Professional Documents
Culture Documents
Ellis - 2018 - Assessment and Management of Posttraumatic Stress Disorder - Revisión
Ellis - 2018 - Assessment and Management of Posttraumatic Stress Disorder - Revisión
Uploaded by
Emmanuel Domínguez RosalesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ellis - 2018 - Assessment and Management of Posttraumatic Stress Disorder - Revisión
Ellis - 2018 - Assessment and Management of Posttraumatic Stress Disorder - Revisión
Uploaded by
Emmanuel Domínguez RosalesCopyright:
Available Formats
Assessment REVIEW ARTICLE
and Management of C O N T I N U UM A U D I O
I NT E R V I E W A V A I L AB L E
ONLINE
Posttraumatic Stress
Disorder S U P P L E M E N T A L D I G I T AL
C O N T E NT ( S D C )
A V AI L A B L E O N L I N E
By Janet Ellis, MBBChir, MD, FRCPC; Ari Zaretsky, MD, FRCPC
ABSTRACT
PURPOSE: The goal of this article is to increase clinicians’ understanding of
posttraumatic stress disorder (PTSD) and improve skills in assessing risk for
and diagnosing PTSD. The importance and sequelae of lifetime trauma
burden are discussed, with reference to trends in prevention, early
intervention, and treatment.
RECENT FINDINGS: PTSD has different clinical phenotypes, which are
reflected in the changes in Diagnostic and Statistical Manual of Mental
Disorders, Fifth Edition (DSM-5) criteria. PTSD is almost always
complicated by comorbidity. Treatment requires a multimodal approach,
usually including medication, different therapeutic techniques, and
management of comorbidity. Interest is growing in the neurobiology of
childhood survivors of trauma, intergenerational transmission of trauma,
and long-term impact of trauma on physical health. Mitigation of the risk of
PTSD pretrauma in the military and first responders is gaining momentum,
given concerns about the cost and disability associated with PTSD. Interest
is also growing in screening for PTSD in medical populations, with evidence
of improved clinical outcomes. Preliminary research supports the
treatment of PTSD with repetitive transcranial magnetic stimulation. CITE AS:
CONTINUUM (MINNEAP MINN)
SUMMARY: PTSD is a trauma-related disorder with features of fear and 2018;24(3, BEHAVIORAL NEUROLOGY
AND PSYCHIATRY):873–892.
negative thinking about the trauma and the future. Untreated, it leads to
ongoing disruption of life due to avoidance, impaired vocational and social Address correspondence to
functioning, and other symptoms, depending on the phenotype. Despite a Dr Janet Ellis, 2075 Bayview Ave,
theoretical understanding of underlying mechanisms, PTSD remains Toronto, Ontario M4N 3M5,
Canada, janet.ellis@
challenging to treat, although evidence exists for benefit of pharmacologic sunnybrook.ca.
agents and trauma-focused therapies. A need still remains for treatments
that are more effective and efficient, with faster onset. RELATIONSHIP DISCLOSURE:
Drs Ellis and Zaretsky report no
disclosures.
INTRODUCTION UNLABELED USE OF
W
PRODUCTS/INVESTIGATIONAL
itnessed or experienced traumatic events may include war, USE DISCLOSURE:
violence, natural disaster, acute physical trauma, unexpected Drs Ellis and Zaretsky report
or unnatural death of a loved one, bullying, and physical no disclosures.
illness. Most people will have some symptoms of acute stress © 2018 American Academy
disorder after a traumatic event, but most will recover. of Neurology.
CONTINUUMJOURNAL.COM 873
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
POSTTRAUMATIC STRESS DISORDER
Posttraumatic stress disorder (PTSD) is a trauma-related syndrome of chronic
distress, with dissociative features, including reexperiencing of the trauma, mood
and cognitive changes, hyperarousal, and avoidance.1 It is associated with personal
chaos; an impaired sense of cohesion; distress; withdrawal from hobbies, work,
and social activities; a poor quality of life; and increased health care utilization.
EPIDEMIOLOGY
Between 10% and 50% of people who have had exposure to a life-threatening
trauma will develop persisting symptoms of PTSD.2,3 The lifetime prevalence of
PTSD varies by the diagnostic system used, gender, country, culture, values, and
exposure to war or crime-related trauma.4 While more exposure to trauma occurs
in lower-income countries compared to higher-income countries, the prevalence
of PTSD is fairly consistent, possibly implying a capacity to adapt to a level of
expected trauma. The exception to this is in postconflict zones, where the prevalence
of PTSD is highest,5 highlighting the increased risk of PTSD with interpersonal
violence. A 2013 study found that 89.7% of 2953 US adults had exposure to at least one
traumatic event and that exposure to multiple traumatic events was the norm.6 A
2017 systematic review of over 7 million primary care patients found a median
point prevalence of PTSD of 12.5% and of 24.5% across studies in veterans.7
Wittchen and colleagues8 found a range of lifetime prevalence of 0.56% to 6.67%
across European countries, with the highest prevalence in Croatia.
CONSEQUENCES OF POSTTRAUMATIC STRESS DISORDER
Exposure to a traumatic event and the duration of PTSD increase the risk
of developing chronic physical conditions, emphasizing the importance of
prevention and intervention.9 An increased risk of hypertension, ischemic heart
disease, obesity, and dementia has been found in those with a high lifetime
burden of trauma.10 Some emerging evidence indicates that overall trauma load
and PTSD increase the risk of later-life cognitive decline.11 PTSD and depression
are strongly associated, and both should be treated to improve outcome. Eating
disorders are another common comorbidity, with reported trauma rates and
PTSD varying from 12% to 45%.12,13
DIAGNOSIS
Since some of the symptoms of PTSD are outside usual experience and,
furthermore, patients are generally not forthcoming about their symptoms
owing to avoidance, it is especially important for clinicians to become familiar
with and understand the diagnostic criteria and experience of PTSD. The
overriding experience of PTSD is that of living in fear and avoidance of
trauma-related triggers.
It is vital to recognize PTSD symptoms before planning treatment for any
mental health issue after a traumatic event. It is important to assess for PTSD
without inadvertently causing repeated trauma. Simply asking the patient to
recount the trauma may lead to a dissociative flashback, distress, shutdown of
any further history, a rupture in the therapeutic relationship, and possibly refusal
to return to treatment. A traumatic event should lead a clinician to conduct a
focused screen for further vulnerability and relevant diagnostic criteria in a
deliberate probe for symptoms rather than asking the patient to recount the trauma.
Patients may require stabilization; out-of-control substance use, unstable
living situation, and untreated comorbidity should all be addressed as much as
874 JUNE 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
possible before starting active trauma therapy. The patient needs to develop KEY POINTS
skills in self-calming (breathing, visualization, or relaxation exercises when
● Posttraumatic stress
dysregulated) and grounding (the ability to reconnect with the present by disorder is a trauma-related
refocusing on sensory information in the present). After stabilization, specialized syndrome of chronic
parallel treatments for both PTSD and comorbid conditions (eg, depression, distress, reexperiencing the
anxiety, substance use) should be undertaken. trauma, dissociative
features with mood and
Pitfalls for clinicians when assessing patients with PTSD include
cognitive changes,
underestimating the distress or impact of the traumatic event (eg, the meaning or hyperarousal, and
subjective experience of a migraine14 or intensive care unit admission); failing avoidance.
to recognize the hidden face of PTSD in a complicated comorbid clinical picture;
and feeling frustrated with such patients as they are prone to unreliable ● Between 10% and 50%
of people who have
follow-up because of avoidance: “I’ll talk about anything else!” had exposure to a life-
PTSD is extremely disruptive to patients, who may not identify the problem as threatening trauma will
PTSD, simply believing that they are not coping. Patients with PTSD often say: develop persistent
“I do not know what this is, but I am not myself.” Many patients immediately symptoms of posttraumatic
stress disorder.
recognize the phrase “living in fear” as descriptive of how they feel, but they
generally do not put this into words themselves. The profound avoidance ● A traumatic event should
associated with PTSD can impact the therapeutic alliance, causing impatience in lead a clinician to conduct a
the clinician who may be faced with the paradox of a patient who is desperately focused screen for further
vulnerability and relevant
seeking help, yet misses appointments and does not follow through on taking
symptoms.
medications or doing homework.
● Pitfalls for clinicians
Identifying Those at Risk in the Clinical Environment when diagnosing patients
Health professionals often fail to recognize illness-related PTSD, apart from in with posttraumatic stress
disorder include
patients who have experienced acute physical trauma or burns. An increasing misdiagnosing the trauma
literature exists on the prevalence and impact of PTSD in patients with human (eg, underestimating the
immunodeficiency (HIV) and cancer and in patients who have experienced impact of an experience of a
childbirth or a stroke, been in intensive care, received an organ transplant, or had migraine or intensive care
unit admission) and failing to
cardiac surgery. recognize the hidden face of
PTSD is more likely to result from interpersonal violence than a natural posttraumatic stress
disaster.15 A higher risk of PTSD occurs with extended exposure to danger, disorder in a complicated
serious injury, dissociation during the event, or the loss of a loved one during the comorbid clinical picture.
traumatic event. The latter, if combined with PTSD, may result in an inability to
● Individual vulnerability to
grieve as the death is a reminder of the trauma.16 These survivors remain in posttraumatic stress
limbo, living in a hypervigilant fearful state with PTSD and without the capacity disorder includes a past
to deal with their complicated (avoided) grief, sometimes for years. Individual history of trauma, any
psychiatric disorder, and
vulnerability to PTSD includes a past history of trauma, any psychiatric disorder,
low social support.
and low social support. The way patients construe the cause of the trauma and
their posttrauma worldview should be carefully ascertained, since self-blame
(eg, “I should not have been walking in the dark”) and blanket negative
assumptions (eg, “I cannot keep myself safe,” “My life has been ruined by this
event”) predict and maintain PTSD.
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
Diagnostic Criteria
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth
Edition (DSM-5),17 a diagnosis of PTSD can only be made 1 month after exposure
to at least one traumatic event. PTSD may also have a delayed onset of 6 months
or more after the event. DSM-5 changed the classification of acute stress disorder
and PTSD from anxiety disorders to trauma-related disorders, reflecting that an
CONTINUUMJOURNAL.COM 875
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
POSTTRAUMATIC STRESS DISORDER
KEY POINTS external traumatic event is required for the illness to develop. A DSM-5 diagnosis
of PTSD includes seven specific criteria, including duration of at least 1 month
● When obtaining the
history, patients with
and functional impairment, an initial traumatic event, intrusive reexperiencing,
possible posttraumatic avoidance, numbing or negative alterations in cognition and mood, and
stress disorder should be alterations in arousal and reactivity (SDC 11-1; links.lww.com/CONT/A252).
asked about reexperiencing When obtaining the history, clinicians should ask the patient about the
the trauma through
following symptoms: reexperiencing (the trauma) through associated thoughts,
associated thoughts,
physiologic response, physiologic response, flashbacks, or nightmares; avoidance of trauma reminders;
flashbacks, or nightmares; loss of enjoyment; negative feelings or thinking; a sense of blame and isolation;
avoidance of trauma hyperarousal; irritability; poor sleep; tension; hypervigilance; and reactivity (more
reminders; loss of
highly emotional, less control of anger, possible self-destructive or aggressive
enjoyment; negative
feelings or thinking, a sense behavior). Avoidance can exhibit as an inability to leave the house for fear of
of blame and isolation; another assault or accident, not speaking with friends in case they ask about the
hyperarousal; irritability; traumatic event, or not being able to watch TV in case there is a trigger such as a
poor sleep; tension; motor vehicle accident. Common physiologic responses to trauma reminders
hypervigilance; and
reactivity. include increased heart and respiratory rate, sweating, nausea, and flushing. Patients
may also have significant features of dissociation, including feeling like an outside
● The different phenotypes observer or feeling detachment from self (depersonalization), or experiencing a
of posttraumatic stress sense of unreality, distance, or distortion of the external world (derealization). The
disorder make it more
difficult to recognize, and
addition of the dissociation subtype in DSM-5 describes acute PTSD and allows
symptoms may be masked what was previously informally called complex PTSD, a phenotype of PTSD
by comorbid substance use, from childhood trauma, to be diagnosed using the same criteria (SDC 11-1;
brain injury, depression, or links.lww.com/CONT/A252).18
anxiety disorder.
A flashback (as compared to the experience of a normal memory) is an
● Two phenotypes of involuntary dissociative episode. The patient temporarily involuntarily
posttraumatic stress reexperiences an aspect of the past traumatic event as if it were happening in the
disorder have been present (eg, smelling or tasting blood after being shot in the jaw or feeling
described, dysphoria and breathless with pain in the sternum after a steering wheel/airbag/seat-belt injury
emotional numbing, both
with reexperiencing, from a multivehicle accident). Once initiated, a flashback often continues
avoidance, and intrusively, as if the play button has been pressed for a horror movie.19 This
hyperarousal but differing in experience is cognitively disorganizing, often terrifying, and highly distressing.
sleep, irritability, and The clinical assessment of PTSD includes identifying events as traumatic and
concentration symptoms.
eliciting their significance, identifying the individual’s risk factors, and detecting
the signs of failure of recovery from the trauma. The different phenotypes of
PTSD make it more difficult to recognize, and symptoms may be masked by
comorbid substance use, brain injury, depression, or anxiety disorder.
PHENOTYPES OF POSTTRAUMATIC STRESS DISORDER
Two main phenotypes of PTSD have been described: dysphoria PTSD with
disrupted sleep and more dysphoric irritability, which often occurs after an acute
traumatic event as an adult (CASE 11-1), and complex PTSD from repeated
childhood trauma, often with an “emotionally numbed” presentation of PTSD
(CASE 11-2).21,22 Both phenotypes have reexperiencing, avoidance, and hyperarousal,
but they differ in sleep, irritability, and concentration symptoms (FIGURE 11-123).
QUESTIONNAIRES AND SCREENING TOOLS
A diagnosis of PTSD should not be made by self-report tools alone; clinical
assessment or clinician-administered semistructured interviews are needed to
confirm the diagnosis, such as the Structured Clinical Interview for DSM-5
(SCID-5)24 and the Clinician Administered PTSD Scale (CAPS).25 A 2005 review
876 JUNE 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
A 22-year-old woman presented for a new episode of psychiatric CASE 11-1
assessment and care with severe depression and posttraumatic stress
disorder (PTSD). Two years earlier, while walking home after an evening
lecture, she was sexually assaulted by a stranger, who held a knife to her
throat. A passerby took her to a police station, and a rape procedure was
conducted. The woman was in a shocked state and felt emotionally
numb. The next day, she began to experience intense fear and startle
reactions to loud sounds. She was unable to watch the news on television
or walk outside unaccompanied without fear, even during the day. She
experienced severe insomnia, nightmares of the rape, and daily flashbacks.
She became suicidally depressed, despite seeing a psychiatrist for
supportive psychotherapy and receiving an antidepressant over a 2-year
period. She was hospitalized twice and received 12 courses of bilateral
electroconvulsive therapy but remained depressed, with profound PTSD.
The patient began trauma-focused therapy with the psychiatrist in this
new episode of care. She was provided with psychoeducation about
trauma, PTSD and avoidance, and the rationale for imaginal and behavioral
exposure to feared memories and situations. She was treated with sertraline
150 mg once daily and risperidone 1 mg at night. Prazosin was carefully
titrated up to 2 mg to treat nightmares.20
The patient wrote out the major “chapters” of the rape memory narrative
to address them, with gradually increasing exposure to distressing details of
the rape both in her journal as well as in sessions. She was asked to recall
the experience as if it were happening in 90-minute taped imaginal exposure
sessions, in which she was asked to recount the trauma in sequence from
start to finish in as much detail as possible, in the present tense, while the
therapist aimed to keep her engaged within a moderate range of anxiety and
distress. This exposure therapy helped her to form a narrative and process
thoughts and emotions surrounding the event. She listened to the tapes
daily between sessions and recorded her subjective units of distress. In
parallel, she listed the things she avoided and began to deliberately expose
herself to these (objectively safe) situations, first accompanied, then alone.
After 6 months, the patient’s overt PTSD symptoms went into remission,
except for brief periods of high stress, and after 1 year, the prazosin was
discontinued. The patient was able to speak about the rape and reestablish
intimate relationships in her social and interpersonal life, but she was unable
to reestablish her chosen career track.
This case exemplifies the dysphoric, fear-based, hyperaroused adult after COMMENT
a single traumatic event, who also developed a severe depression
comorbid with the PTSD. Left untreated, most people with severe PTSD
will develop another psychiatric disorder. Like this woman, these patients
will mostly not recover until their PTSD is recognized and treated by
someone with PTSD expertise.
CONTINUUMJOURNAL.COM 877
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
POSTTRAUMATIC STRESS DISORDER
CASE 11-2 A 24-year-old man from Bosnia was referred for psychiatric assessment
while undergoing treatment for sarcoma, as he was missing oncology
appointments and had difficulty coping with his treatment because of
extreme anxiety and difficulty surrounding treatment decisions and side
effects. His childhood experience included an absent father, a mother
with an alcohol use disorder, and little routine. At age 12, he witnessed his
mother, two siblings, and others being killed outside their family home,
while he managed to keep hidden. He spontaneously recounted this story
during the consultation with a flat, disengaged affect.
His main symptoms were flat mood (with a loss of meaning in life and
little joy or positive emotion but no feelings of guilt or worthlessness),
decreased energy, and sense of hopelessness. He reported feeling
numb, shut down, and internally dysphoric. He did not startle easily and
reported good sleep but did not wake refreshed. He was not especially
irritable. He experienced flashbacks and nightmares, and he avoided
Bosnians and reminders of genocide. He did not seek psychiatric help
after he immigrated, because he could not bear to “open up” the
memories. He did not have hypervigilance but was disoriented and dazed
during flashbacks and for some of the day, especially after his cancer
diagnosis. Overall, his flat, dysphoric state could have been mistaken for
a sole diagnosis of depression but without a feeling of heaviness or guilt
to account for his lack of functioning. However, this was a shut-down,
flat, numbed presentation of comorbid depression and complex
posttraumatic stress disorder; he was difficult to access/engage,
preoccupied, and slow, with derealization.
Venlafaxine XR was begun and titrated up to 150 mg, and he was given
support with the logistics of making appointments and treatment
decisions. He was referred to a local specialized center for victims of
torture for trauma-focused therapy, processing, and eye movement
desensitization and reprocessing therapy to help with recovery from his
childhood trauma. He was seen for existential concerns at the cancer
center; he struggled to accept that something else had gone wrong in his
life, as if he were cursed. He completed treatment and eventually
returned to school. One year later, he was noted to be more animated and
engaged in conversation, able to withstand direct gaze, and present in the
moment. He said he felt better than he ever remembered feeling in his life.
COMMENT This case exemplifies the difficulty of adapting to new trauma in those with
complex posttraumatic stress disorder (PTSD) or childhood trauma. It also
demonstrates how easy it can be to misdiagnose PTSD as depression in this
type of shut-down, numbed presentation. All patients with significant
complex trauma will be at risk of an increase in symptoms or new
symptoms of PTSD when faced with serious medical illness or acute
physical trauma.
878 JUNE 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
concluded that the mean KEY POINTS
diagnostic efficiency of screening
● Patients having four or
tools was over 85% and that more categories of
using a small number of core childhood trauma had a 4 to
symptoms of PTSD was effective 12 times greater increased
across trauma populations.26 risk for substance abuse,
depression, and suicide
Four validated self-report scales
attempts; a 2 to 4 times
are commonly used: the Impact greater risk of smoking, 50
of Event Scale–Revised (IES-R),27 or more sexual partners, and
the PTSD Checklist–Civilian sexually transmitted
disease; and a 1.4 to 1.6 times
Version (PCL-C),28 the PTSD
greater risk of physical
Symptom Scale-Self-Report inactivity and morbid
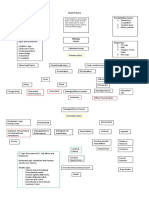
Version (PSS-SR),29 and the FIGURE 11-1 obesity.
Davidson Trauma Scale (DTS).30 Posttraumatic stress disorder (PTSD) and
complex PTSD in classification hierarchy. This ● Of deployed US military
figure demonstrates the underlying similarity in personnel, 14% to 16% were
IMPACT ON LONG-TERM found to have posttraumatic
symptom clusters in both PTSD and complex
PHYSICAL AND PTSD. Since complex PTSD usually results from stress disorder, which was
MENTAL HEALTH repeated trauma in childhood, thus impacting prospectively associated
The physical and mental health development, personality traits often include with early-age heart disease
difficulties with sense of self/self-esteem mortality among those free
correlates of a lifetime trauma of heart disease at baseline.
(self-organization), intense uncontrolled
load are consistent with an emotions (affect dysregulation), and trust of
epigenetic understanding of the others, as well as attachment difficulties
etiology and comorbidity of (leading to difficulties in relationships).
PTSD.31–33 One mechanism Consequently, both groups need treatment for
PTSD. In addition, patients with complex PTSD
involves repeated states of require longer-term attachment-informed
physiologic stress response and psychological work to change the way they cope
loss of regulation, with increased and experience the world and themselves.
Modified from Cloitre M, et al, Eur J Psychotraumatol.23
risk of psychiatric and physical © 2013 The Authors.
disorders. In a landmark paper,
Felitti and colleagues34 reported a
strong relationship between abuse
or childhood family dysfunction and increased adult health risk behaviors and
mortality, including mortality from cancer and heart, liver, lung, and skeletal
disease. Patients having four or more categories of childhood trauma had
a 4 to 12 times greater risk for substance abuse, depression, and suicide
attempts; a 2 to 4 times greater risk for smoking, 50 or more sexual partners,
and sexually transmitted disease; and a 1.4 to 1.6 times greater risk of
physical inactivity and morbid obesity compared to patients with no
childhood trauma.34
Literature examining the mental and behavioral health in armed forces deployed
in Iraq and Afghanistan suggests that depression is more common in women and
substance use is more common among men.35 Of deployed US military personnel,
14% to 16% were found to have PTSD, which was prospectively associated with
early-age heart disease mortality among those free of heart disease at baseline.36
This finding suggests that early-age heart disease may be an outcome after
military service in veterans with PTSD.37
PTSD is associated with smoking, drug and alcohol abuse, and obesity in
military veterans and civilian trauma survivors.38 This may be due to maladaptive
coping with distress with habitual use of substance or food. Alcohol and nicotine
use is high in PTSD; the odds of alcohol use disorders increase with the number
CONTINUUMJOURNAL.COM 879
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
POSTTRAUMATIC STRESS DISORDER
of PTSD criteria the patient meets. Research on comorbid PTSD and substance use
disorder supports parallel treatment to reduce PTSD severity and drug/alcohol
use posttreatment and improve subsequent follow-up.39
POSTTRAUMATIC STRESS DISORDER AND NEUROLOGIC DISORDERS
Stroke-related PTSD is common, with 25% of patients developing PTSD in the
first year after stroke and over 10% having chronic PTSD 1 year later,40 which
can be an important factor in secondary prevention with medication adherence.
Patients with respiratory failure due to Guillain-Barré syndrome should also be
screened for PTSD afterward.41 In one study, 5.17% (12) of 232 patients with
multiple sclerosis developed PTSD.42
It used to be assumed that people with traumatic brain injury (TBI) had
decreased risk for PTSD, as they could not remember the trauma,43 and
TBI-related amnesia may be confused with traumatic dissociative amnesia, which
results in the patient being unable to recall some parts of the trauma without
evidence of a significant TBI. However, mild TBI confers extra risk of PTSD, and
the combination is synergistic, with increased symptoms, cognitive impairment,
and difficulty in treatment.44
Migraine may predispose patients to PTSD and headache-related disability,14
especially in male patients.45,46
DEVELOPMENT OF POSTTRAUMATIC STRESS DISORDER
Learning and evolutionary theory add to our theoretical understanding of two main
experiences of PTSD: (1) extreme distress when faced with any trauma-associated
cues due to fear conditioning (the learned association of all trauma-related
experience to fear/distress, such as an assault by a tall bald man may generalize
to fear of all tall or all bald men, as tallness or baldness becomes associated
with fear) and (2) avoidance
behavior, which is reinforced by
immediate relief when a trauma
cue is removed or avoided (this is
called negative reinforcement, as it
is relief on removal of aversive
cue).47 During exposure therapy,
the patient is guided to engage
with a fear memory repeatedly
while feeling safe in the here and
now (in the therapist’s office)
and to discuss and process the
thoughts and emotions of this
“silent horror movie” memory
FIGURE 11-2 cognitively with the therapist,
Fear consolidation. Individuals with posttraumatic thus disrupting and altering the
stress disorder show increased sensitization to memory by extinguishing fear
stress, overgeneralization of fear, and impaired
extinction of fear memories. Individuals who recover
and enabling a different way of
from stress appropriately demonstrate an ability thinking about it. This is
to discriminate between fear-inducing and normal followed by reconsolidation of
stimuli as well as normal extinction of fear the less distressing, more
memories.
Reprinted with permission from Mahan AL, Ressler KJ,
processed memory
Trends in Neurosciences.48 © 2012 The Authors. (FIGURE 11-248).
880 JUNE 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Understanding Posttraumatic Stress Disorder Using Cognitive and KEY POINTS
Learning Theory
● Mild traumatic brain injury
Classic fear conditioning involves the pairing of an innate fear reaction confers extra risk of
(adrenergic response: startle, increased heart rate) to an unconditioned stimulus posttraumatic stress
(eg, stabbing) with a previously neutral valence (conditioned) stimulus (eg, disorder, and the
sound of ambulance, sight of blood). If PTSD ensues, the sound of a siren or the combination is synergistic,
with evidence of increased
sight of spilled ketchup may induce a fear response and flashbacks. Avoidance
symptoms, cognitive
symptoms are negatively reinforced by operant conditioning, as avoidance of impairment, and difficulty
triggers reduces distress and leads to reinforced learning that avoidance is the in treatment.
best action. Failure to recover from a trauma results in continued maladaptive
avoidance, repeatedly reinforced. ● Learning theory, along
with memory engagement,
disruption, alteration, and
Neurobiology, Neuroendocrinology, and Neurocircuitry reconsolidation, underpins
Animal models of PTSD have elucidated neurobiological underpinnings in the use of prolonged
humans. PTSD-like effects have been induced in rats, with anxiety behaviors of exposure therapy for
posttraumatic stress
avoidance, reduced concentration and sleep, decreased hippocampal volume, disorder.
physiologic changes in the hypothalamic-pituitary-adrenal (HPA) axis, and
amygdala hyperactivity.49 Traumatic events interfere with the memory function ● Animal models of
of the hippocampus and increase the plasticity processes in the amygdala.50 posttraumatic stress
disorder have elucidated
Physiologic changes have been reproduced, including decreased growth rate and
neurobiological
thymus weight and increased adrenal weight, anxiety and startle response, underpinnings in humans.
cardiovascular reactivity, and hormonal reactivity, while fear stimuli result in
freezing and avoidance. Zoladz and colleagues49 also found that predator ● Three main brain
exposure alone did not cause persistent PTSD-like behavior, so a social instability structures involved in
appraising threat and
model was introduced by randomly changing the rat roommate combinations, regulating fear have been
which successfully produced PTSD-like symptoms with predator exposure, studied in posttraumatic
replicating findings in humans that insufficient social support and instability are stress disorder: the
associated with increased risk of PTSD. prefrontal cortex, the
hippocampus, and
Neurobiological correlates support the learning hypothesis of PTSD and explain the amygdala.
its symptoms. Three main brain structures involved in appraising threat and
regulating fear have been studied in PTSD: the prefrontal cortex, the hippocampus, ● In posttraumatic stress
and the amygdala.51 disorder, the amygdala is
mostly hyperactive,
The amygdala plays a pivotal role in the brain circuit regulating fear
promoting an abnormal fear
conditioning.52 The central amygdala is responsible for sending fear signals to response of hypervigilant
the hypothalamus and brainstem. The medial prefrontal cortex is able to inhibit and hyperaroused behavior.
the amygdala in a top-down manner and reduces subjective distress. The
hippocampus codes fear memories and appraises and interprets the context and
threat of memories evoked. Together with the medial prefrontal cortex, the
hippocampus modulates fear, regulating the amygdala’s output to subcortical
brain regions that activate the fear response.
In PTSD, the amygdala is mostly hyperactive, promoting an abnormal fear
response of hypervigilant and hyperaroused behavior.53 PTSD results from an
acquired impaired capacity for fear extinction, possibly mediated by less activity
in the medial prefrontal cortex. Stress causes limbic activation, which inhibits
prefrontal cortex functioning, reducing inhibition of the amygdala and resulting in a
further fear response (FIGURE 11-3).
Neuroanatomic changes have been found in PTSD, including a decreased volume
of the prefrontal cortex, with decreased activation on exposure to traumatic
events.54 This loss of cortical reappraisal and ability to reduce the heightened
amygdala response allows repeated activation of the amygdala and dysregulated
CONTINUUMJOURNAL.COM 881
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
POSTTRAUMATIC STRESS DISORDER
FIGURE 11-3
Limbic system of the brain and its involvement in posttraumatic stress disorder (PTSD). The
prefrontal cortex is responsible for reactivating past emotional association and emotional
regulation. The hippocampus allows for conditioned fear of traumatic events and learned
responses to contextual cues. Both the hippocampus and the prefrontal cortex have altered
responsiveness in patients with PTSD. The top-down control of the amygdala by the
hippocampus and prefrontal cortex could play a role in the hyperactivity of the amygdala
seen in patients with PTSD who are hypervigilant. The ultimate effects of PTSD include
increased stress reactivity, generalized fear responses, and impaired extinction. Other
affected regions of the brain include the anterior cingulate cortex, the orbitofrontal
cortex, the parahippocampal gyrus, the thalamus, and the sensorimotor cortex, which
contributes to fear regulation and PTSD.
Reprinted with permission from Mahan AL, Ressler KJ, Trends in Neurosciences.48 © 2012 The Authors.
circuits between the prefrontal cortex and the limbic system. Reconsolidation of
unstable fear memories can lead to ongoing distressing flashbacks that feed into
further activation of the amygdala, with reduced prefrontal cortex inhibition. This
leads to the trauma memories becoming more intrusive over time, with persistent
hyperarousal and distress. Unstable trauma memories also provide an opportunity
for exposure therapy and thus extinction of fear from the memory before
reconsolidation of a more stable and less fear-linked memory.
Reduced prefrontal cortex function may also explain the impaired executive
function seen in PTSD as well as cognitive deficits due to decreased volume and
dysfunction in the hippocampus, with specific deficits in hippocampal-dependent
learning and memory.55 PTSD leads to changes in the HPA axis stress response
(with possible epigenetic changes) and the sympathetic nervous system, with
increased arousal, skin conductance, adrenaline and noradrenaline levels, blood
pressure, and anxiety behavior (FIGURE 11-456).57
Lifetime trauma burden increases the risk for developing acute disabling
symptoms of PTSD in those who have experienced previous trauma or have
882 JUNE 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
● Reconsolidation of
unstable fear memories can
lead to ongoing distressing
flashbacks that feed into
further activation of the
amygdala, with reduced
prefrontal cortex inhibition.
This leads to the trauma
memories becoming more
intrusive over time, with
persistent hyperarousal
and distress.
● Lifetime trauma burden
increases the risk for
developing acute disabling
symptoms of posttraumatic
stress disorder in those who
have experienced previous
trauma or have chronic
complex posttraumatic
stress disorder.
FIGURE 11-4
Stress response. Normal responses to stress (A), stress response in a patient with major
depressive disorder (B), and stress response in a patient with posttraumatic stress disorder
(PTSD) (C). In each panel, arrow thickness denotes the magnitude of biological response.
In healthy subjects and those with depression, periods of stress are associated with
increased cortisol and corticotropin-releasing factor. Corticotropin-releasing factor acts
on the anterior pituitary to stimulate corticotropin, which, in turn, stimulates cortisol
production by the adrenal cortex. Cortisol inhibits the release of both corticotropin and
corticotropin-releasing factor while also inhibiting many other stress-related biological
reactions. In patients with PTSD, cortisol levels are low, which allows for increased levels
of corticotropin-releasing factors. Additionally, the negative-feedback system of the
hypothalamic-pituitary-adrenal axis is more sensitive in patients with PTSD, contributing to
altered stress regulation in PTSD.
Reprinted with permission from Yehuda R, N Engl J Med.56 © 2002 Massachusetts Medical Society.
chronic complex PTSD. A longer and stronger physiologic reaction occurs
on anticipation or exposure to stress in those previously traumatized (due to the
initial increased secretion of cortisol and receptor density) compared to those
who have not experienced trauma, although enhanced negative feedback
follows, with an ongoing lower baseline cortisol.58 This phenomenon provides
the neurobiological explanation of why those with past trauma might be more
likely to develop PTSD with subsequent trauma.
Recent Trends in the Neurobiology of Posttraumatic Stress Disorder
An important area of recent research in PTSD is the study of genetic and
epigenetic phenomena with increasing trauma load. Epigenetic alteration of
the BDNF gene has been linked with brain function, memory, stress, and
neuropsychological changes.59 Using the psychosocial predator stress model,
Zoladz and colleagues demonstrated hypermethylation of the BDNF gene in the
dorsal hippocampus in mice.49 Changes in brain structures and pathways have
been explored in those with childhood trauma.60
CONTINUUMJOURNAL.COM 883
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
POSTTRAUMATIC STRESS DISORDER
Interventional research with the aim of regulating the HPA-prefrontal
cortex-amygdala circuitry includes electroconvulsive therapy, deep brain
stimulation, vagus nerve stimulation, repetitive transcranial magnetic
stimulation (rTMS), and transcranial direct current stimulation.
Neurotransmitters involved in control of thinking (such as g-aminobutyric acid
[GABA]) could be a target of treatment for PTSD. The current understanding
of the neurobiology of PTSD may explain the efficacy of selective serotonin
reuptake inhibitors (SSRIs) as a partial treatment for PTSD, as they increase
plasticity and learning capacity so that memories and danger assessment
of trauma-related cues can be altered more easily and sympathetic overdrive
is lessened.
TREATMENT OF POSTTRAUMATIC STRESS DISORDER
A broad, evidence-based approach is often needed in the treatment of PTSD,
including managing comorbid psychiatric illness, brain injury, and chronic pain;
medication; and using different therapeutic techniques, including prolonged
exposure therapy, cognitive processing therapy, and eye movement
desensitization and reprocessing therapy.
Early evidence supports new treatments for PTSD, such as rTMS, and
preliminary effectiveness has been shown for virtual reality exposure therapy,
Internet-based cognitive therapy, mindfulness-based cognitive therapy,
brainspotting, and yoga.61,62
A systematic review and meta-analysis of psychological treatments for
adults with PTSD demonstrated the efficacy of exposure therapy, including
prolonged exposure therapy, cognitive therapy, cognitive-behavioral
therapy mixed therapies, cognitive processing therapy, eye-movement
desensitization and reprocessing therapy, and narrative exposure therapy, in
improving PTSD symptoms.63 However, evidence is limited on whether any
one treatment or approach is more effective for particular symptoms or
patients. The tolerability and potential adverse effects of a particular
psychotherapy intervention over medication have also not yet been
fully explored.
In February 2017, the American Psychological Association published a
guideline for the treatment of PTSD in adults.64 The recommendations
were based on the strength of the evidence, outcomes, patient-reported
preference, balance of benefits, and applicability to the treatment population.
Cognitive-behavioral therapy, cognitive processing therapy, cognitive therapy,
and prolonged exposure therapy received strong recommendations. Other
suggested treatments included brief eclectic psychotherapy, eye movement
desensitization and reprocessing therapy, and narrative exposure therapy.
Recommended medications included fluoxetine, paroxetine, sertraline,
and venlafaxine, while insufficient evidence was found for risperidone
and topiramate.
Prolonged exposure therapy uses learning theory to extinguish fear from the
trauma memory by repeatedly engaging in the memories in a safe environment
without a feared outcome.65 Grounding and distraction may be needed in a
patient who quickly dissociates (the patient is physically present in the room but
increasingly goes back to the traumatic event in his/her mind, to the extent of
smelling smoke, coughing, feeling hot and terrified, as if back in the fire). In
prolonged exposure therapy, the memory is associated with less and less fear
884 JUNE 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
each time it is engaged, processed, and consolidated, gradually reversing the KEY POINTS
classic conditioned response. The patient listens to a tape of the session daily,
● The current
while also gradually reducing avoidance behavior (eg, leaving the house, walking understanding of the
down a street, crossing the street, being a passenger in a car, driving), which neurobiology of
reverses the operant negative reinforcement, and the patient’s world gradually posttraumatic stress
opens up again. disorder may explain the
efficacy of selective
Cognitive theory provides a model of PTSD as a failure to accept and integrate
serotonin reuptake
a trauma and explains symptoms of avoidance.66 Cognitive processing therapy inhibitors as a partial
addresses the distressing thoughts (eg, “it was my fault”) and associated feelings treatment for posttraumatic
(eg, guilt) that people may have in response to trauma.67 Self-blame and guilt stress disorder as they
increase plasticity and
will make patients avoid trauma-associated cues, and, depending on how they
learning capacity so that
think about the future, they may become extremely avoidant and limited in their memories and danger
daily life (eg, thinking that the world is a dangerous place and they cannot assessment of trauma-related
keep themselves safe). cues can be altered more
Eye movement desensitization and reprocessing therapy is a therapy easily and sympathetic
overdrive is lessened.
developed in 1987 for the treatment of PTSD.68,69 A good evidence base exists
for eye movement desensitization and reprocessing therapy, although ● A broad, evidence-based
controversy exists over whether the mechanism of eye movement approach is often needed in
desensitization and reprocessing therapy is distinct from prolonged exposure the treatment of
posttraumatic stress
therapy and whether it offers a treatment that is any more effective. In eye disorder, including
movement desensitization and reprocessing therapy, the patient is asked to allow managing comorbid
distressing trauma images to emerge while remaining aware of associated psychiatric illness, brain
thoughts, emotions, and bodily sensations and using side-to-side eye movements injury, and chronic pain;
medication; and using
or bilateral stimulation such as hand tapping.68,69 This is thought to allow
different therapeutic
processing of the trauma memory. techniques, including
prolonged exposure
Brief Eclectic Psychotherapy therapy, cognitive
Brief eclectic psychotherapy combines and integrates elements from processing therapy and eye
psychodynamic therapy, cognitive-behavioral therapy, and directive movement desensitization
and reprocessing therapy.
psychotherapy.70 Psychoeducation and exposure occur jointly with the patient
and therapist; a structured writing task and memorabilia are used to help ● The 2017 American
the patient access, feel, and express his or her trauma-related emotions. Psychological Association
This combination could be argued to effectively target social connection and guideline for the treatment
of posttraumatic stress
prefrontal cortex emotional regulation, correct cognitive distortions, and
disorder in adults gives
allow habituation. strong recommendation for
cognitive-behavioral
Recent Trends in the Treatment of Posttraumatic Stress Disorder therapy, cognitive
A recent consensus statement called for more research into novel pharmacologic processing therapy,
agents, therapeutic strategies, and targets based on our current understanding cognitive therapy, and
prolonged exposure
of PTSD neurocircuitry and mechanisms.71 Two reviews confirm new evidence
therapy.
for the use of rTMS based on interrupting the brain circuitry of PTSD (including
reducing hyperactivity of the amygdala), facilitating fear extinction capacity ● Prolonged exposure
and increasing cognitive control in the salience network (a network of brain therapy uses learning theory
regions of the brain that discriminate between stimuli, deciding how to allocate to extinguish fear from the
trauma memory by
attention to new stimuli and coordinating the brain's responses).72,73 Combining repeatedly engaging in the
brief script-driven exposure with deep transcranial magnetic stimulation was memories in a safe
found to reduce PTSD in patients who were treatment resistant.74 environment without a
feared outcome.
ONLINE THERAPY/VIRTUAL REALITY. In the past decade, e–mental health has been
shown to be a viable treatment for PTSD through virtual platforms in the form of
individual online psychotherapy, virtual reality programs, and Internet-based
CONTINUUMJOURNAL.COM 885
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
POSTTRAUMATIC STRESS DISORDER
self-help programs as the accessible first step of care.75 Internet-based
cognitive-behavioral therapy using video, audio, and virtual reality has
evidence as a preventive intervention early in the posttrauma period.76
TREATMENT OF COMPLEX TRAUMA
The picture and experience of complex trauma is different from acute
adult-onset PTSD after a single traumatic event. Some authors make the
argument that short-term, non–attachment-attuned treatment (treatment that is
not predicated on the therapeutic relationship being part of the treatment) for
single-trauma PTSD should not be assumed to be effective in those with complex
trauma.77,78 Little robust literature exists on effective treatment for complex
PTSD resulting from repeated trauma, including trauma in childhood. Some
Level 2 and Level 3 evidence exists for sensorimotor therapy and brainspotting
in the treatment of complex trauma. In brainspotting, the patient is guided
in a state of “focused activation” to correlate neurologic stimulation and
internal experience and allow for processing.61 It is posited that holding attention
on that “brainspot” allows processing of the traumatic event to continue
until activation has cleared. Significant controversy remains regarding the
mechanism of action of brainspotting, and strong evidence for its effectiveness
is lacking, partly because of the difficulty of manualizing this therapy into a
semistructured model of exact replicable steps.
PREVENTION OF AND EARLY INTERVENTION FOR POSTTRAUMATIC
STRESS DISORDER
Mitigation of the risk of PTSD pretrauma in the military and first responders is
gaining momentum, given concerns about the cost and disability associated with
PTSD. Interest is also growing in screening for PTSD in medical populations,
with evidence of improved clinical outcomes with secondary prevention and
early treatment.
Primary Prevention
Currently, a strong literature on successful primary prevention is lacking. Various
strategies have been used, such as pharmacologic intervention, pre–military
deployment screening for risk factors or stress, promotion of resilience, and
immediate postdeployment individual exposure therapy. Two recent studies
showed some promise for hydrocortisone in pretraumatic injury,79 and four
sessions of computerized attention bias modification training, thought to
disrupt threat monitoring and anticipatory stress response, reduced the risk
for PTSD.80
Secondary Prevention
Early posttrauma intervention, such as early brief exposure starting in the
emergency department to disrupt memory consolidation by habituating and
reducing the fear associated with the trauma memory, has had some success.81
Other early interventions to attempt to disrupt fear conditioning by reducing the
level of fear and arousal using propranolol or opioids have mixed evidence;
previous trials with clonidine and prazosin were not effective in reducing PTSD,
although prazosin has some evidence for reducing nightmares and improving
sleep in established PTSD (via a1 receptor antagonism).20
886 JUNE 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Recent Trends in the Prevention of Posttraumatic Stress Disorder KEY POINTS
Interest in how PTSD impacts the brain in the neurobiology of childhood
● Cognitive processing
survivors of trauma and in understanding and preventing intergenerational therapy addresses the
transmission of trauma is growing. Intergenerational transmission of trauma distressing thoughts and
may involve epigenetic phenomena and can also be understood in terms of associated feelings that
attachment and the impact of unprocessed trauma on the parent’s capacity to people may have in
response to trauma.
nurture his or her children (as illustrated in the Still Face Experiment82).83
PTSD in medical populations is the subject of ongoing program development ● Emerging evidence exists
and research, including patients in the intensive care unit; patients with HIV, for the use of repetitive
cancer, or stroke; patients who have had cardiac surgery or an organ transplant; transcranial magnetic
or patients who have given birth. Identifying those at particular risk and screening stimulation for
posttraumatic stress
for symptoms allows for sustainable stepped care, timely interventions, and disorder based on
judicious use of limited resources.84 interrupting the brain
Screening and early intervention in medical populations is an area of current circuitry of posttraumatic
research. Zatzick and colleagues84 conducted a trial in 207 acute physical stress disorder (including
reducing hyperactivity of
trauma survivors, screening for PTSD symptoms and then randomly the amygdala), facilitating
assigning to a stepped-care combined intervention (psychopharmacology and fear extinction capacity, and
cognitive-behavioral therapy, n = 104) or control (usual care, n = 103). At increasing cognitive control
6, 9, and 12 months postinjury, intervention participants had significantly in the salience network.
reduced PTSD symptoms compared to controls; they also showed improved
● Internet-based
physical function 1 year after hospitalization. Similarly, a stepped-care cognitive-behavioral
cognitive-behavioral therapy model of intervention in those who have had therapy using video, audio,
myocardial infarctions was found to improve outcomes.85 and virtual reality has
evidence as a preventive
A 2017 review demonstrated evidence that trauma-focused cognitive-behavioral
intervention early in the
therapy and modified prolonged exposure therapy delivered within weeks posttrauma period.
for individuals showing signs of distress due to a potential traumatic event
are effective to treat acute stress and early PTSD symptoms as well as to prevent ● Early posttrauma
PTSD.86 Posttrauma escitalopram improved sleep quality and had a signal intervention, such as early
brief exposure starting in
for secondary prevention in a subgroup of participants, and peritrauma the emergency department
intranasal oxytocin showed reduced PTSD symptoms after 1 month in those to disrupt memory
with high PTSD symptoms at baseline.87,88 Early intervention using video consolidation by habituating
games in the emergency department showed some success. This distracted and reducing the fear
associated with the trauma
patients, reduced further distressing activation of the fear memory, and was memory, has had some
associated with physiologic calming before memory consolidation in the success.
immediate posttraumatic period. Some research supports the use of agents
such as D-cycloserine (partial agonist of the N-methyl-D-aspartate [NMDA] ● Interest in how
posttraumatic stress
receptor) to augment the effects of learning.89
disorder impacts the brain
in the neurobiology of
EXISTENTIAL DISTRESS IN TRAUMA AND POSTTRAUMATIC GROWTH childhood survivors of
Apart from biological factors (eg, family history, past personal history of trauma and in understanding
psychiatric illness, TBI), psychological factors (eg, early loss, past trauma, low and preventing
intergenerational
self-esteem), and social factors (eg, low social support, financial difficulty), transmission of trauma
existential factors (finding meaning in an altered existence/life posttrauma, is growing.
coping with a threat to survival) can also play a part in trauma recovery.
Existential distress may result from a sense of demoralization, the inability to
accept the trauma, uncertainty about safety, death anxiety, and lost faith, and
they can all interfere with recovery.
In contrast, posttraumatic growth describes a philosophical change in
worldview after trauma, including increased gratitude to be alive, a sense of
connection to others, greater sense of meaning, spiritual well-being, and a sense
CONTINUUMJOURNAL.COM 887
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
POSTTRAUMATIC STRESS DISORDER
KEY POINTS of clear priority, with constructs of openness, optimism, and social support.90 A
2015 meta-analysis suggested active psychological intervention facilitates
● Identifying those at
particular risk for
posttraumatic growth and can help people make the most of adversity.91
posttraumatic stress
disorder and screening for
symptoms allows for CONCLUSION
sustainable stepped care,
Untreated PTSD is associated with a sense of personal chaos and distress.
timely interventions, and
judicious use of limited Patients cannot live normal lives, fully connect in relationships, or function at
resources. work and are highly avoidant of internal or external trauma-related cues; their
lives become painfully restricted. Since PTSD can easily be misdiagnosed, a
● Posttraumatic growth clear understanding and knowledge of the different presentations of PTSD
describes a philosophical
change in worldview after and patterns of functional impairment are important to prevent and mitigate
trauma, including increased PTSD-associated distress, adverse health consequences, and comorbidity.
gratitude to be alive, a sense The downstream health costs, suffering, and disability associated with PTSD
of connection to others, make it imperative to continue to research feasible, acceptable, effective,
spiritual well-being, and a
sense of clear priority, with
efficient, and accessible treatments for PTSD from single events as well as
constructs of openness, repeated childhood trauma. Ideally, primary and secondary prevention will
optimism, and social reduce the incidence and severity of PTSD. A failure to address acute or
support. lifelong PTSD can lead to epigenetic and attachment-based intergenerational
transmission of trauma.
● Untreated posttraumatic
stress disorder is associated It is hoped that understanding the neurobiological correlates of PTSD
with a sense of personal (hyperaroused amygdala and fear network and inhibition of the prefrontal
chaos and distress. Patients cortex salience network, with consequent emotional dysregulation) will combat
cannot live normal lives,
vestiges of internalized stigma or doubt by the general public in the existence of
fully connect in
relationships, or function at PTSD. This may reduce the associated shame of trauma vulnerability and
work and are highly avoidant increase the recognition of PTSD as a war wound or civilian trauma-related
of internal or external disorder that requires specialized multimodal treatment.
trauma-related cues; their The link between the mind and the body is a hot topic in medicine; PTSD
lives become painfully
restricted. provides the ideal paradigm for biopsychosocial research in biomarkers,
pharmacologic interventions, rTMS, sensorimotor psychotherapy, and
● The downstream health existential and trauma-focused cognitive therapies.
costs, suffering, and
disability associated with
PTSD make it imperative to
continue to research ACKNOWLEDGMENTS
feasible, acceptable, The authors would like to thank Saurav Barua, MPH, for his assistance with
effective, efficient, and references and literature review; Andrew Irwin, BSc, for his assistance with the
accessible treatments for
figures; and Clare Pain, MD, and Anthony Feinstein, MD, for their expert advice
posttraumatic stress
disorder from single events and comments.
as well as repeated
childhood trauma.
REFERENCES
1 Stam R. PTSD and stress sensitisation: a tale of 3 Kessler RC, Sonnega A, Bromet E, et al.
brain and body Part 1: human studies. Neurosci Posttraumatic stress disorder in the National
Biobehav Rev 2007;31(4):530–557. doi:10.1016/ Comorbidity Survey. Arch Gen Psychiatry 1995;
j.neubiorev.2006.11.010. 52(12):1048–1060. doi:10.1001/archpsyc.
1995.03950240066012.
2 Gradus JL. Prevalence and prognosis of stress
disorders: a review of the epidemiologic 4 Burri A, Maercker A. Differences in prevalence
literature. Clin Epidemiol 2017;9:251–260. rates of PTSD in various European countries
doi:10.2147/CLEP.S106250. explained by war exposure, other trauma and
cultural value orientation. BMC Res Notes 2014;
7(1):407. doi:10.1186/1756-0500-7-407.
888 JUNE 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
5 Atwoli L, Stein DJ, Koenen KC, McLaughlin KA. 18 Thompson-Hollands J, Jun JJ, Sloan DM. The
Epidemiology of posttraumatic stress disorder: association between peritraumatic dissociation
prevalence, correlates and consequences. Curr and PTSD symptoms: the mediating role of
Opin Psychiatry 2015;28(4):307–311. doi:10.1097/ negative beliefs about the self. J Trauma Stress
YCO.0000000000000167. 2017;30(2):190–194. doi:10.1002/jts.22179.
6 Kilpatrick DG, Resnick HS, Milanak ME, et al. 19 Brewin CR. Re-experiencing traumatic events in
National estimates of exposure to traumatic PTSD: new avenues in research on intrusive
events and PTSD prevalence using DSM-IV and memories and flashbacks. Eur J Psychotraumatol
DSM-5 criteria. J Trauma Stress 2013;26(5): 2015;6(1):27180. doi:10.3402/ejpt.v6.27180.
537–547. doi:10.1002/jts.21848.
20 George KC, Kebejian L, Ruth LJ, et al.
7 Spottswood M, Davydow DS, Huang H. The Meta-analysis of the efficacy and safety of
prevalence of posttraumatic stress disorder in prazosin versus placebo for the treatment of
primary care: a systematic review. Harv Rev nightmares and sleep disturbances in adults
Psychiatry 2017;25(4):159–169. doi:10.1097/ with posttraumatic stress disorder. J Trauma
HRP.0000000000000136. Dissociation 2016;17(4):494–510. doi:10.1080/
15299732.2016.1141150.
8 Wittchen HU, Jacobi F, Rehm J, et al. The size
and burden of mental disorders and other 21 Elhai JD, Biehn TL, Armour C, et al. Evidence for a
disorders of the brain in Europe 2010. unique PTSD construct represented by PTSD’s
Eur Neuropsychopharmacol 2011;21(9):655–679. D1-D3 symptoms. J Anxiety Disord 2011;25(3):
doi:10.1016/j.euroneuro.2011.07.018. 340–345. doi:10.1016/j.janxdis.2010.10.007.
9 Keyes KM, McLaughlin KA, Demmer RT, et al. 22 Lanius RA, Vermetten E, Loewenstein RJ, et al.
Potentially traumatic events and the risk of six Emotion modulation in PTSD: clinical and
physical health conditions in a population-based neurobiological evidence for a dissociative
sample. Depress Anxiety 2013;30(5):451–460. subtype. Am J Psychiatry 2010;167(6):640–647.
doi:10.1002/da.22090. doi:10.1176/appi.ajp.2009.09081168.
10 Edmondson D, Kronish IM, Shaffer JA, et al. 23 Cloitre M, Garvert DW, Brewin CR, et al. Evidence
Posttraumatic stress disorder and risk for coronary for proposed ICD-11 PTSD and complex PTSD: a
heart disease: a meta-analytic review. Am Heart J latent profile analysis. Eur J Psychotraumatol 2013;
2013;166(5):806–814. doi:10.1016/j.ahj.2013.07.031. 15:4. doi:10.3402/ejpt.v4i0.20706.
11 Greenberg MS, Tanev K, Marin MF, Pitman RK. 24 First MB, Williams JB, Karg RS, Spitzer RL.
Stress, PTSD, and dementia. Alzheimers Dement Structured Clinical Interview for DSM-5—
2014;10(3):S155–S165. doi:10.1016/j.jalz.2014.04.008. Research Version (SCID-5 for DSM-5, Research
Version; SCID-5-RV). Arlington, VA: American
12 Hudson JI, Hiripi E, Pope HG, Kessler RC. The
Psychiatric Association, 2015.
prevalence and correlates of eating disorders in
the National Comorbidity Survey Replication. Biol 25 Blake DD, Weathers FW, Nagy LM, et al. The
Psychiatry 2007;61(3):348–358. doi:10.1016/ development of a clinician-administered PTSD
j.biopsych.2006.03.040. scale. J Trauma Stress 1995;8(1):75–90.
doi:10.1002/jts.2490080106.
13 Mitchell KS, Mazzeo SE, Schlesinger MR, et al.
Comorbidity of partial and subthreshold PTSD 26 Brewin CR. Systematic review of screening
among men and women with eating disorders in instruments for adults at risk of PTSD. J Trauma
the national comorbidity survey-replication Stress 2005;18(1):53–62. doi:10.1002/jts.20007.
study. Int J Eat Disord 2012;45(3):307–315.
27 Horowitz M, Wilner N, Alvarez W. Impact of
doi:10.1002/eat.20965.
Event Scale: a measure of subjective stress.
14 Smitherman TA, Kolivas ED. Trauma exposure Psychosom Med 1979;41(3):209–218.
versus posttraumatic stress disorder: relative
28 Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE.
associations with migraine. Headache 2013;53(5):
Psychometric properties of the PTSD
775–786. doi:10.1111/head.12063.
Checklist—Civilian version. J Trauma Stress
15 Monson CM, Gradus JL, La Bash HAJ, et al. The 2003;16(5):495–502.
role of couples' interacting world assumptions
29 Foa EB, Riggs DS, Dancu CV, Rothbaum BO.
and relationship adjustment in women's
Reliability and validity of a brief instrument
postdisaster PTSD symptoms. J Trauma Stress
for assessing posttraumatic stress disorder.
2009;22(4):276–281. doi:10.1002/jts.20432.
J Trauma Stress 1993;6(4):459–473. doi:10.1002/
16 Simon NM, Shear KM, Thompson EH, et al. The jts.2490060405.
prevalence and correlates of psychiatric
30 Davidson JR, Book SW, Colket JT, et al.
comorbidity in individuals with complicated
Assessment of a new self-rating scale for
grief. Compr Psychiatry 2007;48(5):395–399.
post-traumatic stress disorder. Psychol Med
doi:10.1016/j.comppsych.2007.05.002.
1997;27(1):153–156.
17 American Psychiatric Association. Diagnostic and
31 Caspi A, Sugden K, Moffitt TE, et al. Influence of
statistical manual of mental disorders, 5th ed
life stress on depression: moderation by a
(DSM-5). Washington, DC: American Psychiatric
polymorphism in the 5-HTT gene. Science 2003;
Association, 2013.
301(5631):386–389. doi:10.1126/science.
CONTINUUMJOURNAL.COM 889
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
POSTTRAUMATIC STRESS DISORDER
32 Zhang TY, Labonté B, Wen XL, et al. Epigenetic 44 Zatzick DF, Rivara FP, Jurkovich GJ, et al.
mechanisms for the early environmental Multisite investigation of traumatic brain injuries,
regulation of hippocampal glucocorticoid posttraumatic stress disorder, and self-
receptor gene expression in rodents and reported health and cognitive impairments. Arch
humans. Neuropsychopharmacology 2013;38(1): Gen Psychiatry 2010;67(12):1291–1300. doi:10.1001/
111–123. doi:10.1038/npp.2012.149. archgenpsychiatry.2010.158.
33 Yehuda R, Daskalakis NP, Lehrner A, et al. 45 Peterlin BL, Gupta S, Ward TN, MacGregor A. Sex
Influences of maternal and paternal PTSD on matters: evaluating sex and gender in migraine
epigenetic regulation of the glucocorticoid and headache research. Headache 2011;51(6):
receptor gene in Holocaust survivor offspring. 839–842. doi:10.1111/j.1526-4610.2011.01900.x.
Am J Psychiatry 2014;171(8):872–880. doi:10.1176/
appi.ajp.2014.13121571. 46 Friedman LE, Aponte C, Hernandez RP, et al.
Migraine and the risk of post-traumatic stress
34 Felitti VJ, Anda RF, Nordenberg D, et al. disorder among a cohort of pregnant women.
Relationship of childhood abuse and household J Headache Pain 2017;18(1):67. doi:10.1186/
dysfunction to many of the leading causes of s10194-017-0775-5.
death in adults. The Adverse Childhood
Experiences (ACE) Study. Am J Prev Med 1998; 47 Blechert J, Michael T, Vriends N, et al. Fear
14(4):245–258. doi:10.1016/S0749-3797(98)00017-8. conditioning in posttraumatic stress disorder:
evidence for delayed extinction of autonomic,
35 Ramchand R, Rudavsky R, Grant S, et al. experiential, and behavioural responses. Behav
Prevalence of, risk factors for, and Res Ther 2007;45(9):2019–2033. doi:10.1016/
consequences of posttraumatic stress disorder j.brat.2007.02.012.
and other mental health problems in military
populations deployed to Iraq and Afghanistan. 48 Mahan AL, Ressler KJ. Fear conditioning, synaptic
Curr Psychiatry Rep 2015;17(5):37. doi:10.1007/ plasticity and the amygdala: implications for
s11920-015-0575-z. posttraumatic stress disorder. Trends Neurosci
2012;35(1):24–35. doi:10.1016/j.tins.2011.06.007.
36 Gates MA, Holowka DW, Vasterling JJ, Keane TM,
Marx BP, Rosen RC. Posttraumatic stress 49 Zoladz PR, Diamond DM. Psychosocial stress in
disorder in veterans and military personnel: rats: animal model of PTSD based on clinically
Epidemiology, screening, and case recognition. relevant risk factors. In: Martin CR, Preedy VR,
Psychol Serv 2012;9(4):361–382. Patel VB, eds. Comprehensive guide to post-
traumatic stress disorder. Cham, Switzerland:
37 Boscarino JA. Posttraumatic stress disorder and
Springer, 2015:1–17. link.springer.com/
mortality among U.S. Army veterans 30 years
referenceworkentry/10.1007%2F978-3-319-
after military service. Ann Epidemiol 2006;
08613-2_58-1. Published June 26, 2015. Accessed
16(4):248–256.
April 2, 2018.
38 Boscarino JA. A prospective study of PTSD and
50 Southwick SM, Vythilingam M, Charney DS.
early-age heart disease mortality among
The psychobiology of depression and resilience
Vietnam veterans: implications for surveillance
to stress: implications for prevention and
and prevention. Psychosom Medicine 2008;
treatment. Annu Rev Clin Psychol 2005;1:
70(6):668–676.
255–291. doi:10.1146/annurev.clinpsy.1.
39 Tipps ME, Raybuck JD, Lattal KM. Substance 102803.143948.
abuse, memory, and post-traumatic stress 51 Shin LM, Rauch SL, Pitman RK. Amygdala, medial
disorder. Neurobiol Learn Mem 2014;112:87–100. prefrontal cortex, and hippocampal function in
doi:10.1016/j.nlm.2013.12.002. PTSD. Ann N Y Acad Sci 2006;1071(1):67–79.
40 Edmondson D, Richardson S, Fausett JK, et al. doi:10.1196/annals.1364.007.
Prevalence of PTSD in survivors of stroke and 52 Davis M. The role of the amygdala in fear and
transient ischemic attack: a meta-analytic anxiety. Annu Rev Neurosci 1992;15(1):353–375.
review. PLoS One 2013;8(6):e66435. doi:10.1371/ doi:10.1146/annurev.ne.15.030192.002033.
journal.pone.0066435.
53 Koenigs M, Grafman J. Posttraumatic stress
41 Chemtob CM, Herriott MG. Post-traumatic disorder: the role of medial prefrontal cortex
stress disorder as a sequela of Guillain-Barre and amygdala. Neuroscientist 2009;15(5):
syndrome. J Trauma Stress 1994;7(4):705–711. 540–548. doi:10.1177/1073858409333072.
doi:10.1007/BF02103017.
54 Dahlgren MK, Laifer LM, VanElzakker MB, et al.
42 Ostacoli L, Carletto S, Borghi M, et al. Prevalence Diminished medial prefrontal cortex activation
and significant determinants of post-traumatic during the recollection of stressful events is an
stress disorder in a large sample of patients acquired characteristic of PTSD [published
with multiple sclerosis. J Clin Psychol Med online ahead of print September 12, 2017].
Settings 2013;20(2):240–246. doi:10.1007/ Psychol Med. doi:10.1017/S003329171700263X.
s10880-012-9323-2.
55 Gilbertson MW, Shenton ME, Ciszewski A, et al.
43 Vanderploeg RD, Belanger HG, Curtiss G. Mild Smaller hippocampal volume predicts pathologic
traumatic brain injury and posttraumatic stress vulnerability to psychological trauma. Nature
disorder and their associations with health Neurosci 2002;5(11):1242–1247. doi:10.1038/nn958.
symptoms. Arch Phys Med Rehabil 2009;90(7):
1084–1093. doi:10.1016/j.apmr.2009.01.023.
890 JUNE 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
56 Yehuda R. Post-traumatic stress disorder. N Engl 70 Gersons BP, Schnyder U. Learning from traumatic
J Med 2002;346(2):108–114. experiences with brief eclectic psychotherapy
for PTSD. Eur J Psychotraumatol 2013;4.
57 Bremner JD, Vythilingam M, Vermetten E, et al.
doi:10.3402/ejpt.v4i0.21369.
Cortisol response to a cognitive stress challenge
in posttraumatic stress disorder (PTSD) related 71 de Kloet CS, Vermetten E, Geuze E, et al.
to childhood abuse. Psychoneuroendocrinology Assessment of HPA-axis function in
2003;28(6):733–750. doi:10.1016/S0306-4530(02) posttraumatic stress disorder: pharmacological
00067-7. and non-pharmacological challenge tests, a
review. J Psychiatr Res 2006;40(6):550–567.
58 Sriram K, Rodriguez-Fernandez M, Doyle III FJ.
doi:10.1016/j.jpsychires.2005.08.002.
Modeling cortisol dynamics in the
neuro-endocrine axis distinguishes normal, 72 Berlim MT, Van den Eynde F. Repetitive
depression, and post-traumatic stress disorder transcranial magnetic stimulation over the
(PTSD) in humans. PLoS Comput Biol 2012;8(2): dorsolateral prefrontal cortex for treating
e1002379. doi:10.1371/journal.pcbi.1002379. posttraumatic stress disorder: an exploratory
meta-analysis of randomized, double-blind
59 Kim TY, Kim SJ, Chung HG, et al. Epigenetic
and sham-controlled trials. Can J Psychiatry
alterations of the BDNF gene in combat-related
2014;59(9):487–496. doi:10.1177/
post-traumatic stress disorder. Acta Psychiatr
070674371405900905.
Scand 2017;135(2):170–179. doi:10.1111/acps.12675.
73 Trevizol AP, Barros MD, Silva PO, et al.
60 McCrory E, De Brito SA, Viding E. The impact of
Transcranial magnetic stimulation for
childhood maltreatment: a review of neurobiological
posttraumatic stress disorder: an updated
and genetic factors. Front Psychiatry 2011;2:48.
systematic review and meta-analysis. Trends
doi:10.3389/fpsyt.2011.00048.
Psychiatry Psychother 2016;38(1):50–55. doi:
61 Grand D. Brainspotting. A new brain-based 10.1590/2237-6089-2015-0072.
psychotherapy approach. Trauma Gewalt
74 Isserles M, Shalev AY, Roth Y, et al.
2011;3:276–285.
Effectiveness of deep transcranial magnetic
62 Cullen M. Mindfulness-based interventions: an stimulation combined with a brief exposure
emerging phenomenon. Mindfulness 2011;2(3): procedure in post-traumatic stress disorder—a pilot
186–193. doi:10.1007/s12671-011-0058-1. study. Brain Stimul 2013;6(3):377–383. doi:10.1016/j.
brs.2012.07.008.
63 Cusack K, Jonas DE, Forneris CA, et al.
Psychological treatments for adults with 75 Maercker A, Hecker T, Heim E. Personalized
posttraumatic stress disorder: a systematic Internet-based treatment services for
review and meta-analysis. Clin Psychol Rev 2016; posttraumatic stress disorder. Nervenarzt 2015;
43:128–141. doi:10.1016/j.cpr.2015.10.003. 86(11):1333–1342. doi:10.1007/s00115-015-4332-7.
64 American Psychological Association Guideline 76 Freedman SA, Dayan E, Kimelman YB, et al. Early
Development Panel for the Treatment of PTSD in intervention for preventing posttraumatic stress
Adults. Clinical practice guideline for the disorder: an Internet-based virtual reality
treatment of posttraumatic stress disorder treatment. Eur J Psychotraumatol 2015;6(1):
(PTSD) in adults. apa.org/ptsd-guideline/ptsd. 25608. doi:10.3402/ejpt.v6.25608.
pdf. Published February 24, 2017. Accessed
77 Corrigan FM, Hull AM. Neglect of the complex:
April 2, 2018.
why psychotherapy for the post-traumatic
65 Foa EB, Hembree EA, Rothbaum BO. Prolonged clinical presentations is often ineffective.
exposure therapy for PTSD: emotional processing BJPsych Bull 2015;39(2):86–89. doi:10.1192/pb.
of traumatic experiences: therapist guide. New bp.114.046995.
York, NY: Oxford University Press, 2007.
78 Corrigan FM, Hull AM. Recognition of the
66 Ehlers A, Clark DM, Hackmann A, et al. Cognitive neurobiological insults imposed by complex
therapy for post-traumatic stress disorder: trauma and the implications for
development and evaluation. Behav Res psychotherapeutic interventions. BJPsych Bull
Ther 2005;43(4):413–431. doi:10.1016/j. 2015;39(2):79–86. doi:10.1192/pb.bp.114.047134.
brat.2004.03.006.
79 Schelling G, Briegel J, Roozendaal B, et al.
67 Chard KM, Ricksecker EG, Healy ET, et al. The effect of stress doses of hydrocortisone
Dissemination and experience with cognitive during septic shock on posttraumatic stress
processing therapy. J Rehabil Res Dev 2012; disorder in survivors. Biol Psychiatry 2001;
49(5):667–678. 50(12):978–985. doi:10.1016/S0006-3223(01)
01270-7.
68 Shapiro F. Eye movement desensitization: a new
treatment for post-traumatic stress disorder. 80 Wald I, Fruchter E, Ginat K, et al. Selective
J Behav Ther Exp Psychiatry 1989;20(3):211–217. prevention of combat-related post-traumatic
doi:10.1016/0005-7916(89)90025-6. stress disorder using attention bias modification
training: a randomized controlled trial. Psychol
69 Shapiro F, Maxfield L. Eye movement
Med 2016;46(12):2627–2636. doi:10.1017/
desensitization and reprocessing (EMDR):
S0033291716000945.
Information processing in the treatment of
trauma. J Clin Psychol 2002;58(8):933–946.
CONTINUUMJOURNAL.COM 891
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
POSTTRAUMATIC STRESS DISORDER
81 Rothbaum BO, Kearns MC, Price M, et al. Early 87 Zohar J, Fostick L, Juven-Wetzler A, et al.
intervention may prevent the development of Secondary prevention of chronic PTSD by early
PTSD: a randomized pilot civilian study with and short-term administration of escitalopram: a
modified prolonged exposure. Biological prospective randomized, placebo-controlled,
Psychiatry 2012;72(11):957–963. doi:10.1016/ double-blind trial. J Clin Psychiatry 2017.
j.biopsych.2012.06.002. doi:10.4088/JCP.16m10730.
82 Tronick E. Still face experiment. youtube.com/ 88 van Zuiden M, Frijling JL, Nawijn L, et al.
watch?v=apzXGEbZht0. Published Intranasal oxytocin to prevent posttraumatic
November 30, 2009. Accessed April 2, 2018. stress disorder symptoms: a randomized
controlled trial in emergency department
83 van Ee E, Kleber RJ, Jongmans MJ. Relational
patients. Biol Psychiatry 2017;81(12):1030–1040.
patterns between caregivers with PTSD and
doi:10.1016/j.biopsych.2016.11.012.
their nonexposed children: a review. Trauma
Violence Abuse 2016;17(2):186–203. doi:10.1177/ 89 Ressler KJ, Rothbaum BO, Tannenbaum L, et al.
1524838015584355. Cognitive enhancers as adjuncts to psychotherapy:
use of D-cycloserine in phobic individuals to
84 Zatzick D, Jurkovich G, Rivara FP, et al. A
facilitate extinction of fear. Arch Gen Psychiatry
randomized stepped care intervention trial
2004;61(11):1136–1144. doi:10.1001/archpsyc.61.11.1136.
targeting posttraumatic stress disorder for
surgically hospitalized injury survivors. 90 Schubert CF, Schmidt U, Rosner R. Posttraumatic
Ann Surg 2013;257(3):390–399. doi:10.1097/ growth in populations with posttraumatic stress
SLA.0b013e31826bc313. disorder—a systematic review on growth-related
psychological constructs and biological
85 Katon W, Von Korff M, Lin E, Simon G. Rethinking
variables. Clin Psychol Psychother 2016;23(6):
practitioner roles in chronic illness: the
469–486. doi:10.1002/cpp.1985.
specialist, primary care physician, and the
practice nurse. Gen Hosp Psychiatry 2001;23(3): 91 Roepke AM. Psychosocial interventions and
138–144. doi:10.1016/S0163-8343(01)00136-0. posttraumatic growth: a meta-analysis.
J Consult Clin Psychol 2015;83(1):129–142. doi:
86 Birur B, Moore NC, Davis LL. An evidence-based
10.1037/a0036872.
review of early intervention and prevention of
posttraumatic stress disorder. Community
Ment Health J 2017;53(2):183–201. doi:10.1007/
s10597-016-0047-x.
892 JUNE 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Unified Huntington's Disease Rating Scale (UHDRS)Document2 pagesUnified Huntington's Disease Rating Scale (UHDRS)Jose Algomas Knorecuerdo0% (2)
- Overall Neuropathy Limitations Scale (ONLS) - UpToDateDocument2 pagesOverall Neuropathy Limitations Scale (ONLS) - UpToDateJose Algomas Knorecuerdo0% (1)
- Operation Instructions TBi BRG-2-VD - Rev 1.01 - eDocument25 pagesOperation Instructions TBi BRG-2-VD - Rev 1.01 - eJordano Fernandes67% (3)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Biomarkers For PDFDocument247 pagesBiomarkers For PDFBuga RazvanNo ratings yet
- ATLS NotesDocument15 pagesATLS NotesXavier Fung86% (7)
- Neuronorma Frontal PDFDocument21 pagesNeuronorma Frontal PDFJose Algomas KnorecuerdoNo ratings yet
- Neuronorma 2 Spans LNS TMT SDMTDocument15 pagesNeuronorma 2 Spans LNS TMT SDMTJose Algomas KnorecuerdoNo ratings yet
- NeurosyphilisDocument15 pagesNeurosyphilisJose Algomas KnorecuerdoNo ratings yet
- 0-0010 PDFDocument11 pages0-0010 PDFAnonymous syRbQm6No ratings yet
- The Spectator in The Text The Rhetoric Stagecoach Browne1975Document14 pagesThe Spectator in The Text The Rhetoric Stagecoach Browne1975Jose Algomas KnorecuerdoNo ratings yet
- Child Death Review Panel ReportDocument46 pagesChild Death Review Panel ReportNEWS CENTER MaineNo ratings yet
- Carroll - Identity Grief and SelfDocument19 pagesCarroll - Identity Grief and SelfMiguelySusy Ramos-RojasNo ratings yet
- Categories of Disability Under IDEADocument15 pagesCategories of Disability Under IDEAHafsa khanNo ratings yet
- Status Epilepticus and ICPDocument9 pagesStatus Epilepticus and ICPjoomds51No ratings yet
- Head Injury Pamphlet PDFDocument2 pagesHead Injury Pamphlet PDFapi-279596675No ratings yet
- Head Injury: Tsegazeab Laeke, MD, FCS (ECSA) August 1,2018Document38 pagesHead Injury: Tsegazeab Laeke, MD, FCS (ECSA) August 1,2018Amanuel AyladoNo ratings yet
- Traumatic Brain Injury - Epidemiology, Classification, and PathophysiologyDocument14 pagesTraumatic Brain Injury - Epidemiology, Classification, and PathophysiologyEdi BackyNo ratings yet
- Conquering The ComaDocument9 pagesConquering The ComamilandeepNo ratings yet
- Traumatic Brain InjuryDocument3 pagesTraumatic Brain InjuryJill Eizavel BertisNo ratings yet
- 13 - Partial Brain Tissue Oxygenation MonitoringDocument2 pages13 - Partial Brain Tissue Oxygenation MonitoringjasminemuammilNo ratings yet
- Traumatic Brain Injury ThesisDocument34 pagesTraumatic Brain Injury Thesisafisher4297100% (1)
- Urbina Barraza David (2019) Return To Work After An Acquired Brain Injury Why The Subjective Experience of The Patient Is ImportantDocument3 pagesUrbina Barraza David (2019) Return To Work After An Acquired Brain Injury Why The Subjective Experience of The Patient Is Importantdavid.urbinaNo ratings yet
- Polytrauma - Student's PresentationDocument24 pagesPolytrauma - Student's PresentationabdulazizNo ratings yet
- Facilitation Technique Sports and ExerciseDocument4 pagesFacilitation Technique Sports and Exerciseapi-339418889No ratings yet
- Intensive Care Management of The Head Injured Patient: Review ArticleDocument14 pagesIntensive Care Management of The Head Injured Patient: Review ArticlerickyGKNo ratings yet
- 2022 - Bedside Ultrasound For Ventricular Size Monitoring in Patients With PEEK Cranioplasty - A Preliminary Experience of Technical Feasibility in Neurotrauma SettingDocument9 pages2022 - Bedside Ultrasound For Ventricular Size Monitoring in Patients With PEEK Cranioplasty - A Preliminary Experience of Technical Feasibility in Neurotrauma SettingRosi MontesNo ratings yet
- Execution Function Perfor Test PDFDocument21 pagesExecution Function Perfor Test PDFLydia MartínNo ratings yet
- Abscesses Lecture - Physiotherapists. 2012Document24 pagesAbscesses Lecture - Physiotherapists. 2012divinaNo ratings yet
- EMVision Investor PresentationDocument22 pagesEMVision Investor PresentationIlya HoffmanNo ratings yet
- 1 - A Randomized Trial of Epinephrine in Out-Of-Hospital Cardiac Arrest - NEJMDocument19 pages1 - A Randomized Trial of Epinephrine in Out-Of-Hospital Cardiac Arrest - NEJMFernando YaksicNo ratings yet
- Phtls 9th Edition Prep Packets 2019aDocument19 pagesPhtls 9th Edition Prep Packets 2019ajuan4401100% (2)
- Traumatic Brain InjuryDocument53 pagesTraumatic Brain InjuryRodriguez AlexNo ratings yet
- Pathophysiology of Head TraumaDocument2 pagesPathophysiology of Head TraumaGrace Jane Dionaldo100% (1)
- Neurological Assessment Seminar TopicDocument19 pagesNeurological Assessment Seminar TopicKhirabdhi Tanaya SahuNo ratings yet
- Cultural ExplorationDocument33 pagesCultural Explorationapi-405667642No ratings yet
- Craniocerebral Traumatology TBIDocument22 pagesCraniocerebral Traumatology TBIconfuisosNo ratings yet
- Pyschological DisorderDocument2 pagesPyschological DisorderFatin AfyqahNo ratings yet