Professional Documents
Culture Documents
Lumasiran: An Investigational Rnai Therapeutic For Primary Hyperoxaluria Type 1 (Ph1)
Uploaded by
Muhammad HaneefOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lumasiran: An Investigational Rnai Therapeutic For Primary Hyperoxaluria Type 1 (Ph1)
Uploaded by
Muhammad HaneefCopyright:
Available Formats
Lumasiran
An investigational RNAi Therapeutic for Primary Hyperoxaluria Type 1 (PH1)
Overview
• Lumasiran (ALN-GO1) is an investigational, subcutaneously administered (under the skin)
RNA interference (RNAi) therapeutic targeting glycolate oxidase (GO) in development for the
treatment of primary hyperoxaluria type 1 (PH1).
• PH1 is a rare, life-threatening disease that can cause serious damage to kidneys and progressively
to other organs.1
• PH1 is characterized by the pathologic overproduction of oxalate by the liver. Oxalate is an end
product of metabolism that, when in excess, is toxic and accumulates in the kidneys forming
calcium oxalate crystals.1,2
• Symptoms of PH1 are often associated with recurrent kidney stones and include flank pain, urinary
tract infections, painful urination, and blood in the urine.2,3
• Currently, the only curative treatment is a liver transplant, to correct the metabolic defect,
combined with a kidney transplant, to replace the terminally damaged kidneys.1,3
Clinical Development
• The safety and efficacy of lumasiran are being evaluated in a randomized, double-blind,
placebo-controlled, global, multicenter Phase 3 study of approximately 30 PH1 patients,
called ILLUMINATE-A (NCT03681184).
• The primary endpoint is percent change in 24-hour urinary oxalate excretion from baseline to
Month 6.
• Key secondary and exploratory endpoints in ILLUMINATE-A will evaluate additional measures
of urinary oxalate, estimated glomerular filtration rate (eGFR), safety, and tolerability.
• Alnylam expects to report topline results in late 2019.
Regulatory Designations
• Breakthrough Therapy Designation by the U.S. Food and Drug Administration (FDA)
• Priority Medicines (PRIME) Designation from the European Medicines Agency (EMA)
• Orphan Drug Designations in both the U.S. and the European Union
For more information about lumasiran, please contact media@alnylam.com.
1.
Cochat P and Rumsby G. Primary hyperoxaluria. N Engl J Med. 2013;369:649-658.
2.
Milliner DS et al. GeneReviews®; [updated Nov 30, 2017]. https://www.ncbi.nlm.nih.gov/books/NBK1283/.
3.
Hoppe B, Beck BB, Milliner DS. The primary hyperoxalurias. Kidney Int. 2009, 75:1264-1271.
You might also like
- PTI Manifesto Final - 2018Document61 pagesPTI Manifesto Final - 2018Insaf.PK74% (47)
- Reading Test 01 - E2Lang PDFDocument25 pagesReading Test 01 - E2Lang PDFMuhammad Haneef100% (12)
- Reading Tests 1 15 PDFDocument342 pagesReading Tests 1 15 PDFMuhammad Haneef79% (14)
- Life Cycle Strategic PlanDocument78 pagesLife Cycle Strategic PlanTancheto111No ratings yet
- Pharmacogenomic and Pharmacogenetics - DIAN PDFDocument34 pagesPharmacogenomic and Pharmacogenetics - DIAN PDFfakultasfarmasiNo ratings yet
- Kitchen Tools & EquipmentDocument40 pagesKitchen Tools & EquipmentLymenson BoongalingNo ratings yet
- Biomonitoring of 5 Flourouracil - AnyDocument23 pagesBiomonitoring of 5 Flourouracil - AnyAgus TianyNo ratings yet
- Pharma Gujjjju IndiaDocument241 pagesPharma Gujjjju IndiaHarsh NimavatNo ratings yet
- Graves' Disease Case Report Links Severe Hypoalbuminemia to ThyrotoxicosisDocument2 pagesGraves' Disease Case Report Links Severe Hypoalbuminemia to ThyrotoxicosisAbdur Rachman Ba'abdullahNo ratings yet
- Farmacologia em Cães GeriátricosDocument12 pagesFarmacologia em Cães GeriátricosRafaela RodriguesNo ratings yet
- Drug Target Pharmacogenomics Lecture: Transporters and ResponseDocument27 pagesDrug Target Pharmacogenomics Lecture: Transporters and ResponseNemer EzzeddineNo ratings yet
- 10 1089@cap 2016 0178Document2 pages10 1089@cap 2016 0178Maria Helena Pedraza MNo ratings yet
- Nihms 119383Document18 pagesNihms 119383Aya AhmedNo ratings yet
- CURCUMINpdfDocument7 pagesCURCUMINpdfDede MulyamanNo ratings yet
- Ni Hms 494512Document14 pagesNi Hms 494512Carolina Duque RodriguezNo ratings yet
- Efficacy of Oral Lycopene in The Treatment of Oral LeukoplakiaDocument6 pagesEfficacy of Oral Lycopene in The Treatment of Oral Leukoplakia2211801733No ratings yet
- 2015 Article 20Document5 pages2015 Article 20anaNo ratings yet
- Lumasiran Expanding The Treatment Options For Patients With Primary Hyperoxaluria Type 1Document11 pagesLumasiran Expanding The Treatment Options For Patients With Primary Hyperoxaluria Type 1NishantNo ratings yet
- Pleasant: 90 Letters TO Editors Br. J. Pharinac. (1 9 78), 5Document2 pagesPleasant: 90 Letters TO Editors Br. J. Pharinac. (1 9 78), 5DesalegnNo ratings yet
- The Effects of Andrographis Paniculata (Burm.f.) Nees On The Pharmacokinetics and Pharmacodynamics of Midazolam in Healthy VolunteersDocument7 pagesThe Effects of Andrographis Paniculata (Burm.f.) Nees On The Pharmacokinetics and Pharmacodynamics of Midazolam in Healthy VolunteersAdquinta Wulandini PutriNo ratings yet
- Dr. Taslim Poniman, SPB-KBDDocument21 pagesDr. Taslim Poniman, SPB-KBDThomas PatrisNo ratings yet
- Gout Management GuideDocument3 pagesGout Management GuideamyrahnurulNo ratings yet
- Alicaforsen For The Treatment of Inflammatory Bowel DiseaseDocument25 pagesAlicaforsen For The Treatment of Inflammatory Bowel Diseaseinfinity TangNo ratings yet
- PredictingAllopurinolResponse in Patient With Gout 2015Document13 pagesPredictingAllopurinolResponse in Patient With Gout 2015นันทสิทธิ์ ศิริวิชญ์ไมตรีNo ratings yet
- Hepatology - April 1993 - Mendenhall - A Study of Oral Nutritional Support With Oxandrolone in Malnourished Patients WithDocument13 pagesHepatology - April 1993 - Mendenhall - A Study of Oral Nutritional Support With Oxandrolone in Malnourished Patients WithkentryzbustamanteNo ratings yet
- fphar-14-1260599Document11 pagesfphar-14-1260599mimi.mca.1921No ratings yet
- Br. J. Cancer 93, 876-883 (2005) .Document8 pagesBr. J. Cancer 93, 876-883 (2005) .hardevNo ratings yet
- Ibuprofen Toxicosis in Dogs, Cats, and Ferrets: Toxicology BriefDocument4 pagesIbuprofen Toxicosis in Dogs, Cats, and Ferrets: Toxicology BriefChan TawasilNo ratings yet
- Febuxostat (Uloric) - A Xanthine Oxidase Inhibitor - Aug 1, 2023Document24 pagesFebuxostat (Uloric) - A Xanthine Oxidase Inhibitor - Aug 1, 2023Ramdas BorhadeNo ratings yet
- Clinical PharmacologDocument81 pagesClinical PharmacologSHILOTANo ratings yet
- Pharmacokinetics and pharmacodynamics of anaesthetic drugs in paediatricsDocument7 pagesPharmacokinetics and pharmacodynamics of anaesthetic drugs in paediatricsR KNo ratings yet
- BLOK 12 - IT 2 - Farmakogenetik 1 - MISDocument38 pagesBLOK 12 - IT 2 - Farmakogenetik 1 - MISMuhammad AdilNo ratings yet
- We Recommend Not Using Recombinant Human (RH) IGF-1 To Prevent or Treat AKIDocument6 pagesWe Recommend Not Using Recombinant Human (RH) IGF-1 To Prevent or Treat AKIMarilya ChandraNo ratings yet
- Philippine Clinical Practice Guidelines For The Management of Gout 2008Document7 pagesPhilippine Clinical Practice Guidelines For The Management of Gout 2008JedNo ratings yet
- DILIDocument28 pagesDILIsepti nurhidayatiNo ratings yet
- Antineoplastic AgentsDocument83 pagesAntineoplastic AgentsDwynwen Aleaume GumapacNo ratings yet
- Anti-Diabetic Effects of Mani-Manian LeavesDocument7 pagesAnti-Diabetic Effects of Mani-Manian Leaveselieza salvadorNo ratings yet
- Efficacy and Safety of MerivaRDocument8 pagesEfficacy and Safety of MerivaRmazsamNo ratings yet
- Pre AnaestheticsDocument69 pagesPre AnaestheticsPraney SlathiaNo ratings yet
- Clinical Nutrition ESPEN: Hiroshige Itakura, Michie Kobayashi, Seiji NakamuraDocument7 pagesClinical Nutrition ESPEN: Hiroshige Itakura, Michie Kobayashi, Seiji NakamuraPáblo EugênioNo ratings yet
- How To Practice Environmental Medicine: The Path AheadDocument8 pagesHow To Practice Environmental Medicine: The Path AheadFabian VolpeNo ratings yet
- Review of metformin evidence for PCOS highlights modest benefitsDocument8 pagesReview of metformin evidence for PCOS highlights modest benefitsNur WahyuniNo ratings yet
- Anti-Diabetic Effect of Flacourtia Jangomas ExtractDocument7 pagesAnti-Diabetic Effect of Flacourtia Jangomas ExtractREMAN ALINGASANo ratings yet
- Pharmacokinetic Interaction Between Fluoxetine and Omeprazole in Healthy Male Volunteers: A Prospective Pilot StudyDocument9 pagesPharmacokinetic Interaction Between Fluoxetine and Omeprazole in Healthy Male Volunteers: A Prospective Pilot StudyCurcubeuAuroraNo ratings yet
- Renal and non renal extretion of drugs, Unit IIDocument12 pagesRenal and non renal extretion of drugs, Unit IIVarshaNo ratings yet
- Mechanisms and Treatment of Anorexia in Hemodialysis PatientsDocument8 pagesMechanisms and Treatment of Anorexia in Hemodialysis PatientsnettoxsNo ratings yet
- Articles: Spironolactone Management of Resistant HypertensionDocument8 pagesArticles: Spironolactone Management of Resistant HypertensionKatherine America Camac DelgadoNo ratings yet
- 23 Ifteni Tit Rápida 1 Acta - Psychiatrica - Scandinavica - 2014 - 130 - (1) - 25Document5 pages23 Ifteni Tit Rápida 1 Acta - Psychiatrica - Scandinavica - 2014 - 130 - (1) - 25observacionfray23No ratings yet
- Antioxidants 09 00950 v2Document20 pagesAntioxidants 09 00950 v2EmirgibraltarNo ratings yet
- Clinical Trials of Biotechnology ProductsDocument8 pagesClinical Trials of Biotechnology Productsokonkwommesoma176No ratings yet
- Carditone Herb Clinical StudyDocument8 pagesCarditone Herb Clinical StudyDr Sreedhar TirunagariNo ratings yet
- 26 Manjula Devi - Docx CorrectedDocument11 pages26 Manjula Devi - Docx Correctednoviantyramadhani12No ratings yet
- PharmacokineticsDocument34 pagesPharmacokineticsAbdelrahman GalalNo ratings yet
- Effectiveness of Interleukin-1 Receptor Antagonist (Anakinra) On Cerulein-Induced Experimental Acute Pancreatitis in RatsDocument8 pagesEffectiveness of Interleukin-1 Receptor Antagonist (Anakinra) On Cerulein-Induced Experimental Acute Pancreatitis in RatsmattpauziNo ratings yet
- BIC 409 - Factors Affecting Drug MetabolismDocument29 pagesBIC 409 - Factors Affecting Drug MetabolismIbraheem BashirNo ratings yet
- Drug Interaction 2Document28 pagesDrug Interaction 2Dixit LanghnejaNo ratings yet
- Olanzapine For Nausea and VomitingDocument42 pagesOlanzapine For Nausea and Vomitingsitiradziah subariNo ratings yet
- Gout CPG Manuscript - PJIM 072808Document16 pagesGout CPG Manuscript - PJIM 072808Francis CastellNo ratings yet
- Laporan MRDocument6 pagesLaporan MRParahmitaNo ratings yet
- Ginger and 6-Shogaol Protect Intestinal Tight Junction and Enteric Dopaminergic Neurons Against 1-Methyl-4-Phenyl 1,2,3,6-Tetrahydropyridine in MiceDocument11 pagesGinger and 6-Shogaol Protect Intestinal Tight Junction and Enteric Dopaminergic Neurons Against 1-Methyl-4-Phenyl 1,2,3,6-Tetrahydropyridine in MiceTram Anh NguyenNo ratings yet
- Evaluation of Fresh Frozen Plasma Administration in Dogs With Pancreatitis: 77 Cases (1995 2005)Document6 pagesEvaluation of Fresh Frozen Plasma Administration in Dogs With Pancreatitis: 77 Cases (1995 2005)soledadDC329No ratings yet
- PPI Role Laryngopharyngeal RefluxDocument5 pagesPPI Role Laryngopharyngeal RefluxROBINSON ELIOTT GONZ�LEZ P�EZNo ratings yet
- GotaDocument17 pagesGotaAtelos EctasiaNo ratings yet
- Histopathology of Preclinical Toxicity Studies: Interpretation and Relevance in Drug Safety EvaluationFrom EverandHistopathology of Preclinical Toxicity Studies: Interpretation and Relevance in Drug Safety EvaluationNo ratings yet
- Writing Sample Pages-1Document2 pagesWriting Sample Pages-1Muhammad HaneefNo ratings yet
- December 2018.docx 1Document2 pagesDecember 2018.docx 1Muhammad HaneefNo ratings yet
- Colon LettersDocument4 pagesColon LettersMuhammad HaneefNo ratings yet
- SaudiJKidneyDisTranspl2751026-1401396 035333Document3 pagesSaudiJKidneyDisTranspl2751026-1401396 035333Muhammad HaneefNo ratings yet
- Writing Sample Pages-3Document2 pagesWriting Sample Pages-3Muhammad HaneefNo ratings yet
- KDIGO Gitelman Conf ReportDocument10 pagesKDIGO Gitelman Conf Reportfelix tanzilNo ratings yet
- This Is An Electronic Report & Not: To Be Used For Any Legal PurposesDocument1 pageThis Is An Electronic Report & Not: To Be Used For Any Legal PurposesMuhammad HaneefNo ratings yet
- ESR Test Report Under 40 CharactersDocument1 pageESR Test Report Under 40 CharactersMuhammad HaneefNo ratings yet
- Writing January 2019 PDFDocument2 pagesWriting January 2019 PDFNirmala PNo ratings yet
- Folic Acid During COVID-19Document4 pagesFolic Acid During COVID-19Muhammad HaneefNo ratings yet
- Unlicensed-Teaching Colleagues-4CKD-17, May, 2016Document36 pagesUnlicensed-Teaching Colleagues-4CKD-17, May, 2016Muhammad HaneefNo ratings yet
- Plasma Potassium Response To Acute Respiratory AlkalosisDocument8 pagesPlasma Potassium Response To Acute Respiratory AlkalosisMuhammad HaneefNo ratings yet
- Medical Record for Uzair Khan from MultanDocument1 pageMedical Record for Uzair Khan from MultanMuhammad HaneefNo ratings yet
- Arteriovenous Fistula Care GuideDocument29 pagesArteriovenous Fistula Care GuideMuhammad HaneefNo ratings yet
- Ophthalmology Notes 2015Document27 pagesOphthalmology Notes 2015Muhammad HaneefNo ratings yet
- Unlicensed-DIALYSIS ADEQUACY PDFDocument56 pagesUnlicensed-DIALYSIS ADEQUACY PDFMuhammad HaneefNo ratings yet
- Document From Kasfatmostafa57 PDFDocument12 pagesDocument From Kasfatmostafa57 PDFMuhammad HaneefNo ratings yet
- Document From Kasfatmostafa57 PDFDocument12 pagesDocument From Kasfatmostafa57 PDFMuhammad HaneefNo ratings yet
- PMDC Code of EthicsDocument26 pagesPMDC Code of EthicsFahad QiamNo ratings yet
- 0007 Oncology Notes 2015 PDFDocument26 pages0007 Oncology Notes 2015 PDFchandanNo ratings yet
- 443418Document7 pages443418Muhammad HaneefNo ratings yet
- MRCP 2 Nephrology NOTESDocument74 pagesMRCP 2 Nephrology NOTESMuhammad HaneefNo ratings yet
- Chemical Bonding Multiple ChoiceDocument13 pagesChemical Bonding Multiple ChoiceMuhammad HaneefNo ratings yet
- Psychiatry Notes 2015Document34 pagesPsychiatry Notes 2015Muhammad HaneefNo ratings yet
- 0009 Rheumatology Notes 2015 PDFDocument56 pages0009 Rheumatology Notes 2015 PDFMuhammad HaneefNo ratings yet
- Neurology Passmedicine & Onexamination Notes 2016Document158 pagesNeurology Passmedicine & Onexamination Notes 2016Muhammad Haneef100% (2)
- Tracing Chronic Fatigue Syndrome Tsfunction Is Key To ME - CFS - B Day PDFDocument91 pagesTracing Chronic Fatigue Syndrome Tsfunction Is Key To ME - CFS - B Day PDFsanthigiNo ratings yet
- GPSForex Robot V2 User GuideDocument40 pagesGPSForex Robot V2 User GuideMiguel Angel PerezNo ratings yet
- C++ Classes and ObjectsDocument4 pagesC++ Classes and ObjectsAll TvwnzNo ratings yet
- Paper 1R MSDocument25 pagesPaper 1R MSAkashNo ratings yet
- Percent CompositionDocument4 pagesPercent CompositionTshiamo MotaungNo ratings yet
- Chap 7Document35 pagesChap 7Nizar TayemNo ratings yet
- TENSION PNEUMOTHORAX (Malav Shah)Document66 pagesTENSION PNEUMOTHORAX (Malav Shah)Sharath PsNo ratings yet
- Insurance - Unit 3&4Document20 pagesInsurance - Unit 3&4Dhruv GandhiNo ratings yet
- The Teacher and Student Relationship of Haydn and BeethovenDocument10 pagesThe Teacher and Student Relationship of Haydn and BeethovenVinny MuscarellaNo ratings yet
- Improving PerformanceDocument2 pagesImproving PerformanceYidne MasreshaNo ratings yet
- Unit 1Document32 pagesUnit 1Viyat RupaparaNo ratings yet
- S/4HANA Margin Analysis, Predictive Accounting, and Continuous CloseDocument27 pagesS/4HANA Margin Analysis, Predictive Accounting, and Continuous Closessbhagat001No ratings yet
- PEC ReviewerDocument17 pagesPEC ReviewerJunallyn ManigbasNo ratings yet
- DCM300E Clamp Meter Measures Earth Leakage CurrentDocument2 pagesDCM300E Clamp Meter Measures Earth Leakage CurrentKatamba RogersNo ratings yet
- Project Management Remote ExamDocument4 pagesProject Management Remote ExamAnis MehrabNo ratings yet
- Epimastic 7200: Product DescriptionDocument2 pagesEpimastic 7200: Product DescriptionSu KaNo ratings yet
- Belt Weigh FeederDocument808 pagesBelt Weigh FeedersatfasNo ratings yet
- 1025 (1029) Anaerobic ChamberDocument8 pages1025 (1029) Anaerobic ChamberSoma GhoshNo ratings yet
- Effecta WoodyDocument21 pagesEffecta WoodyMR XNo ratings yet
- School Annual Data For Financial YearDocument3 pagesSchool Annual Data For Financial YearRamesh Singh100% (1)
- Anatolii PapanovDocument8 pagesAnatolii PapanovKyrademNo ratings yet
- Future Developments in Management AccountingDocument4 pagesFuture Developments in Management AccountingAmar narayanNo ratings yet
- Solar Bloc DatasheetDocument2 pagesSolar Bloc DatasheetandresNo ratings yet
- ADC0804 Datasheet - ADC 0804 Pin Diagram & Description - EngineersGarageDocument3 pagesADC0804 Datasheet - ADC 0804 Pin Diagram & Description - EngineersGarageMehanathan Maggie MikeyNo ratings yet
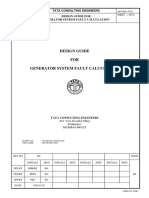
- Generator System Fault Calculation Design GuideDocument22 pagesGenerator System Fault Calculation Design Guidedheerajdorlikar100% (2)
- CH9-Diversification and AcquisitionsDocument9 pagesCH9-Diversification and AcquisitionsVincent LeruthNo ratings yet
- 5.1 Quadratic Functions: 344 Learning ObjectivesDocument15 pages5.1 Quadratic Functions: 344 Learning ObjectiveskhadijaNo ratings yet
- Underwater FHPP Welding of Steel Sleeve JointsDocument10 pagesUnderwater FHPP Welding of Steel Sleeve JointsMohsen KeramatiNo ratings yet
- Guided Noteboo Kin GED10 2 (Mathe Matics in The Modern World)Document5 pagesGuided Noteboo Kin GED10 2 (Mathe Matics in The Modern World)Aaronie DeguNo ratings yet