Professional Documents
Culture Documents
Skor PELOD Cohort
Skor PELOD Cohort
Uploaded by
Tiwi QiraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Skor PELOD Cohort
Skor PELOD Cohort
Uploaded by
Tiwi QiraCopyright:
Available Formats
Paediatrica Indonesiana
p-ISSN 0030-9311; e-ISSN 2338-476X; Vol.59, No.6(2019). p. 318-24; doi: http://dx.doi.org/10.14238/pi59.6.2019.318-24
Original Article
Severe sepsis criteria, PELOD-2, and
pSOFA as predictors of mortality in critically ill
children with sepsis
Anindita Wulandari, Pudjiastuti, Sri Martuti
S
Abstract epsis is one of the leading causes of death in
Background Sepsis is one of the main causes of death in infants infants and children all over the world.1-4
and children. Currently, it is defined as a life-threatening organ Currently, sepsis is defined as multiple organ
dysfunction, caused by an inflammatory response of infection.
Several organ dysfunction assessment methods are available, but dysfunction due to an unregulated host
they are not uniformly used. response to infection, which affects the course of the
Objective To compare the accuracy of three mortality predictor disease and prognosis in patients.5,6 Several scoring
tools: severe sepsis criteria, pediatric logistic organ dysfunction systems are used to assess organ dysfunction, which
(PELOD)-2, and pediatric sequential organ failure assessment
(pSOFA), in critically ill children with sepsis. in turn are used to diagnose sepsis. These assessment
Methods This prospective cohort study was conducted in the methods aim to consider the risk of mortality, outcome
pediatric intensive care unit (PICU) and pediatric high care unit predictions, prediction of the severity of the disease,
(HCU) of dr. Moewardi Hospital, Surakarta, Central of Java. All
patients who met the systemic inflammatory response syndrome
and organ failure. Such grading systems also assist
(SIRS) criteria were included in our study. The exclusion criteria clinical decision-making, research standardizing, and
were congenital anomalies of heart or kidney, malignancy, or he- comparison of patient services among intensive care
matological abnormalities. The data were taken from laboratory units.5-9
and physical examinations by the physicians on duty. The outcome
assessed was mortality. In 2005, the International Pediatric Sepsis Consensus
Results Of 30 subjects, the mean age was 22.22 (SD 29.36) Conference (IPSCC) introduced the SIRS criteria
months; the most common infection source was the respiratory with several additional parameters to assess organ
tract, followed by gastrointestinal tract and central nervous system.
Most subjects were treated in the PICU and had a mean length of
dysfunction in diagnosing severe sepsis,9 considered
stay of 8.70 (SD 11.91) days. Severe sepsis and PELOD-2 were the same as those uses to diagnose sepsis nowadays.6
not significant predictors of death. However, pSOFA score was a
statistically significant predictor of mortality, with odds ratio 10.11
(95%CI 1.054 to 97.002; P=0.039).
Conclusion Pediatric SOFA (pSOFA) is a better predictor of
mortality compared to PELOD-2 and SIRS-severe sepsis. A pSOFA From the Department of Child Health, Universitas Sebelas Maret Medical
score ≥ 2 increases the risk of mortality by 10.11-fold. [Paediatr School/Dr. Moewardi Hospital, Surakarta, Central Java, Indonesia.
Indones. 2019;59:318-24; doi: http://dx.doi.org/10.14238/
pi59.6.2019.318-24]. Corresponding author: Anindita Wulandari. Department of Child
Health, Universitas Sebelas Maret Medical School/Dr. Moewardi Hospital.
Jl. Kolonelk Soetarto No. 132 Surakarta, Central Java, Indonesia; Email:
Keywords: children; mortality; sepsis; PELOD-2; ilmiah.anin@gmail.com.
SIRS; SOFA
Submitted July 11, 2019. Accepted December 6, 2019.
318 • Paediatr Indones, Vol. 59, No. 6, November 2019
Anindita Wulandari et al.: Severe sepsis criteria, PELOD-2, and pSOFA as predictors of mortality in sepsis
The Indonesian Pediatric Association (IPA) currently < 2. The mortality outcome assessed and subjects were
recommends PELOD-2 to assess multiple organ divided into two groups, namely alive (survivors) and
dysfunction in sepsis.8 The latest consensus regarding died (non-survivors). Examination and assessment
sepsis in adults (Sepsis-3) uses SOFA to assess organ of the dependent variable was performed by the
dysfunction.6 In pediatric population, Matics et al.10 physician in charge of the ICU within the first 24 hours
proposed the pediatric SOFA which has been adapted of treatment and was followed until the patient was
to age and normal pediatric physiology. discharged from the ICU (survived or died).
In Indonesia, few studies have compared The description of each study variable was
mortality prediction accuracy in pediatric patients performed for the whole sample according to the
using the new internationally introduced pSOFA distribution of outcome categories (mortality).
criteria. Hence, we aimed to compare several systems
for evaluating organ dysfunction (severe sepsis criteria, Table 1. Organ dysfunction criteria9
PELOD-2, and pSOFA) and used to diagnose sepsis in Cardiovascular dysfunction
children, with regards to their accuracy in predicting Despite administration of isotonic intravenous uid bolus 40
mL/kg in 1 hr
mortality. Decrease in BP (hypotension) 5th percentile for age or systolic
BP <2 SD below normal for age
OR
Methods Need for vasoactive drug to maintain BP in normal range
(dopamine >5 µg/kg/min or dobutamine, epinephrine, or
norepinephrine at any dose)
This prospective cohort study was conducted to OR
Two of the following:
compare severe sepsis criteria, PELOD-2, and pSOFA Unexplained metabolic acidosis: base de cit >5.0 mEq/L
in predicting mortality among critically ill pediatric Increased arterial lactate >2 times upper limit of normal
patients with sepsis treated in the PICU and HCU in Oliguria: urine output <0.5 mL/kg/hr
Prolonged capillary re ll: >5 secs
Dr. Moewardi General Hospital, Surakarta, Central
Core to peripheral temperature gap >3°C
of Java. The study started in September 2018, ended
Respiratory
in March 2019, and employed a consecutive sampling PaO2/FIO2 <300 in absence of cyanotic heart disease or
method. All pediatric patients diagnosed with sepsis preexisting lung disease
based on the SIRS criteria 9 and whose parents OR
PaCO2 >65 torr or 20 mm Hg over baseline PaCO2
provided written informed consent were included in OR
our study. Patients with previously known malignancy, Proven need or >50% FIO2 to maintain saturation 92%
hematological abnormalities, or congenital heart, lung, OR
Need for nonelective invasive or noninvasive mechanical
or kidney anomalies were excluded from the study. ventilation
We assessed the variables of severe sepsis criteria, Neurologic
PELOD-2 scores, pSOFA scores, and mortality Glasgow Coma Score 11 (57)
incidence. OR
Acute change in mental status with a decrease in Glasgow
Subjects were assessed by three methods and Coma Score 3 points from abnormal baseline
divided into (+) and (-) groups accordingly. Sepsis is
Hematologic
defined as systemic inflammatory response syndrome Platelet count <80,000/mm3 or a decline of 50% in platelet
caused by suspected or proven infection. Subject count from highest value recorded over the past 3 days (for
chronic hematology/oncology patients)
with sepsis categorized as severe sepsis (-), while
OR
subject with sepsis plus one of organ dysfunction as International normalized ratio >2
mentioned in Table 1 was categorized as severe sepsis Renal
(+).9 The PELOD-2 was assessed using two cut-off Serum creatinine 2 times upper limit of normal for age or
values, namely ≥ 8 and ≥ 11; PELOD-2 score ≥ 8 2-fold increase in baseline creatinine
was rated as (+) and score < 8 as (-). Similarly, if Hepatic
Total bilirubin 4 mg/dL (not applicable for newborn)
we used the higher cut-off score, PELOD-2 score ≥ OR
11 was rated as (+) and score < 11 as (-). Scores ALT 2 times upper limit of normal for age
for pSOFA were considered (+) for ≥ 2, and (-) for BP=blood pressure; ALT=alanine transaminase.
Paediatr Indones, Vol. 59, No. 6, November 2019 • 319
Anindita Wulandari et al.: Severe sepsis criteria, PELOD-2, and pSOFA as predictors of mortality in sepsis
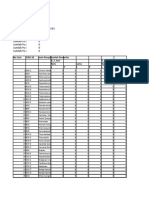
Numerical variables are presented as frequency and Table 2. Subjects’ characteristics
percentage (n and %), while categorical variables are Characteristics N=30
presented in mean and standard deviation (mean Mean age (SD), months 2.22 (29.36)
and SD). The OR value to state mortality risk Gender, n
was calculated and the relationship between each Male 20
Female 10
assessment criteria (severe sepsis criteria, PELOD-2,
Mean weight (SD), kg 8.51 (5.62)
and pSOFA) with mortality was analyzed by Chi-
square or Fisher's exact test for the unmet minimum Infection, n
Respiratory tract 22
expected value in cross-distribution. Results with GI tract 3
P value <0.05 were considered to be statistically CNS 4
significant. The accuracy of predicting mortality Other 1
for each tool and the comparison of the three tools Hospital unit, n
PICU 25
were also assessed by various diagnostic parameters HCU 5
including sensitivity, specificity, negative predictive Mean LOS (SD), day 8.70 (11.91)
value (NPV), positive predictive value (PPV), positive
Outcome, n
likelihood ratio (LR +), and negative likelihood ratio Died 14
(LR -). All data were analyzed with Microsoft Excel Survived 16
2007 and SPSS version 21 for Windows software.
This study was approved by the Health Research
Ethics Committee of the Universitas Sebelas Maret The significance of prediction accuracy of severe
Medical School/Dr. Moewardi Hospital Surakarta. sepsis criteria, PELOD-2, and pSOFA on mortality
was analyzed by Fisher's exact test, which revealed
that severe sepsis criteria and PELOD-2 were not
Results significant predictors for mortality (P> 0.05).
However, the pSOFA was a significant predictor for
Of 30 subjects, the mean age was 22.22 (SD 29.36) mortality (P=0.039). The OR value for the pSOFA
months. The proportion of males was twice the was also the highest at 10.111 (95%CI 1.054 to
number of females. The most common infection was 97.002). These results indicate that pSOFA was the
respiratory tract infection (22/30). Most subjects best predictor for mortality compared to severe sepsis
(25/30) were treated in the PICU and the rest were in criteria and PELOD-2 with both cut-off scores of 8
the HCU. The mean of length of stay (LOS) was 8.70 and 11 (Table 5).
days. The proportion of subjects who died reached
46.7%. The demographic characteristics of subjects Table 3. Subjects’ characteristics based on outcome
are presented in Table 2.
Characteristics Died Survived
In comparing subjects who died to subjects who (n=14) (n=16)
survived, the group who died had younger mean age Mean age (SD), months 12.61 (16.20) 30.62 (35.74)
(12.61 vs. 30.62 months, respectively), lower mean Gender, n
body weight (6.42 vs.10.33 kg, respectively), and Male 7 13
shorter mean length of stay (5.00 vs. 11.94 days, Female 7 3
respectively). All subjects who died were treated in Mean weight (SD), kg 6.42 (3.24) 10.33 (SD 6.65)
the PICU. The characteristics of subjects based on the Infection, n
outcome are shown in Table 3. Respiratory tract 11 11
GI tract 2 1
The three methods to assess organ dysfunction CNS 0 4
(severe sepsis criteria, PELOD-2, and pSOFA) were Others 1 0
analyzed in accordance to mortality incidence (Table Hospital unit, n
4). The PELOD-2 cut-off scores used in this study PICU 14 11
HCU 0 5
were ≥ 8 and ≥ 11, while the pSOFA cut-off score
Mean length of stay (SD), days 5.00 (7.64) 11.94 (14.13)
was ≥ 2.
320 • Paediatr Indones, Vol. 59, No. 6, November 2019
Anindita Wulandari et al.: Severe sepsis criteria, PELOD-2, and pSOFA as predictors of mortality in sepsis
Table 4. Organ dysfunction assessment system in
accordance to mortality incidence
Variables Total Died Survived
(N=30) (n=14) (n=16)
Severe sepsis criteria
Positive 25 13 12
Negative 5 1 4
PELOD-2 (score 11)
Positive 6 5 1
Negative 24 9 15
PELOD-2 (score 8)
Positive 14 9 5
Negative 16 5 11
pSOFA (score 2)
Positive 22 13 9
Negative 8 1 7
Table 5. Statistical analysis and OR value of the relationship between mortality and
severe sepsis criteria, PELOD-2, and pSOFA scores
Organ dysfunction assessment system OR 95%CI P value
SIRS (severe sepsis) 4.333 0.423 to 44.428 0.336
PELOD-2 (score 11) 8.333 0.835 to 83.167 0.072
PELOD-2 (score 8) 3.960 0.865 to 18.119 0.070
pSOFA (score 2) 10.111 1.054 to 97.002 0.039
The prognostic accuracy of the three methods and pSOFA, namely 92.9% for both. The PELOD-2
of assessment for sepsis can be compared with score ≥ 11 had the highest specificity (93.8%).
various diagnostic parameters. The highest The diagnostic parameter values for each tool are
sensitivity was found using severe sepsis criteria shown in Table 6.
Table 6. The diagnostic parameters of severe sepsis criteria, PELOD-2, and pSOFA as
mortality predictors.
Diagnostic parameters SIRS PELOD-2 PELOD-2 pSOFA
(severe sepsis) (score 11) (score 8) (score 2)
Sensitivity 92.9% 35.7% 64.3% 92.9%
Speci city 25.0% 93.8% 68.8% 43.8%
NPV 80.0% 62.5% 68.8% 87.5%
PPV 52.0% 83.3% 64.3% 59.1%
Positive LR 1.238 5.714 2.057 1.651
Negative LR 0.286 0.686 0.519 0.163
Positive PP 52.0% 83.3% 64.3% 59.1%
Negative PP 20.0% 37.5% 31.3% 12.5%
Paediatr Indones, Vol. 59, No. 6, November 2019 • 321
Anindita Wulandari et al.: Severe sepsis criteria, PELOD-2, and pSOFA as predictors of mortality in sepsis
Discussion >90% of pediatric patients with fever in the emergency
room, but in <5% of those who needed intensive care.
In our study, the mean age of subjects who met the Tachycardia and tachypnea are among the SIRS criteria
SIRS criteria and were treated in the PICU or HCU often found in mild, non-lethal, viral diseases, thus, the
was 22.22 months (1 year 10 months). The subjects SIRS criteria have a low specificity for identifying the
who died had a younger mean age than the survived risk of death.16 In our study, we compared the criteria for
group (12.61 months vs. 30.62 months, respectively). severe sepsis with other organ dysfunction criteria and
A study in Jakarta stated the same results, which found that PELOD-2 and pSOFA predictive accuracy
analyzed mortality in pediatric patients with sepsis were better than severe sepsis criteria.
and found out that the median age of subjects was 15 Agyeman et al.17 explained that SIRS conditions
months (range 2-192) with the highest distribution in with bacteremia increased the risk of death by 1% in
the 1 month - 1 year age group (62%).11 Younger age the first 30 days, but such risk would increase by 17%
has been associated with immune system immaturity if accompanied by organ dysfunction. Hence, the SIRS
and is usually accompanied by comorbidities, such as criteria has been abandoned and replaced by organ
congenital heart disease and kidney disease, thus the dysfunction assessment criteria to assess mortality
incidence of infections that cause sepsis is a factor that outcomes in intensive care pediatric patients.
increases the risk of mortality.1,11–13 Also, the Sepsis Previous studies have compared SIRS criteria to
Prevalence, Outcomes, and Therapies Study (SPROUT) other sepsis criteria, because the 2005 International
conducted in 128 PICUs in 26 countries revealed that Consensus introduced SIRS as a tool for diagnosing
patients who met SIRS-severe sepsis criteria based on sepsis.18,19 Only a few studies comparing severe sepsis-
international consensus had a mean age of 3 years, and SIRS criteria due to changes in the definition of sepsis
the foci of infection were the respiratory system (40%) that sepsis is considered equivalent to the diagnosis
and bacteremia (19%).1 In our study, the most common of severe sepsis according to the old consensus. This
focus of infection was the respiratory system, followed by current definition was published in sepsis-3.
the central nervous system (CNS) and gastrointestinal In our study, the criteria for severe sepsis were
(GI) infections. Respiratory tract infection is a major not statistically significant (P=0.336) in predicting
cause of illness and death in infants and children. mortality, although the sensitivity, specificity, NPV,
Environmental factors and highly contagious, air-borne and PPV were 92.9%, 25%, 80.0%, and 52%,
pathogens cause airway infections.14 respectively. A previous study showed that the criteria
All subjects who died were treated in the PICU for severe sepsis had a 74.5% sensitivity, 42.7%
with mean LOS of 8.7 days, which was shorter than specificity, 96.5% NPV, and 7.4% PPV for predicting
that of the survived group (11.94 days). This finding mortality. They also noted that the criteria for severe
was likely due to the fact that PICU patients tend sepsis was not good enough to predict mortality of
to have more severe clinical conditions than those critically ill children.19
treated in HCU. Furthermore, patients with severe We used PELOD-2 score of ≥ 11 based on the
airway infections generally require invasive breathing consensus guidelines for diagnosis and management
support, which is available only in the PICU. In a of sepsis in children from the Indonesian Pediatric
study validating the PELOD-2 method of the use of Association.8 We also analyzed the PELOD-2 cut-
mechanical ventilation led to OR of 3.99 (95%CI 2.07 off score of ≥ 8, since it is commonly used for a
to 7.70) on mortality (P <0.0001).15 A previous study comparison in previous studies.19 To date, there is not
also stated that sepsis increased the risk of death by 18 a uniform, internationally-recognized, cut-off value
times compared to non-sepsis patients with infection for PELOD-2 scores. The initial PELOD-2 validation
(OR 18; 95%CI 11 to 28). Most of them died because study found that PELOD-2 scores were significantly
of sepsis or septic shock (65%), and the course of higher in non-survivors compared to survivors [mean
disease necessitated intensive care unit treatment.10 14.9 (SD 6.1) vs. mean 4.2 (SD 3.2), respectively,
The SIRS criteria (IPSCC 2005) have been used P <0.0001].20 The study showed failure of three organ
to diagnose sepsis for a long time, but not specific. systems and a mean PELOD-2 score of 7.5 predicted a
The components of these criteria were found in mortality rate of 7.1%. Whereas failure of three organ
322 • Paediatr Indones, Vol. 59, No. 6, November 2019
Anindita Wulandari et al.: Severe sepsis criteria, PELOD-2, and pSOFA as predictors of mortality in sepsis
systems and mean PELOD-2 score of 11.5 predicted a PELOD-2 (AUC 0.94; 95% CI 0.92 to 0.95), and
mortality rate of 30.5%.15 A previous study reported better than PMODS (AUC 0.93; 95% CI 0.91 to 0.95)
that PELOD-2 score of ≥ 8 had sensitivity of 85.0%, (P<0.001) as a predictor of mortality in patients with
while PELOD-2 score of ≥ 11 had sensitivity of sepsis. They also reported that the relationship between
92.6% in the incidence of mortality. Their median pSOFA score on the first day of treatment (AUC 0.88;
PELOD-2 score was significantly higher in the group 95% CI 0.86 to 0.91) and patient mortality was better
who died than those who lived (died : survived = 13 than the other organ dysfunction assessment systems.
: 3; P=0.0001).20 It was also proportional to PRISM III (AUC 0.88;
We found that PELOD-2 score ≥ 8 lower 95%CI 0.86 to 0.91). In addition, pSOFA criteria ≥
prognostic value compared to other mortality 2 had an increased risk of death (OR 18; 95%CI 11
predictors. Although it was not the best predictor of to 28), and the most optimal pSOFA cut-off score for
mortality, PELOD-2 score ≥ 8 was better than severe predicting mortality was > 8.10
sepsis criteria based on diagnostic parameters. Both A similar study found that pSOFA [(adjusted
PELOD-2 scores of ≥ 11 and pSOFA scores had AUROC 0.892 (range 0.791-0.868)] was statistically
advantages in several diagnostic parameters that we significant in assessing mortality outcomes in sepsis
analyzed. PELOD-2 score ≥ 11 in our study had the patients and even better than PELOD-2 score of
highest specificity and PPV rates of 93.8% and 83.3%, ≥8 (AUROC 0.816; 0.777-0.854), qSOFA (AUROC
respectively, suggesting the lowest mortality predictor 0.739; 0.695-0.784), and SIRS (AUROC 0.710;
error and highest accuracy of life expectancy, with OR 0.664-0.756). 9 Our results suggest that pSOFA
8.33 (95%CI 0.835 to 83.16). However, this PELOD-2 and PELOD-2 are better than severe sepsis criteria
cut-off was not statistically significant (P=0.072). to predict mortality. This finding may have been
Schlapbach et al.19 demonstrated good results using related to the examination parameters in pSOFA
PELOD-2 score of ≥ 8 in predicting mortality, with and PELOD-2, which are better at describing organ
sensitivity, specificity, NPV, and PPV of 88.1%, 55.7%, function failure than the SIRS method.19
97%, and 22.2%, respectively. In addition, study in Our study had several limitations. The assessment
Indonesia used a PELOD-2 cut-off value of ≥20, and of organ dysfunction was done only once when the
found that such patients had a 7.75 times greater risk patient was admitted to the PICU or HCU. If the
of death.21 patients experienced a worsening of symptoms during
The SOFA, a system for evaluating organ the treatment, their scores may have actually gone
dysfunction, was recommended by the most recent higher. Also, the study was conducted in two different
consensus. 6,19 Pediatric SOFA is SOFA with places (PICU and pediatric HCU), hence, the severity
adjustments.10 The cut-off value in our study was of the disease, environmental factors, and supporting
≥2 as suggested by consensus.6 Our results showed care may have been different. In conclusion, pediatric
that pSOFA had advantages in sensitivity, NPV, SOFA (pSOFA) is the best predictor for mortality
negative LR, and negative PP than the other tools. compared to PELOD-2 and severe sepsis criteria. A
The pSOFA was better than other assessment positive pSOFA score (pSOFA ≥ 2) increases the risk
methods, if the aim is to get a more accurate of death by 10.11 times.
screening result for estimating the risk of death, as
pSOFA had the highest odds ratio (OR) value 10.11
(95%CI 1.054 to 97,.002; P<0.05). In contrast, Conflict of interest
severe sepsis criteria and PELOD-2 scores had a
lower risk of mortality and were not statistically None declared.
significant (P=0.336 and P=0.072, respectively;
P> 0.05).
Our result is parallel with that of a previous Funding acknowledgement
study which stated that the maximum score of pSOFA
(AUC 0.94; 95% CI 0.92 to 0.95) was proportional The authors received no specific grants from any funding agency
to PELOD (AUC 0.93; 95% CI 0.91 to 0.95) and in the public, commercial, or not-for-profit sectors.
Paediatr Indones, Vol. 59, No. 6, November 2019 • 323
Anindita Wulandari et al.: Severe sepsis criteria, PELOD-2, and pSOFA as predictors of mortality in sepsis
References DR, Kurniati N. Faktor risiko yang berperan pada mortalitas
sepsis. Sari Pediatr 2014;15:281-8.
1. Weiss SL, Fitzgerald JC, Pappachan J, Wheeler D, 12. Rusmawatiningtyas D, Nurnaningsih N. Mortality rates in
Jaramillo -bustamante JC, Salloo A, et al. Global pediatric septic shock. Paediatr Indones 2017;56:304. https://
epidemiology of pediatric severe sepsis: The sepsis doi.org/10.14238/pi56.5.2016.304-10.
prevalence, outcomes, and therapies study. Am J Respir 13. Mathias B, Mira JC, Larson SD. Pediatric sepsis. Wolters
Crit Care Med 2015;191:1147-57. DOI: https://doi. Kluwer Heal. 2016;28:1-8. DOI: https://doi.org/10.1097/
org/10.1164/rccm.201412-2323OC. MOP.0000000000000337.
2. Hartman ME, Linde-Zwirble WT, Angus DC, Watson 14. Everard ML. Paediatric respiratory infections. Eur Respir Rev
RS. Trends in the epidemiology of pediatric severe sepsis. 2016;25:36-40. DOI: https://doi.org/10.1183/16000617.0084-
Pediatr Crit Care Med 2013;14:686-93. DOI: https://doi. 2015.
org/10.1097/PCC.0b013e3182917fad. 15. Leteurtre S, Duhamel A, Salleron J, Grandbastien B, Lacroix
3. Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global, J, Leclerc F. PELOD-2: An update of the pediatric logistic
regional, and national causes of child mortality in 2000-13, organ dysfunction score. Crit Care Med 2013;41:1761-73.
with projections to inform post-2015 priorities: An updated DOI: https://doi.org/10.1097/CCM.ObOI.
systematic analysis. Lancet 2015;385:430-40. DOI: https:// 16. Scott HF, Deakyne SJ, Woods JM, Bajaj L. The prevalence
doi.org/10.1016/S0140-6736(14)61698-6. and diagnostic utility of systemic inflammatory response
4. Schlapbach LJ, Straney L, Alexander J, MacLaren G, Festa syndrome vital signs in a pediatric emergency department.
M, Schibler A, et al. Mortality related to invasive infections, Acad Emerg Med 2015;22:382-9.
sepsis, and septic shock in critically ill children in Australia 17. Agyeman PKA, Schlapbach LJ, Giannoni E, Stocker M,
and New Zealand, 2002-13: A multicentre retrospective Posfay-Barbe KM, Heininger U, et al. Epidemiology of blood
cohort study. Lancet Infect Dis 2015;15:46-54. DOI: https:// culture-proven bacterial sepsis in children in Switzerland:
doi.org/10.1016/S1473-3099(14)71003-5. a population-based cohort study. Lancet Child Adolesc
5. Kawasaki T. Update on pediatric sepsis : a review. J Intensive Heal 2017;1:124-33. DOI: https://doi.org/10.1016/S2352-
Care 2017;5:1-12. DOI: https://doi.org/10.1186/s40560-017- 4642(17)30010-X.
0240-1. 18. Raith EP, Udy AA, Bailey M, McGloughlin S, MacIsaac C,
6. Singer M, Deutschman CS, Seymour C, Shankar-Hari Bellomo R, et al. Prognostic accuracy of the SOFA score, SIRS
M, Annane D, Bauer M, et al. The Third International criteria, and qSOFA score for in-hospital mortality among
Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). adults with suspected infection admitted to the intensive
JAMA 2017;315:801-10. DOI: https://doi.org/10.1001/ care unit. JAMA - J Am Med Assoc 2017;317:290-300. DOI:
jama.2016.0287. https://doi.org/10.1001/jama.2016.20328.
7. Plunkett A, Tong J. Sepsis in children. BMJ 2015;7350:3017. 19. Schlapbach LJ, Straney L, Bellomo R, Maclaren G, Pilcher
DOI: https://doi.org/10.1136/bmj.h3017. D. Prognostic accuracy of age-adapted SOFA, SIRS,
8. Hadinegoro SRS, Chairulfatah A, Latief A, Pudjiadi AH, PELOD -2, and qSOFA for in-hospital mortality among
Karyanti M, Setiabudi D, et al. Diagnosis dan tata laksana children with suspected infection admitted to the intensive
sepsis pada anak. Jakarta: Badan Penerbit IDAI; 2016. care unit. Intensive Care Med 2018;44:179-88. DOIhttps://
p.1-9. doi.org/10.1007/s00134-017-5021-8.
9. Goldstein B, Giroir B, Randolph A. International Pediatric 20. Leteurtre S, Leclerc F, Duhamel A, Deken V, Grandbastien
Sepsis Consensus Conference: Definitions for sepsis and organ B, Biarent D, et al. Groupe Francophone de Reanimation
dysfunction in pediatrics*. Pediatr Crit Care Med 2005;6:2-8. et Urgences Pediatrques (GFRUP). Can the pediatric
DOI: https://doi.org/10.1097/01.PCC.0000149131.72248. logistic organ dysfunction (PELOD)-2 score on day 1 be
E6. used in clinical criteria for sepsis in children? Pediatr Crit
10. Matics TJ, Sanchez-Pinto LN. Adaptation and validation Care Med 2017;18:758-63. DOI: https://doi.org/10.1097/
of a pediatric sequential organ failure assessment score and PCC.0000000000001182.
evaluation of the Sepsis-3 definitions in critically ill children. 21. Bramantyo TB, Martuti S, Salimo H. Perbandingan prediktor
JAMA Pediatr 2017;60611:1-9. DOI: https://doi.org/10.1001/ mortalitas skor PRISM III dan PELOD 2 pada anak sakit
jamapediatrics.2017.2352. kritis non bedah. Sari Pediatr 2018;19:284. DOI: https://doi.
11. Saraswati DD, Pudjiadi AH, Djer MM, Supriyatno B, Syarif org/10.14238/sp19.5.2018.284-9.
324 • Paediatr Indones, Vol. 59, No. 6, November 2019
You might also like
- Workbook 2Document82 pagesWorkbook 2Jobelle Cariño Resuello67% (3)
- How To Write A Case HistoryDocument4 pagesHow To Write A Case HistoryMink's ImranNo ratings yet
- Cosh Post Test New JbeDocument3 pagesCosh Post Test New Jbehernie w. vergel de dios jr0% (1)
- Cancer Simplified Lighter VersionDocument33 pagesCancer Simplified Lighter VersionRama KrisnaNo ratings yet
- DONOR SELECTION (Deferral) - BBDocument5 pagesDONOR SELECTION (Deferral) - BBMaikka IlaganNo ratings yet
- MCQ Combined PDFDocument304 pagesMCQ Combined PDFRahul GurjarNo ratings yet
- Pediatric SepsisDocument16 pagesPediatric SepsisOsiithaa CañaszNo ratings yet
- Practical Algorithms in Pediatric EndocrinologyDocument22 pagesPractical Algorithms in Pediatric EndocrinologyTiwi QiraNo ratings yet
- GSIS VS. ESTEVES, G.R. NO. 182297, JUNE 21, 2017 (Employees' Compensation)Document2 pagesGSIS VS. ESTEVES, G.R. NO. 182297, JUNE 21, 2017 (Employees' Compensation)mae ann rodolfoNo ratings yet
- O.safety Engineer Mohammed MoinuddinDocument3 pagesO.safety Engineer Mohammed MoinuddinMohammed MoinuddinNo ratings yet
- Hospital Planning: Prepared & Presented By-Awantika Diwan MBA (HA&HC)Document32 pagesHospital Planning: Prepared & Presented By-Awantika Diwan MBA (HA&HC)Pooja Jain100% (1)
- Paediatrica Indonesiana: Muhammad Aulia, Silvia Triratna, Yulia Iriani, Achirul Bakri, Indra SaputraDocument7 pagesPaediatrica Indonesiana: Muhammad Aulia, Silvia Triratna, Yulia Iriani, Achirul Bakri, Indra Saputrachartreuse avonleaNo ratings yet
- JournalDocument8 pagesJournaladindaNo ratings yet
- Pelod ScoreDocument7 pagesPelod ScoreAgus SarjonoNo ratings yet
- Paediatrica IndonesianaDocument6 pagesPaediatrica IndonesianayusrinastitiNo ratings yet
- Schlapbach2017 PDFDocument10 pagesSchlapbach2017 PDFAswin ChristantoNo ratings yet
- Role of Laboratory Diagnostic Tests in First Febrile SeizureDocument4 pagesRole of Laboratory Diagnostic Tests in First Febrile SeizureAlbertNo ratings yet
- Paediatrica Indonesiana: Fanny Listiyono, Sumadiono, Cahya Dewi Satria, Indah K. MurniDocument6 pagesPaediatrica Indonesiana: Fanny Listiyono, Sumadiono, Cahya Dewi Satria, Indah K. MurniRay PradityaNo ratings yet
- Clasificación PIRO en Sepsis Grave y Shock Séptico Pediátrico Daniela Arriagada, Franco Diaz, Alejandro Donoso, Pablo CrucesDocument7 pagesClasificación PIRO en Sepsis Grave y Shock Séptico Pediátrico Daniela Arriagada, Franco Diaz, Alejandro Donoso, Pablo CrucesDiana Paola Castaño SalazarNo ratings yet
- Mortalidad PardsDocument9 pagesMortalidad PardsBarbara Seminario RamirezNo ratings yet
- Paediatrica Indonesiana: Lukman Oktadianto, Risky Vitria Prasetyo, Ninik Asmaningsih Soemyarso, Mohammad Sjaifullah NoerDocument6 pagesPaediatrica Indonesiana: Lukman Oktadianto, Risky Vitria Prasetyo, Ninik Asmaningsih Soemyarso, Mohammad Sjaifullah Noerazwin lubisNo ratings yet
- 2004 - Category Based Treatment of Tuberculosis in ChildrenDocument4 pages2004 - Category Based Treatment of Tuberculosis in ChildrenTammy Utami DewiNo ratings yet
- Journal of Clinical & Translational Endocrinology: SciencedirectDocument6 pagesJournal of Clinical & Translational Endocrinology: SciencedirecthildaNo ratings yet
- 12 11 PBDocument168 pages12 11 PBYS NateNo ratings yet
- Hamijoyo Et Al 2022 Comparison of Clinical PreDocument6 pagesHamijoyo Et Al 2022 Comparison of Clinical PreLinhNo ratings yet
- 46-51 WinandaDocument7 pages46-51 WinandaRIMA MELATI ANGGRAENINo ratings yet
- Pneumonia PDFDocument11 pagesPneumonia PDFWidya MelianitaNo ratings yet
- 1 s2.0 S0300289622006640 MainDocument7 pages1 s2.0 S0300289622006640 MainInda MegaNo ratings yet
- Journal 4Document5 pagesJournal 4Claudia JessicaNo ratings yet
- Correlation of Serum Lactate Levels With Survival in Patients With SepsisDocument6 pagesCorrelation of Serum Lactate Levels With Survival in Patients With SepsisIJAR JOURNALNo ratings yet
- SIRS, qSOFA, and Organ Failure For Assessing Sepsis at The Emergency DepartmentDocument4 pagesSIRS, qSOFA, and Organ Failure For Assessing Sepsis at The Emergency DepartmentAnnitaCristalNo ratings yet
- Paediatrica IndonesianaDocument8 pagesPaediatrica IndonesianaRendra SyaniNo ratings yet
- 2021 Amaylia Oehadian - Putri - Uun - Bahti - Evan - Jeffery (U) - Erythropoiesis Differences in Various ClinicalDocument6 pages2021 Amaylia Oehadian - Putri - Uun - Bahti - Evan - Jeffery (U) - Erythropoiesis Differences in Various ClinicalEvan SusandiNo ratings yet
- 5754-Article Text-43741-3-10-20220520Document18 pages5754-Article Text-43741-3-10-20220520Ricardo TanNo ratings yet
- Delirium in Elderly Is Age The Sole Factor in Determining PrognosisDocument7 pagesDelirium in Elderly Is Age The Sole Factor in Determining PrognosisKarina CabayNo ratings yet
- Quick Sepsis-Related OrganDocument12 pagesQuick Sepsis-Related OrganArnavjyoti DasNo ratings yet
- 00002Document5 pages00002Oscar F. Vargas AlvaradoNo ratings yet
- PCMC Journal No 2rDocument82 pagesPCMC Journal No 2rwarlock ibanezNo ratings yet
- Predicting Outcome in Neonates With Possible Clinical Sepsis by Estimating An Early Score For Neonatal Acute Physiology-II (SNAP-II)Document8 pagesPredicting Outcome in Neonates With Possible Clinical Sepsis by Estimating An Early Score For Neonatal Acute Physiology-II (SNAP-II)ida ayu agung WijayantiNo ratings yet
- Jurnal Pediatric ShockDocument6 pagesJurnal Pediatric ShockHhhNo ratings yet
- 2723-Article Text-12167-2-10-20221223Document8 pages2723-Article Text-12167-2-10-20221223irbah khoirunisaNo ratings yet
- Prognostic of Sepsis in A Congolese Pediatric Emergency Service Using PSOFA Score A Prospective StudyDocument6 pagesPrognostic of Sepsis in A Congolese Pediatric Emergency Service Using PSOFA Score A Prospective StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Risk of OSA in DM Type 2 PatientsDocument9 pagesRisk of OSA in DM Type 2 Patientskryshna maqNo ratings yet
- Comparative Analysis of Severe Pediatric and Adult Leptospirosis in Sa o Paulo, BrazilDocument3 pagesComparative Analysis of Severe Pediatric and Adult Leptospirosis in Sa o Paulo, BrazilShofura AzizahNo ratings yet
- JCM 12 03447 v2Document11 pagesJCM 12 03447 v2Marcellia AngelinaNo ratings yet
- Jurnal GnaDocument5 pagesJurnal Gnairvan halimNo ratings yet
- Brini2017 PDFDocument16 pagesBrini2017 PDFAde Maghvira PutriNo ratings yet
- 2313-Article Text-7719-2-10-20200828Document8 pages2313-Article Text-7719-2-10-20200828Suryadi LimardiNo ratings yet
- 147-Article Text-494-1-10-20211209Document14 pages147-Article Text-494-1-10-20211209Marcellia AngelinaNo ratings yet
- Serum Neuroinflammatory Disease-Induced Central Nervous System Proteins Predict Clinical Onset of Experimental Autoimmune EncephalomyelitisDocument15 pagesSerum Neuroinflammatory Disease-Induced Central Nervous System Proteins Predict Clinical Onset of Experimental Autoimmune EncephalomyelitisIchim MadalinaNo ratings yet
- Santoso 2020Document10 pagesSantoso 2020Aldo VictoriaNo ratings yet
- Epidemiology of ParkinsonismDocument26 pagesEpidemiology of Parkinsonismelenac67No ratings yet
- Markers of Disease Severity and Prolonged Length of Stay For Paediatric Diabetic KetoacidosisDocument6 pagesMarkers of Disease Severity and Prolonged Length of Stay For Paediatric Diabetic KetoacidosisSSR-IIJLS JournalNo ratings yet
- Short-Term Outcome of Proliferative Lupus Nephritis A Single Center StudyDocument12 pagesShort-Term Outcome of Proliferative Lupus Nephritis A Single Center StudyTJPRC PublicationsNo ratings yet
- Fitzgerald 2019Document10 pagesFitzgerald 2019senkonenNo ratings yet
- Indar KumarDocument4 pagesIndar Kumargwenn satunyaNo ratings yet
- Eria 2Document11 pagesEria 2ruth angelinaNo ratings yet
- Estudio 3Document11 pagesEstudio 3Medico CuriosoNo ratings yet
- Sjogren ILD1Document12 pagesSjogren ILD1Dra Daphne Rivero GallegosNo ratings yet
- A Placebo-Controlled Trial of Oral Fingolimod in Relapsing Multiple SclerosisDocument15 pagesA Placebo-Controlled Trial of Oral Fingolimod in Relapsing Multiple SclerosisNidia BracamonteNo ratings yet
- Serrum Ferritin: A Prognostic Marker in Patients With Sepsis in Pediatric Age Group: A Prospective Cohort StudyDocument4 pagesSerrum Ferritin: A Prognostic Marker in Patients With Sepsis in Pediatric Age Group: A Prospective Cohort StudyclaudyNo ratings yet
- Ep15754 orDocument6 pagesEp15754 orsiskaNo ratings yet
- Research Article: The Analysis of Etiology and Risk Factors For 192 Cases of Neonatal SepsisDocument7 pagesResearch Article: The Analysis of Etiology and Risk Factors For 192 Cases of Neonatal Sepsisflorentina lulutNo ratings yet
- Adaptation and Validation of A Pediatric Sequential Organ 2017 Matics JAMADocument9 pagesAdaptation and Validation of A Pediatric Sequential Organ 2017 Matics JAMALUIS FRANCISCO GUERRERO MARTÍNEZNo ratings yet
- NutritionDocument10 pagesNutritionDani ursNo ratings yet
- 307 974 1 PBDocument8 pages307 974 1 PBRifdah AmalinaNo ratings yet
- Abc 104 01 0058Document8 pagesAbc 104 01 0058Trung Nguyễn BảoNo ratings yet
- Img#Document5 pagesImg#AngelNo ratings yet
- Status Epilepticus in Adults: A Study From Nigeria: SciencedirectDocument6 pagesStatus Epilepticus in Adults: A Study From Nigeria: SciencedirectLuther ThengNo ratings yet
- The Prevention and Treatment of Disease with a Plant-Based Diet Volume 2: Evidence-based articles to guide the physicianFrom EverandThe Prevention and Treatment of Disease with a Plant-Based Diet Volume 2: Evidence-based articles to guide the physicianNo ratings yet
- Impacts of The COVID-19 Pandemic On Children: An Ethical Analysis With A Global-Child LensDocument10 pagesImpacts of The COVID-19 Pandemic On Children: An Ethical Analysis With A Global-Child LensTiwi QiraNo ratings yet
- Tugas Dr. M Riza, Sp.A (K), M.KesDocument19 pagesTugas Dr. M Riza, Sp.A (K), M.KesTiwi QiraNo ratings yet
- Ethics in Pediatric Patient CareDocument12 pagesEthics in Pediatric Patient CareTiwi QiraNo ratings yet
- Neonatal Sepsis - A Review: January 2012Document9 pagesNeonatal Sepsis - A Review: January 2012Tiwi QiraNo ratings yet
- Guidelines For Surfactant Replacement Therapy in Neonates Canadian Paediatric SocietyDocument8 pagesGuidelines For Surfactant Replacement Therapy in Neonates Canadian Paediatric SocietyTiwi QiraNo ratings yet
- Practical-Algorithms-Diare KronisDocument20 pagesPractical-Algorithms-Diare KronisTiwi QiraNo ratings yet
- AHA Hypertension JournalDocument10 pagesAHA Hypertension JournalTiwi QiraNo ratings yet
- Traumatic Optic Neuropathy: Review ArticleDocument9 pagesTraumatic Optic Neuropathy: Review ArticleTiwi QiraNo ratings yet
- 4.1. Hasil Pengamatan 4.1.1.data Pengamatan MangroveDocument2 pages4.1. Hasil Pengamatan 4.1.1.data Pengamatan MangroveTiwi QiraNo ratings yet
- Definitions: Herpes Simplex Virus Epstein-Barr Virus (EBV) Cytomegalovirus Adenovirus Measles VirusDocument4 pagesDefinitions: Herpes Simplex Virus Epstein-Barr Virus (EBV) Cytomegalovirus Adenovirus Measles VirusSarah OvinithaNo ratings yet
- Conditional ZeroDocument2 pagesConditional ZeroJimmy JuanNo ratings yet
- Texto 1Document7 pagesTexto 1christiamNo ratings yet
- Frances Miller ResumeDocument1 pageFrances Miller Resumeapi-522165600No ratings yet
- High-Pressure Fluid Injection Injuries: Toolbox TalkDocument3 pagesHigh-Pressure Fluid Injection Injuries: Toolbox TalkRahulNo ratings yet
- Journal of Psychiatric ResearchDocument7 pagesJournal of Psychiatric ResearchGiovane PiresNo ratings yet
- Rural OutreachDocument35 pagesRural OutreachPriyanshu Agrawal100% (1)
- Riem Badr, MD, FCAP Named Chief of Pathology and Laboratory ServicesDocument2 pagesRiem Badr, MD, FCAP Named Chief of Pathology and Laboratory ServicesPR.comNo ratings yet
- Company Name: Company Address:: Please Provide Copy of The PolicyDocument5 pagesCompany Name: Company Address:: Please Provide Copy of The Policyjosephr_4No ratings yet
- Acute EpiglottitisDocument12 pagesAcute EpiglottitisDr. Sarthak MishraNo ratings yet
- I. Choose The Meaning of The Underlined Words Using Context CluesDocument4 pagesI. Choose The Meaning of The Underlined Words Using Context CluesVanessaCastillo100% (1)
- Positive Youth Development ModuleDocument7 pagesPositive Youth Development ModuleRenny BrisonNo ratings yet
- Society Achievers June 2023Document92 pagesSociety Achievers June 2023magnatepublishingpvtltdNo ratings yet
- Laporan SP3 LB1Document35 pagesLaporan SP3 LB1Citra AuliyaNo ratings yet
- Idusohan Moizer2013Document12 pagesIdusohan Moizer2013patricia lodeiroNo ratings yet
- Tarlac State University: Code Remarks Subject Title Final Grade Credit Units Class Section RE-ExamDocument1 pageTarlac State University: Code Remarks Subject Title Final Grade Credit Units Class Section RE-ExamNicole Anne TungolNo ratings yet
- Summative AssessmentDocument4 pagesSummative Assessmentapi-349641989No ratings yet
- Case Manager (Senderos) : Morrison - Child & Family ServicesDocument2 pagesCase Manager (Senderos) : Morrison - Child & Family ServicesJamie RobinsonNo ratings yet
- Screenshot 2023-06-06 at 20.22.37Document8 pagesScreenshot 2023-06-06 at 20.22.37Ovidiu-Lucian BajenaruNo ratings yet
- Integumentary PT AssessmentDocument12 pagesIntegumentary PT AssessmentkumaninaNo ratings yet
- Dr. Ahmed Curriculum 2019Document9 pagesDr. Ahmed Curriculum 2019Dr.Ahmed AlnoumanNo ratings yet