 (i.q.r. 59–73) years and most patients
statistical analyses were undertaken in SPSS version 25 were men (789, 75⋅1 per cent). The ASA fitness grade
(IBM, Armonk, New York, USA) and SAS® version 9.4 was II or less in 578 patients (62⋅5 per cent). There was
(SAS Institute, Cary, North Carolina, USA). a history of cirrhosis, HBV and HCV infection in 404
(38⋅5 per cent), 272 (26⋅1 per cent) and 319 (30⋅6 per
Results cent) patients respectively. One-quarter of the patients
A total of 1053 patients who underwent resection of HCC (257, 24⋅5 per cent) underwent a minimally invasive pro-
with curative intent met the inclusion criteria and were cedure and one-third (354, 34⋅6 per cent) had a major
© 2020 BJS Society Ltd www.bjs.co.uk BJS
Published by John Wiley & Sons Ltd
D. I. Tsilimigras, D. Moris, J. M. Hyer, F. Bagante, K. Sahara, A. Moro et al.
Fig. 3 Kaplan–Meier overall survival curves according to com-
patients with BCLC-0 HCC had a low TBS. Patients with
bined tumour burden score and Barcelona Clinic Liver Cancer BCLC-A tumours had a low (206, 24⋅9 per cent), medium
stage subgroups (535, 64⋅8 per cent) or high (85, 10⋅3 per cent) TBS,
whereas those with BCLC-B HCC had a medium (140,
BCLC-A/low TBS
85⋅4 per cent) or high (24, 14⋅6 per cent) TBS (P < 0⋅001).
BCLC-A/medium TBS
BCLC-A/high TBS
BCLC-B/medium TBS
BCLC-B/high TBS Tumour burden score predicts survival across
1·0 BCLC stages
0·8 After a median follow-up of 27⋅4 (i.q.r. 12⋅6–52⋅4) months,
5-year OS following liver resection with curative intent
Overall survival
0·6 was 62⋅9 per cent for the entire cohort. Five-year OS
varied based on BCLC stage (78, 63⋅8 and 52⋅8 per cent
0·4
respectively for BCLC-0, BCLC-A and BCLC-B respec-
0·2 tively; P = 0⋅010) (Fig. 1a). TBS was also able to stratify
prognosis as OS worsened incrementally with higher TBS
0 12 24 36 48 60 (5-year OS: 77⋅9, 61 and 39 per cent for low, medium and
Time after surgery (months) high TBS respectively; P < 0⋅001) (Fig. 1b). Of note, TBS
No. at risk was also associated with DFS (5-year DFS: 40⋅7, 35⋅4 and
BCLC-A/low
206 164 118 90 66 47
28⋅5 per cent for low, medium and high TBS respectively;
TBS
BCLC-A/medium
P < 0⋅001) (Fig. 1c).
535 417 314 223 153 111
TBS To investigate whether TBS could predict outcomes
BCLC-A/high
TBS
85 47 32 24 18 13 across BCLC stages, subgroup analyses were performed
BCLC-B/medium among patients with BCLC-A and BCLC-B HCC. In
140 106 71 53 37 23
TBS the BCLC-A group, OS worsened incrementally with
BCLC-B/high
TBS
24 16 6 4 2 1 higher TBS (5-year OS: 78, 61⋅6 and 45 per cent for low,
medium and high TBS respectively; P < 0⋅001) (Fig. 2a).
BCLC, Barcelona Clinic Liver Cancer; TBS, tumour burden score. Similarly, among patients with BCLC-B HCC, those
P < 0⋅001 (overall), P < 0⋅001 (BCLC-A/low TBS versus BCLC-B/high with a high TBS had worse 5-year OS than those with
TBS), P = 0⋅007 (BCLC-A/low TBS versus BCLC-B/medium TBS), a medium TBS (13 versus 58⋅9 per cent respectively;
P = 0⋅005 (BCLC-A/high TBS versus BCLC-B/medium TBS) (log rank
test).
P < 0⋅001) (Fig. 2b). DFS also worsened incrementally
with higher TBS among both patients with BCLC-A
HCC (3-year DFS: 57⋅4, 49⋅4 and 38 per cent for
resection. Among 668 patients (65⋅4 per cent) who had a low, medium and high TBS respectively; P = 0⋅008)
minor resection, 459 (68⋅7 per cent) underwent anatom- (Fig. 2c) and those with BCLC-B tumours (medium
ical and 209 (31⋅3 per cent) non-anatomical resection. versus high 31⋅4 and 15 per cent respectively; P = 0⋅043)
Median tumour size was 5⋅0 (3⋅0–8⋅5) cm and the major- (Fig. 2d).
ity of patients (806, 80⋅2 per cent) had a well or moder-
ate tumour differentiation grade. On final pathology, 343
Tumour burden score as a tool to select patients
patients (38⋅0 per cent) had lymphovascular invasion and
for resection beyond BCLC criteria
244 (32⋅2 per cent) had liver capsule involvement. Surgical
margin status was R0 in the majority of patients (907, To identify subgroups of patients with BCLC-B tumours
88⋅6 per cent). who had favourable outcomes after resection, combina-
tions of BCLC stage and TBS were analysed. Patients
with a similar TBS had comparable outcomes, irrespec-
Distribution of tumour burden score
tive of BCLC stage (5-year OS: 61⋅6 versus 58⋅9 per
Patients were divided into three groups according to the cent for BCLC-A/medium TBS versus BCLC-B/medium
TBS: high TBS (over 13⋅74; 109, 10⋅4 per cent), medium TBS, P = 0⋅930; 45 versus 13 per cent for BCLC-A/high
TBS (3⋅36–13⋅74; 675, 64⋅1 per cent) and low TBS (less TBS versus BCLC-B/high TBS; P = 0⋅175) (Fig. 3). Per-
than 3⋅36; 269, 25⋅5 per cent) (Fig. S1, supporting informa- haps of more interest, patients with BCLC-B HCC and a
tion). The distribution of TBS values across BCLC stages medium TBS had even better 5-year OS than those with
is shown in Fig. S2 (supporting information). Of note, all 63 BCLC-A tumours and a high TBS (58⋅9 versus 45 per cent;
© 2020 BJS Society Ltd www.bjs.co.uk BJS
Published by John Wiley & Sons Ltd
Tumour burden score for hepatocellular carcinoma
Table 2 Multivariable Cox regression analysis of survival
BCLC-A BCLC-B
Hazard ratio P Hazard ratio P
Age (years)
≤ 65 1⋅00 (reference)
> 65 1⋅48 (1⋅13, 1⋅93) 0⋅004
ASA fitness grade
≤2 1⋅00 (reference)
>2 2⋅05 (1⋅17, 3⋅60) 0⋅012
Cirrhosis
No 1⋅00 (reference)
Yes 2⋅07 (1⋅56, 2⋅75) < 0⋅001
HBV infection
No 1⋅00 (reference)
Yes 0⋅74 (0⋅53, 1⋅04) 0⋅087
AFP (ng/ml)
≤ 400 1⋅00 (reference)
> 400 1⋅65 (1⋅23, 2⋅22) 0⋅001
Differentiation grade
Well/moderate 1⋅00 (reference) 1⋅00 (reference)
Poor/undifferentiated 1⋅33 (0⋅98, 1⋅80) 0⋅059 2⋅80 (1⋅57, 5⋅02) 0⋅001
Lymphovascular involvement
No 1⋅00 (reference)
Yes 1⋅86 (1⋅41, 2⋅46) < 0⋅001
Margin status
R0 1⋅00 (reference)
R1 1⋅61 (1⋅07, 2⋅42) 0⋅020
Tumour burden score
Low 1⋅00 (reference)
Medium 2⋅07 (1⋅42, 3⋅02) < 0⋅001 1⋅00 (reference)
High 4⋅05 (2⋅40, 6⋅82) < 0⋅001 3⋅85 (2⋅03, 7⋅30) < 0⋅001
Values in parentheses are 95 per cent confidence intervals. The final step of the backward stepwise model is presented for both Barcelona Clinic Liver
Cancer (BCLC) A and B stages. HBV, hepatitis B virus; AFP, α-fetoprotein.
P = 0⋅005). In contrast, patients with BCLC-A HCC and a to 1⋅93; P = 0⋅004), cirrhosis (HR 2⋅07, 1⋅56 to 2⋅75;
low TBS had better 5-year OS than those with BCLC-B P < 0⋅001), AFP level exceeding 400 ng/ml (HR 1⋅65, 1⋅23
tumours and a medium (78 versus 58⋅9 per cent; P = 0⋅007) to 2⋅22; P = 0⋅001), lymphovascular involvement (HR
or high (78 versus 13 per cent; P < 0⋅001) TBS. 1⋅86, 1⋅41 to 2⋅46; P < 0⋅001), R1 resection (HR 1⋅61,
1⋅07 to 2⋅42; P = 0⋅020) and higher TBS (versus low TBS;
Factors associated with overall survival after medium TBS: HR 2⋅07, 1⋅42 to 3⋅02, P < 0⋅001; high TBS:
resection for BCLC-A and BCLC-B hepatocellular HR 4⋅05, 2⋅40 to 6⋅82, P < 0⋅001) remained independent
carcinoma predictors of OS among patients with BCLC-A HCC
(Table 2). Only ASA grade above II (HR 2⋅05, 1⋅17 to 3⋅60;
A number of clinicopathological factors were associ- P = 0⋅012), poor/undifferentiated tumour grade (HR 2⋅80,
ated with prognosis after resection for BCLC-A and 1⋅57 to 5⋅02; P = 0⋅001) and high TBS (versus medium TBS:
BCLC-B HCC (Table S1, supporting information). In HR 3⋅85, 2⋅03 to 7⋅30; P < 0⋅001) independently predicted
univariable analysis, minimally invasive surgery was not worse outcomes among patients with BCLC-B HCC.
associated with long-term survival among patients with
BCLC-A (hazard ratio (HR) 0⋅76, 95 per cent c.i. 0⋅54
External validation of tumour burden score
to 1⋅08; P = 0⋅127) or BCLC-B (HR 0⋅62, 0⋅24 to 1⋅55;
P = 0⋅305) disease. In multivariable analysis, after adjusting The ability of TBS to stratify prognosis among patients
for competing factors, age over 65 years (HR 1⋅48, 1⋅13 undergoing resection with curative intent for HCC was
© 2020 BJS Society Ltd www.bjs.co.uk BJS
Published by John Wiley & Sons Ltd
D. I. Tsilimigras, D. Moris, J. M. Hyer, F. Bagante, K. Sahara, A. Moro et al.
Fig. 4 Kaplan–Meier survival curves by tumour burden score for external validation cohort
a Overall survival, entire cohort b Overall survival, BCLC-A
1·0 1·0
0·8 0·8
Overall survival
Overall survival
0·6 0·6
0·4 0·4
Low TBS
0·2 Medium TBS 0·2
High TBS
0 12 24 36 48 60 0 12 24 36 48 60
Time after surgery (months) Time after surgery (months)
No. at risk No. at risk
Low TBS 42 33 24 17 13 10 Low TBS 32 26 17 12 10 8
Medium TBS 100 66 43 32 19 15 Medium TBS 75 48 34 25 15 13
High TBS 16 11 8 3 3 2 High TBS 12 8 5 2 2 1
c Disease-free survival, entire cohort d Disease-free survival, BCLC-A
1·0 1·0
0·8 0·8
Disease-free survival
Disease-free survival
0·6 0·6
0·4 0·4
0·2 0·2
0 12 24 0 12 24
Time after surgery (months) Time after surgery (months)
No. at risk No. at risk
Low TBS 42 26 20 Low TBS 32 20 8
Medium TBS 100 43 27 Medium TBS 74 31 20
High TBS 16 3 2 High TBS 12 2 1
Overall survival for a entire cohort and b Barcelona Clinic Liver Cancer (BCLC) A subgroup; and disease-free survival for c entire cohort and d BCLC-A
subgroup by tumour burden score (TBS). a P = 0⋅010, b P = 0⋅006, c P < 0⋅001, d P < 0⋅001 (log rank test).
validated using an external cohort of 158 patients from Survival analysis based on the TBS revealed excellent
Cleveland Clinic. A total of 41 patients (25⋅9 per cent) prognostic discrimination across the entire cohort. Patients
underwent minimally invasive surgery in the external val- with a low, medium and high TBS had a 5-year OS of
idation cohort, similar to the multi-institutional data set. 79, 51⋅2 and 28 per cent respectively (P = 0⋅010) (Fig. 4a).
Ten patients (6⋅3 per cent) had BCLC-0, 119 (75⋅3 per Similarly, patients with BCLC-A tumours had an incre-
cent) had BCLC-A and 29 (18⋅4 per cent) had BCLC-B mentally worse 5-year OS with higher TBS (72, 55 and
HCC. The distribution of TBS in the entire cohort was 21 per cent respectively for low, medium and high TBS;
low (42, 26⋅6 per cent), medium (100, 63⋅3 per cent) and P = 0⋅006) (Fig. 4b). Among patients with a medium TBS,
high (16, 10⋅1 per cent). there was no difference in OS between those with BCLC-A
© 2020 BJS Society Ltd www.bjs.co.uk BJS
Published by John Wiley & Sons Ltd
Tumour burden score for hepatocellular carcinoma
versus BCLC-B HCC (5-year OS: 55 versus 42 per cent: subclassified patients with BCLC-B HCC into four dif-
P = 0⋅214). Similarly, DFS worsened with higher TBS ferent groups according to the beyond Milan and up-to-7
among patients in the entire cohort (3-year DFS: 71, 53⋅8 criteria, suggesting distinct prognosis and treatment
and 17 per cent for low, medium and high TBS respectively; approaches for each subgroup. Wang and co-workers26
P < 0⋅001) (Fig. 4c), as well as among those with BCLC-A proposed a modified BCLC system, with HCC exceeding
HCC (3-year DFS: 74, 54 and 12 per cent respectively; 7 cm considered BCLC-B instead of BCLC-A. The ITA
P = 0⋅001) (Fig. 4d). .LI.CA study group25 proposed a new staging system and
suggested subclasses within BCLC stages, considering
different cut-off values for tumour number and size. No
Discussion
previous study has used the TBS to stratify prognosis after
In the USA, the incidence of HCC has increased steadily resection of HCC across BCLC stages.
over the past three decades, with a concomitant increase By using the Pythagorean theorem (α2 = β2 + γ2 ), TBS
in HCC mortality1,3 . Cancer staging is necessary to accu- takes into account the collective impact of tumour number
rately predict the prognosis of patients with HCC as well and tumour size, which are known predictors of overall dis-
as to define the appropriate treatment strategy5,6 . Among ease burden18 . Of note, the TBS calculates disease burden
the traditional staging systems, the BCLC classification in a continuous, rather than dichotomous, fashion, which
is unique in that it assesses patient prognosis, but also allows a more granular prognostication of outcomes than
recommends a specific treatment strategy based on the the established Milan or up-to-7 criteria18,27 . The ITA.LI
respective prognostic stages defined by the classification .CA group27 recently demonstrated better discriminative
itself7,8 . Nevertheless, there has recently been debate as ability of the TBS compared with the Milan criteria and
to whether this system performs well in terms of prog- other tumour-specific scores, with a 6 per cent increased
nostic stratification. Previous studies11,12 have shown het- risk of death for each point increase in TBS. By using the
erogeneous outcomes after HCC resection of the same X-tile bioinformatics tool21 , the optimal cut-off values of
stage, especially among patients with BCLC-A HCC. TBS in relation to OS were determined in the present
Indeed, a strong relationship between tumour size and inci- study. Interestingly, although patients with BCLC-0 dis-
dence of microvascular invasion has been demonstrated, ease had only low TBS values, patients with BCLC-A
suggesting an increased possibility of recurrence among tumours had scores ranging from low to high (Fig. S2,
patients with large BCLC-A HCC22,23 . Previous studies supporting information). In turn, outcomes after resection
have attempted to subclassify patients within BCLC stages, for BCLC-A HCC were largely dependent on TBS; the
yet none of these suggestions have been adopted by the 5-year OS rate was as high as 78 per cent for patients with
most recent BCLC classification8 . In addition, these sub- a low TBS, but only 45 per cent among those with a high
classifications have largely used arbitrary cut-off values of TBS. Similarly, TBS was able to stratify prognosis among
tumour number and size that assume an independent rather patients with BCLC-B HCC. Patients with BCLC-B dis-
than related effect of these variables on outcomes after ease and a medium TBS had a 5-year OS rate that was
resection. even better than that of patients with BCLC-A HCC and a
The present study used TBS, a recently developed mea- high TBS (58⋅9 versus 45 per cent; P = 0⋅005). Importantly,
sure that incorporates both tumour number and size in a TBS remained an independent predictor of OS among
continuous fashion, to determine prognosis after resection both BCLC-A and BCLC-B groups. TBS could also pre-
of HCC across different BCLC stages. Of note, patients dict DFS across the entire cohort, as well as within the
had a range of TBS values among the different BCLC different BCLC stages. The value of TBS and its predic-
stages, yet those with a similar TBS had comparable out- tive performance in terms of OS and DFS was validated
comes, irrespective of BCLC stage. In fact, patients with in an independent external cohort. Data from the present
BCLC-B HCC and a medium TBS had better outcomes study strongly suggest that TBS could be used as an adjunc-
than those with BCLC-A tumours who had a high TBS. tive tool to stratify prognosis among patients undergoing
Furthermore, TBS remained an independent predictor of resection for HCC, and to identify subgroups of patients
OS among both BCLC-A and BCLC-B stages even after within each BCLC stage who may benefit most from
controlling for competing factors. Importantly, the TBS surgery.
could discriminate prognosis accurately when applied to an Although the current BCLC guidelines recommend
external validation cohort. surgery only for BCLC-A HCC, hepatobiliary sur-
Several investigators24,25 have suggested subclassifica- geons have questioned whether resection of HCC
tions within BCLC stages. Bolondi and colleagues24 should be undertaken in selected patients with BCLC-B
© 2020 BJS Society Ltd www.bjs.co.uk BJS
Published by John Wiley & Sons Ltd
D. I. Tsilimigras, D. Moris, J. M. Hyer, F. Bagante, K. Sahara, A. Moro et al.
tumours16,28,29 . Indeed, an increasing number of influenced the results of the study. Finally, the lack of a
studies16,30 – 35 have reported acceptable outcomes after comparison group did not allow assessment of whether
resection for BCLC-B HCC, suggesting that liver resec- the TBS would also be able to stratify prognosis among
tion may be justified beyond the BCLC resection criteria patients with BCLC-B HCC who underwent locoregional
in selected patients. For example, Wada and colleagues13 therapies (TACE). The present data emphasize the need
reported a 5-year OS rate of 63⋅4 per cent after liver for further subclassification within the current BCLC
resection for multinodular BCLC-B HCC. Kim and guidelines, and highlight the need for refinement of the
co-workers30 reported superior outcomes with resection proposed treatment algorithm using an assessment of total
versus non-surgical treatment for BCLC-B HCC in a tumour burden.
propensity score-matched analysis (5-year OS: 63 versus
22 per cent). In another study33 , resection of multinodular Disclosure
HCC was associated with an acceptable 5-year OS rate
of 57 per cent among patients with BCLC-B disease. The authors declare no conflict of interest.
A propensity-score matched study34 from Asia similarly
noted a survival benefit with liver resection versus TACE References
for patients with BCLC-B/C HCC. Of note, a recent
1 Beal EW, Tumin D, Kabir A, Moris D, Zhang XF,
meta-analysis16 revealed a survival benefit of surgery com- Chakedis J et al. Trends in the mortality of hepatocellular
pared with TACE for BCLC-B disease, raising questions carcinoma in the United States. J Gastrointest Surg 2017; 21:
about the treatment algorithm proposed by the current 2033–2038.
BCLC classification. 2 Lafaro KJ, Demirjian AN, Pawlik TM. Epidemiology of
In the present analysis of a large multi-institutional hepatocellular carcinoma. Surg Oncol Clin N Am 2015; 24:
database, an acceptable 5-year OS rate of 52⋅8 per cent was 1–17.
noted among patients with BCLC-B HCC. Furthermore, 3 Fujiwara N, Friedman SL, Goossens N, Hoshida Y. Risk
applying the TBS, it was found that patients with BCLC-B factors and prevention of hepatocellular carcinoma in the
era of precision medicine. J Hepatol 2018; 68: 526–549.
and a medium TBS had outcomes comparable to those with
4 Petrick JL, Kelly SP, Altekruse SF, McGlynn KA,
BCLC-A HCC and a medium TBS, and even better out-
Rosenberg PS. Future of hepatocellular carcinoma incidence
comes than those with BCLC-A HCC and a high TBS. in the United States forecast through 2030. J Clin Oncol
Collectively, these data suggest that surgery could indeed 2016; 34: 1787–1794.
be beneficial in selected patients with BCLC-B HCC and 5 Marrero JA, Fontana RJ, Barrat A, Askari F, Conjeevaram
so resection should not be denied a priori to such patients. HS, Su GL et al. Prognosis of hepatocellular carcinoma:
Rather, the TBS may be helpful in identifying patients with comparison of 7 staging systems in an American cohort.
BCLC-B HCC beyond the current BCLC criteria who Hepatology 2005; 41: 707–716.
may derive a survival benefit and therefore be candidates 6 O’Neil BH, Venook AP. Hepatocellular carcinoma: the role
for resection. of the North American GI Steering Committee
Hepatobiliary Task Force and the advent of effective drug
The present study has certain limitations that should be
therapy. Oncologist 2007; 12: 1425–1432.
taken into consideration when interpreting the results. As
7 Cillo U, Vitale A, Grigoletto F, Farinati F, Brolese A,
with all retrospective studies, it may be subject to selec- Zanus G et al. Prospective validation of the Barcelona
tion bias regarding which patients were offered surgery Clinic Liver Cancer staging system. J Hepatol 2006; 44:
(patients with BCLC-B HCC likely had a more favourable 723–731.
tumour profile and were fit for surgery). In addition, 8 European Association for the Study of the Liver. Electronic
most patients included in the analysis had Child–Pugh address: easloffice@easloffice.eu; European Association for
grade A liver function; the conclusions may not per- the Study of the Liver. EASL clinical practice guidelines:
tain to those with more severe underlying liver disease. management of hepatocellular carcinoma. J Hepatol 2018;
Furthermore, owing to smaller numbers in the external 69: 182–236.
9 Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS,
validation cohort, it was not possible to undertake fur-
Abecassis MM et al. Diagnosis, staging, and management of
ther survival analyses to examine whether patients with
hepatocellular carcinoma: 2018 practice guidance by the
BCLC-B HCC and a medium TBS had better outcomes American Association for the Study of Liver Diseases.
than those with BCLC-A tumours and a high TBS, as Hepatology 2018; 68: 723–750.
shown in the multi-institutional cohort. There was also a 10 European Association for the Study of the Liver; European
slight difference in study periods for the multi-institutional Organisation For Research and Treatment of Cancer.
and external validation cohorts, but this is unlikely to have EASL-EORTC clinical practice guidelines: management of
© 2020 BJS Society Ltd www.bjs.co.uk BJS
Published by John Wiley & Sons Ltd
Tumour burden score for hepatocellular carcinoma
hepatocellular carcinoma. J Hepatol 2012; 56: histologic grade: implications for selection of surgical
908–943. treatment for hepatocellular carcinoma. Liver Transpl 2005;
11 Guo H, Wu T, Lu Q, Li M, Guo JY, Shen Y et al. Surgical 11: 1086–1092.
resection improves long-term survival of patients with 24 Bolondi L, Burroughs A, Dufour JF, Galle PR,
hepatocellular carcinoma across different Barcelona Clinic Mazzaferro V, Piscaglia F et al. Heterogeneity of patients
Liver Cancer stages. Cancer Manag Res 2018; 10: with intermediate (BCLC B) hepatocellular carcinoma:
361–369. proposal for a subclassification to facilitate treatment
12 Cho Y, Sinn DH, Yu SJ, Gwak GY, Kim JH, Yoo YJ et al. decisions. Semin Liver Dis 2012; 32: 348–359.
Survival analysis of single large (> 5 cm) hepatocellular 25 Farinati F, Vitale A, Spolverato G, Pawlik TM, Huo TL,
carcinoma patients: BCLC A versus B. PLoS One 2016; 11: Lee YH et al.; ITA.LI.CA study group. Development
e0165722. and validation of a new prognostic system for patients
13 Wada H, Eguchi H, Noda T, Ogawa H, Yamada D, with hepatocellular carcinoma. PLoS Med 2016; 13:
Tomimaru Y et al. Selection criteria for hepatic resection in e1002006.
intermediate-stage (BCLC stage B) multiple hepatocellular 26 Wang YY, Zhong JH, Xu HF, Xu G, Wang LJ, Xu D et al. A
carcinoma. Surgery 2016; 160: 1227–1235. modified staging of early and intermediate hepatocellular
14 Bhandare MS, Patkar S, Shetty N, Polnaya A, Kulkarni S, carcinoma based on single tumour >7 cm and multiple
Dusane RR et al. Liver resection for HCC outside the tumours beyond up-to-seven criteria. Aliment Pharmacol
BCLC criteria. Langenbecks Arch Surg 2018; 403: Ther 2019; 49: 202–210.
37–44. 27 Vitale A, Lai Q, Farinati F, Bucci L, Giannini EG, Napoli L
15 Moris D, Felekouras E. Ignore reality but not the et al. Utility of tumor burden score to stratify prognosis of
consequences of its ignorance: broaden guidelines in surgery patients with hepatocellular cancer: results of 4759 cases
of hepatocellular carcinoma. Hepatology 2017; 65: from ITA.LI.CA study group. J Gastrointest Surg 2018; 22:
1772–1773. 859–871.
16 Hyun MH, Lee YS, Kim JH, Lee CU, Jung YK, Seo YS 28 Moris D, Tsilimigras DI, Kostakis ID,
et al. Hepatic resection compared to chemoembolization in Ntanasis-Stathopoulos I, Shah KN, Felekouras E et al.
intermediate- to advanced-stage hepatocellular carcinoma: a Anatomic versus non-anatomic resection for hepatocellular
meta-analysis of high-quality studies. Hepatology 2018; 68: carcinoma: a systematic review and meta-analysis. Eur
977–993. J Surg Oncol 2018; 44: 927–938.
17 Golfieri R, Bargellini I, Spreafico C, Trevisani F. Patients 29 Lim C, Salloum C, Osseis M, Lahat E, Gómez-Gavara C,
with Barcelona Clinic Liver Cancer stages B and C Compagnon P et al. Short-term outcomes following
hepatocellular carcinoma: time for a subclassification. Liver hepatectomy for hepatocellular carcinoma within and
Cancer 2019; 8: 78–91. beyond the BCLC guidelines: a prospective study. HPB
18 Sasaki K, Morioka D, Conci S, Margonis GA, Sawada Y, (Oxford) 2018; 20: 222–230.
Ruzzenente A et al. The tumor burden score: a new 30 Kim H, Ahn SW, Hong SK, Yoon KC, Kim HS,
‘metro-ticket’ prognostic tool for colorectal liver metastases Choi YR et al.; Korean Liver Cancer Association. Survival
based on tumor size and number of tumors. Ann Surg 2018; benefit of liver resection for Barcelona Clinic Liver Cancer
267: 132–141. stage B hepatocellular carcinoma. Br J Surg 2017; 104:
19 Tsilimigras DI, Bagante F, Moris D, Merath K, Paredes AZ, 1045–1052.
Sahara K et al. Defining the chance of cure after resection for 31 Liang L, Xing H, Zhang H, Zhong J, Li C, Lau WY et al.
hepatocellular carcinoma within and beyond the Barcelona Surgical resection versus transarterial chemoembolization
Clinic Liver Cancer guidelines: a multi-institutional analysis for BCLC intermediate stage hepatocellular carcinoma: a
of 1010 patients. Surgery 2019; 166: 967–974. systematic review and meta-analysis. HPB (Oxford) 2018; 20:
20 Strasberg SM. Nomenclature of hepatic anatomy and 110–119.
resections: a review of the Brisbane 2000 system. 32 Tsilimigras DI, Bagante F, Sahara K, Moris D, Hyer JM,
J Hepatobiliary Pancreat Surg 2005; 12: 351–355. Wu L et al. Prognosis after resection of Barcelona Clinic
21 Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new Liver Cancer (BCLC) stage 0, A, and B hepatocellular
bio-informatics tool for biomarker assessment and carcinoma: a comprehensive assessment of the current
outcome-based cut-point optimization. Clin Cancer Res BCLC classification. Ann Surg Oncol 2019; 26:
2004; 10: 7252–7259. 3693–3700.
22 Esnaola NF, Lauwers GY, Mirza NQ, Nagorney DM, 33 Torzilli G, Belghiti J, Kokudo N, Takayama T,
Doherty D, Ikai I et al. Predictors of microvascular invasion Capussotti L, Nuzzo G et al. A snapshot of the effective
in patients with hepatocellular carcinoma who are indications and results of surgery for hepatocellular
candidates for orthotopic liver transplantation. J Gastrointest carcinoma in tertiary referral centers: is it adherent to the
Surg 2002; 6: 224–232. EASL/AASLD recommendations?: an observational study
23 Pawlik TM, Delman KA, Vauthey JN, Nagorney DM, Ng of the HCC East–West study group. Ann Surg 2013; 257:
IO, Ikai I et al. Tumor size predicts vascular invasion and 929–937.
© 2020 BJS Society Ltd www.bjs.co.uk BJS
Published by John Wiley & Sons Ltd
D. I. Tsilimigras, D. Moris, J. M. Hyer, F. Bagante, K. Sahara, A. Moro et al.
34 Zhong JH, Ke Y, Gong WF, Xiang BD, Ma L, Ye XP et al. 35 Wang JH, Changchien CS, Hu TH, Lee CM, Kee KM, Lin
Hepatic resection associated with good survival for selected CY et al. The efficacy of treatment schedules according to
patients with intermediate and advanced-stage Barcelona Clinic Liver Cancer staging for hepatocellular
hepatocellular carcinoma. Ann Surg 2014; 260: carcinoma – survival analysis of 3892 patients. Eur J Cancer
329–340. 2008; 44: 1000–1006.
Supporting information
Additional supporting information can be found online in the Supporting Information section at the end of the
article.
© 2020 BJS Society Ltd www.bjs.co.uk BJS
Published by John Wiley & Sons Ltd
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- PANCE Prep Pearls Cardio Questions PDFDocument9 pagesPANCE Prep Pearls Cardio Questions PDFkat100% (3)
- Imaging of Kidney Cancer - GuermaziDocument439 pagesImaging of Kidney Cancer - GuermaziNar RungrojanarakNo ratings yet
- Sop Icu H & FW 12725 28.04.2018Document20 pagesSop Icu H & FW 12725 28.04.2018shah007zaadNo ratings yet
- Hse Statistics Report Pp701 Hse f04 Rev.bDocument1 pageHse Statistics Report Pp701 Hse f04 Rev.bMohamed Mouner100% (1)
- Stadardization of Ayurvedic Clinical TerminologiesDocument242 pagesStadardization of Ayurvedic Clinical TerminologiesAbhishek100% (1)
- Reproductive and Child Health ProgrammeDocument10 pagesReproductive and Child Health ProgrammeMebin NinanNo ratings yet
- Constipation 508Document12 pagesConstipation 508Shishir Kumar SinghNo ratings yet
- Icru Report 62Document62 pagesIcru Report 62Luis Ramirez100% (1)
- IELTS WordsDocument97 pagesIELTS WordsLeeNo ratings yet
- An Unresectable Klatskin's Tumor?: Johannes Hartl, Tobias Werner, and Christoph SchrammDocument2 pagesAn Unresectable Klatskin's Tumor?: Johannes Hartl, Tobias Werner, and Christoph SchrammLourdes MollardNo ratings yet
- Optimal Timing For Surgical Reconstruction of BDI PDFDocument11 pagesOptimal Timing For Surgical Reconstruction of BDI PDFLourdes MollardNo ratings yet
- Optimal Timing For Surgical Reconstruction of BDI PDFDocument11 pagesOptimal Timing For Surgical Reconstruction of BDI PDFLourdes MollardNo ratings yet
- Surgical Management of Portal Hypertension in Children PDFDocument14 pagesSurgical Management of Portal Hypertension in Children PDFLourdes MollardNo ratings yet
- Multimodality Imaging of The Meso-Rex Bypass PDFDocument16 pagesMultimodality Imaging of The Meso-Rex Bypass PDFLourdes MollardNo ratings yet
- Meso Rex Bypass A Procedure To Cure Prehepatic Portal Hypertension The Insight and The Inside PDFDocument14 pagesMeso Rex Bypass A Procedure To Cure Prehepatic Portal Hypertension The Insight and The Inside PDFLourdes MollardNo ratings yet
- Laparosc. VS Open Distal Resecction PDFDocument64 pagesLaparosc. VS Open Distal Resecction PDFLourdes MollardNo ratings yet
- Efficacy of Doctorvox On Mutational FalsettoDocument8 pagesEfficacy of Doctorvox On Mutational FalsettoANA CRISTINA MENDEZ DIAZNo ratings yet
- FM - Hse.020 Statistik HSE TahunanDocument2 pagesFM - Hse.020 Statistik HSE TahunanEka Nanda HermarianyNo ratings yet
- Quality Assurance LaboratoryDocument118 pagesQuality Assurance LaboratoryMahesh KumarNo ratings yet
- ReferensiDocument2 pagesReferensiYuanita RosalinaNo ratings yet
- Zat Aktif & PBFDocument153 pagesZat Aktif & PBFnabilaNo ratings yet
- Alpha Thalassemia PDFDocument21 pagesAlpha Thalassemia PDFAnonymous Yo0mStNo ratings yet
- The Nurse Leader's Role: Crisis ManagementDocument3 pagesThe Nurse Leader's Role: Crisis Managementravsab GaikwadNo ratings yet
- Food Industry TrainingDocument18 pagesFood Industry TrainingSumit KumarNo ratings yet
- Areport 08Document247 pagesAreport 08Mithilesh JhaNo ratings yet
- Assessment Dianosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Dianosis Planning Intervention Rationale Evaluationkyaw100% (1)
- FNCP (Open Drainage) For Soft BoundDocument3 pagesFNCP (Open Drainage) For Soft BoundSean Maghinay BanicoNo ratings yet
- Glucagon and Its Metabolic EffectsDocument31 pagesGlucagon and Its Metabolic EffectsnikenNo ratings yet
- Community Radio Script - Why We Have COVID Vaccines NowDocument2 pagesCommunity Radio Script - Why We Have COVID Vaccines NowBenBuilds PHNo ratings yet
- Xiong Et AlDocument21 pagesXiong Et AlVanessa AndradeNo ratings yet
- Blood Grouping ReagentsDocument7 pagesBlood Grouping ReagentsDominic EmerencianaNo ratings yet
- Artemisia Vulgaris MonographDocument4 pagesArtemisia Vulgaris MonographEmer BonesNo ratings yet
- GB PerforationDocument13 pagesGB Perforationmudasir61No ratings yet
- Transforming Growth Factor Beta TGFBDocument8 pagesTransforming Growth Factor Beta TGFBxxxxxxxNo ratings yet
- Running Head:: Prothrombotic Effect of Mimosa PudicDocument28 pagesRunning Head:: Prothrombotic Effect of Mimosa PudicGINAROSE DEGUZMANNo ratings yet
- A Epithelial - Tissue1 16 12 14Document32 pagesA Epithelial - Tissue1 16 12 14Abdulaziz AbdullahiNo ratings yet
- Curs de Limba PortughezaDocument16 pagesCurs de Limba PortughezaMădălina TodincaNo ratings yet