Professional Documents
Culture Documents
Physiology Pancreas
Uploaded by
Ko HakuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Physiology Pancreas
Uploaded by
Ko HakuCopyright:
Available Formats
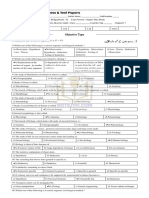
PHYSIOLOGY 4TH BIMO
ENDOCRINE SYSTEM- PANCREAS - GLUCOSE is the primary stimulus of insulin
DR.PALOMA secretion
PANCREATIC HORMONES:
- GLUT2 transporter facilitates entry of glucose
1. INSULIN into beta cells
- Protein hormone from beta cells of the
pancreas
- Belongs to the gene family that include: insulin- - GLUTOKINASE ENZYME- the “GLUCOSE
like growth factors I and II (IGF I & IGF II) and SENSOR” of beta cells. This phosphorylates
relaxin glucose to G6P once it enters the beta cells. It
- Synthesized on the polyribosomes as has been found that the rate of glucose entry is
preproinsulin endoplasmic reticulum as correlated to the rate of glucose
proinsulin golgi apparatus as secretory phosphorylation and directly related to insulin
granules in zinc-bound crystals exocytosis secretion.
…INSULIN
- ATP-SENSITIVE K+ CHANNELS- closes with G6P
metabolism by beta cells. This has ATP-binding
subunit called SUR which is also activated by
sulfonylurea drugs (oral agents for
hyperglycemia)
- VOLTAGE GATED CALCIUM CHANNELS open-
activates exocytosis of insulin/proinsulin
secretory granules
OTHER FACTORS THAT INCREASE INSULIN SECRETION:
- Amino Acid
- Beta keto acids
- Glucagon
*The peptide chain of insulin’s prohormone folds back on - Acetylcholine-vagal (parasympathetic)
itself with the help of disulfide (S-S) bonds. The prohormone cholinergic innervation (i.e.- in response to a
cleaves to insulin and C-peptide meal)
1 - DocTROJAN
Free fatty acids (through a G-protein coupled
reactor)
…INSULIN - Intestinal hormones (i.e.-glucagon-like peptide1
- Is an anabolic and hypoglycemic hormone (GPL-1), gastric inhibitory polypeptide- GIP)- act
- Facilitates glucose entry into cells except brain, by raising cyclic-AMP which amplifies the effect
kidney tubules, intestinal mucosa, and red of calcium
blood cells - BUT THESE AGENTS DO NOT INCREASE INSULIN
- Indirectly facilitates glucose entry into SECRETION IN THE ABSENCE OF GLUCOSE
hepatocytes by promoting glycogenesis
(reducing intracellular glucose) FACTORS THAT INHIBIT INSULIN SECRETION:
- Directly facilitates glucose entry in other cells - ALPHA 2 ADRENERGIC RECEPTORS w/c are
by its action on the cell membrane activated by epinephrine from adrenal medulla
- Has a half-life of 5-8 minutes & norepinephrine from postganglionic
- Degraded rapidly from the blood by sympathetic fibers. This act by decreasing cyclic
INSULINASE in the liver, kidney and other AMP.
tissues - Adrenergic inhibition of insulin serve to protect
- Because insulin is secreted into the portal vein, against hypoglycemia especially during exercise
it is exposed to liver insulinase before it enters - Beta adrenergic blockers
the peripheral circulation. As a consequence, - Thiazides
almost half the insulin is degraded before - Alloxan
leaving the liver. Thus peripheral tissues are - Somatostatin from D cells (unclear in humans)
exposed to only half the serum insulin THE INSULIN RECEPTOR:
concentration as the liver - Member of the RECEPTOR TYROSINE KINASE
(RTK) family
- Insulin begins to be released a few minutes - Composed of alpha/beta monomers. The alpha
after food intake subunit are external and contain the hormone
- If stimulus is maintained, insulin secretion falls binding sites. The beta span the membrane and
within 10 mins. And slowly rise again within 1 contain the tyrosine kinase domain
hour. These are the EARLY PHASE AND LATE - Binding of insulin to the receptor induces cross
PHASE OF INSULIN RELEASE. The early phase phosphorylation of each beta subunit on 3
releases the pre-formed whereas the late tyrosine residues
phase releases the newly formed insulin.
- Termination of insulin/IR signaling potentially circulation, a large portion of the hormone
play a role in insulin resistance and type 2 never reach the systemic circulation.
diabetes mellitus
- Insulin down-regulate its own receptor by FACTORS THAT STIMULATE GLUCAGON SECRETION
receptor mediated endocytosis
- Several serine/ threonine protein kinases are - Drop in blood glucose. A major stimulus for
activated by insulin w/c inactivate IR and IRS glucagon secretion
proteins - Circulating catecholamines stimulate glucagon
- Activation of “suppressor of cytokine signaling” secretion via Beta 2 adrenergic receptors
(SOCS) family of protein which residues activity - Serum amino acids. This means that a protein
levels of IR and IRS proteins meal will increase postprandial levels of both
insulin and glucagon which protects against
PRINCIPAL ACTIONS OF INSULIN hypoglycemia; whereas a carbohydrate meal
stimulates inly insulin.
ADIPOSE TISSUE - Fasting hypoglycemia, exercise, CCK, cortisol,
- Increase glucose entry stress, and cholesterol.
- Increase fatty acid synthesis
- Increase glycerol phosphate synthesis FACTORS THAT STIMULATE INSULIN INHIBIT GLUCAGON
- Increase triglyceride deposition SECRETION.
- Activation of lipoprotein lipase
- Inhibition of hormone-sensitive lipase GLUCAGON SECRETION IS INHIBITED BY SOMATOSTATIN, FREE
- Increased potassium uptake FATTY ACIDS, SECRETIN, KETONES AND INSULIN
SKELETAL MUSCLE SOMATOSTATIN
- From DELTA CELLS
- Increased glucose entry - 15-amino acid single chain polypeptide
- Increased glycogen synthesis - A local regulator of insulin and glucagon
- Increased amino acid uptake secretion
- Increased protein synthesis in ribosomes - Inhibits secretion of both insulin and glucagon
- Decreased protein catabolism - Also found in the hypothalamus (GH secretion
- Decreased release of gluconeogenic amino inhibitor)
acids
- Increased ketone uptake DIABETES MELLITUS
2 - Increased potassium uptake DocTROJAN
A.BASIC BIOCHEMICAL DEFECTS
LIVER
- Decreased cyclic AMP 1. Decreased glucose uptake by cells leading to:
- Decreased ketogenesis - Hyperglycemia
- Increased protein synthesis - Glucosuria
- Increased lipid synthesis - Osmotic diuresis
- Decreased glucose output due to decreased - Urinary loss of sodium and potassium
gluconeogenesis and increased glycogen - Dehydration if water intake is inhibited
synthesis
2. Increased protein catabolism increasing:
GLUCAGON - Plasma amino acid conc.
- From alpha cells - Nitrogen loss in the urine
- The primary “COUNTERREGULATORY”
HORMONE that INCREASES BLOOD GLUCOSE 3. Increased lipolysis leading to:
LEVELS through its effects on liver glucose - Increased plasma free fatty acids
output - Ketonemia, ketonuria, metabolic acidosis
- A CATABOLIC, GLYCOGENOLYTIC, - Respiratory compensation lowering PCO2
GLUCONEOGENIC, LIPOLYTIC AND KETOGENIC
HORMONE 4. Increased glycogenolysis
- A member of the secretin gene family. The 5. Increased gluconeogenesis
precursor preglucagon has the AA sequences
for glucagon (GPL1 and GPL2) which is cleaved CLINICAL SIGNS AND SYMPTOMS
to produce the 29-amino acid peptide glucagon
- Circulates in an unbound form with a short half - Polyuria, nocturia and polydipsia
life of 6 minutes - Polyphagia with weight loss
- LIVER is the primary target of glucagon with - Dehydration in cases of failure to drink water
only small effects on peripheral tissues. This is - Acetone breath
also THE PREDOMINANT SITE OF GLUCAGON - Kussmaul’s breathing
DEGRADATION (80%). Because the glucagon - Vomiting and abdominal pain
(from gut or pancreas) enters the hepatic portal - Stupor coma and death
vein to the liver before reaching the systemic
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- (Current Topics in Microbiology and Immunology) Dong Yu, Benjamin Petsch - mRNA Vaccines. 437-Springer (2023) PDFDocument215 pages(Current Topics in Microbiology and Immunology) Dong Yu, Benjamin Petsch - mRNA Vaccines. 437-Springer (2023) PDFJean Bosco VuningomaNo ratings yet
- Metabolic OR Endocrine Disorders: Amanda Du, MD, DPPS, DPSNBM Pediatrician-NeonatologistDocument124 pagesMetabolic OR Endocrine Disorders: Amanda Du, MD, DPPS, DPSNBM Pediatrician-NeonatologistLyn LynNo ratings yet
- PCP Obe-Cbtp Dops Rtp-Acc Form#7Document6 pagesPCP Obe-Cbtp Dops Rtp-Acc Form#7Ko HakuNo ratings yet
- 1.concepts of Growth & DevelopmentDocument107 pages1.concepts of Growth & DevelopmentYuvashreeNo ratings yet
- Respiratory System Study Questions Directions: Each of The Numbered Items or Incompl Ete Statements in This Section Is Followed by AnswersDocument7 pagesRespiratory System Study Questions Directions: Each of The Numbered Items or Incompl Ete Statements in This Section Is Followed by AnswersKo Haku100% (1)
- GROUP 2 Exercise 2 Gene Segregation and Interaction PDFDocument9 pagesGROUP 2 Exercise 2 Gene Segregation and Interaction PDFMary Joy Annika MagtibayNo ratings yet
- Genome Editing: Toni Cathomen Matthew Hirsch Matthew Porteus EditorsDocument276 pagesGenome Editing: Toni Cathomen Matthew Hirsch Matthew Porteus EditorsSorin Dinu100% (2)
- Synopsis On Agriculture (Second Edition)Document146 pagesSynopsis On Agriculture (Second Edition)milind73% (11)
- Physical Principles of Gas ExchangeDocument12 pagesPhysical Principles of Gas ExchangeKo HakuNo ratings yet
- Normality, Mental Health, Life Cycle TheoryDocument2 pagesNormality, Mental Health, Life Cycle TheoryKo HakuNo ratings yet
- The Cerebellum (Revised)Document8 pagesThe Cerebellum (Revised)Ko HakuNo ratings yet
- Cranial Fossa Notes - HelpfulDocument4 pagesCranial Fossa Notes - HelpfulKo HakuNo ratings yet
- Contents of Cranial FossaDocument1 pageContents of Cranial FossaKo HakuNo ratings yet
- RTRMF-CM - Pedia Clinics GuideDocument7 pagesRTRMF-CM - Pedia Clinics GuideKo HakuNo ratings yet
- Solved MCQsDocument3 pagesSolved MCQssaman iftikharNo ratings yet
- CladisticDocument27 pagesCladisticKylie MorganNo ratings yet
- Meat 2.0 - The Regulatory Environment of Plant-Based and Cultured MeatDocument10 pagesMeat 2.0 - The Regulatory Environment of Plant-Based and Cultured MeatmaurOznNo ratings yet
- Article - A New Light On Skin ColorDocument2 pagesArticle - A New Light On Skin ColorAref AhmadNo ratings yet
- HemtDocument42 pagesHemtSaily JaquezNo ratings yet
- Bogard Et Al (2019) Deep Neural Network For Predicting and EngineeringDocument40 pagesBogard Et Al (2019) Deep Neural Network For Predicting and EngineeringFRANCISCO ELI LEZAMA GUTIERREZNo ratings yet
- Science 9 Quarter 1 Week 3 Sim 4Document17 pagesScience 9 Quarter 1 Week 3 Sim 4Rodel CamposoNo ratings yet
- S4 Mock 1 2006 Biology P1Document8 pagesS4 Mock 1 2006 Biology P1cyber sec100% (1)
- 2022 Springer Nature Fully Open Access JournalsDocument36 pages2022 Springer Nature Fully Open Access JournalsEntertainment HubNo ratings yet
- Miscellaneous Blood GroupsDocument4 pagesMiscellaneous Blood GroupsIan Leo SantosNo ratings yet
- Self-Healing DNA Nanostructures - American Chemical SocietyDocument3 pagesSelf-Healing DNA Nanostructures - American Chemical Societydanutzza90No ratings yet
- 2010 Goh Vulnera - EngDocument5 pages2010 Goh Vulnera - EngFernandoCedroNo ratings yet
- 10.1007@s00216 019 02113 5Document10 pages10.1007@s00216 019 02113 5habib diopNo ratings yet
- Streptomicina - Streptomyces Griseus.Document16 pagesStreptomicina - Streptomyces Griseus.Adonai Lemus GarcíaNo ratings yet
- The Obsolescence of Formocresol: B. LewisDocument4 pagesThe Obsolescence of Formocresol: B. LewisAlan Vargas100% (1)
- ACTIVITY# 1 The Microscope: I. ObjectivesDocument9 pagesACTIVITY# 1 The Microscope: I. ObjectivesPatrick BugarinNo ratings yet
- Evolution of Temporomandibular Joint e A ReviewDocument8 pagesEvolution of Temporomandibular Joint e A ReviewsathyaNo ratings yet
- Zhao 2017Document10 pagesZhao 2017LUIS GIANFRANCO GONZALEZ ALVAREZNo ratings yet
- Cellular Injury and AdaptationDocument42 pagesCellular Injury and AdaptationSamuel fikaduNo ratings yet
- Unit 4Document34 pagesUnit 4adarshclash18No ratings yet
- EGCSE Biology 2021-2023 SyllabusDocument35 pagesEGCSE Biology 2021-2023 SyllabusANONY MOUSNo ratings yet
- Flavonoid Transport Mechanisms: How To Go, and With WhomDocument10 pagesFlavonoid Transport Mechanisms: How To Go, and With WhomDulceNo ratings yet
- CompelementDocument32 pagesCompelementMona AdamNo ratings yet
- EmbryologyDocument215 pagesEmbryologyMunewer AbdellaNo ratings yet