Professional Documents
Culture Documents
2017 - Gastrointestinal Tract As Entry Route For Hantavirus Infection - Frontiers
Uploaded by
Florin BranisteOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2017 - Gastrointestinal Tract As Entry Route For Hantavirus Infection - Frontiers
Uploaded by
Florin BranisteCopyright:
Available Formats
ORIGINAL RESEARCH
published: 08 September 2017
doi: 10.3389/fmicb.2017.01721
Gastrointestinal Tract As Entry Route
for Hantavirus Infection
Peter T. Witkowski 1*, Casey C. Perley 2 , Rebecca L. Brocato 2 , Jay W. Hooper 2 ,
Christian Jürgensen 3 , Jörg-Dieter Schulzke 4*, Detlev H. Krüger 1† and Roland Bücker 4†
1
Institute of Virology, Charité – Universitätsmedizin Berlin, Berlin, Germany, 2 Virology Division, United States Army Medical
Research Institute of Infectious Diseases, Fort Detrick, MD, United States, 3 Division of Hepatology and Gastroenterology,
Charité – Universitätsmedizin Berlin, Berlin, Germany, 4 Institute of Clinical Physiology, Charité – Universitätsmedizin Berlin,
Berlin, Germany
Background: Hantaviruses are zoonotic agents that cause hemorrhagic fevers and
are thought to be transmitted to humans by exposure to aerosolized excreta of infected
rodents. Puumala virus (PUUV) is the predominant endemic hantavirus in Europe. A large
proportion of PUUV-infected patients suffer from gastrointestinal symptoms of unclear
origin. In this study we demonstrate that PUUV infection can occur via the alimentary
tract.
Edited by:
Slobodan Paessler,
Methods: We investigated susceptibility of the human small intestinal epithelium for
University of Texas Medical Branch, PUUV infection and analyzed the resistance of virions to gastric juice. As model for
United States
intestinal virus translocation we performed infection experiments with human intestinal
Reviewed by:
Caco-2 monolayers. In animal experiments we infected Syrian hamsters with PUUV
Takaaki Koma,
Tokushima University Graduate via the intragastric route and tested seroconversion and protective immunity against
School of Medical Science, Japan subsequent Andes virus challenge.
David Safronetz,
Public Health Agency of Canada, Results: PUUV retained infectivity in gastric juice at pH >3. The virus invaded
Canada
Caco-2 monolayers in association with endosomal antigen EEA1, followed by virus
*Correspondence:
replication and loss of epithelial barrier function with basolateral virus occurrence.
Peter T. Witkowski
peter.witkowski@charite.de Cellular disturbance and depletion of the tight junction protein ZO-1 appeared after
Jörg-Dieter Schulzke prolonged infection, leading to paracellular leakage (leak flux diarrhea). Moreover, animal
joerg.schulzke@charite.de
†
experiments led to dose-dependent seroconversion and protection against lethal Andes
Shared senior authorship.
virus challenge.
Specialty section: Conclusions: We provide evidence that hantavirus can infect the organism via the
This article was submitted to
alimentary tract and suggest a novel aspect of hantavirus infection and pathogenesis.
Virology,
a section of the journal Significance: Hantaviruses are zoonotic pathogens causing severe hemorrhagic fevers
Frontiers in Microbiology
worldwide. They are transmitted to humans by small mammals. To date, these viruses
Received: 13 June 2017
Accepted: 24 August 2017
were thought to infect exclusively through the airborne route by inhalation of aerosols
Published: 08 September 2017 from infectious animal droppings or by rodent bites. In our work we could show that
Citation: the alimentary tract is an alternative path of infection for hantaviruses, meaning a
Witkowski PT, Perley CC, Brocato RL,
new association of virus and disease. These findings have impact on current textbook
Hooper JW, Jürgensen C,
Schulzke J-D, Krüger DH and knowledge and bring many implications for hantavirus epidemiology and outbreak
Bücker R (2017) Gastrointestinal Tract prevention measures.
As Entry Route for Hantavirus
Infection. Front. Microbiol. 8:1721. Keywords: hantavirus, puumala virus, hemorrhagic fever with renal syndrome, virus entry, gastrointestinal
doi: 10.3389/fmicb.2017.01721 infection, gastric barrier, tight junction, hamster model
Frontiers in Microbiology | www.frontiersin.org 1 September 2017 | Volume 8 | Article 1721
Witkowski et al. Gastrointestinal Hantavirus Infection
INTRODUCTION in vitro and in vivo studies with PUUV, the main European
hantavirus responsible for HFRS, to ascertain its viability as a
Hantaviruses are zoonotic viruses harbored by small mammals route of infection. In vitro we investigated susceptibility of the
such as, rodents, shrews, or bats. They can cause disease in human small intestinal epithelium for hantavirus infection, based
humans, leading to hemorrhagic fevers of varied severity. Old on the polarized Caco-2 cell culture system, an established model
World hantavirus infections usually lead to Hemorrhagic Fever for intestinal barrier function, and analyzed the resistance of
with Renal Syndrome (HFRS), with case fatality rates of up to virus particles to gastric juice. In vivo we demonstrated that
15%, while the clinical course of New World hantavirus infection intragastric infection of Syrian hamsters with PUUV can lead
is mainly linked with Hantavirus Cardiopulmonary Syndrome to seroconversion and protective immunity against subsequent
(HCPS) and case fatality rates of up to 50%. The symptomatology lethal hantavirus challenge.
of both manifestations is not strict and mixed clinical courses, as
well as asymptomatic infection can occur (Kruger et al., 2015).
In Europe most cases of hantavirus disease are caused by one MATERIALS AND METHODS
of two hantavirus species. Human infection with Puumala virus Virus Cultivation
(PUUV), which is harbored by the bank vole (Myodes glareolus), For in vitro studies: PUUV strain Sotkamo was grown on Vero-
typically leads to less severe disease, while individuals infected E6 cells (ATCC CRL-1586; American Type Culture Collection,
with Dobrava-Belgrade virus (DOBV), whose three genotypes Manassas, USA) under standard cell culture conditions. Viruses
Dobrava, Kurkino, and Sochi are carried by rodents of the mouse were harvested by ultracentrifugation through a sucrose cushion,
genus Apodemus, are more likely to exhibit severe symptoms in order to remove residual cell culture components and titers
(Kruger et al., 2015). Pathogenic hantaviruses are generally were determined by focus titration, as previously described
thought to enter the human body by inhalation of contaminated (Heider et al., 2001). For in vivo studies: PUUV strain K27 and
droppings from infected host animals, followed by infection of ANDV strain Chile-9717869 were grown on Vero-E6 cells in T-
the lung epithelium. Moreover, in rare cases, rodent bites were 150 flasks and collected from infected-monolayer supernatants.
reported to be the cause of infection (Vaheri et al., 2013). Cell debris were removed by low speed centrifugation at 1000×g
Hantaviruses preferentially use different β-integrins and for 10 min, and virus was twice plaque purified (Hooper et al.,
CD55/DAF for cell entry (Gavrilovskaya et al., 1999; Krautkrämer 2001). Virus stocks were aliquoted and stored at −60◦ C or colder.
and Zeier, 2008; Raftery et al., 2014). However, the presence
of some of the receptor molecules on the basolateral side of
the affected tissues requires effective disruption, or at least Virus Inactivation by Gastric Juice
penetration, of the cell barrier, as shown in vitro for different Gastric juice was taken from adult patients who underwent
tissue types (Krautkrämer et al., 2012). Interference with cellular gastroscopy for other diagnostic reasons and were not treated by
barrier function of infected tissues can lead to capillary leakage any acid suppressing medication. According to the Declaration
and is a crucial aspect of hantavirus pathogenesis (Vaheri et al., of Helsinki (Ethical Principles for Medical Research Involving
2013). As a prototypical member of the genus Orthohantavirus, Human Subjects) all patients gave written informed consent.
Hantaan virus, was shown to enter cells by clathrin-dependent The gastric juice was stored for 1–2 h in a refrigerator after its
endocytosis after receptor-mediated binding to the cell surface sampling. For each experiment the juice was taken from one
(Jin et al., 2002). patient. The initial pH-value (of approx. pH 1 on average) was
Besides the typical organ preference of hantavirus disease, measured by a pH-meter. The pH was attuned to different values
several studies have shown that the majority of patients exhibits by use of NaOH pellets. The PUUV stock was incubated with
hemorrhagic gastropathy (Nuutinen et al., 1992). Moreover, in gastric juice of different pH for given time periods of 0–15 min.
the Syrian hamster model established for South American Andes Subsequently pH was set to a value of 7 and culture medium was
virus (ANDV) intragastric inoculation can result in lethal disease, added. The treated virus solution was serially diluted and titrated
albeit with a higher 50% lethal dose (LD50 ) than the more on Vero-E6 cells.
effective intramuscular (i.m.), subcutaneous, intranasal (i.n.), and
intraperitoneal delivery routes (Hooper et al., 2008). In rare cases, Cell Culture
contact to contaminated food was named as a possible risk factor Caco-2 cells (ATCC HTB-37) were cultivated at 37◦ C with
for human hantavirus infections (Ruo et al., 1994). Moreover, 5% CO2 and maintained in minimal essential medium (MEM)
smoking was shown to be a risk factor for a PUUV infection with 10% fetal bovine serum, and 1% L-glutamine. For
in at least two studies (Van Loock et al., 1999; Vapalahti et al., immunofluorescence assays (IFA) Caco-2 cells were grown on
2010) and a possible ingestion of rodent feces or urine caused coverslips in 24-well plates. For measurement of transepithelial
by poor hand hygiene was stated in this context (Clement et al., electrical resistance (TER) the cells were seeded on permeable
2011). These findings indicate that the gut is affected in human PCF filter inserts with an area of 0.6 cm2 and a pore size of
hantavirus disease and that the infection via the alimentary tract 0.4 µm (Millipore, Germany). The cells were grown for 21
might be a possible route of infection. days for differentiation toward small intestinal properties. Cell
However, a gastrointestinal infection route for HFRS-causing medium was replaced every 2 or 3 days. TER was measured by
hantaviruses has not been explicitly proposed or excluded for an ohmmeter fitted with chopstick electrodes (EVOM, World
either humans or rodents. For this reason we conducted both Precision Instruments, USA) before infection. Confluent cell
Frontiers in Microbiology | www.frontiersin.org 2 September 2017 | Volume 8 | Article 1721
Witkowski et al. Gastrointestinal Hantavirus Infection
monolayers showing epithelial resistances above 500 ·cm2 were (aerosol, upper respiratory tract) by using a clean needle for each
used for experiments. hamster, loading the needles prior to removing hamsters from the
anesthesia chamber, and blotting the gavage needle prior to use.
Infection Experiments on Human Intestinal The ID99 for PUUV intranasal infection is a few hundred viruses
Epithelial Cells (unpublished data, Hooper lab), making infection by upper
Caco-2 cells on coverslips or filter inserts were infected for respiratory tract contamination unlikely with these precautions.
1 h at a multiplicity of infection (MOI) of 0.1–1.0. Afterwards Forty-two days post PUUV infection hamsters were challenged
remaining inoculum was washed away and the cells were i.m. (caudal thigh) with 200 PFU ANDV diluted in 0.2 mL sterile
incubated in culture medium at described conditions. TER PBS delivered with a 1 mL syringe with a 25-gauge five-eighths-
measurements in filter inserts were conducted every 24 h. inch needle. All work involving hamsters were performed in
Samples for microscopy were fixated with 4% methanol-free an animal biosafety level 4 (ABSL-4) facility. Euthanasia was
paraformaldehyde, afterwards blocked by 25 mM glycine in performed on hamsters meeting early endpoint criteria.
phosphate buffered saline (PBS). Samples for quantitative PCR In order to test if the inoculation procedure can affect the
(qPCR) were collected in AVL buffer (Qiagen, Germany) in case pH of gastric juice we administered 1 mL of PBS intragastrically
of culture medium or in RLT buffer (Qiagen) in case of cells to three hamsters, and euthanized them within 10 min of
and stored at −80◦ C. For virus titration from infection kinetics administration. The stomach contents (of both the forestomach
culture medium was stored at −80◦ C. and glandular stomach) were removed and centrifuged at high
speed to isolate the gastric juice. The pH of the gastric juice was
Quantitative RT-PCR then compared for the hamsters that had (n = 3) and had not
RNA from culture supernatants and cell lysates was extracted (n = 3) received PBS. The pH of the forestomach was essentially
according to manufacturer’s specifications by QIAamp Viral RNA unchanged (1 mL PBS intragastrically: pH 1.3 vs. untreated:
Mini Kit and RNeasy Mini Kit, respectively. Reverse transcription pH 1.5), and the pH of the stomach was similar (1 mL PBS
was performed with M-MLV reverse transcriptase (Invitrogen, intragastrically: pH 5.3 vs. untreated: pH 6.0) between the two
Germany). Virus quantification was conducted by real-time RT- groups. These data indicate that the volume of PBS used for the
PCR, as described before (Kramski et al., 2007). intragastric inoculation did not significantly affect the acidity of
either the hamster forestomach or glandular stomach.
Fluorescence Microscopy
Fluorescence staining and confocal laser-scanning microscopy N-Specific ELISA Assay
(CLSM) was performed as previously described (Bücker et al., ELISA plates (Costar, United States) were coated with
2014). The following antibodies were used: anti-ZO-1 (Zonula recombinant PUUV N-antigen in carbonate buffer (pH
occludens protein-1), anti-EEA1 (early endosomal antigen 1), 9.6) overnight at 4◦ C. Plates were blocked with PBS, 5% skim
anti-hantaviral nucleocapsid protein (1:100), Alexa-Fluor488 milk, and 0.05% Tween 20 (blocking solution) for 1 h at 37◦ C,
goat anti-mouse or -rabbit IgG, and Alexa-Fluor594 goat anti- washed once with PBS and 0.05% Tween 20 (wash solution),
mouse or -rabbit IgG (1:500; Invitrogen). Cell nuclei were stained and incubated with hamster sera (beginning with a 1:100
with 4′ -6-diamidino-2-phenylindole dihydrochloride (DAPI, dilution) diluted in blocking solution plus 2% Escherichia coli
1:1,000). lysate for 30 min at 37◦ C. Plates were washed 3 times with
wash buffer and incubated for 30 min at 37◦ C with horseradish
Epithelial Apoptosis peroxidase-conjugated goat anti-hamster IgG [Kikegaard &
Occurrence of apoptosis was visualized by TUNEL assay Perry Laboratories (KPL), USA] in blocking solution. Plates
(terminal deoxynucleotidyl transferase–mediated deoxyuridine were washed 3 times with wash buffer and incubated for 10
triphosphate nick-end labeling, In-situ Cell Death Detection Kit- min at room temperature with tetra-methylbenzidine substrate
Fluorescein, Roche, Germany) in Caco-2 monolayers 4 days post (KPL). The colorimetric reaction was stopped by adding Stop
infection as previously described (Bücker et al., 2014). Percent solution (KPL) and the absorbance at 450 nm was determined.
of apoptotic events were calculated as ratio of all cells in a The specific sum optical density (OD) was calculated by adding
low-power field (200x magnification). Six pictures per sample the background subtracted OD values, for dilutions whose
containing more than 1,300 cells each were counted for the OD was greater than the mean OD for serum samples from
analysis. negative-control wells plus 3 standard deviations. The PUUV
N-antigen was used to detect not only PUUV but also ANDV
Animal Infection Experiments N-specific antibody responses as previously reported (Hooper
Female Syrian golden hamsters, age 6–8 weeks (Envigo, et al., 2001). Hamster sera were heat inactivated before testing by
Indianapolis, USA) were anesthetized by inhalation of vaporized ELISA.
isoflurane using IMPAC 6 veterinary anesthesia machine. Once
anesthetized hamsters were challenged intragastrically with 1,000 Statistics
PFU PUUV, 10,000 PFU PUUV, or 10,000 PFU γ-irradiated Data are expressed as mean values ± standard error of the mean.
PUUV (3 × 106 rad) diluted in 1 mL sterile PBS delivered Statistical analysis was performed using 2-tailed Student t-test.
by a 3 mL syringe with a 2-inch 18 gauge gavage needle. P ≤ 0.05 was considered to be statistically significant. GraphPad
Steps were taken to mitigate non-gastric routes of exposure Prism 6 software was used for the analysis.
Frontiers in Microbiology | www.frontiersin.org 3 September 2017 | Volume 8 | Article 1721
Witkowski et al. Gastrointestinal Hantavirus Infection
Ethics Statements on their surface (data not shown). Experimental infection of
Animal Subjects human intestinal cells, Caco-2, with PUUV at MOI 0.1 revealed
This study was carried out in accordance with the a time-dependent increase of intra- and extracellular viral
recommendations of Guide for the Care and Use of Laboratory load by quantitative RT-PCR assays (Figure 2A). Titration of
Animals, National Research Council, 2011. The procedures used supernatant confirmed the increase of viable virus progeny (data
in this animal research were approved by the local animal welfare not shown). The intracellular localization of hantavirus in Caco-
body known as the USAMRIID Institutional Animal Care and 2 cells could also be visualized by CLSM between 24 and 96
Use Committee (IACUC). h post infection (p.i.). Translocation of PUUV through Caco-2
monolayers after apical infection could be shown by qRT-PCR
Human Subjects detection of viral RNA in basal culture medium. The basal release
This study was carried out in accordance with the of viruses was detectable after 24 h and it increased by 2 log10 over
recommendations of GCP guidelines, Ethics Committee of the next 216 h (Figure 2B).
the Charité, with written informed consent from all subjects. All Hantavirus antigens were found intracellularly in co-
subjects gave written informed consent in accordance with the localization with EEA1, demonstrating endosomal localization of
Declaration of Helsinki. virus particles (Figure 3). In cells infected with UV-inactivated
virus such signals were not present (data not shown).
RESULTS
Epithelial Barrier Dysfunction in Infected
Susceptibility of Hantavirus toward Gastric Caco-2 Monolayers
Juice Infection of Caco-2 monolayers at MOI 0.1 revealed stable TER
PUUV survival in the gastric lumen was tested in vitro by values up to 48 h p.i. However, after 72 h p.i. the TER decreased
incubation of virus stocks in human gastric juice of varying pH. to 60% of the initial value (Figure 4). Using CLSM, viral antigen
The antiviral activity of gastric juice was effective at low pH was observed intracellularly, in close proximity to the tight
between 1.0 and 3.0, with no virus surviving an exposure as junctions, which exhibit condensed zonula occludens protein-1
short as 1 min. PUUV did survive exposure at pH values of 4.0 (ZO-1) (Figure 5A). However, clear co-localization of PUUV N-
or 5.0 with an effective titer reduction below 1 log10 at pH 7.0 protein and ZO-1 did not occur, as evidenced by a lack of yellow
(Figure 1). signal, excluding a direct interaction. Moreover, the condensed
ZO-1 staining pattern could indicate a disturbed gate function,
Virus Replication in Caco-2 Monolayers by actomoysin-constriction-mediated tight junction protein re-
Prior to beginning experiments we confirmed that Caco-2 distribution, which could also lead to a loss of cell-cell contacts.
cells expressed ß1- and ß3-integrins as well as CD55/DAF, In CLSM analysis, cytoskeletal rearrangements were visible in
the receptors preferentially used by hantaviruses for entry, response to virus infection after 48 h (Figure 5B). Cytoskelatal F-
actin signal density increased during the course of the infection.
After 96 h p.i. condensation of actin appeared as sign of
apical membrane ruffling or actomyosin constriction of the
perijunctional cytoskeleton. Close-by the basolateral membrane
the intracellular actin formed stress fibers. To exclude the
possible induction of cell death by apoptosis Caco-2 monolayers
were stained by TUNEL 240 h p.i. at low MOI. Apoptotic
events counted in PUUV-infected monolayers did not differ
significantly from mock-infected monolayers (0.46% ± 0.10% vs.
0.42% ± 0.05%, n = 5, P = 0.73).
Infection of Caco-2 monolayers with higher concentrations
of PUUV (MOI 1.0) revealed earlier and more pronounced
effects (Figure 5C). Here, the condensation of ZO-1 was found by
48 h p.i., followed by disappearance of ZO-1 signals, and finally
cell detachment and/or cell exfoliation leading by 96 h p.i. to
epithelial leakage.
Administration of PUUV Intragastrically
FIGURE 1 | Hantavirus survival in gastric juice. Infectious dose of 106
Puumala virus particles was suspended to pure gastric juice set to pH 1–7
Leads to Productive Infection in Syrian
with NaOH for 1, 10, or 15 min. After given incubation intervals the gastric Hamsters
juice was neutralized with NaOH and the virus suspension was used to infect Groups of eight hamsters were instilled intragastrically with
VERO-E6 cells for focus titration of infectious particles (n = 4). As at low pH either 1,000 PFU PUUV or 10,000 PFU PUUV. To confirm
the inactivation activity was expected to be high pH 2 was omitted to save
valuable sample volume.
that seroconversion was caused by active viral replication, and
not input virus, a control group of eight hamsters was injected
Frontiers in Microbiology | www.frontiersin.org 4 September 2017 | Volume 8 | Article 1721
Witkowski et al. Gastrointestinal Hantavirus Infection
FIGURE 2 | (A) Growth kinetics of hantaviruses in Caco-2 cells. Caco-2 cells growing on cell culture slides were infected with Puumala virus at MOI of 0.1. Viral
replication was monitored by qPCR in culture medium and cells (n = 3). (B) Translocation of hantavirus through polarized Caco-2 monolayers. Caco-2 cells growing
on filter inserts for at least 3 weeks were infected by Puumala virus at MOI 0.1. Apical and basal medium were collected at 24, 120, and 240 h p.i. and investigated for
viral replication by qPCR (n = 3).
FIGURE 4 | Epithelial barrier dysfunction in infected Caco-2 monolayers.
Caco-2 cells growing on filter inserts were infected by Puumala virus at MOI
FIGURE 3 | Intracellular localization of hantavirus in Caco-2 cells. Confocal 0.1. Transepithelial electrical resistance (TER) was measured during infection
laser-scanning microscopy of infected cell monolayers. Caco-2 cells growing with chopstick electrodes (n = 4).
on coverslips were infected with Puumala virus at MOI of 0.1. The cells were
fixed with methanol-free formaldehyde and stained with antibodies against
PUUV nucleocapsid protein (red) and early endosomal antigen 1 (EEA1,
green). Cell nuclei were stained by DAPI (blue). PUUV administration all hamsters were challenged with 200
PFU of ANDV. 5/5 (100%) of the seroconverted hamsters
survived ANDV challenge, confirming infection. Additional
three hamsters that had been challenged with live PUUV virus
with 10,000 PFU γ-irradiated PUUV. 35 days post challenge
survived ANDV challenge, while only one hamster, who had
the hamsters were bled, and seroconversion evaluated by N- received irradiated virus intragastrically, survived. The survival
ELISA (Figure 6A). 2/8 hamsters in the 1,000 PFU challenge curves for PUUV intragastrically “vaccinated” hamsters are given
group, and 3/8 hamsters in the 10,000 PFU challenge group in Figure 6B.
seroconverted. All seroconverted hamsters had a titer of 3
log10 . None of the hamsters instilled with irradiated virus
seroconverted, confirming that viral replication occurred in DISCUSSION
seroconverted animals.
Prior infection with PUUV is able to protect animals from Stomach Physiology, Survival in the
lethal ANDV challenge, and is a more sensitive measure of Gastric Lumen
prior infection than seroconversion. To confirm that hamsters, In the human alimentary tract, entering viruses encounter gastric
which had seroconverted, were truly infected, at 42 days post acid and proteolytic enzymes with gastric contents falling below
Frontiers in Microbiology | www.frontiersin.org 5 September 2017 | Volume 8 | Article 1721
Witkowski et al. Gastrointestinal Hantavirus Infection
FIGURE 5 | (A) Tight junction disturbance. Caco-2 cells grown on filter inserts were infected with Puumala virus at MOI of 0.1 and analyzed by confocal
laser-scanning microscopy. At 48 h cells were fixed and stained for PUUV nucleocapsid protein (red) and zonula occludens protein 1 (green). Cell nuclei were stained
by DAPI (blue). (B) Cytoskeleton rearrangements in infected Caco-2 monolayers. Caco-2 cells were infected with PUUV at MOI of 0.1. At different time points the cells
were fixed with methanol-free formaldehyde and stained with antibodies against PUUV nucleocapsid protein (red) and actin (white). Cell nuclei were stained by DAPI
(blue). (C) Leaks in Caco-2 cells monolayers at high MOI. Caco-2 cells grown on coverslips were infected with Puumala virus at MOI of 1.0. At different time points the
cells were fixed and stained with antibodies against Puumala virus nucleocapsid protein (red) and zonula occludens protein 1 (green) and analyzed by confocal
laser-scanning microscopy. Mock control is shown at 96 h.
pH 4 for 70% of the time (Mitchell et al., 2001). pH values and nutritional preferences (buffer capacity of the food) leading
in human stomach can postprandially easily increase above pH to variable risk factors for hantavirus survival and therefore
5.0, even up to pH 7.0 in young children after consumption of infection through the gastrointestinal tract.
food with high buffer capacity such as, milk or milk products In our hamster infection model, the pH of gastric juice
(Mitchell et al., 2001; Bücker et al., 2012). Stomach transit time can range between pH 1.3 and pH 6.0, the viruses have
can vary between 5 min and 2 h, depending on food and liquid to overcome these stomach conditions after oral uptake,
intake (Worsøe et al., 2011). Dyspepsia, which is diagnosed in and also after experimental intragastric inoculation. Since the
up to 25% of western population, is treated with proton pump gastric pH was unchanged after inoculation (see Methods), the
inhibitors (PPIs), leading to elevated pH and higher susceptibility inoculation procedure did not contribute to a more favorable
to gastrointestinal infections (Cook, 1994). environment in the stomach lumen for virus survival. Intragastric
In our study, PUUV was shown to be able to survive human inoculation followed by a systemic infection has been previously
gastric juice for at least 15 min at pH 4.0, though viral titers were demonstrated in the hamster model of hantavirus pulmonary
reduced by 3 log10 . Exposed to gastric juice at pH 5.0 for 15 min, syndrome using Andes virus (Hooper et al., 2008). In hamsters
the reduction of virus titer amounted to 2 log10 , and at pH 7.0 less the intragastric 50% lethal dose (LD50 ) of 225 plaque forming
than a 1 log10 loss of viability was observed, suggesting the virus units (pfu) is higher than the LD50 for both intranasal (LD50 = 95
can survive long enough to be viably released into the duodenum. pfu) and intramuscular (LD50 = 8 pfu) infection, indicating that
Postprandial decrease in gastric pH can lead to reduced activity the intragastric route was the least efficient of the three (Hooper
of gastric proteolytic enzymes, like pepsin A or pepsin C, making et al., 2008). Based on our data it is likely that gastrointestinal
the environment even more conducive to viral survival. Under route of infection of animals is one possible way of virus infection
postprandial or achlorhydric conditions the antimicrobial gastric also in nature. Host animals can shed virus in saliva, urine and
barrier is vulnerable and can be overcome by pathogens (Mitchell feces (Hardestam et al., 2008). Even if studies about inter-animal
et al., 2001; Haastrup et al., 2014). Finally, stomach conditions are transmission were performed and showed a significant male
dependent on the host’s age, health status (gastric secretion rate), predominance among infected rodents as well as the importance
Frontiers in Microbiology | www.frontiersin.org 6 September 2017 | Volume 8 | Article 1721
Witkowski et al. Gastrointestinal Hantavirus Infection
FIGURE 6 | (A) Intragastral infection of hamster by Puumala virus. Syrian hamsters (animal identification numbers given on the x-axis) were infected with either 1,000
plaque forming units (PFU), 10,000 PFU or 10,000 PFU γ-irradiated PUUV. Thirty five days post infection hamsters were bled to test for seroconversion by N-ELISA.
Dots represent hamsters for which subsequent Andes virus challenge was lethal. Specific OD sum is the sum of the optical densities (ODs) greater than background,
and represents the area under the titer curve. (B) Survival curves for hamsters “vaccinated” intragastrically with Puumala virus. Forty two days post intragastric
Puumala virus challenge, the same hamsters were challenged with 200 PFU ANDV i.m.
of wounds and scarring, the role of ingestion could so far not be interactions between old world hantaviruses and DAF/CD55
ruled out as it was never an aspect of such studies, nor could it (Krautkrämer and Zeier, 2008). The data presented here,
efficiently be monitored (Calisher et al., 2007). including the proximity of viral nucleocapsid protein to tight
junctions together with ZO-1 ruffling, reinforce the idea that
Endocytotic Cell Entry PUUV uses similar mechanisms during its infection of intestinal
The small intestinal tissue, with its major absorptive function, epithelial cells.
is an entry site for pathogens including Norovirus or Yersinia
enterocolitica. The MALT (mucosa-associated lymphoid tissue) Epithelial Barrier Dysfunction
is the site for replication and dissemination for several pathogens As the result of hantavirus infection, transcytotic viral uptake
including HIV (Epple et al., 2010). In our experiments, Caco- occurs as seen in our cell culture infection model, even at
2-derived human intestinal epithelial cells are capable of being low MOIs. In cell culture experiments using higher viral
infected by PUUV. The virus localized to the endocytic pathway, concentrations, cell detachment, and severe epithelial damage
as visualized by co-localization of virus N-protein with EEA1, takes place with preceding cytoskeletal rearrangements and tight
as already shown for Hantaan virus in Vero-E6 cells (Jin et al., junction impairment. Finally, cell rounding and detachment lead
2002), while the membrane ruffling visible at later time points to significant barrier dysfunction. Loss of cells due to apoptosis
of infection could be an additional sign of high endocytic could be excluded, but cell exfoliation or shedding, as well
activity. Moreover, interactions of pathogenic viruses with tight as other cell death mechanisms like autophagy or necrosis,
junction proteins containing PDZ domains (PSD-95/Dlg/ZO-1) could play a role in the pathogenic action of hantaviruses in
or CAR (Coxsackie virus and adenovirus-receptor) have been the gut. The latter condition may more accurately resemble
frequently described (reviewed in Zihni et al., 2014) as have clinical cases of hemorrhagic fever, where a manifestation of
Frontiers in Microbiology | www.frontiersin.org 7 September 2017 | Volume 8 | Article 1721
Witkowski et al. Gastrointestinal Hantavirus Infection
hantavirus disease can compromise endothelial barrier function hamsters “intragastrically vaccinated” with PUUV that survived
leading to petechiae or even hemorrhages (Vaheri et al., 2013). ANDV challenge, without seroconverting, had PUUV antibodies
Since disturbance of epithelial barrier function in the intestine that were below our level of detection. Cross-reactivity between
leads to paracellular antigen influx (leaky gut concept Bücker ANDV and PUUV antigens makes it impossible to test for the
et al., 2014), entry of further virus particles and luminal development of PUUV antibodies post ANDV challenge. It is for
bacterial antigens is possible. This could provoke immune this reason, that survival of ANDV challenge is a more sensitive
activation and gastrointestinal symptoms like diarrhea, vomiting, measure of productive PUUV infection.
or abdominal pain, which are often found in clinical HFRS
cases. Hantavirus Route of Infection
Here, we present evidence that the oral route of infection,
Animal Model of PUUV Infection potentially by contaminated food, is plausible for PUUV. The
In the Syrian hamster model of intragastric PUUV infection results of our work imply a new aspect of hantavirus pathogenesis
we were able to confirm that the virus is capable of infecting, to be included in epidemiological considerations.
and replicating within the animal at a challenge dose of 1,000
PFU, as measured by seroconversion and protection from lethal AUTHOR CONTRIBUTIONS
ANDV challenge. Given the limited number of doses tested it is
not possible to determine a precise infectious dose that infects Conceived and designed the experiments: DK, PW, RB, JS, and
99% (ID99) of hamsters, however, given that only 3/8 hamsters JH. Performed the experiments: PW, CP, RLB, and RB. Analyzed
infected with 10,000 PFU PUUV survived ANDV challenge, the data: PW, RB, CP, RLB, and JH. Important intellectual
the ID99 must be higher than that dose. This would make support: CJ and JH. Contributed reagents/materials/analysis
the ID99 for intragastric infection at least 10-fold higher than tools: CJ, JS, JH, and DK. Wrote the paper: PW and RB. Critical
for intramuscular or intranasal (unpublished data, Hooper lab), revision and study supervision: DK and JS.
indicating that, while intragastric infection is possible, it is less
efficient than other methods used in the laboratory. FUNDING
There are two main limitations of the PUUV infection of
hamsters. First is that infection is transient, and it is difficult to This work was supported by the German Research Council
locate live virus, viral RNA, or viral antigen in the animal post (grants KR1293/13 to DK and SCHU559/11 to JS) and the
challenge. After a 1,000 PFU intranasal challenge, all animals German Federal Ministry for Education and Research in frame
seroconvert but live virus or viral RNA was not detected in the of Infect-ERA (grant 031L0096B to DK). Work at USAMRIID
sera or tissues at any time-point within the first 4 weeks of was funded by the U.S. Army Medical Research and Material
infection (unpublished data Hooper lab). For this reason we are Command, Military Infectious Disease Research Program,
unable to confirm the hypotheses regarding PUUV disruption Program Area T.
of the intestinal epithelial barrier during infection in an animal
model. However, as none of the hamsters challenged with 10,000 ACKNOWLEDGMENTS
PFU irradiated virus seroconverted, viral replication (though
unable to be detected) must have occurred as it is a requirement We are grateful to Brita Auste, Christine Spingies, and Britta
for anti-PUUV antibody production. Second, PUUV infection Jebautzke for excellent technical assistance, as well as to Walid
in hamsters with viral doses close to the ID99 leads to long Azab and Annett Petrich for their methodical support. Opinions,
seroconversion times. Animals challenged with the ID99 via interpretations, conclusions, and recommendations are those of
the i.m. or i.n. route do not seroconvert until 35 days post the authors and not necessarily endorsed by the U.S. Army or the
infection (unpublished data, Hooper lab). It is possible that the Department of Defense.
REFERENCES Cook, G. C. (1994). Hypochlorhydria and vulnerability to intestinal infection. Eur.
J. Gastroenterol. Hepatol. 6, 693–696. doi: 10.1097/00042737-199408000-00008
Bücker, R., Azevedo-Vethacke, M., Groll, C., Garten, D., Josenhans, C., Suerbaum, Epple, H. J., Allers, K., Tröger, H., Kühl, A., Erben, U., Fromm, M., et al. (2010).
S., et al. (2012). Helicobacter pylori colonization critically depends on Acute HIV infection induces mucosal infiltration with CD4+ and CD8+ T
postprandial gastric conditions. Sci. Rep. 2:994. doi: 10.1038/srep00994 cells, epithelial apoptosis, and a mucosal barrier defect. Gastroenterology 139,
Bücker, R., Schulz, E., Günzel, D., Bojarski, C., Lee, I. F., John, L. J., et al. (2014). 1289–1300. doi: 10.1053/j.gastro.2010.06.065
α-Haemolysin of Escherichia coli in IBD: a potentiator of inflammatory activity Gavrilovskaya, I. N., Brown, E. J., Ginsberg, M. H., and Mackow, E. R. (1999).
in the colon. Gut 63, 1893–1901. doi: 10.1136/gutjnl-2013-306099 Cellular entry of hantaviruses which cause hemorrhagic fever with renal
Calisher, C. H., Wagoner, K. D., Amman, B. R., Root, J. J., Douglass, R. J., Kuenzi, syndrome is mediated by beta3 integrins. J. Virol. 73, 3951–3959.
A. J., et al. (2007). Demographic factors associated with prevalence of antibody Haastrup, P., Paulsen, M. S., Begtrup, L. M., Hansen, J. M., and Jarbøl, D. E. (2014).
to Sin Nombre virus in deer mice in the western United States. J. Wildl. Dis. 43, Strategies for discontinuation of proton pump inhibitors: a systematic review.
1–11. doi: 10.7589/0090-3558-43.1.1 Fam. Pract. 31, 625–630. doi: 10.1093/fampra/cmu050
Clement, J. P., Crowcroft, N. S., Maes, P., Van Loock, F., Colson, P., Van Ranst, M., Hardestam, J., Karlsson, M., Falk, K. I., Olsson, G., Klingström, J., and Lundkvist,
et al. (2011). Smoking and other risk factors for hantavirus infections: the whole A. (2008). Puumala hantavirus excretion kinetics in bank voles (Myodes
story. Epidemiol. Infect. 139, 1284–1286. doi: 10.1017/S0950268810002244 glareolus). Emerg. Infect. Dis. 14, 1209–1215. doi: 10.3201/eid1408.080221
Frontiers in Microbiology | www.frontiersin.org 8 September 2017 | Volume 8 | Article 1721
Witkowski et al. Gastrointestinal Hantavirus Infection
Heider, H., Ziaja, B., Priemer, C., Lundkvist, A., Neyts, J., Krüger, D. H., release of neutrophil extracellular traps. J. Exp. Med. 211, 1485–1497.
et al. (2001). A chemiluminescence detection method of hantaviral antigens doi: 10.1084/jem.20131092
in neutralization assays and inhibitor studies. J. Virol. Methods 96, 17–23. Ruo, S. L., Li, Y. L., Tong, Z., Ma, Q. R., Liu, Z. L., Tang, Y. W., et al.
doi: 10.1016/S0166-0934(01)00314-7 (1994). Retrospective and prospective studies of hemorrhagic fever
Hooper, J. W., Ferro, A. M., and Wahl-Jensen, V. (2008). Immune serum produced with renal syndrome in rural China. J. Infect. Dis. 170, 527–534.
by DNA vaccination protects hamsters against lethal respiratory challenge with doi: 10.1093/infdis/170.3.527
Andes virus. J. Virol. 82, 1332–1338. doi: 10.1128/JVI.01822-07 Vaheri, A., Strandin, T., Hepojoki, J., Sironen, T., Henttonen, H., Mäkelä, S., et al.
Hooper, J. W., Larsen, T., Custer, D. M., and Schmaljohn, C. S. (2001). A (2013). Uncovering the mysteries of hantavirus infections. Nat. Rev. Microbiol.
lethal disease model for hantavirus pulmonary syndrome. Virology 289, 6–14. 11, 539–550. doi: 10.1038/nrmicro3066
doi: 10.1006/viro.2001.1133 Van Loock, F., Thomas, I., Clement, J., Ghoos, S., and Colson, P. (1999).
Jin, M., Park, J., Lee, S., Park, B., Shin, J., Song, K. J., et al. (2002). Hantaan virus A case-control study after a hantavirus infection outbreak in the south
enters cells by clathrin-dependent receptor-mediated endocytosis. Virology 294, of Belgium: who is at risk? Clin. Infect. Dis. 28, 834–839. doi: 10.1086/
60–69. doi: 10.1006/viro.2001.1303 515196
Kramski, M., Meisel, H., Klempa, B., Kruger, D. H., Pauli, G., and Nitsche, A. Vapalahti, K., Virtala, A. M., Vaheri, A., and Vapalahti, O. (2010). Case-control
(2007). Detection and typing of human pathogenic hantaviruses by real-time study on Puumala virus infection: smoking is a risk factor. Epidemiol. Infect.
reverse transcription-PCR and pyrosequencing. Clin. Chem. 53, 1899–1905. 138, 576–584. doi: 10.1017/S095026880999077X
doi: 10.1373/clinchem.2007.093245 Worsøe, J., Fynne, L., Gregersen, T., Schlageter, V., Christensen, L. A., Dahlerup,
Krautkrämer, E., Lehmann, M. J., Bollinger, V., and Zeier, M. (2012). Polar release J. F., et al. (2011). Gastric transit and small intestinal transit time and
of pathogenic Old World hantaviruses from renal tubular epithelial cells. Virol. motility assessed by a magnet tracking system. BMC Gastroenterol. 11:145.
J. 9:299. doi: 10.1186/1743-422X-9-299 doi: 10.1186/1471-230X-11-145
Krautkrämer, E., and Zeier, M. (2008). Hantavirus causing hemorrhagic fever with Zihni, C., Balda, M. S., and Matter, K. (2014). Signalling at tight junctions
renal syndrome enters from the apical surface and requires decay-accelerating during epithelial differentiation and microbial pathogenesis. J. Cell Sci. 127,
factor (DAF/CD55). J. Virol. 82, 4257–4264. doi: 10.1128/JVI.02210-07 3401–3413. doi: 10.1242/jcs.145029
Kruger, D. H., Figueiredo, L. T., Song, J. W., and Klempa, B. (2015).
Hantaviruses–globally emerging pathogens. J. Clin. Virol. 64, 128–136. Conflict of Interest Statement: The authors declare that the research was
doi: 10.1016/j.jcv.2014.08.033 conducted in the absence of any commercial or financial relationships that could
Mitchell, D. J., McClure, B. G., and Tubman, T. R. (2001). Simultaneous be construed as a potential conflict of interest.
monitoring of gastric and oesophageal pH reveals limitations of conventional
oesophageal pH monitoring in milk fed infants. Arch. Dis. Child. 84, 273–276. Copyright © 2017 Witkowski, Perley, Brocato, Hooper, Jürgensen, Schulzke, Krüger
doi: 10.1136/adc.84.3.273 and Bücker. This is an open-access article distributed under the terms of the Creative
Nuutinen, H., Vuoristo, M., Färkkilä, M., Kahri, A., Seppälä, K., Valtonen, V., Commons Attribution License (CC BY). The use, distribution or reproduction in
et al. (1992). Hemorrhagic gastropathy in epidemic nephropathy. Gastrointest. other forums is permitted, provided the original author(s) or licensor are credited
Endosc. 38, 476–480. doi: 10.1016/S0016-5107(92)70480-5 and that the original publication in this journal is cited, in accordance with accepted
Raftery, M. J., Lalwani, P., Krautkrämer, E., Peters, T., Scharffetter-Kochanek, academic practice. No use, distribution or reproduction is permitted which does not
K., Krüger, R., et al. (2014). β2 integrin mediates hantavirus-induced comply with these terms.
Frontiers in Microbiology | www.frontiersin.org 9 September 2017 | Volume 8 | Article 1721
You might also like
- 12 Brkic HelicobacterDocument6 pages12 Brkic HelicobacterHrvoje BrkićNo ratings yet
- Thannesberger 2017Document15 pagesThannesberger 2017Денис КрахоткинNo ratings yet
- The Role of Animals in Emerging Viral DiseasesFrom EverandThe Role of Animals in Emerging Viral DiseasesRating: 5 out of 5 stars5/5 (1)
- Handbook for Microbiology Practice in Oral and Maxillofacial Diagnosis: A Study Guide to Laboratory Techniques in Oral MicrobiologyFrom EverandHandbook for Microbiology Practice in Oral and Maxillofacial Diagnosis: A Study Guide to Laboratory Techniques in Oral MicrobiologyNo ratings yet
- Cat FluDocument11 pagesCat FluAsafarid AndrianiNo ratings yet
- Providencia InfectionsDocument2 pagesProvidencia InfectionsEllagEszNo ratings yet
- Models of Protection Against HIV/SIV: Models of Protection Against HIV/SIVFrom EverandModels of Protection Against HIV/SIV: Models of Protection Against HIV/SIVGianfranco PancinoNo ratings yet
- Human Pathology: Case Reports: SciencedirectDocument2 pagesHuman Pathology: Case Reports: SciencedirectIvan MaulanaNo ratings yet
- Zhang Et Al-2019-Frontiers in MicrobiologyDocument11 pagesZhang Et Al-2019-Frontiers in MicrobiologyhadeelNo ratings yet
- 2020 - Immunocytochemical and Ultrastructural Evidence Supporting That Andes Hantavirus (ANDV) Is Transmitted Person-to-Person Through The Respiratory Andor Salivary Pathways - FrontiersDocument20 pages2020 - Immunocytochemical and Ultrastructural Evidence Supporting That Andes Hantavirus (ANDV) Is Transmitted Person-to-Person Through The Respiratory Andor Salivary Pathways - FrontiersFlorin BranisteNo ratings yet
- COVID-19 LEGACY: SARS-CoV-2 clinical trials, vaccines trials and bioethicsFrom EverandCOVID-19 LEGACY: SARS-CoV-2 clinical trials, vaccines trials and bioethicsNo ratings yet
- Estomatite Vet Pathol 2011 Reis 547 57Document12 pagesEstomatite Vet Pathol 2011 Reis 547 57Roberio OlindaNo ratings yet
- BlastocystisDocument4 pagesBlastocystisParasito BioudosucNo ratings yet
- Location and Pathogenic Potenctial of Blastocystis in The Porcine IntestineDocument8 pagesLocation and Pathogenic Potenctial of Blastocystis in The Porcine Intestinesebasrd07No ratings yet
- Hep 20268Document7 pagesHep 20268ewNo ratings yet
- Wolfram, 2013 PDFDocument25 pagesWolfram, 2013 PDFmangiemrNo ratings yet
- Aedes Aegypti Wolbachia: Limited Dengue Virus Replication in Field-Collected Mosquitoes Infected WithDocument10 pagesAedes Aegypti Wolbachia: Limited Dengue Virus Replication in Field-Collected Mosquitoes Infected WithRama BiomantaraNo ratings yet
- Gastroenteritis in Childhood A Retrospective StudyDocument8 pagesGastroenteritis in Childhood A Retrospective StudyTiara Sekar AyudhipashaNo ratings yet
- Typhoid Fever: Disease PrimersDocument18 pagesTyphoid Fever: Disease PrimersErick HernandezNo ratings yet
- Jpids Pis043 FullDocument3 pagesJpids Pis043 FullRani Eva DewiNo ratings yet
- CatfluDocument13 pagesCatflumvdaniela.santanaNo ratings yet
- Molecular DiagnosisDocument6 pagesMolecular DiagnosisLe Minh DuyNo ratings yet
- Orthohantavirus Pathogenesis and Cell TropismDocument14 pagesOrthohantavirus Pathogenesis and Cell TropismJesus Barraza SánchezNo ratings yet
- Microbial Diseases of The Respiratory System: Pertussis (Whooping Cough) PathogenesisDocument15 pagesMicrobial Diseases of The Respiratory System: Pertussis (Whooping Cough) PathogenesisCharlene SibugNo ratings yet
- Pertussis Detection in Children With Cough of Any Duration: Researcharticle Open AccessDocument9 pagesPertussis Detection in Children With Cough of Any Duration: Researcharticle Open AccessLee제노No ratings yet
- Disentri AmubaDocument8 pagesDisentri AmubaVivi DeviyanaNo ratings yet
- A Review of Plague Persistence With Special Emphasis On FleasDocument15 pagesA Review of Plague Persistence With Special Emphasis On FleasJuan Carlos Colina VenegasNo ratings yet
- 1 s2.0 S0195561619301652 MainDocument19 pages1 s2.0 S0195561619301652 MainLuan MachadoNo ratings yet
- Literatur 2 WolbachiaDocument19 pagesLiteratur 2 Wolbachialidya sianturiNo ratings yet
- Feeding Cyprinus Carpio With Infectious Materials Mediates Cyprinid Herpesvirus 3 Entry Through Infection of Pharyngeal Periodontal MucosaDocument10 pagesFeeding Cyprinus Carpio With Infectious Materials Mediates Cyprinid Herpesvirus 3 Entry Through Infection of Pharyngeal Periodontal MucosaKarina RuizNo ratings yet
- Pathobiology of Cell Wall and Cell Signal Transduction: Pneumocystis Pneumonia: Life CycleDocument12 pagesPathobiology of Cell Wall and Cell Signal Transduction: Pneumocystis Pneumonia: Life CycleVanessa YanzaguanoNo ratings yet
- 4019.NEJM, gastroentDocument11 pages4019.NEJM, gastroentbrian.p.lucasNo ratings yet
- Sanitation and Water Treatment Lower Intestinal Protozoa RiskDocument13 pagesSanitation and Water Treatment Lower Intestinal Protozoa RiskWiwien HendrawanNo ratings yet
- Journal Pone 0249341Document12 pagesJournal Pone 0249341harrisart04No ratings yet
- Insect Pathology V1: An Advanced TreatiseFrom EverandInsect Pathology V1: An Advanced TreatiseEdward SteinhausNo ratings yet
- Virus Survival in The Environment: E.C. Pirtleandg.W. BeranDocument16 pagesVirus Survival in The Environment: E.C. Pirtleandg.W. BeranSoul LyricsNo ratings yet
- Biological and Chemical Hazards of Forensic Skeletal AnalysisDocument9 pagesBiological and Chemical Hazards of Forensic Skeletal AnalysisOskar GomezNo ratings yet
- Pathophysiology of Campylobacter Jejuni Infections of Humans 1999 Microbes and InfectionDocument11 pagesPathophysiology of Campylobacter Jejuni Infections of Humans 1999 Microbes and InfectionFrancisco GonzálezNo ratings yet
- Case Report Pasteurella Multocida Septicemia in A Patient With CirrhosisDocument4 pagesCase Report Pasteurella Multocida Septicemia in A Patient With CirrhosisSilviyah MujionoNo ratings yet
- Common and Emerging InfectiousDocument14 pagesCommon and Emerging InfectiousRachel AutranNo ratings yet
- Aspergilus 2015 CFDocument8 pagesAspergilus 2015 CFLudmila BalanetchiNo ratings yet
- A New Coronavirus Associated With Human Respiratory Disease in ChinaDocument20 pagesA New Coronavirus Associated With Human Respiratory Disease in ChinaAbraham Guerra OspinoNo ratings yet
- Human MonkeypoxDocument17 pagesHuman MonkeypoxJessica C. S.No ratings yet
- Pseudomonas Aeruginosa - Pathogenesis and Pathogenic MechanismsDocument24 pagesPseudomonas Aeruginosa - Pathogenesis and Pathogenic MechanismsFitryNo ratings yet
- Eliminating Murine Norovirus by Cross-FosteringDocument5 pagesEliminating Murine Norovirus by Cross-FosteringKiluaZhuNo ratings yet
- Microorganisms 11 02496Document11 pagesMicroorganisms 11 02496Robert StryjakNo ratings yet
- Studies on Epidemic Influenza: Comprising Clinical and Laboratory InvestigationsFrom EverandStudies on Epidemic Influenza: Comprising Clinical and Laboratory InvestigationsNo ratings yet
- MainDocument20 pagesMainruiNo ratings yet
- Aspergillus and Vaginal Colonization-2329-8731.1000e115Document2 pagesAspergillus and Vaginal Colonization-2329-8731.1000e115Hervis Francisco FantiniNo ratings yet
- Humanmonkeypox: Epidemiologic and Clinical Characteristics, Diagnosis, and PreventionDocument17 pagesHumanmonkeypox: Epidemiologic and Clinical Characteristics, Diagnosis, and PreventionAlejandro GraterolNo ratings yet
- 2002 - Hantaan Virus Enters Cells by Clathrin-Dependent Receptor-Mediated EndocytosisDocument10 pages2002 - Hantaan Virus Enters Cells by Clathrin-Dependent Receptor-Mediated EndocytosisFlorin BranisteNo ratings yet
- 1990 - The Protean Manifestations of Hemorrhagic Fever With Renal Syndrome. A Retrospective Review of 26 Cases From KoreaDocument7 pages1990 - The Protean Manifestations of Hemorrhagic Fever With Renal Syndrome. A Retrospective Review of 26 Cases From KoreaFlorin BranisteNo ratings yet
- 2004 JACC A Simple Risk Score For Prediction of Contrast Induced NephropathyDocument9 pages2004 JACC A Simple Risk Score For Prediction of Contrast Induced NephropathyFlorin BranisteNo ratings yet
- 2018 NEJM Outcomes After Angiography With Sodium Bicarbonate and AcetylcysteineDocument12 pages2018 NEJM Outcomes After Angiography With Sodium Bicarbonate and AcetylcysteineFlorin BranisteNo ratings yet
- AACEDocument13 pagesAACEFlorin BranisteNo ratings yet
- Acromegaly: An Endocrine Society Clinical Practice GuidelineDocument19 pagesAcromegaly: An Endocrine Society Clinical Practice GuidelineHeidy Bravo RamosNo ratings yet
- 2000 - Persistent Hantavirus Infections Characteristics and MechanismsDocument7 pages2000 - Persistent Hantavirus Infections Characteristics and MechanismsFlorin BranisteNo ratings yet
- 1999 - Hantavirus Infections Epidemiology and Pathogenesis - ElsevierDocument9 pages1999 - Hantavirus Infections Epidemiology and Pathogenesis - ElsevierFlorin BranisteNo ratings yet
- 1978 - Isolation of The Etiologic Agent of Korean Hemorrhagic Fever - OxfordDocument11 pages1978 - Isolation of The Etiologic Agent of Korean Hemorrhagic Fever - OxfordFlorin BranisteNo ratings yet
- 1995 - Hantaviruses Clinical, Microbiologic, and Epidemiologic AspectsDocument40 pages1995 - Hantaviruses Clinical, Microbiologic, and Epidemiologic AspectsFlorin BranisteNo ratings yet
- 2017 - Insufficient Efficacy and Safety of Intravenous Ribavirin in Treatment of Haemorrhagic Fever With Renal Syndrome Caused by Puumala Virus.Document8 pages2017 - Insufficient Efficacy and Safety of Intravenous Ribavirin in Treatment of Haemorrhagic Fever With Renal Syndrome Caused by Puumala Virus.Florin BranisteNo ratings yet
- 1999 - Cellular Entry of Hantaviruses Which Cause Hemorrhagic Fever with Renal Syndrome Is Mediated by β3 Integrins - JOVDocument9 pages1999 - Cellular Entry of Hantaviruses Which Cause Hemorrhagic Fever with Renal Syndrome Is Mediated by β3 Integrins - JOVFlorin BranisteNo ratings yet
- 2017 - Risk of Venous Thromboembolism Following Hemorrhagic Fever With Renal Syndrome A Self-Controlled Case Series StudyDocument6 pages2017 - Risk of Venous Thromboembolism Following Hemorrhagic Fever With Renal Syndrome A Self-Controlled Case Series StudyFlorin BranisteNo ratings yet
- 2017 - Kidney Disease in Puumala Hantavirus InfectionDocument13 pages2017 - Kidney Disease in Puumala Hantavirus InfectionFlorin BranisteNo ratings yet
- 2017 - Human Hantavirus Infection Elicits Pronounced Redistribution of Mononuclear Phagocytes in Peripheral Blood and AirwaysDocument24 pages2017 - Human Hantavirus Infection Elicits Pronounced Redistribution of Mononuclear Phagocytes in Peripheral Blood and AirwaysFlorin BranisteNo ratings yet
- 2015 - Hantavirus-Induced Disruption of The Endothelial Barrier Neutrophils Are On The Payroll - FrontiersDocument9 pages2015 - Hantavirus-Induced Disruption of The Endothelial Barrier Neutrophils Are On The Payroll - FrontiersFlorin BranisteNo ratings yet
- 2014 - Acute Hantavirus Infection Induces Galectin-3-Binding ProteinDocument30 pages2014 - Acute Hantavirus Infection Induces Galectin-3-Binding ProteinFlorin BranisteNo ratings yet
- 2017 - Raport Anual Epidemiologic Despre Hanta - ECDCDocument6 pages2017 - Raport Anual Epidemiologic Despre Hanta - ECDCFlorin BranisteNo ratings yet
- 2015 - Hantaviral Proteins Structure, Functions, and Role in Hantavirus Infection - FrontiersDocument10 pages2015 - Hantaviral Proteins Structure, Functions, and Role in Hantavirus Infection - FrontiersFlorin BranisteNo ratings yet
- 2015 - Sex, Gender, and Hemorrhagic Fever Viruses - SpringerDocument20 pages2015 - Sex, Gender, and Hemorrhagic Fever Viruses - SpringerFlorin BranisteNo ratings yet
- 1999 - Cellular Entry of Hantaviruses Which Cause Hemorrhagic Fever with Renal Syndrome Is Mediated by β3 Integrins - JOVDocument9 pages1999 - Cellular Entry of Hantaviruses Which Cause Hemorrhagic Fever with Renal Syndrome Is Mediated by β3 Integrins - JOVFlorin BranisteNo ratings yet
- 2013 - Teoria Operon - SpringerDocument64 pages2013 - Teoria Operon - SpringerFlorin BranisteNo ratings yet
- 2015 - Hantaviruses Globally Emerging Pathogens - ElsevierDocument9 pages2015 - Hantaviruses Globally Emerging Pathogens - ElsevierFlorin BranisteNo ratings yet
- 2013 - How Hantaviruses Modulate Cellular Pathways For Efficient ReplicationDocument13 pages2013 - How Hantaviruses Modulate Cellular Pathways For Efficient ReplicationFlorin BranisteNo ratings yet
- 2014 - Acute Hantavirus Infection Induces Galectin-3-Binding ProteinDocument30 pages2014 - Acute Hantavirus Infection Induces Galectin-3-Binding ProteinFlorin BranisteNo ratings yet
- 2013 - Uncovering The Mysteries of Hantavirus InfectionsDocument12 pages2013 - Uncovering The Mysteries of Hantavirus InfectionsFlorin BranisteNo ratings yet
- 2015 - Diagnosis of Hantavirus Infection in HumansDocument8 pages2015 - Diagnosis of Hantavirus Infection in HumansFlorin BranisteNo ratings yet
- 2013 - The Broad Spectrum of Hantaviruses and Their Hosts in Central Europe - AEPressDocument8 pages2013 - The Broad Spectrum of Hantaviruses and Their Hosts in Central Europe - AEPressFlorin BranisteNo ratings yet
- 2013 - Uncovering The Mysteries of Hantavirus InfectionsDocument12 pages2013 - Uncovering The Mysteries of Hantavirus InfectionsFlorin BranisteNo ratings yet
- 2013 - How Hantaviruses Modulate Cellular Pathways For Efficient ReplicationDocument13 pages2013 - How Hantaviruses Modulate Cellular Pathways For Efficient ReplicationFlorin BranisteNo ratings yet
- A Ghost StoryDocument10 pagesA Ghost StoryTrần MạnhNo ratings yet
- A Cause For Our Times: Oxfam - The First 50 YearsDocument81 pagesA Cause For Our Times: Oxfam - The First 50 YearsOxfamNo ratings yet
- Chimdesa J. Functional FoodsDocument201 pagesChimdesa J. Functional FoodsChimdesa100% (1)
- A Case of Haemochromatosis and Diabetes A Missed OpportunityDocument111 pagesA Case of Haemochromatosis and Diabetes A Missed Opportunitymimran1974No ratings yet
- Lesson 1 Context CluesDocument33 pagesLesson 1 Context CluesRomnick BistayanNo ratings yet
- Abnormal Psychology Unit IDocument14 pagesAbnormal Psychology Unit IMahadevan K V100% (1)
- Spreadsheet and Presentation Skills SyllabusDocument4 pagesSpreadsheet and Presentation Skills SyllabusGbox CTCNo ratings yet
- Test Bank For American Pageant Volume 1 16th EditionDocument36 pagesTest Bank For American Pageant Volume 1 16th Editionzoonwinkfoxyj8100% (48)
- Business Decision Making Assignment (July 2015)Document23 pagesBusiness Decision Making Assignment (July 2015)Michael Oppong100% (1)
- Amelia Wills CV 2021 VDocument4 pagesAmelia Wills CV 2021 Vapi-446566858No ratings yet
- Evosys Fixed Scope Offering For Oracle Fusion Procurement Cloud ServiceDocument12 pagesEvosys Fixed Scope Offering For Oracle Fusion Procurement Cloud ServiceMunir AhmedNo ratings yet
- Marine Clastic Reservoir Examples and Analogues (Cant 1993) PDFDocument321 pagesMarine Clastic Reservoir Examples and Analogues (Cant 1993) PDFAlberto MysterioNo ratings yet
- Merger Case AnalysisDocument71 pagesMerger Case Analysissrizvi2000No ratings yet
- Create Sales Order (Bapi - Salesorder - Createfromdat2) With Bapi Extension2Document5 pagesCreate Sales Order (Bapi - Salesorder - Createfromdat2) With Bapi Extension2raky03690% (1)
- The Tale of Sweet-Friend and Ali-NurDocument2 pagesThe Tale of Sweet-Friend and Ali-NurJomarie Siason Sumagpao100% (1)
- Surveying 2 Practical 3Document15 pagesSurveying 2 Practical 3Huzefa AliNo ratings yet
- Types of Companies Classified by Incorporation, Membership, Liability and ControlDocument11 pagesTypes of Companies Classified by Incorporation, Membership, Liability and ControlPrasad BulbuleNo ratings yet
- Review of Esu Yoruba God Power and The IDocument7 pagesReview of Esu Yoruba God Power and The IBoris MilovicNo ratings yet
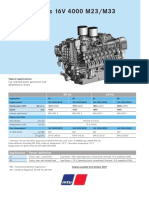
- Diesel Engines 16V 4000 M23/M33: 50 HZ 60 HZDocument2 pagesDiesel Engines 16V 4000 M23/M33: 50 HZ 60 HZAlberto100% (1)
- Warren BuffetDocument11 pagesWarren BuffetSopakirite Kuruye-AleleNo ratings yet
- On Healing Powers: Asclepius, Caduceus and AntibodiesDocument4 pagesOn Healing Powers: Asclepius, Caduceus and AntibodiesasclepiuspdfsNo ratings yet
- PCC 3300 PDFDocument6 pagesPCC 3300 PDFdelangenico4No ratings yet
- USD - DPF Cleaning Machine - POSEYDON1000 - PolDocument8 pagesUSD - DPF Cleaning Machine - POSEYDON1000 - PolAbaidi RabieNo ratings yet
- Lab Manual 06 CSE 314 Sequence and Communication DiagramDocument6 pagesLab Manual 06 CSE 314 Sequence and Communication DiagramMufizul islam NirobNo ratings yet
- Jumpin' Beans Cafe Near SchoolDocument4 pagesJumpin' Beans Cafe Near SchoolJhon Axl Heart RaferNo ratings yet
- SYLLABUS FYUP-PoliticalScience PDFDocument105 pagesSYLLABUS FYUP-PoliticalScience PDFIshta VohraNo ratings yet
- Group Assgnmt 8 Rev080515Document9 pagesGroup Assgnmt 8 Rev080515Suhaila NamakuNo ratings yet
- Og FMTDocument5 pagesOg FMTbgkinzaNo ratings yet
- Stephen Mace Seizing PowerDocument168 pagesStephen Mace Seizing PowerLuke AndrewsNo ratings yet
- Common Expressions in Business 2Document2 pagesCommon Expressions in Business 2abdeljelil manelNo ratings yet