Professional Documents
Culture Documents
Medical History Form 2020 - College
Uploaded by
Apple Gee Libo-onOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medical History Form 2020 - College
Uploaded by
Apple Gee Libo-onCopyright:
Available Formats
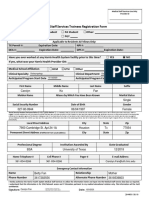
SILLIMAN UNIVERSITY CLINIC
COLLEGE STUDENT’S MEDICAL HISTORY FORM
Name: ________________________________________________________ Age: _______ Sex: _________
Address: ______________________________________________________ Contact No.: ______________________
Birthdate: ________________ Citizenship: _____________________ Religion: ________________________
Father’s Name: _______________________________ Mother’s Name: ______________________________________
Contact person in case of emergency: ________________________________ Contact No.: _____________________
Spouse (if married): _____________________________________________
PAST MEDICAL HISTORY
General Condition for the past year: ____________________________________________________________________
ILLNESS NO YES YEAR ILLNESS NO YES YEAR
Allergy Heart Disorder
Anemia Hyperacidity
Asthma Indigestion
Behavioral Problem Insomnia
Bleeding Problem Kidney Problem
Blood Abnormality Liver Problem
Chickenpox Measles
Convulsion Mumps
Dengue Parasitism
Diabetes Pneumonia
Ear Problem Primary Complex
Eating Disorder Scoliosis
Epilepsy Skin Problem
Eye Problem Tonsillitis
Fracture Typhoid Fever
Hearing Problem Vision Defect
Others Others
Any history of hospitalization or surgical operation (Yes/No, specify)? ________________________________________
__________________________________________________________________________________________________
Special Medical Concerns: ____________________________________________________________________________
Any FOOD Allergies? _______________________________ Any DRUG Allergies? ____________________________
IMMUNIZATION RECORD
VACCINES NO YES VACCINES NO YES
BCG Chicken pox
OPV Hepatitis A
DPT / Td / T.T. Hepatitis B
Measles Others (Pls. Specify)
MMR (measles, mumps, rubella)
FOR FEMALES
Age of First Menstruation: _____ Days of Dysmenorrhea: _____
Is it Regular (Monthly)? _______ Duration of Menses: ________
If irregular, pls. indicate the month interval and medications taken: _____________________________________
FOR MATERNAL/OBSTETRICAL HISTORY (for women only)
First Sexual contact (Age) : ___________
Gravida (no. of times pregnant) : _______
Parity (no. of times you gave birth): ______
Full Term: _____ Abortion/Miscarriage: _____ Pre Term: _____ Children currently living: _____
Year of Pap Smear done: _________________ Cervical Immunization: ____________________
Hormonal Medications Maintained: ________________________________________________________
Reason for taking: ____________________________________________________________________
Please check and indicate how many times per week
__________ coffee drinker __________ smoker __________ sexually active
__________ alcohol drinker __________ illicit drug use (pls. specify)
FAMILY HISTORY
DISEASE NO YES RELATION(S) TO STUDENT
Asthma
Bleeding tendency
Cancer
Diabetes
Heart Disorder
High Blood Pressure
Kidney Problem
Mental Disorder
Obesity
Seizure Disorder
Stroke
Thyroid Problem
Tuberculosis
Others (pls. specify)
Is your house screened? ________________________________________
What is your source of potable water? _____________________________
PHYSICIAN’S REPORT
Name : _________________________________________________________
General Appearance:
Excellent _______ Good _______ Fair ______ Poor _______
Vital Signs
BP _______ RR _______ PR _______ T ______ Ht _______ Wt _______ BMI _______
Any health issues today? _____________________________________________________________________________
Skin / Lesions : ________________________________ Gynecologic Findings / Abnormalities :
Head/Scalp : __________________________________ _____________________________________________
Eyes, Visions, and Other conditions : _______________ ____________________
Ears, Hearing, and Other condition:_________________ Back and Posture : _____________________________
Nose, Nasal passage, and sinuses : _________________ Extremities : __________________________________
Mouth, Pharynx : _______________________________ Nervous System :
Neck, Thyroid, Cervical Lymph Nodes : ____________ Cranial nerves : _________________________
Chest and Lungs : ______________________________ Motor : _______________________________
Breast and Axilla : ______________________________ Sensory : ______________________________
Cardiovascular : ________________________________ Reflexes : _____________________________
Abdomen : ____________________________________ MSE:_______________________________________
Genitourinary Tract : ____________________________
Results of required tests: CBC _________________________________
Chest X-ray ____________________________
Urinalysis______________________________
Recommendations: __________________________________________________________________________________
__________________________________
Physician’s Name & Signature
License Number: _______________
Date: ________________________
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Human Biology 1607118109. - PrintDocument1,724 pagesHuman Biology 1607118109. - PrintI100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Facts: Vergara Vs People GR No. 160328 February 4, 2005Document2 pagesFacts: Vergara Vs People GR No. 160328 February 4, 2005Apple Gee Libo-onNo ratings yet
- Ang Nars Partylist V Exec SecDocument3 pagesAng Nars Partylist V Exec SecApple Gee Libo-onNo ratings yet
- JBJBDocument116 pagesJBJBk.saikumarNo ratings yet
- CiceroDocument12 pagesCiceroApple Gee Libo-onNo ratings yet
- Drug Study MMRDocument2 pagesDrug Study MMRErika Marie Calucab100% (2)
- Criminal Law Case DigestDocument3 pagesCriminal Law Case DigestApple Gee Libo-onNo ratings yet
- DEF Complainant FINALDocument6 pagesDEF Complainant FINALApple Gee Libo-onNo ratings yet
- Facts: Republic Vs Eugenio GR No. 174629 February 14, 2008Document2 pagesFacts: Republic Vs Eugenio GR No. 174629 February 14, 2008Apple Gee Libo-onNo ratings yet
- GR 113213 - Wright V Court of AppealsDocument1 pageGR 113213 - Wright V Court of AppealsApple Gee Libo-on100% (1)
- Petitioners: La Bugal-B'Laan Tribal Association Inc, Rep. Chariman F'Long Miguel Lumayong Etc Respondent: Secretary Victor O. Ramos, DENR EtcDocument2 pagesPetitioners: La Bugal-B'Laan Tribal Association Inc, Rep. Chariman F'Long Miguel Lumayong Etc Respondent: Secretary Victor O. Ramos, DENR EtcApple Gee Libo-onNo ratings yet
- CaseDocument43 pagesCaseApple Gee Libo-onNo ratings yet
- Kant'S Legal Philosophy: Group 6Document30 pagesKant'S Legal Philosophy: Group 6Apple Gee Libo-onNo ratings yet
- Name: Teacher: Date: Score:: Word ProblemsDocument2 pagesName: Teacher: Date: Score:: Word ProblemsApple Gee Libo-onNo ratings yet
- Knowledge, Attitude and Practice of Mothers Toward Children's Obligatory VaccinationDocument7 pagesKnowledge, Attitude and Practice of Mothers Toward Children's Obligatory VaccinationkrishnasreeNo ratings yet
- With Help From Lisa Evers, RN, BSN, CWO4)Document20 pagesWith Help From Lisa Evers, RN, BSN, CWO4)jbmowerNo ratings yet
- Community Health NursingDocument4 pagesCommunity Health NursingKirstin del CarmenNo ratings yet
- Application Form For Romania 2019Document7 pagesApplication Form For Romania 2019darkangelNo ratings yet
- Immunization in New BornDocument5 pagesImmunization in New BornRose Lyn Camarista VelascoNo ratings yet
- Travel VaccinationsDocument3 pagesTravel VaccinationsOlive Health Travel ClinicNo ratings yet
- Chapter 41: The Child With An Infectious Disease Test Bank: Multiple ChoiceDocument10 pagesChapter 41: The Child With An Infectious Disease Test Bank: Multiple ChoiceNurse UtopiaNo ratings yet
- Vaccination ChartDocument3 pagesVaccination ChartszawNo ratings yet
- Parent Ver SCH 0 6yrsDocument2 pagesParent Ver SCH 0 6yrsSrinivasamurthy KamarthiNo ratings yet
- Harris Health Trainees Registration Packet (10!8!19)Document8 pagesHarris Health Trainees Registration Packet (10!8!19)Carolyn FanNo ratings yet
- White Paper Measles AIM v1.9Document40 pagesWhite Paper Measles AIM v1.9rush999No ratings yet
- MMRDocument2 pagesMMRShrinivas YuvanNo ratings yet
- Grade 10 Summative TestDocument4 pagesGrade 10 Summative TestJaymar B. MagtibayNo ratings yet
- Merged File - HLTH 101Document14 pagesMerged File - HLTH 101Harshana Sandaruwan SomarathneNo ratings yet
- Autism - Kopie PDFDocument214 pagesAutism - Kopie PDFMohrscribdNo ratings yet
- Activity 1-13 StudentDocument3 pagesActivity 1-13 StudentTian KevinNo ratings yet
- Longer Authorised: Annex I Summary of Product CharacteristicsDocument28 pagesLonger Authorised: Annex I Summary of Product CharacteristicsEllaNo ratings yet
- Dd/Mm/Yyyy Dd/Mm/Yyyy Dd/Mm/YyyyDocument6 pagesDd/Mm/Yyyy Dd/Mm/Yyyy Dd/Mm/YyyyJohn50% (2)
- What Is Mumps in ChildrenDocument4 pagesWhat Is Mumps in ChildrenFoster K KaundaNo ratings yet
- 4ec1 01r Rms 20220825Document21 pages4ec1 01r Rms 20220825Mark PrincelyNo ratings yet
- Preventive Pediatrics Part 1Document6 pagesPreventive Pediatrics Part 1mkct111No ratings yet
- CHN TP ReviewDocument40 pagesCHN TP ReviewPatrick Jon LumaghanNo ratings yet
- NSW Immunisation ScheduleDocument1 pageNSW Immunisation ScheduleKristinaNo ratings yet
- ImmunisationDocument58 pagesImmunisationBharatBGNo ratings yet
- RubellaDocument10 pagesRubellaKiran Kumar100% (1)
- Final Research Paper 1 Enc 1102 Tamryn Webb-GurleyDocument11 pagesFinal Research Paper 1 Enc 1102 Tamryn Webb-Gurleyapi-490436143100% (1)
- Mediplus: 2019 Benefit GuideDocument24 pagesMediplus: 2019 Benefit GuideBruce FerreiraNo ratings yet