Professional Documents
Culture Documents
Postoperative Care: Post Operative Note and Orders
Postoperative Care: Post Operative Note and Orders
Uploaded by
Jarda DacuagOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Postoperative Care: Post Operative Note and Orders
Postoperative Care: Post Operative Note and Orders
Uploaded by
Jarda DacuagCopyright:
Available Formats
Postoperative care
Post operative note and orders
The patient should be discharged to the ward with comprehensive orders for
the following:
• Vital signs
• Pain control
• Rate and type of intravenous fluid
• Urine and gastrointestinal fluid output
• Other medications
• Laboratory investigations
The patient’s progress should be monitored and should include at least:
• A comment on medical and nursing observations
• A specific comment on the wound or operation site
• Any complications
• Any changes made in treatment
Aftercare: Prevention of complications
• Encourage early mobilization:
o Deep breathing and coughing
o Active daily exercise
o Joint range of motion
o Muscular strengthening
o Make walking aids such as canes, crutches and walkers available
and provide instructions for their use
• Ensure adequate nutrition
• Prevent skin breakdown and pressure sores:
o Turn the patient frequently
o Keep urine and faeces off skin
• Provide adequate pain control
Discharge note
On discharging the patient from the ward, record in the notes:
• Diagnosis on admission and discharge
• Summary of course in hospital
• Instructions about further management, including drugs prescribed.
Ensure that a copy of this information is given to the patient, together with
details of any follow-up appointment
WHO/EHT/CPR: WHO Surgical Care at the District Hospital 2003
Postoperative Management
If the patient is restless, something is wrong.
Look out for the following in recovery:
• Airway obstruction
• Hypoxia
• Haemorrhage: internal or external
• Hypotension and/or hypertension
• Postoperative pain
• Shivering, hypothermia
• Vomiting, aspiration
• Falling on the floor
• Residual narcosis
The recovering patient is fit for the ward when:
• Awake, opens eyes
• Extubated
• Blood pressure and pulse are satisfactory
• Can lift head on command
• Not hypoxic
• Breathing quietly and comfortably
• Appropriate analgesia has been prescribed and is safely established
WHO/EHT/CPR: WHO Surgical Care at the District Hospital 2003
Post operative pain relief
• Pain is often the patient’s presenting symptom. It can provide useful clinical information
and it is your responsibility to use this information to help the patient and alleviate
suffering.
• Manage pain wherever you see patients (emergency, operating room and on the ward)
and anticipate their needs for pain management after surgery and discharge.
• Do not unnecessarily delay the treatment of pain; for example, do not transport a patient
without analgesia simply so that the next practitioner can appreciate how much pain the
person is experiencing.
Pain management is our job.
Pain Management and Techniques
• Effective analgesia is an essential part of postoperative management.
• Important injectable drugs for pain are the opiate analgesics. Nonsteroidal anti-
inflammatory drugs (NSAIDs), such as diclofenac (1 mg/kg) and ibuprofen can also be
given orally and rectally, as can paracetamol (15 mg/kg).
• There are three situations where an opiate might be given:
o Preoperatively
o Intraoperatively
o Postoperatively
• Opiate premedication is rarely indicated, although an injured patient in pain may have
been given an opiate before coming to the operating room.
• Opiates given pre- or intraoperatively have important effects in the postoperative period
since there may be delayed recovery and respiratory depression, even necessitating
mechanical ventilation.
• Short acting opiate fentanyl is used intra-operatively to avoid this prolonged effect.
• Naloxone antagonizes (reverses) all opiates, but its effect quickly wears off.
• Commonly available inexpensive opiates are pethidine and morphine.
• Morphine has about ten times the potency and a longer duration of action than pethidine.
(continued next page)
WHO/EHT/CPR: WHO Surgical Care at the District Hospital 2003
Post operative pain relief (continued)
• Ideal way to give analgesia postoperatively is to:
o Give a small intravenous bolus of about a quarter or a third of the maximum dose
(e.g. 25 mg pethidine or 2.5 mg morphine for an average adult)
o Wait for 5–10 minutes to observe the effect: the desired effect is analgesia, but
retained consciousness
o Estimate the correct total dose (e.g. 75 mg pethidine or 7.5 mg morphine) and
give the balance intramuscularly.
o With this method, the patient receives analgesia quickly and the correct dose is
given
• If opiate analgesia is needed on the ward, it is most usual to give an intramuscular
regimen:
¾ Morphine:
– Age 1 year to adult: 0.1–0.2 mg/kg
– Age 3 months to 1 year: 0.05–0.1 mg/kg
¾ Pethidine: give 7–10 times the above doses if using pethidine
• Opiate analgesics should be given cautiously if the age is less than 1 year. They are
not recommended for babies aged less than 3 months unless very close monitoring in
a neonatal intensive care unit is available.
Anaesthesia & Pain Control in Children
• Ketamine anaesthesia is widely used for children in rural centres (see pages 14–14 to 14–21),
but is also good for pain control.
• Children suffer from pain as much as adults, but may show it in different ways.
• Make surgical procedures as painless as possible:
o Oral paracetamol can be given several hours prior to operation
o Local anaesthetics (bupivacaine 0.25%, not to exceed 1 ml/kg) administered in the
operating room can decrease incisional pain
o Paracetamol (10–15 mg/kg every 4–6 hours) administered by mouth or rectally is a
safe and effective method for controlling postoperative pain
o For more severe pain, use intravenous narcotics (morphine sulfate 0.05–0.1 mg/kg IV)
every 2–4 hours
o Ibuprofen 10 mg/kg can be administered by mouth every 6–8 hours
o Codeine suspension 0.5–1 mg/kg can be administered by mouth every 6 hours, as
needed.
WHO/EHT/CPR: WHO Surgical Care at the District Hospital 2003
You might also like
- Veterinary Emergency Medicine SecretsDocument585 pagesVeterinary Emergency Medicine SecretsDea Marie Lopez100% (21)
- 25 Cardiovascular DiseaseDocument35 pages25 Cardiovascular DiseaseBramantyo NugrosNo ratings yet
- The Dialysis ProcessDocument125 pagesThe Dialysis Processacque100% (1)
- Nursing Care Plan For "Lung Cancer Postoperative Care"Document12 pagesNursing Care Plan For "Lung Cancer Postoperative Care"jhonroks94% (18)
- Allergy and Immunology: Immunodeficiency 10 Warning Signs of ImmunodeficiencyDocument24 pagesAllergy and Immunology: Immunodeficiency 10 Warning Signs of Immunodeficiencyacque100% (2)
- Congenital Heart Disease: Education and Practice GapsDocument18 pagesCongenital Heart Disease: Education and Practice GapsAlvaro Ignacio Lagos SuilNo ratings yet
- Objective Structured Clinical & Practical ExaminationDocument72 pagesObjective Structured Clinical & Practical ExaminationNihad Oteifa75% (4)
- Anaesthesia For The Obese Obstetric PatientDocument85 pagesAnaesthesia For The Obese Obstetric PatientDr.Deb Sanjay Nag100% (1)
- 13.24 Abdominal-InjuryDocument42 pages13.24 Abdominal-InjuryMuhammad FajarNo ratings yet
- Navair 01-1a-35 PDFDocument390 pagesNavair 01-1a-35 PDFcataninoNo ratings yet
- Operating Room Preparation: Philipp Acaso Ralph ArcoDocument158 pagesOperating Room Preparation: Philipp Acaso Ralph ArcoTiffany Luv Adrias100% (1)
- ObsGyn OSCE Notes PDFDocument52 pagesObsGyn OSCE Notes PDFNorman Ahmad RiyandiNo ratings yet
- Anaesthesia For Renal TransplantationDocument46 pagesAnaesthesia For Renal TransplantationShehan WijayasiriwardanaNo ratings yet
- Anesthesia: Mrs - SanthiDocument59 pagesAnesthesia: Mrs - SanthisanthiyasandyNo ratings yet
- Department of Internal Medicine: Orientation Package For ClerksDocument23 pagesDepartment of Internal Medicine: Orientation Package For Clerksxjoedu100% (1)
- Et CareDocument15 pagesEt CarePaulo GarciaNo ratings yet
- Asthma Review PDFDocument12 pagesAsthma Review PDFdanielc503No ratings yet
- Surgery CaseDocument43 pagesSurgery CaseAvni GuptaNo ratings yet
- Airway ManagmentDocument42 pagesAirway Managmentkader abdiNo ratings yet
- Metal-Earth Imbalance.! Treats ANY Tai Yin Problems & ANY Yang Ming Problems!! Wood-Earth Imbalance. !Document1 pageMetal-Earth Imbalance.! Treats ANY Tai Yin Problems & ANY Yang Ming Problems!! Wood-Earth Imbalance. !Diego NicoliniNo ratings yet
- Principles of Icu VentilatorsDocument98 pagesPrinciples of Icu VentilatorsshivamNo ratings yet
- OSCE Surgery Block PDFDocument31 pagesOSCE Surgery Block PDFanabanananNo ratings yet
- 17-18 Chong Kar Mun's Anaesthesia NotesDocument32 pages17-18 Chong Kar Mun's Anaesthesia NotesElaineNo ratings yet
- Day Case Surgery SajeebDocument34 pagesDay Case Surgery SajeebMahbubur Rahman0% (1)
- Preanesthetic Medication JasminaDocument44 pagesPreanesthetic Medication Jasminaanjali sNo ratings yet
- NCM119ClinicalLab Pediatric Ward Pneumonia Case Study Group 4Document40 pagesNCM119ClinicalLab Pediatric Ward Pneumonia Case Study Group 4Allysa MacalinoNo ratings yet
- ShockDocument25 pagesShockSurya Mohan Jha100% (1)
- Effect of Postoperative Continuation of Antibiotic Prophylaxis On The Incidence of Surgical Site InfectionDocument11 pagesEffect of Postoperative Continuation of Antibiotic Prophylaxis On The Incidence of Surgical Site InfectionAde Ewa Permana100% (1)
- DR - Abeidi's Review FinalDocument157 pagesDR - Abeidi's Review FinalSandra AbboudNo ratings yet
- Fluid & Electrolytes Management (Nabil)Document78 pagesFluid & Electrolytes Management (Nabil)Ahmad Nabil Md RosliNo ratings yet
- Sepsis PowerPoint Slide Presentation - The Guidelines - Implementation For The FutureDocument25 pagesSepsis PowerPoint Slide Presentation - The Guidelines - Implementation For The FutureDwiyanti OktaviaNo ratings yet
- Day Care SurgeryDocument5 pagesDay Care SurgeryazharmoNo ratings yet
- Pneumothorax: Dr. Sivaraj KarriDocument50 pagesPneumothorax: Dr. Sivaraj KarriYamini ChowdaryNo ratings yet
- OSCE Station 1 Diabetic LL ExamDocument5 pagesOSCE Station 1 Diabetic LL ExamJeremy YangNo ratings yet
- Meaning of Different Types of SputumDocument10 pagesMeaning of Different Types of SputumCharlotte's WebNo ratings yet
- Physiology of PleuraDocument16 pagesPhysiology of PleuraMohamedSalah100% (2)
- Cme Fluid and Electrolytes 2902016Document37 pagesCme Fluid and Electrolytes 2902016Mohd Faie Ramli0% (1)
- 21 - Postoperative Complications and Managament IDocument30 pages21 - Postoperative Complications and Managament IAmmarNo ratings yet
- Ii. Poor Exercise Tolerance Ii. PalpationDocument14 pagesIi. Poor Exercise Tolerance Ii. PalpationLeyana AbdullahNo ratings yet
- Post Operative HemorrhageDocument16 pagesPost Operative Hemorrhagenishimura89No ratings yet
- Thyroid Function TestsDocument25 pagesThyroid Function TestsEva SinghNo ratings yet
- PRE ANAESTHETIC ASSESSMENT New 1Document41 pagesPRE ANAESTHETIC ASSESSMENT New 1lokeswara reddyNo ratings yet
- MBBS2014 SurgeryCaseAnalysisDocument194 pagesMBBS2014 SurgeryCaseAnalysisDaniel LimNo ratings yet
- Approach To Septic ShockDocument16 pagesApproach To Septic ShockRaja EllysyaNo ratings yet
- Pre Anaesthetic Check-UpDocument4 pagesPre Anaesthetic Check-UpUdoy PaulNo ratings yet
- Carcinoma Penis Management: Dr. Lilamani Rajthala MS Resident Moderator: Dr. Samir ShresthaDocument63 pagesCarcinoma Penis Management: Dr. Lilamani Rajthala MS Resident Moderator: Dr. Samir ShresthaBibek GhimireNo ratings yet
- Intercollegiate Surgical Curriculum ENTDocument98 pagesIntercollegiate Surgical Curriculum ENTMendhi Ashish AnilNo ratings yet
- OSCE BoursicotDocument55 pagesOSCE BoursicotShouja ChauduryNo ratings yet
- TriageDocument42 pagesTriageNic JiNo ratings yet
- Premedication: by Alif Moderator: Dr. JasmineDocument45 pagesPremedication: by Alif Moderator: Dr. JasmineAlef AminNo ratings yet
- Practice Guidelines For Juniors 01 June 2016Document3 pagesPractice Guidelines For Juniors 01 June 2016ElaineNo ratings yet
- Critical Care Update PDFDocument25 pagesCritical Care Update PDFHugo PozoNo ratings yet
- 25 Common Surgical ConditionsDocument3 pages25 Common Surgical ConditionsMu AbNo ratings yet
- Antepartum Haemorrhage: BY: Ms. R. Liangkiuwiliu Assistant Professor, Obg SSNSR, SuDocument44 pagesAntepartum Haemorrhage: BY: Ms. R. Liangkiuwiliu Assistant Professor, Obg SSNSR, SuLiangkiuwiliuNo ratings yet
- August - September - 2002 Osce Stations MelbourneDocument12 pagesAugust - September - 2002 Osce Stations Melbournemnigam64No ratings yet
- Thoracotomy: Surgery For Lung ProblemsDocument14 pagesThoracotomy: Surgery For Lung ProblemsPutri ChalqieNo ratings yet
- UGIHDocument59 pagesUGIHEkkawit IamthonginNo ratings yet
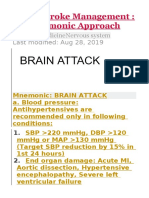
- Acute Stroke ManagementDocument8 pagesAcute Stroke ManagementГурам ЧахвадзеNo ratings yet
- Standard Management of Various Medical ConditionsDocument47 pagesStandard Management of Various Medical ConditionsManik bhushan ShrivastavNo ratings yet
- General Surgery: Post-Operative Care and ManagementDocument9 pagesGeneral Surgery: Post-Operative Care and ManagementMohammed Yousif AbdualjabbarNo ratings yet
- STAGES of AnesthesiaDocument4 pagesSTAGES of AnesthesiaMabz Posadas BisnarNo ratings yet
- Pain Management in The Emergency: Dr. Prathiba Prasad Emergency Physician Masafi HospitalDocument50 pagesPain Management in The Emergency: Dr. Prathiba Prasad Emergency Physician Masafi HospitalPrathiba PrassaddNo ratings yet
- Revision Long Case Obs GynaeDocument10 pagesRevision Long Case Obs GynaeHo Yong WaiNo ratings yet
- R Reeggaarrddiinngg Tthhee Eexxaam Miinnaattiioonn: GDD ? H@Qka A9Fk KMJ? GFK H9Cakl9FDocument3 pagesR Reeggaarrddiinngg Tthhee Eexxaam Miinnaattiioonn: GDD ? H@Qka A9Fk KMJ? GFK H9Cakl9FAnaesthesiologistIntensivistNo ratings yet
- What Is A Gastrectomy?Document4 pagesWhat Is A Gastrectomy?Priyanka JangraNo ratings yet
- Obstetric Gynaecology Jan 11Document32 pagesObstetric Gynaecology Jan 11selvie87No ratings yet
- Pulsus ParadoxusDocument2 pagesPulsus ParadoxusHassan.shehriNo ratings yet
- Pre Exam Surgical Notes 2Document166 pagesPre Exam Surgical Notes 2flor vickyNo ratings yet
- Membership Transfers: Process For Granting and Accepting Membership Transfers Additional Transfer InformationDocument3 pagesMembership Transfers: Process For Granting and Accepting Membership Transfers Additional Transfer InformationacqueNo ratings yet
- Salvation in The TribulationDocument4 pagesSalvation in The TribulationacqueNo ratings yet
- Uniform ESRD Transient Hemodialysis FormDocument3 pagesUniform ESRD Transient Hemodialysis FormacqueNo ratings yet
- Cardiac QuestionsDocument13 pagesCardiac Questionsacque100% (1)
- Erik Erikson: by Dr. C. George BoereeDocument9 pagesErik Erikson: by Dr. C. George Boereeacque100% (1)
- KMXT Run WaiverDocument1 pageKMXT Run WaiveracqueNo ratings yet
- C CCC !"#" $ !"#" C !"#" !%# # # C#%$#C #""$Document10 pagesC CCC !"#" $ !"#" C !"#" !%# # # C#%$#C #""$acqueNo ratings yet
- Medical Checkup Requirement For Permission Work Visa in Kingdom of BahrainDocument1 pageMedical Checkup Requirement For Permission Work Visa in Kingdom of BahrainAngle_BahNo ratings yet
- NURSING CARE PLAN Lung Cancer..jonardDocument2 pagesNURSING CARE PLAN Lung Cancer..jonardJ.C. Kate Cruz67% (3)
- MSDS Antiscalant HAI 1020TDocument2 pagesMSDS Antiscalant HAI 1020TKumbang KambingNo ratings yet
- Affordable House Designs To Improve Health in Rural Africa - Northeastern TanzaniaDocument12 pagesAffordable House Designs To Improve Health in Rural Africa - Northeastern TanzaniaAlberto CumerlatoNo ratings yet
- Start CPR Shout For Help/Activate Emergency Response: Give Oxygen Attach Monitor/DefibrillatorDocument2 pagesStart CPR Shout For Help/Activate Emergency Response: Give Oxygen Attach Monitor/DefibrillatorFelicia ErikaNo ratings yet
- Certificate of Consent - ExamineeDocument1 pageCertificate of Consent - Examineemariele100% (4)
- ASPERGILLOSISDocument8 pagesASPERGILLOSISEsshai Painaga PelingonNo ratings yet
- Bedlam MSDSDocument2 pagesBedlam MSDSmfspongebobNo ratings yet
- COVID 19 Bharat India Daily Cases 18454 20 10 2021 397 DaysBasedAn Analytical InformativeView DownLoadExcelFileReadPages1+Page5Document182 pagesCOVID 19 Bharat India Daily Cases 18454 20 10 2021 397 DaysBasedAn Analytical InformativeView DownLoadExcelFileReadPages1+Page5P Eng Suraj SinghNo ratings yet
- Opt Out Mask FormDocument1 pageOpt Out Mask FormWTXL ABC27No ratings yet
- BULETIN DE ANALIZA Nr. 3241708 / 05.12.2021: Osoianu AndreiDocument2 pagesBULETIN DE ANALIZA Nr. 3241708 / 05.12.2021: Osoianu AndreiandreiNo ratings yet
- Material Safety Data Sheet Cemfair FD: 1: Product and Company IdentificationDocument4 pagesMaterial Safety Data Sheet Cemfair FD: 1: Product and Company IdentificationZeya AliNo ratings yet
- I - PAV+ Clinical Summary - Carteaux Et Al - EnGDocument2 pagesI - PAV+ Clinical Summary - Carteaux Et Al - EnGJuan Genaro Martinez PeñaNo ratings yet
- Polyaluminium Chloride MSDSDocument6 pagesPolyaluminium Chloride MSDSNandhakumarNo ratings yet
- DrowningDocument9 pagesDrowningCarlos Alberto Torres LópezNo ratings yet
- Asam Asetat 3% - MSDS MyDocument6 pagesAsam Asetat 3% - MSDS MyAnnisa Nur JNo ratings yet
- نسخة COPD case A.AmriehDocument14 pagesنسخة COPD case A.AmriehMarwa sweityNo ratings yet
- Hexametafosfato de SodioDocument5 pagesHexametafosfato de SodioYeison DuránNo ratings yet
- Gambaran Usia Pada Kejadian Covid-19: Rosyada Elviani Chairil Anwar Rico Januar SitorusDocument6 pagesGambaran Usia Pada Kejadian Covid-19: Rosyada Elviani Chairil Anwar Rico Januar SitorusRizka ZahroNo ratings yet
- Medical Certificate: Luz, Daxx Raven DDocument2 pagesMedical Certificate: Luz, Daxx Raven DRobbie Rose LavaNo ratings yet
- Corning Guardiant™ Antimicrobial Particles: WarningDocument1 pageCorning Guardiant™ Antimicrobial Particles: WarningmulysieNo ratings yet
- Critical Equipment and Technologies Developed by DRDO For Combating COVID-19 Pandemic 09/06/2020Document76 pagesCritical Equipment and Technologies Developed by DRDO For Combating COVID-19 Pandemic 09/06/2020Yamini PatarNo ratings yet