Professional Documents
Culture Documents
Pulmonary Alveolar Microlithiasis Complicated by Tuberculosis
Pulmonary Alveolar Microlithiasis Complicated by Tuberculosis
Uploaded by
Balla ElkhiderOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pulmonary Alveolar Microlithiasis Complicated by Tuberculosis
Pulmonary Alveolar Microlithiasis Complicated by Tuberculosis
Uploaded by
Balla ElkhiderCopyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
Images in Clinical Medicine
Chana A. Sacks, M.D., Editor
Pulmonary Alveolar Microlithiasis
Complicated by Tuberculosis
A B C
A
Gunar Günther, M.D. 36-year-old woman presented to the outpatient clinic with a
Chalese Einbeck, M.D. 2-month history of fever, night sweats, cough, and worsening shortness of
Katutura State Hospital breath. On examination, her oxygen saturation was 88% while she was
Windhoek, Namibia breathing ambient air. A chest radiograph showed widespread fine micronodular
gunar.guenther@insel.ch opacities with a “sandstorm” appearance (Panel A). Computed tomography of the
chest revealed calcified micronodules, ground-glass opacities, and a cavitation
(Panel B). A sputum smear was negative for acid-fast bacilli. Subsequently, a trans-
bronchial biopsy was performed, and pathological examination of the tissue re-
vealed microliths (Panel C, arrow). The bronchial aspirate was positive for Myco-
bacterium tuberculosis. Testing for human immunodeficiency virus antibodies was
negative. A diagnosis of pulmonary alveolar microlithiasis complicated by tuber-
culosis was made. The patient began treatment for tuberculosis. Four weeks later,
the fever, night sweats, and cough had abated, but her shortness of breath per-
sisted. Lung transplantation — the only established treatment for pulmonary
alveolar microlithiasis — was not an available intervention in this case owing to
resource constraints.
DOI: 10.1056/NEJMicm2028047
Copyright © 2021 Massachusetts Medical Society.
e36 n engl j med 384;10 nejm.org March 11, 2021
The New England Journal of Medicine
Downloaded from nejm.org on March 15, 2021. For personal use only. No other uses without permission.
Copyright © 2021 Massachusetts Medical Society. All rights reserved.
You might also like
- Catana Brown - Virginia C Stoffel - Jaime Munoz - Occupational Therapy in Mental Health - A Vision For Participation-F. A. Davis Company (2019) PDFDocument844 pagesCatana Brown - Virginia C Stoffel - Jaime Munoz - Occupational Therapy in Mental Health - A Vision For Participation-F. A. Davis Company (2019) PDFRoss50% (6)
- Amanda Carfagnini Weebly ResumeDocument3 pagesAmanda Carfagnini Weebly Resumeapi-400235950No ratings yet
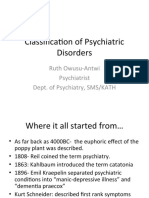
- Copy-Classification of Psychiatric DisordersDocument56 pagesCopy-Classification of Psychiatric Disordersshadrach bineyNo ratings yet
- MRCOG Part 2 Exam March 2016Document30 pagesMRCOG Part 2 Exam March 2016Hasan Dahamsheh86% (7)
- Infective EndocarditiDocument31 pagesInfective EndocarditiMansi DabolaNo ratings yet
- APLS Aide MemoireDocument2 pagesAPLS Aide Memoirecolinj100% (1)
- Leadership Skills For NursesDocument34 pagesLeadership Skills For NursesAdelaine Dalang-Ano100% (2)
- Nejmicm 2114345Document1 pageNejmicm 2114345jone6No ratings yet
- Painful Nodules On The Arms: Images in Clinical MedicineDocument1 pagePainful Nodules On The Arms: Images in Clinical MedicineBalla ElkhiderNo ratings yet
- Mycoplasma Pneumoniae-Associated Mucositis: Images in Clinical MedicineDocument1 pageMycoplasma Pneumoniae-Associated Mucositis: Images in Clinical MedicineAbo Marwan AlhomsiNo ratings yet
- Acquired Hypertrichosis LanuginosaDocument1 pageAcquired Hypertrichosis LanuginosaDaniela SerbanNo ratings yet
- Medicine: An Unusual Extranodal Natural Killer/t-Cell Lymphoma Presenting As Chronic LaryngitisDocument4 pagesMedicine: An Unusual Extranodal Natural Killer/t-Cell Lymphoma Presenting As Chronic Laryngitisnurul atika havizNo ratings yet
- Tuberculosis of The FingerDocument1 pageTuberculosis of The FingerGipsi MartinezNo ratings yet
- Nejmicm 1616156Document1 pageNejmicm 1616156Lucas AnicichNo ratings yet
- REPORTE CASO TBC y COVID 19Document6 pagesREPORTE CASO TBC y COVID 19Farmaco VigilanciaNo ratings yet
- Usg Abses ParuDocument2 pagesUsg Abses Parugiant nitaNo ratings yet
- Nejmicm 2216444Document1 pageNejmicm 2216444Mihaela BulboreaNo ratings yet
- Laryngocele: Images in Clinical MedicineDocument1 pageLaryngocele: Images in Clinical MedicineUzair KhanNo ratings yet
- Nejmicm 2211399Document1 pageNejmicm 2211399Muthia Farah AshmaNo ratings yet
- 10 1056@NEJMicm1911882Document1 page10 1056@NEJMicm1911882tabareeNo ratings yet
- Nej M CPC 2201244Document10 pagesNej M CPC 2201244ahmad saadNo ratings yet
- Nejmcpc 2115847Document10 pagesNejmcpc 2115847j8hcyh8j2jNo ratings yet
- Lung Poorly Differentiated Adenocarcinoma With Cerebral MetastasesDocument2 pagesLung Poorly Differentiated Adenocarcinoma With Cerebral MetastasesasclepiuspdfsNo ratings yet
- Case 24-2022: A 31-Year-Old Man With Perianal and Penile Ulcers, Rectal Pain, and RashDocument10 pagesCase 24-2022: A 31-Year-Old Man With Perianal and Penile Ulcers, Rectal Pain, and RashCorina OanaNo ratings yet
- Bartonella Neuroretinitis: Images in Clinical MedicineDocument1 pageBartonella Neuroretinitis: Images in Clinical MedicineBalla ElkhiderNo ratings yet
- 2013 9 1 045 ChuangDocument8 pages2013 9 1 045 ChuangRamaMahardikaNo ratings yet
- JCM 00137-21Document6 pagesJCM 00137-21lenithNo ratings yet
- Case 12-2020: A 24-Year-Old Man With Fever, Cough, and DyspneaDocument10 pagesCase 12-2020: A 24-Year-Old Man With Fever, Cough, and DyspneatabareeNo ratings yet
- Hussain 2024Document6 pagesHussain 2024jose mendozaNo ratings yet
- Confirmed Tuberculous Brain Miliary in An Immunocompetent Patient: A Case ReportDocument3 pagesConfirmed Tuberculous Brain Miliary in An Immunocompetent Patient: A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Disseminated Tuberculous Myositis in A Child With Acut 2009 Pediatrics NeoDocument4 pagesDisseminated Tuberculous Myositis in A Child With Acut 2009 Pediatrics NeoFrankenstein MelancholyNo ratings yet
- Medicina 58 01353 v4Document13 pagesMedicina 58 01353 v4PREEDIPAT PHINTHIPNo ratings yet
- 10 1056@NEJMcpc1913468 PDFDocument10 pages10 1056@NEJMcpc1913468 PDFAbdelkader HociniNo ratings yet
- Meningitis BacterianaDocument13 pagesMeningitis BacterianaFanny Mariela AroNo ratings yet
- Nej Mic M 1609306Document1 pageNej Mic M 1609306anggiNo ratings yet
- Case Bezold AbscessDocument3 pagesCase Bezold AbscessCarimaGhalieNo ratings yet
- Seminar: Diederik Van de Beek, Matthijs C Brouwer, Uwe Koedel, Emma C WallDocument13 pagesSeminar: Diederik Van de Beek, Matthijs C Brouwer, Uwe Koedel, Emma C WallNestor AmaroNo ratings yet
- S221326002030504XDocument12 pagesS221326002030504XJocilene Dantas Torres NascimentoNo ratings yet
- AbscessDocument12 pagesAbscesslittlecandiesNo ratings yet
- Catastrophic Cerebral Hemorrhage and Edema in A Patient With Pneumococcal MeningitisDocument3 pagesCatastrophic Cerebral Hemorrhage and Edema in A Patient With Pneumococcal MeningitisRizky Ishak PridataNo ratings yet
- Mediastinal Abscess After EndobronchialDocument3 pagesMediastinal Abscess After EndobronchialDm LdNo ratings yet
- Bronchiectasis - Diagnosis and TreatmentDocument9 pagesBronchiectasis - Diagnosis and Treatmentalfred1294No ratings yet
- Lung Abscess Secondary To Lung Cancer With Eikenella Corrodens and Streptococcus Anginosus: A Case ReportDocument6 pagesLung Abscess Secondary To Lung Cancer With Eikenella Corrodens and Streptococcus Anginosus: A Case ReportWidiaika Melrisda1106No ratings yet
- Tuberculosis of The Nasal Cavities About Four CasesDocument5 pagesTuberculosis of The Nasal Cavities About Four CasesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- MAR 3 Primary HyperoxaluriaDocument1 pageMAR 3 Primary HyperoxaluriaED SANNo ratings yet
- Tuberculosis of Sphenoid Sinus Report of Two CasesDocument4 pagesTuberculosis of Sphenoid Sinus Report of Two CasesDevikaNo ratings yet
- Blastic Plasmacytoid Dendritic-Cell Neoplasm: Images in Clinical MedicineDocument1 pageBlastic Plasmacytoid Dendritic-Cell Neoplasm: Images in Clinical MedicineJuan JoseNo ratings yet
- Community-Acquired Bacterial Meningitis (Van de Beek)Document13 pagesCommunity-Acquired Bacterial Meningitis (Van de Beek)gaz.med20No ratings yet
- 1-S2.0-S1726490112000895-Main Baru - En.idDocument5 pages1-S2.0-S1726490112000895-Main Baru - En.idHenandwita Fadilla PravitasariNo ratings yet
- Case 2-2022: A 70-Year-Old Man With A Recurrent Left Pleural EffusionDocument10 pagesCase 2-2022: A 70-Year-Old Man With A Recurrent Left Pleural Effusionpogesil46No ratings yet
- Piis0002962919300771 Presentacion de CasoDocument2 pagesPiis0002962919300771 Presentacion de Casoveronica alexandra navarroNo ratings yet
- Congenital Tuberculosis in A Premature InfantDocument6 pagesCongenital Tuberculosis in A Premature InfantTwhieNo ratings yet
- ECMM Guidelines For MucormycosisDocument17 pagesECMM Guidelines For MucormycosisSaurabh AgrawalNo ratings yet
- Wa0015.4Document7 pagesWa0015.4jeyiy92174No ratings yet
- ActaNCh 142 1 067 CandidaInfectionCSFDocument9 pagesActaNCh 142 1 067 CandidaInfectionCSFMutasem KhawaldehNo ratings yet
- Laryngeal Tuberculosis - A Neglected Disease That Can Mimic Laryngeal CarcinomaDocument8 pagesLaryngeal Tuberculosis - A Neglected Disease That Can Mimic Laryngeal CarcinomagremmyshelbyNo ratings yet
- ScrofulodermDocument4 pagesScrofulodermIzmi AzizahNo ratings yet
- Emphysema in Young AdultDocument9 pagesEmphysema in Young AdultCorina GrosuNo ratings yet
- 273 Full PDFDocument4 pages273 Full PDFAngelica Maria Rueda SerranoNo ratings yet
- Image DownloadDocument6 pagesImage DownloadRosel RomarateNo ratings yet
- RX Ileus Meconial CFDocument1 pageRX Ileus Meconial CFRaluca MosoiaNo ratings yet
- Disseminated Miliary Cerebral Candidiasis: Candida Albicans Is The Most Common Nos-C AlbicansDocument4 pagesDisseminated Miliary Cerebral Candidiasis: Candida Albicans Is The Most Common Nos-C Albicansdrian pamungkasNo ratings yet
- Ijhs 12577+883 892Document10 pagesIjhs 12577+883 892hai1No ratings yet
- Tuberculosis of The Spinal Cord.5Document15 pagesTuberculosis of The Spinal Cord.5noiNo ratings yet
- Rat Bite Fever: Images in Clinical MedicineDocument1 pageRat Bite Fever: Images in Clinical MedicineAbo Marwan AlhomsiNo ratings yet
- Diagnostics: Multi-Channel Based Image Processing Scheme For Pneumonia IdentificationDocument26 pagesDiagnostics: Multi-Channel Based Image Processing Scheme For Pneumonia IdentificationAk shatha SNo ratings yet
- Neurosciences Research: Volume 3From EverandNeurosciences Research: Volume 3S EhrenpreisNo ratings yet
- Dissociative Disorders: Halima Sadia Qureshi Lecturer/ Clinical Psychologist PPD, BuicDocument16 pagesDissociative Disorders: Halima Sadia Qureshi Lecturer/ Clinical Psychologist PPD, BuicHalima S QureshiNo ratings yet
- A CDDocument54 pagesA CDDoc QueenieNo ratings yet
- Daniels Criteria - EKG in PEDocument10 pagesDaniels Criteria - EKG in PEbrookswalsh100% (2)
- Natural Trans Fats in Milk - Are Trans Fats Good For YouDocument16 pagesNatural Trans Fats in Milk - Are Trans Fats Good For YouJosemar SantosNo ratings yet
- How Satisfied Are Patients Attending A Nigerian Eye Clinic in University of Calabar Teaching HospitalDocument9 pagesHow Satisfied Are Patients Attending A Nigerian Eye Clinic in University of Calabar Teaching HospitalEditor_IAIMNo ratings yet
- Chromosomal Disorder WebquestDocument2 pagesChromosomal Disorder WebquestEmmy CNo ratings yet
- Need Roles and Importance of Legislation in Building IndustryDocument6 pagesNeed Roles and Importance of Legislation in Building Industry12483.2020No ratings yet
- Medical Examinations of Seafarers, ExplanationDocument3 pagesMedical Examinations of Seafarers, ExplanationGinalyn QuimsonNo ratings yet
- Fortified Instant Noodle SpecsDocument4 pagesFortified Instant Noodle Specsnietz2No ratings yet
- MCQsin ENTwith Explanations Module 2 OtologyDocument7 pagesMCQsin ENTwith Explanations Module 2 OtologyFatina AryanNo ratings yet
- Unit 4 Written Assiignment RDocument4 pagesUnit 4 Written Assiignment RJackson LtorishaNo ratings yet
- Blood Drawings For Human Subject ResearchDocument32 pagesBlood Drawings For Human Subject ResearchnNo ratings yet
- Rabies PresentationDocument23 pagesRabies PresentationAvdhesh YadavNo ratings yet
- Risk Analysis in Food Safety - A Fresh TakeDocument7 pagesRisk Analysis in Food Safety - A Fresh TakePatrick EmbwagaNo ratings yet
- Gendrano Resume 2Document1 pageGendrano Resume 2Cep Loreine GendranoNo ratings yet
- MEDICARDDocument19 pagesMEDICARDSrcdc CooperativeNo ratings yet
- Sample Family Nursing Care PlanDocument8 pagesSample Family Nursing Care PlanReygie MataNo ratings yet
- Health Safety and Nutrition Resource GuideDocument14 pagesHealth Safety and Nutrition Resource Guideapi-516280936No ratings yet
- Study Guide Cycling and RaquetalDocument14 pagesStudy Guide Cycling and RaquetalIvanakbarPurwamaskaNo ratings yet
- Podcaster Inc Issue 1Document38 pagesPodcaster Inc Issue 1Hubert NomamiukorNo ratings yet
- Current TrendDocument4 pagesCurrent TrendShane Jay FabugaisNo ratings yet
- Personal Development: Senior High SchoolDocument30 pagesPersonal Development: Senior High SchoolElmer EmperosoNo ratings yet
- New Zealand Data Sheet: Amoxiclav MultichemDocument17 pagesNew Zealand Data Sheet: Amoxiclav MultichemdoodrillNo ratings yet