Professional Documents
Culture Documents
Nosocomial Bacterial Meningitis PDF
Uploaded by
Susy OcampoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nosocomial Bacterial Meningitis PDF
Uploaded by
Susy OcampoCopyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
review article
Current Concepts
Nosocomial Bacterial Meningitis
Diederik van de Beek, M.D., Ph.D., James M. Drake, M.B., B.Ch.,
and Allan R. Tunkel, M.D., Ph.D.
N
From the Department of Neurology, Cen- osocomial bacterial meningitis may result from invasive pro-
ter of Infection and Immunity Amsterdam, cedures (e.g., craniotomy, placement of internal or external ventricular cath-
Academic Medical Center, University of
Amsterdam, Amsterdam (D.B.); the Divi- eters, lumbar puncture, intrathecal infusions of medications, or spinal anes-
sion of Neurosurgery, Department of thesia), complicated head trauma, or in rare cases, metastatic infection in patients
Surgery, Hospital for Sick Children, Uni- with hospital-acquired bacteremia. These cases of meningitis are caused by a differ-
versity of Toronto, Toronto (J.M.D.); and
the Department of Medicine, Monmouth ent spectrum of microorganisms than cases acquired in the community setting, and
Medical Center, Long Branch, NJ (A.R.T.). illness is the result of diverse pathogenetic mechanisms (Fig. 1).
Address reprint requests to Dr. van de
Beek at the Department of Neurology,
Center of Infection and Immunity Am- Epidemiol o gy a nd Patho gene sis
sterdam (CINIMA), Academic Medical
Center, University of Amsterdam, P.O. Box The central nervous system is protected against microbial entry from the bloodstream
22660, 1100 DD Amsterdam, the Nether-
lands, or at d.vandebeek@amc.uva.nl. by the blood–brain barrier and by an external barrier that is formed by the skull and
leptomeninges. Consequently, pathogens may enter the central nervous system by di-
N Engl J Med 2010;362:146-54. rect invasion through the external barrier or through the bloodstream in association
Copyright © 2010 Massachusetts Medical Society.
with a breakdown of the blood–brain barrier. The following sections review the pre-
disposing conditions and risk factors for the development of nosocomial meningitis.
Craniotomy
Bacterial meningitis is a serious complication of craniotomy; it occurs in 0.8 to 1.5%
of patients who undergo craniotomy.1,2 Among cases of meningitis that develop in
patients after craniotomy, approximately one third occur in the first week after sur-
gery, one third in the second week, and one third after the second week, with some
cases occurring years after the initial surgery.1 The risk of postoperative meningitis
can be minimized by the practice of careful surgical techniques, especially those
that decrease the likelihood of cerebrospinal fluid leakage.1 Other factors that are
associated with the development of meningitis after craniotomy are concomitant
infection at the site of the incision and a duration of surgery of more than 4 hours.
Specific neurosurgical techniques that may minimize the risk of postoperative men-
ingitis are listed in Table 1.
Internal Ventricular Catheters
The case incidence of meningitis associated with internal ventricular catheters (i.e.,
cerebrospinal fluid shunts), which are commonly used for the treatment of hydro-
cephalus, ranges from 4 to 17%.3,4 The most important causal factor is colonization
of the catheter at the time of surgery, since the majority of infections are manifested
within 1 month after surgery.3,4 One prospective, observational study identified holes
in the surgical gloves, combined with direct handling of the shunt catheter by the
surgical team, as a possible risk factor5; double gloving led to a reduction in the rates
of catheter infections as compared with the rates among historical controls.6 One
study suggested that changing the outer pair of gloves before handling catheter mate-
rial during surgery may further decrease the rates of infection.7
146 n engl j med 362;2 nejm.org january 14, 2010
The New England Journal of Medicine
Downloaded from nejm.org by SERVICIO MEDICINA INTERNA TESAI on February 9, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
current concepts
External Ventricular Catheters of the cranium, the wound should be carefully ex-
External ventricular catheters are used for the amined and débrided, and preventive antimicro-
monitoring of intracranial pressure or the tem- bial therapy should be administered (Table 1). Non-
porary diversion of cerebrospinal fluid from an ob- operative management is an option if there is no
structed ventricular system, or as part of the treat- clinical or radiographic evidence of the following:
ment approach for infected internal catheters. The dural penetration, large intracranial hematoma,
rate of infection associated with external catheters depression that is deeper than 1 cm, involvement
is approximately 8%.8 The risk of infection is re- of the frontal sinuses, gross cosmetic deformity,
ported to be increased with an increased duration wound infection, pneumocephalus, or gross con-
of drainage, but the extent of increase per unit of tamination of the wound.12
time is uncertain. Although one study showed a The majority of patients in whom meningitis
sharp increase in the risk of infection after 5 days develops as a complication of closed head trauma
of external drainage,8 a prospective, randomized have a basilar skull fracture,11 which causes the
trial showed that removing external catheters with- subarachnoid space to be connected to the sinus
in 5 days is unnecessary and that catheters can be cavity and is associated with an increased risk of
left in place for longer periods with no obvious infection; rates of infection are reported to be as
increase in the daily risk of infection.9 Since in- high as 25%, with a median time between injury
fection may be acquired by the introduction of bac- and the onset of meningitis of 11 days.11,13 Leak-
teria after the insertion of a new catheter, chang- age of cerebrospinal fluid is the major risk factor
ing uninfected catheters might actually increase for the development of meningitis, although most
the risk of infection. Other risk factors for in- leaks that occur after trauma are unrecognized.11,13
fection are the routine sampling of cerebrospinal Most leaks resolve spontaneously within 7 days,
fluid, leakage of cerebrospinal fluid at the site, but surgical intervention is indicated if leakage
blockage of the drain, and intraventricular hem- persists. Head trauma is the most common cause
orrhage. of recurrent bacterial meningitis.14
external Lumbar catheters Lumbar Puncture
External lumbar catheters, which are placed Meningitis develops after lumbar puncture in ap-
mainly to aid in the diagnosis of normal-pressure proximately 1 in 50,000 cases, with about 80 cases
hydrocephalus, have been associated with menin- reported annually in the United States.15 The ma-
gitis rates of up to 5%.10 The risk factors associ- jority of cases occur after spinal anesthesia or my-
ated with these catheters include disconnection of elography. The risk of meningitis after lumbar
the external drainage system and the presence of puncture may be substantially decreased if asep-
other infections. In a recent study involving 233 tic conditions are met (i.e., hand disinfection and
consecutive patients who underwent placement of the use of sterile gloves) and if operators wear face
an external lumbar catheter, the rate of meningitis masks and operating caps when performing spi-
was low (0.8%)10; the investigators in that study nal anesthesia or myelography.
used a strict protocol that called for no surveil-
lance testing of cerebrospinal fluid, drainage of Patho gens
cerebrospinal fluid for a maximum of 5 days, ster-
ile reconnection after disconnection or fracture The specific bacteria that cause nosocomial men-
of the drain, and permanent removal of the cath- ingitis vary according to the pathogenesis and
eter after a second disconnection or fracture — timing of the infection after the predisposing
protocols that minimized the risk of infection. event.1,2,11,13,15-17 Meningitis that develops after
neurosurgery or in patients who are hospitalized
Head Trauma for a prolonged period after penetrating trauma
The incidence of meningitis after moderate or se- or basilar skull fracture can be caused by staphy-
vere head trauma is estimated to be 1.4%.11 Open lococci or by facultative or aerobic gram-negative
compound cranial fractures are complications of bacilli. In patients in whom foreign bodies (e.g.,
up to 5% of head injuries and have been associated internal ventricular drains) have been placed, men-
with rates of meningitis that range from 2 to 11%.12 ingitis is often caused by cutaneous organisms
In patients with compound fractures in which such as coagulase-negative staphylococci or Propi-
the skull is depressed deeper than the thickness onibacterium acnes. The majority of meningitis cases
n engl j med 362;2 nejm.org january 14, 2010 147
The New England Journal of Medicine
Downloaded from nejm.org by SERVICIO MEDICINA INTERNA TESAI on February 9, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
External CSF catheter
A
Craniotomy with Bacteria
separation of
skin and skull
Frontal horn of
lateral ventricle
C
Leukocyte
Bacteria
D E
Basal skull
fracture
Cauda
equina
Orbit
Lumbar
puncture
Needle
L5
CSF in
maxillary sinus
that occur after basilar skull fracture or early after CL INIC A L FINDINGS A ND DI AGNOSIS
COLOR
otorhinologic surgery are caused by microorgan-
FIGURE
Draft 5 isms that colonize the nasopharynx (especially
12/15/09 A clinical suspicion of nosocomial bacterial men-
Author Van de Beek Streptococcus pneumoniae). These infecting microor- ingitis should prompt a diagnostic workup and
Fig # 1
Title
ganisms are important to consider in the approach antimicrobial therapy. Fever and a decreased level
ME to empirical antimicrobial therapy (see below). of consciousness are the most consistent clinical
DE
Artist SBL
148Figure hasAUTHOR PLEASE NOTE:
been redrawn and type has been reset n engl j med 362;2 nejm.org january 14, 2010
Please check carefully
Issue date The New England Journal of Medicine
Downloaded from nejm.org by SERVICIO MEDICINA INTERNA TESAI on February 9, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
current concepts
before lumbar puncture is performed. Cerebro-
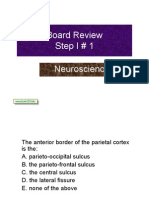
Figure 1 (facing page). Pathogenetic Mechanisms
at the Most Common Sites of Nosocomial Bacterial spinal fluid can be obtained through the cathe-
Meningitis. ter in patients with internal or external ventricu-
Bacteria may enter the meninges and subarachnoid lar catheters; otherwise, a lumbar puncture is
space from contiguous sites of colonization or foci of necessary. However, in patients with obstructive
suppuration after craniotomy (Panel A). Cerebrospinal hydrocephalus, lumbar cerebrospinal fluid may not
fluid (CSF) catheters (Panel B) have a proximal portion
be reflective of ventricular infection because of the
that enters the cerebrospinal fluid space and a distal
portion that may also be internal, terminating in the lack of communication between ventricular and
peritoneal, pleural, or vascular space, or that may be lumbar cerebrospinal fluid.
external, when the need for the catheter is temporary. The diagnosis of nosocomial bacterial menin-
Cerebrospinal fluid catheters may become infected by gitis is made on the basis of the results of a ce-
retrograde infection from the distal end of the shunt,
rebrospinal fluid culture; aerobic and anaerobic
wound or skin breakdown overlying the catheter, meta-
static infection in patients with bacteremia, or coloni- culturing techniques are obligatory. However, cul-
zation of the catheter at the time of surgery. Concen- tures require prolonged incubation before being
trations of leukocytes, antibodies, and complement confirmed as negative, and results may be nega-
components in the subarachnoid space are low, facili- tive in patients who have received previous anti-
tating multiplication of bacteria (Panel C). After head
microbial therapy. Cerebrospinal fluid should be
trauma, microorganisms may enter the subarachnoid
space through direct invasion as a result of the trauma analyzed to determine cell counts, including dif-
or, in the case of a basilar skull fracture, through a dural ferential counts, and biochemical tests for glucose
tear, which may provide an avenue for invasion of the and protein, as well as Gram’s staining, should
central nervous system by bacteria located in the audi- be performed. One study that compared Gram’s
tory canal, nose, or nasopharynx (Panel D). Bacteria
staining with cerebrospinal fluid cultures for the
may also be introduced by lumbar puncture (Panel E).
diagnosis of bacterial meningitis showed that
Gram’s staining had a high specificity but a low
features,3,4,11,14-16 although they are nonspecific sensitivity.19
and difficult to recognize in patients who are se- Cell counts in cerebrospinal fluid may be help-
dated, who have just undergone neurosurgery, or ful but have low sensitivity and specificity in clini-
who have an underlying disease that may mask the cal subgroups of patients.17,19 In a prospective
symptoms.18 Infections associated with cerebro- study involving 172 patients with external ventricu-
spinal fluid shunts may cause nonspecific symp- lar catheters, cell counts in cerebrospinal fluid
toms such as low-grade fever or general malaise3; were normal in 4 of 18 patients in whom menin-
signs of meningeal irritation are seen in less than gitis was confirmed by culture (22%)17; a similar
50% of patients. Symptoms and signs of infection proportion of patients without positive cultures
may also be associated with the distal portion of had pleocytosis. The interpretation of the numbers
the shunt (i.e., peritonitis or bacteremia). of white cells in cerebrospinal fluid is especially
The diagnostic workup consists of neuroim- problematic in patients who have meningitis that
aging, cerebrospinal fluid analysis (cell counts, develops after intraventricular hemorrhage; al-
Gram’s staining, biochemical tests for glucose and though a formula has been proposed for interpre-
protein, and cultures), and cultures of blood. Neu- tation,20 the diagnostic accuracy is unknown.21
roimaging is indicated in most patients with sus- Among patients assessed for postoperative men-
pected nosocomial bacterial meningitis, since it ingitis, aseptic meningitis as a result of the local
allows for an evaluation of ventricular size and inflammatory reaction to blood breakdown prod-
provides information on whether there is a mal- ucts may account for up to 70% of cases.22
function of the shunt or whether potentially con- Additional tests to establish the diagnosis of
taminated catheters retained from previous surgi- bacterial meningitis have been evaluated. In pa-
cal procedures are present. Multislice computed tients who had undergone neurosurgery, a lactate
tomographic (CT) scanners with multiplanar re- concentration of 4 mmol per liter or more in the
formatting capabilities may be helpful in local- cerebrospinal fluid was shown to have a sensitiv-
izing leaks of cerebrospinal fluid (Fig. 2). Neu- ity of 88%, a specificity of 98%, a positive predic-
roimaging may also show expanding masses (i.e., tive value of 96%, and a negative predictive value
hemorrhage, subdural empyema, or hydrocepha- of 94% for the diagnosis of bacterial meningitis.23
lus) and brain shift, which should be identified However, a retrospective review of cases of bac-
n engl j med 362;2 nejm.org january 14, 2010 149
The New England Journal of Medicine
Downloaded from nejm.org by SERVICIO MEDICINA INTERNA TESAI on February 9, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 1. Neurosurgical Techniques to Minimize the Risk of Postoperative evaluated for their effectiveness in detecting the
Meningitis. presence of bacterial DNA in cerebrospinal fluid
from patients with ventricular catheters. In one
Before surgery
study that used PCR to detect gram-positive bac-
Wash scalp hair, remove dirt or debris, and cover open wounds with a clean teria in 86 specimens, 42 were negative as assessed
dressing
by culture but positive as assessed by PCR; there
Clip, but do not shave, hair
were no positive culture results in patients with
Use chlorhexidine or an iodine-based skin preparation
negative PCR results, suggesting that a negative
Drape the surgical site with adhesive drapes and transparent adhesive film to
prevent implantable hardware from coming in contact with exposed skin PCR result is predictive of the absence of infec-
Maintain sterile field with careful aseptic techniques tion.25 More studies are needed, however, before
Administer prophylactic antibiotics to achieve adequate tissue concentrations routine use of PCR assays is recommended for the
before incision diagnosis of bacterial meningitis, especially be-
During surgery cause contaminating bacteria may lead to false
Minimize blood loss and tissue trauma; avoid hypothermia unless it is delib- positive results.
erately induced
Remove devitalized and grossly contaminated tissue and small bone frag-
ments A n t imicrobi a l Ther a py
Use a double layer of gloves when handling implantable devices
The choice of empirical antimicrobial therapy for
Irrigate the operative field with warmed sterile physiologic solution
nosocomial bacterial meningitis depends on the
Perform careful hemostasis to avoid postoperative wound hematomas
pathogenesis of the infection (Table 2). The ther-
Position the cerebrospinal fluid drainage devices carefully to maintain a contin-
uous flow of cerebrospinal fluid; ensure that the exit site is fashioned so apy for patients in whom meningitis develops af-
that there is no leakage around the cerebrospinal fluid drain; ensure that ter neurosurgery or for patients who are hospital-
the catheter is tunneled from the insertion site and secured to the skin so ized for a prolonged period after penetrating head
that it cannot be dislodged and that it is connected securely to a sterile
drainage system; sample the cerebrospinal fluid under sterile conditions trauma or basilar skull fracture should consist of
Close the skin carefully, with wound edges secured to prevent leakage of vancomycin in combination with cefepime, cef-
cerebrospinal fluid but with good skin perfusion; avoid passing hardware tazidime, or meropenem26; the choice of the sec-
directly beneath the incision
ond agent should be based on the antimicrobial-
After surgery
susceptibility profiles of the local gram-negative
Use percutaneous drains to collect postoperative hemorrhage; ensure that
the drains are tunneled so that they will not leak and secured so that they
bacilli. Meropenem is the agent of choice if one
cannot be dislodged of the carbapenems is used, given the lower risk
Apply a barrier dressing where necessary, particularly to prevent the patient of seizure with meropenem than with imipenem,
from inadvertently opening the wound and given the clinical studies that have shown its
Avoid putting pressure on the wound in the postoperative period; take mea- usefulness in the treatment of bacterial meningi-
sures to prevent pressure sores in other areas
tis.26 Empirical therapy after basilar skull fracture
or early after otorhinologic surgery should con-
sist of vancomycin plus a third-generation cepha-
terial meningitis associated with a cerebrospinal losporin (either cefotaxime or ceftriaxone).11,13,14
fluid shunt showed that with the use of that Once a specific pathogen has been isolated, anti-
cutoff value for lactate, almost half of the infec- microbial therapy can be modified for optimal
tions would have been missed.3 Concentrations management.
of C-reactive protein in serum or cerebrospinal Concerns have been raised regarding the ad-
fluid, and serum concentrations of procalcitonin, equacy of the penetration of vancomycin into the
have been evaluated for their usefulness in deter- cerebrospinal fluid in patients with nosocomial
mining the diagnosis24; although elevated con- meningitis, as well as the potential for side effects
centrations are suggestive of bacterial infection, when the elimination of vancomycin is hampered
they do not establish the diagnosis, and further in patients with multiorgan system dysfunction.27
studies are needed to determine the usefulness of Linezolid and daptomycin have been shown to
these markers in the diagnosis of nosocomial bac- have efficacy in some cases of staphylococcal men-
terial meningitis. ingitis28,29; linezolid has also been shown to have
Nucleic acid–amplification tests, such as poly- favorable pharmacokinetic characteristics (i.e., ce-
merase-chain-reaction (PCR) assays, have been rebrospinal fluid penetration of approximately
150 n engl j med 362;2 nejm.org january 14, 2010
The New England Journal of Medicine
Downloaded from nejm.org by SERVICIO MEDICINA INTERNA TESAI on February 9, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
current concepts
treatment should be withdrawn after 72 hours if
A the results of cerebrospinal fluid cultures are
negative.31 When this recommendation was eval-
uated in a prospective study, complications were
shown to be rare after treatment was withdrawn,
if Gram’s staining of cerebrospinal fluid and ce-
rebrospinal fluid cultures were negative for bac-
terial meningitis after 72 hours.22 However, the
therapeutic approach to nosocomial bacterial men-
ingitis must be individualized, and some patients,
especially those who have received previous or
concurrent antimicrobial therapy, may require
treatment with an appropriate antimicrobial agent
despite negative culture results.
Direct infusion of antimicrobial agents into the
ventricles through a catheter is occasionally nec-
B essary, when infections that develop after neuro-
surgical procedures or in association with cerebro-
spinal fluid catheters are difficult to eradicate with
parenteral antimicrobial therapy alone.26,27,32-34
However, no antimicrobial agent has been ap-
proved by the Food and Drug Administration for
intraventricular use, and the indications for this
mode of administration are not well defined.
Vancomycin and gentamicin are the antimicro-
bial agents that have been used most often.27,31-34
Dosages have been determined empirically (Ta-
ble 3), with adjustments made on the basis of the
concentration of the agent in the cerebrospinal
fluid. The drain is usually closed for 1 hour after
the administration of the first intraventricular
Figure 2. Cranial CT Scans in a 51-Year-Old Woman dose. Subsequent doses can be determined by
with Pneumococcal Meningitis 1 Week after Nasal measuring the trough concentration in a sample
Septum Surgery. of cerebrospinal fluid obtained immediately before
ICM AUTHOR van de Beek RETAKE 1st
The scan in Panel A shows bilateral subdural air col2nd
REG F FIGURE 2a&b
the infusion of the next dose. The trough con-
lections, a finding referred to as “Mount Fuji sign.” 3rd centration divided by the minimal inhibitory con-
CASE
The scan inTITLE
Panel B shows a bony defect of Revised
the lamina
cribrosa on the Line
right (arrow). 4-C
The patient underwent
centration of the agent for the isolated bacterial
SIZE
Enon ARTIST: mst
neurosurgical defect. H/T
closure of theH/T 16p6
pathogen should generally exceed 10 to 20 for
FILL Combo
consistent sterilization of the cerebrospinal fluid.
AUTHOR, PLEASE NOTE:
Figure has been redrawn and type has been reset. Although this procedure is not standardized, it is
Please check carefully. a reasonable approach to adopt when agents whose
80% at steady state) in neurosurgical patients in concentrations can be routinely measured are
JOB: 36202 ISSUE: 1-14-09
critical care units.30 However, vancomycin is rec- used. At some centers, peak and trough antimi-
ommended as the first-line therapy and is admin- crobial concentrations in cerebrospinal fluid are
istered at dosages aimed at achieving a serum monitored by the placement of a separate ventricu-
trough concentration of 15 to 20 μg per millili- lar access device,36 although it is unclear whether
ter.26 Alternative agents may be used in patients the peak level that is reached above the minimal
in whom an adequate response is not seen. inhibitory concentration or the length of time that
The British Society for Antimicrobial Chemo- the level remains above the minimal inhibitory
therapy recommends empirical therapy for all pa- concentration is a better predictor of the out-
tients who have signs of postoperative meningitis; come.33
n engl j med 362;2 nejm.org january 14, 2010 151
The New England Journal of Medicine
Downloaded from nejm.org by SERVICIO MEDICINA INTERNA TESAI on February 9, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 2. Recommended Empirical Antimicrobial Therapy for Nosocomial Bacterial Meningitis, According to the Pathogenesis
of the Infection.
Pathogenesis Common Bacterial Pathogens Antimicrobial Therapy*
Postneurosurgical infection Facultative and aerobic gram-negative bacilli (includ- Vancomycin plus cefepime, ceftazidime, or mero-
ing Pseudomonas aeruginosa), Staphylococcus penem†
aureus, and coagulase-negative staphylococci
(especially S. epidermidis)
Ventricular or lumbar catheter Coagulase-negative staphylococci (especially S. epi- Vancomycin plus cefepime, ceftazidime, or mero-
dermidis), S. aureus, facultative and aerobic gram- penem†
negative bacilli (including P. aeruginosa),
Propionibacterium acnes
Penetrating trauma S. aureus, coagulase-negative staphylococci (espe- Vancomycin plus cefepime, ceftazidime, or mero-
cially S. epidermidis), facultative and aerobic penem†
gram-negative bacilli (including P. aeruginosa)
Basilar skull fracture Streptococcus pneumoniae, Haemophilus influenzae, Vancomycin plus a third-generation cephalosporin
group A β-hemolytic streptococci (i.e., ceftriaxone or cefotaxime)
* The preferred daily dosages of antimicrobial agents in adults with normal renal and hepatic function are as follows: vancomycin, 15 mg per
kilogram of body weight every 8 to 12 hours to maintain a serum vancomycin trough concentration of 15 to 20 µg per milliliter; cefepime,
2 g every 8 hours; ceftazidime, 2 g every 8 hours; meropenem, 2 g every 8 hours; ceftriaxone, 2 g every 12 hours; and cefotaxime, 2 g every
4 to 6 hours. For patients with severe allergy to penicillin or cephalosporins, aztreonam, 2 g every 6 to 8 hours, or ciprofloxacin, 400 mg ev-
ery 8 to 12 hours, can be used for treatment of infection caused by gram-negative bacilli.
† The choice of the specific agent should be based on local antimicrobial susceptibility of aerobic gram-negative bacilli.
ly or by the intraventricular or intrathecal route,
Mult idrug -R e sis ta n t
Gr a m-Neg at i v e B acil l i cerebrospinal fluid sterilization was achieved in
all cases, and 13 patients were cured.38 In a retro-
Given the emergence of multidrug-resistant gram- spective review of 51 cases of acinetobacter men-
negative bacilli, the approach to antimicrobial ther- ingitis, all 8 patients who were treated with in-
apy in patients with nosocomial meningitis that travenous and intrathecal colistin survived.35
is caused by these pathogens has become prob-
lematic.37 In particular, acinetobacter species have R emova l of C athe ter s
become more common in patients with nosoco-
mial meningitis,34 and these bacteria are frequently If bacterial meningitis develops in a patient who
resistant to third-generation and fourth-genera- has an external ventricular catheter, the catheter
tion cephalosporins; resistance to carbapenems should be removed to increase the likelihood that
has also been reported. Therefore, adequate con- the infection can be cured. In the case of internal
centrations of these agents in the cerebrospinal ventricular catheters, antimicrobial therapy, re-
fluid may not be achieved after parenteral admin- moval of all components of the infected catheter,
istration. For empirical treatment of acinetobacter and placement of an external drain appear to be
meningitis, intravenous meropenem, with or with- the most effective treatment, with success in more
out an aminoglycoside administered by the intra- than 85% of patients; external drainage leads to
ventricular or intrathecal route, has been recom- more rapid resolution of the ventriculitis, allows
mended34; if the organism is subsequently found monitoring of cerebrospinal fluid findings and
to be resistant to carbapenems, colistin (usually cultures, and allows continued treatment of the
formulated as colistimethate sodium) or polymyx- underlying hydrocephalus. The optimal timing for
in B should be substituted for meropenem and reimplantation of the shunt is not clearly defined,
may also need to be administered by the intraven- although general guidelines can be suggested. In
tricular or intrathecal route.37 In a review of 14 patients with shunt infections that are caused by
patients with multidrug-resistant Acinetobacter bau- a coagulase-negative staphylococcus or P. acnes in
mannii meningitis or ventriculitis who were treat- association with abnormalities of the cerebrospi-
ed with colistin administered either intravenous- nal fluid (e.g., pleocytosis), antimicrobial therapy
152 n engl j med 362;2 nejm.org january 14, 2010
The New England Journal of Medicine
Downloaded from nejm.org by SERVICIO MEDICINA INTERNA TESAI on February 9, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
current concepts
for 7 days is commonly recommended before
Table 3. Recommended Doses of Selected Antimicrobial Agents Administered
placement of a new shunt; if repeat cultures are by the Intraventricular Route.*
positive, antimicrobial therapy should generally be
continued until cerebrospinal fluid cultures have Antimicrobial Agent Daily Intraventricular Dose
been negative for 10 consecutive days before a new Vancomycin 5–20 mg†
shunt is placed. In the case of shunt infections Gentamicin 1–2 mg in infants and children; 4–8 mg in adults
caused by Staphylococcus aureus or gram-negative Amikacin 5–50 mg‡
bacilli, 10 days of antimicrobial therapy after re-
Polymyxin B 2 mg in infants and children; 5 mg in adults
peated negative cultures are recommended before
placement of a new shunt, although some author- Colistin, usually formulated 10 mg once daily or 5 mg every 12 hr§
as colistimethate sodium
ities recommend an even longer duration of ther-
apy when gram-negative bacilli are isolated. Some * There are no data that define the exact dose of an antimicrobial agent that may
experts have recommended a 3-day observation be administered by the intraventricular route, but the dose can be estimated
period after the completion of antimicrobial ther- through the measurement of the cerebrospinal fluid trough concentration, in
the case of agents for which these measurements can be obtained. Medica
apy before a new shunt is placed to confirm that tions administered by the intraventricular route should be preservative-free.
the infection has been cleared, although this is † Most studies have used a 10-mg or 20-mg dose.
not uniformly recommended. ‡ The usual daily dose is 30 mg.
§ In one study, patients received 10 mg every 12 hours without an increase in
Removal of the catheter hardware, followed by side effects.35
immediate replacement and intravenous antimi-
crobial therapy, cures approximately 65% of pa-
tients with catheter-related infections.39 Conserva- F u t ur e Dir ec t ions
tive management (i.e., leaving the internal catheter
in place and administering intravenous or intra- The prevention and management of nosocomial
ventricular antimicrobial therapy) has generally bacterial meningitis pose a substantial challenge,
been associated with a low success rate (approxi- especially with the emergence of disease caused
mately 35%)39,40 but has been successfully used by multidrug-resistant pathogens. Protocols must
in selected patients with infections from cerebro- be developed to standardize surgical techniques
spinal fluid catheters that were caused by less in order to minimize the risk of infection. Clini-
virulent microorganisms such as coagulase-neg- cal trials of simple interventions, such as chang-
ative staphylococci. In an observational study of ing the outer pairs of gloves before handling the
43 patients, 84% were cured with systemic and catheter material during surgery, should be initi-
intraventricular antimicrobial agents (infused ated. Early recognition and aggressive treatment
through a separate ventricular access device), with may improve the outcome for patients with noso-
a 92% success rate in the case of infections caused comial bacterial meningitis.
by bacteria other than S. aureus.35 Regardless of the Supported by grants from the Netherlands Organization for
manner of treatment, infections from cerebro- Health Research and Development (NWO-Veni grant 2006
[916.76.023]) and the Academic Medical Center (AMC Fellow-
spinal fluid shunts can recur. In one study, the ship 2008), both to Dr. van de Beek.
recurrence rate was 26%, with two thirds of the No potential conflict of interest relevant to this article was
cases caused by the same microorganism.41 reported.
References
1. Korinek AM, Baugnon T, Golmard JL, and treatment outcome of cerebrospinal 6. Tulipan N, Cleves MA. Effect of an in-
van Effenterre R, Coriat P, Puybasset L. fluid shunt-associated infections in adults: traoperative double-gloving strategy on the
Risk factors for adult nosocomial menin- a retrospective analysis over an 11-year incidence of cerebrospinal fluid shunt in-
gitis after craniotomy: role of antibiotic period. Clin Infect Dis 2008;47:73-82. fection. J Neurosurg 2006;104:Suppl:S5-S8.
prophylaxis. Neurosurgery 2006;59:126-33. 4. Vinchon M, Dhellemmes P. Cerebro- 7. Sørensen P, Ejlertsen T, Aaen D, Poul
2. McClelland S III, Hall WA. Postopera- spinal fluid shunt infection: risk factors sen K. Bacterial contamination of sur-
tive central nervous system infection: in- and long-term follow-up. Childs Nerv Syst geons gloves during shunt insertion: a pilot
cidence and associated factors in 2111 2006;22:692-7. study. Br J Neurosurg 2008;22:675-7.
neurosurgical procedures. Clin Infect Dis 5. Kulkarni AV, Drake JM, Lamberti- 8. Lozier AP, Sciacca RR, Romagnoli
2007;45:55-9. Pasculli M. Cerebrospinal fluid shunt in- MF, Connolly ES Jr. Ventriculostomy-relat-
3. Conen A, Walti LN, Merlo A, Fluckiger fection: a prospective study of risk fac- ed infections: a critical review of the lit-
U, Battegay M, Trampuz A. Characteristics tors. J Neurosurg 2001;94:195-201. erature. Neurosurgery 2008;62:688-700.
n engl j med 362;2 nejm.org january 14, 2010 153
The New England Journal of Medicine
Downloaded from nejm.org by SERVICIO MEDICINA INTERNA TESAI on February 9, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
current concepts
9. Wong GK, Poon WS, Wai S, Yu LM, meningitis in neurocritical care patients. neurointensive care patients with staphy-
Lyon D, Lam JM. Failure of regular exter- J Neurol 2008;255:1617-24. lococcal ventriculitis associated with ex-
nal ventricular drain exchange to reduce 21. Pfausler B, Beer R, Engelhardt K, ternal ventricular drains. Antimicrob
cerebrospinal fluid infection: result of a Kemmler G, Mohsenipour I, Schmutzhard Agents Chemother 2007;51:379-82.
randomised controlled trial. J Neurol Neu- E. Cell index — a new parameter for the 31. The management of neurosurgical
rosurg Psychiatry 2002;73:759-61. early diagnosis of ventriculostomy (exter- patients with postoperative bacterial or
10. Governale LS, Fein N, Logsdon J, nal ventricular drainage)-related ventricu- aseptic meningitis or external ventricular
Black PM. Techniques and complications litis in patients with intraventricular drain-associated ventriculitis. Br J Neuro-
of external lumbar drainage for normal hemorrhage? Acta Neurochir (Wien) surg 2000;14:7-12.
pressure hydrocephalus. Neurosurgery 2004;146:477-81. 32. Wen DY, Bottini AG, Hall WA, Haines
2008;63:Suppl 2:379-84. 22. Zarrouk V, Vassor I, Bert F, et al. Eval- SJ. The intraventricular use of antibiotics.
11. Baltas I, Tsoulfa S, Sakellariou P, Vo- uation of the management of postopera- Neurosurg Clin N Am 1992;3:343-54.
gas V, Fylaktakis M, Kondodimou A. Post- tive aseptic meningitis. Clin Infect Dis 33. Ziai WC, Lewin JJ III. Improving the
traumatic meningitis: bacteriology, hy- 2007;44:1555-9. role of intraventricular antimicrobial
drocephalus, and outcome. Neurosurgery 23. Leib SL, Boscacci R, Gratzl O, Zim- agents in the management of meningitis.
1994;35:422-6. merli W. Predictive value of cerebrospinal Curr Opin Neurol 2009;22:277-82.
12. Bullock MR, Chesnut R, Ghajar J, et fluid (CSF) lactate level versus CSF/blood 34. Kim BN, Peleg AY, Lodise TP, et al.
al. Surgical management of depressed glucose ratio for the diagnosis of bacterial Management of meningitis due to antibi-
cranial fractures. Neurosurgery 2006;58: meningitis following neurosurgery. Clin otic-resistant Acinetobacter species. Lan-
Suppl:S56-S60. Infect Dis 1999;29:69-74. cet Infect Dis 2009;9:245-55.
13. Choi D, Spann R. Traumatic cerebro- 24. Nathan BR, Scheld WM. The potential 35. Rodríguez Guardado A, Blanco A,
spinal fluid leakage: risk factors and the roles of C-reactive protein and procalci- Asensi V, et al. Multidrug-resistant Acine-
use of prophylactic antibiotics. Br J Neu- tonin in the serum and cerebrospinal fluid tobacter meningitis in neurosurgical pa-
rosurg 1996;10:571-5. in the diagnosis of bacterial meningitis. tients with intraventricular catheters:
14. Adriani KS, van de Beek D, Brouwer Curr Clin Top Infect Dis 2002;22:155-65. assessment of different treatments. J An-
MC, Spanjaard L, de Gans J. Community- 25. Banks JT, Bharara S, Tubbs RS, et al. timicrob Chemother 2008;61:908-13.
acquired recurrent bacterial meningitis in Polymerase chain reaction for the rapid 36. Brown EM, Edwards RJ, Pople IK.
adults. Clin Infect Dis 2007;45:e46-e51. detection of cerebrospinal fluid shunt or Conservative management of patients
15. Baer ET. Post-dural puncture bacterial ventriculostomy infections. Neurosurgery with cerebrospinal shunt infections. Neu-
meningitis. Anesthesiology 2006;105:381- 2005;57:1237-43. rosurgery 2006;58:657-65.
93. 26. Tunkel AR, Hartman BJ, Kaplan SL, et 37. Falagas ME, Bliziotis IA, Tam VH. In-
16. Weisfelt M, van de Beek D, Spanjaard al. Practice guidelines for the manage- traventricular or intrathecal use of poly-
L, de Gans J. Nosocomial bacterial men- ment of bacterial meningitis. Clin Infect myxins in patients with gram-negative
ingitis in adults: a prospective series of 50 Dis 2004;39:1267-84. meningitis: a systematic review of the
cases. J Hosp Infect 2007;66:71-8. 27. Pfausler B, Spiss H, Beer R, et al. available evidence. Int J Antimicrob Agents
17. Mayhall CG, Archer NH, Lamb VA, et Treatment of staphylococcal ventriculitis 2007;29:9-25.
al. Ventriculostomy-related infections: associated with external cerebrospinal fluid 38. Katragkou A, Roilides E. Successful
a prospective epidemiologic study. N Engl drains: a prospective randomized trial of treatment of multidrug-resistant Acineto-
J Med 1984;310:553-9. intravenous compared with intraventricu- bacter baumannii central nervous system
18. Muttaiyah S, Ritchie S, Upton A, Rob- lar vancomycin therapy. J Neurosurg 2003; infections with colistin. J Clin Microbiol
erts S. Clinical parameters do not predict 98:1040-4. 2005;43:4916-7.
infection in patients with external ven- 28. Kessler AT, Kourtis AP. Treatment of 39. Schreffler RT, Schreffler AJ, Wittler
tricular drains: a retrospective observa- meningitis caused by methicillin-resistant RR. Treatment of cerebrospinal fluid shunt
tional study of daily cerebrospinal fluid Staphylococcus aureus with linezolid. In- infections: a decision analysis. Pediatr In-
analysis. J Med Microbiol 2008;57:207-9. fection 2007;35:271-4. fect Dis J 2002;21:632-6.
19. Schade RP, Schinkel J, Roelandse FW, 29. Lee DH, Palermo B, Chowdhury M. Suc- 40. Yogev R. Cerebrospinal fluid shunt
et al. Lack of value of routine analysis of cessful treatment of methicillin-resistant infections: a personal view. Pediatr Infect
cerebrospinal fluid for prediction and di- Staphylococcus aureus meningitis with Dis 1985;4:113-8.
agnosis of external drainage-related bac- daptomycin. Clin Infect Dis 2008;47:588- 41. Kestle JRW, Garton HJL, Whitehead
terial meningitis. J Neurosurg 2006;104: 90. WE, et al. Management of shunt infec-
101-8. 30. Beer R, Engelhardt KW, Pfausler B, et tions: a multicenter pilot study. J Neuro-
20. Beer R, Lackner P, Pfausler B, Schmut- al. Pharmacokinetics of intravenous line- surg 2006;105:Suppl:177-81.
zhard E. Nosocomial ventriculitis and zolid in cerebrospinal fluid and plasma in Copyright 2010 Massachusetts Medical Society.
collections of articles on the journal’s web site
The Journal’s Web site (NEJM.org) sorts published articles into
more than 50 distinct clinical collections, which can be used as convenient
entry points to clinical content. In each collection, articles are cited in reverse
chronologic order, with the most recent first.
154 n engl j med 362;2 nejm.org january 14, 2010
The New England Journal of Medicine
Downloaded from nejm.org by SERVICIO MEDICINA INTERNA TESAI on February 9, 2017. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
You might also like
- Maternal Lec Semi Final.Document26 pagesMaternal Lec Semi Final.Kate Onniel RimandoNo ratings yet
- Central Nervous System Infection in The PediatricDocument5 pagesCentral Nervous System Infection in The PediatricJeriz Marie GamboaNo ratings yet
- (10920684 - Neurosurgical Focus) Intracranial Infections - Lessons Learned From 52 Surgically Treated CasesDocument8 pages(10920684 - Neurosurgical Focus) Intracranial Infections - Lessons Learned From 52 Surgically Treated CasesIsmail MuhammadNo ratings yet
- Absceso Cerebral en RN Asociado A Infeccion UmbilicalDocument5 pagesAbsceso Cerebral en RN Asociado A Infeccion UmbilicalAbrahamKatimeNo ratings yet
- Focus: Intracranial Infections: Lessons Learned From 52 Surgically Treated CasesDocument8 pagesFocus: Intracranial Infections: Lessons Learned From 52 Surgically Treated Casesjena maraNo ratings yet
- 13 Management and Prevention of Cranioplasty InfectionsDocument8 pages13 Management and Prevention of Cranioplasty InfectionsCatarine OttobeliNo ratings yet
- Brain Abscess PDFDocument28 pagesBrain Abscess PDFdoctordilafrozaNo ratings yet
- Nosocomial VentriculitisDocument8 pagesNosocomial VentriculitisCrhistian GarcíaNo ratings yet
- Treatment of Infections Associated With Surgical ImplantsDocument8 pagesTreatment of Infections Associated With Surgical ImplantsDiego Bedón AscurraNo ratings yet
- Infectious Complications After Head InjuryDocument20 pagesInfectious Complications After Head InjurySaleh DrehemNo ratings yet
- Clinical Case Reports - 2020 - Franceschi - Brain Abscess and Periodontal Pathogens Fusobacterium Nucleatum Report of ADocument6 pagesClinical Case Reports - 2020 - Franceschi - Brain Abscess and Periodontal Pathogens Fusobacterium Nucleatum Report of Awibowo gunawanNo ratings yet
- Emergency Workup in Patients With Suspected Acute Bacterial MeningitisDocument7 pagesEmergency Workup in Patients With Suspected Acute Bacterial MeningitisLIla SierraNo ratings yet
- Management of Post-Operative Endophthalmitis: A ReviewDocument8 pagesManagement of Post-Operative Endophthalmitis: A ReviewIJAR JOURNALNo ratings yet
- Ejm 17 1 40 45Document6 pagesEjm 17 1 40 45Ujean Santos SagaralNo ratings yet
- Do Brain Abscesses Have A Higher Incidence of Odontogenic Origin Than Previously Thought?Document7 pagesDo Brain Abscesses Have A Higher Incidence of Odontogenic Origin Than Previously Thought?Haytham JamilNo ratings yet
- Medicina 58 01758Document8 pagesMedicina 58 01758charlaayasyafefiNo ratings yet
- 8 Pseudocyst of Pinna and Its Treatment With Surgical Deroofing - An Experience at Tertiary Hospitals 2013Document13 pages8 Pseudocyst of Pinna and Its Treatment With Surgical Deroofing - An Experience at Tertiary Hospitals 2013solikin ikinNo ratings yet
- Epidemiology and Risk Factors of NeurosurgicalDocument6 pagesEpidemiology and Risk Factors of NeurosurgicalNovia khasanahNo ratings yet
- Management of Infections Associated With Neurosurgical Implanted DevicesDocument17 pagesManagement of Infections Associated With Neurosurgical Implanted DevicesRaymond OiNo ratings yet
- Gerberding - 2002 - Academia and Clinic Hospital-Onset Infections A Patient Safety Issue of E VENTSDocument8 pagesGerberding - 2002 - Academia and Clinic Hospital-Onset Infections A Patient Safety Issue of E VENTSEllen Luisa PatolaNo ratings yet
- Brain Abcess Journal 2Document4 pagesBrain Abcess Journal 2ansyemomoleNo ratings yet
- Postoperative Meningitis After Spinal Surgery: A Review of 21 Cases From 20,178 PatientsDocument5 pagesPostoperative Meningitis After Spinal Surgery: A Review of 21 Cases From 20,178 PatientsntnquynhproNo ratings yet
- Brain Abcess in ChildrenDocument5 pagesBrain Abcess in Childrencamelia musaadNo ratings yet
- 1 s2.0 S0165587617302975 Main PDFDocument4 pages1 s2.0 S0165587617302975 Main PDFAchmad YunusNo ratings yet
- Infections Associated With Surgical Implants-Nejm04Document8 pagesInfections Associated With Surgical Implants-Nejm04Iulian CosteanuNo ratings yet
- Submandibular Space Infection: A Potentially Lethal InfectionDocument7 pagesSubmandibular Space Infection: A Potentially Lethal InfectionAnonymous 9KcGpvNo ratings yet
- Jurnal 3Document14 pagesJurnal 3ifranNo ratings yet
- Jurnal Medical Terminology (Hal 7-10 Belum)Document10 pagesJurnal Medical Terminology (Hal 7-10 Belum)Ajiss MahriNo ratings yet
- 1 s2.0 S1078588413007946 Main 2Document7 pages1 s2.0 S1078588413007946 Main 2Saffa AzharaaniNo ratings yet
- 15 Submandibular Space Infection A Potentially Lethal Infection PDFDocument8 pages15 Submandibular Space Infection A Potentially Lethal Infection PDFAhmad Rifqi RizalNo ratings yet
- (Methods in Molecular Medicine) Andrew J. Pollard, Martin C.J. Maiden - Meningococcal Disease (2001, Humana Press)Document662 pages(Methods in Molecular Medicine) Andrew J. Pollard, Martin C.J. Maiden - Meningococcal Disease (2001, Humana Press)gnkgbjkgjkNo ratings yet
- 001 Hipoglucemia NeonatalDocument6 pages001 Hipoglucemia NeonatalErick Lozada OlivaNo ratings yet
- Bacterial Brain AbscessDocument16 pagesBacterial Brain AbscessYunike DindaNo ratings yet
- Bi FrontalDocument8 pagesBi FrontalDian Nita Eka SaptariniNo ratings yet
- SSI Webinar Series 1 PABIDocument18 pagesSSI Webinar Series 1 PABISafira Wahyu NurhardiyantiNo ratings yet
- Trauma Bazo Art 3Document7 pagesTrauma Bazo Art 3Javi MontañoNo ratings yet
- Meningitis - StatPearls - NCBI BookshelfDocument13 pagesMeningitis - StatPearls - NCBI Bookshelfaslan tonapaNo ratings yet
- Murray A.d., Meyers A.D. Deep Neck Infections. Otolaryngology and Facial Plastic SurgeryDocument17 pagesMurray A.d., Meyers A.D. Deep Neck Infections. Otolaryngology and Facial Plastic SurgeryAndi Karwana CiptaNo ratings yet
- 2 5373127936972950922Document6 pages2 5373127936972950922teguh sNo ratings yet
- art3A10.10072Fs10096 013 2026 2Document7 pagesart3A10.10072Fs10096 013 2026 2mekonen fisehaNo ratings yet
- Prevention of Blood Flow Infections Associated With The Central Venous Catheter Systematic ReviewDocument9 pagesPrevention of Blood Flow Infections Associated With The Central Venous Catheter Systematic ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Empijem SinusaDocument4 pagesEmpijem SinusaIvan GalicNo ratings yet
- Otogenic Complications of Otitis Media Experience at Tertiary Care HospitalDocument5 pagesOtogenic Complications of Otitis Media Experience at Tertiary Care HospitalAjeng Ratna HaryantiNo ratings yet
- Current Problems in Diagnostic RadiologyDocument11 pagesCurrent Problems in Diagnostic Radiologyviena mutmainnahNo ratings yet
- Imaging of Intracranial InfectionsDocument12 pagesImaging of Intracranial Infectionsrafael rocha novaesNo ratings yet
- Prevention, Diagnosis, and Management of Acute Postoperative Bacterial EndophthalmitisDocument16 pagesPrevention, Diagnosis, and Management of Acute Postoperative Bacterial EndophthalmitisNiñoTanNo ratings yet
- Epilepsy in Tropics: Indian Perspective: Review ArticleDocument5 pagesEpilepsy in Tropics: Indian Perspective: Review ArticleBoyke SitompulNo ratings yet
- Ocular Mucormycosis May Need A Multi-Pronged Approach On A War Path - An Observational StudyDocument10 pagesOcular Mucormycosis May Need A Multi-Pronged Approach On A War Path - An Observational StudyIJAR JOURNALNo ratings yet
- EsofagoDocument6 pagesEsofagoWillie VanegasNo ratings yet
- MSD Pro DocumentDocument6 pagesMSD Pro DocumentMuhammedNo ratings yet
- Early Management and Wound Dressing Selection For Cervical Necrotizing Fasciitis: A Case ReportDocument6 pagesEarly Management and Wound Dressing Selection For Cervical Necrotizing Fasciitis: A Case ReportDeka Dharma PutraNo ratings yet
- Severe Deep Neck Space Infection and Bilateral Pneumonia of Odontogenic Origin: A Case ReportDocument3 pagesSevere Deep Neck Space Infection and Bilateral Pneumonia of Odontogenic Origin: A Case ReportAyu DamayantiNo ratings yet
- Internal Medicine Journal - 2018 - Young - Meningitis in Adults Diagnosis and ManagementDocument14 pagesInternal Medicine Journal - 2018 - Young - Meningitis in Adults Diagnosis and Managementfitri dwiyantiNo ratings yet
- Clinical Features and Diagnosis of Acute Bacterial Meningitis in AdultsDocument30 pagesClinical Features and Diagnosis of Acute Bacterial Meningitis in AdultsZarick SaenzNo ratings yet
- Tonsillectomy in Children: MedicineDocument12 pagesTonsillectomy in Children: MedicineRonald ShieldsNo ratings yet
- Bodil Sen 2018Document15 pagesBodil Sen 2018Sannita Mayusda BadiriNo ratings yet
- Bone Graft SubstitutesDocument5 pagesBone Graft SubstitutessarraNo ratings yet
- Brain Abscess: Current Management: Go ToDocument17 pagesBrain Abscess: Current Management: Go ToretnoNo ratings yet
- How Do I Manage Nocardiosis?Document9 pagesHow Do I Manage Nocardiosis?Dan JaiNo ratings yet
- Arachnoid CystDocument14 pagesArachnoid CystJaya PrabhaNo ratings yet
- 2016 Pediatric HydrocephalusDocument15 pages2016 Pediatric HydrocephalusYudit Arenita100% (1)
- Hydrocephalus PDFDocument17 pagesHydrocephalus PDFEdna López100% (1)
- Usmle Board Review Step 1Document357 pagesUsmle Board Review Step 1pereje7067% (3)
- Chapter 8 - Nervous ReviewerDocument18 pagesChapter 8 - Nervous Reviewerchristian anchetaNo ratings yet
- Day 5 - APPEC 2021 PDFDocument643 pagesDay 5 - APPEC 2021 PDFGaurieNo ratings yet
- Case Study (Undifferentiated Schizophrenia)Document12 pagesCase Study (Undifferentiated Schizophrenia)allenmariec88% (8)
- Cerebrospinal FluidDocument29 pagesCerebrospinal FluidRiyan SaputraNo ratings yet
- Anaphy NervousDocument6 pagesAnaphy NervousArcher RiegoNo ratings yet
- HydrocephalusDocument21 pagesHydrocephalusprecillathoppil100% (2)
- Approach To Head CTDocument72 pagesApproach To Head CTFatima AmirlouNo ratings yet
- Fetal BrainDocument97 pagesFetal BrainRicky AnthonyNo ratings yet
- Shunt Exposure As A Ventriculoperitoneal Shunt Complication A CaseDocument8 pagesShunt Exposure As A Ventriculoperitoneal Shunt Complication A CasePutri Tamara DasantosNo ratings yet
- Nbde Part 1 NerveDocument12 pagesNbde Part 1 NerveMrunal DoiphodeNo ratings yet
- Biology Memory MapDocument40 pagesBiology Memory MapadditpleasNo ratings yet
- Chapter 9 CSFDocument4 pagesChapter 9 CSFJhunrick Corpuz TumpalanNo ratings yet
- Neuro - PathophysiologyDocument107 pagesNeuro - Pathophysiologyjmosser100% (4)
- Unit 11 Nervous SystemDocument117 pagesUnit 11 Nervous SystemChandan Shah100% (1)
- NeuropathologyDocument88 pagesNeuropathologyminayokiNo ratings yet
- Head CT ScanDocument84 pagesHead CT ScanAbegail IbañezNo ratings yet
- Hydrocephalus: Mohd Roslee Bin Abd GhaniDocument44 pagesHydrocephalus: Mohd Roslee Bin Abd GhaniSaha DirllahNo ratings yet
- FCPS Pretest Golden File 1Document450 pagesFCPS Pretest Golden File 1Khadija AurangzebNo ratings yet
- Quiz Neuroscience Part 1 of 4Document55 pagesQuiz Neuroscience Part 1 of 4MedShare80% (5)
- Endorsement Template SURGERYDocument2 pagesEndorsement Template SURGERYElizalde HusbandNo ratings yet
- CNS Part 2 Targeted NeurosonographyDocument11 pagesCNS Part 2 Targeted NeurosonographyLeydi Laura QuirozNo ratings yet
- Yoga Jnaana PrakasikaDocument77 pagesYoga Jnaana PrakasikasevattapillaiNo ratings yet
- PDFDocument570 pagesPDFEshaal FatimaNo ratings yet
- Handbook of Practical NeurophysiotherapyDocument379 pagesHandbook of Practical NeurophysiotherapyAlbert Manimtim100% (2)
- Stage 1: Dorsal Induction: Pediatric NeuroradiologyDocument8 pagesStage 1: Dorsal Induction: Pediatric Neuroradiologysarguss14100% (1)