Professional Documents
Culture Documents
Timing and Management of Inguinal Hernia in The Premature Baby
Uploaded by
RENATA ULI AVIOLAOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Timing and Management of Inguinal Hernia in The Premature Baby
Uploaded by
RENATA ULI AVIOLACopyright:
Available Formats
Review Article
Timing and Management of Inguinal Hernia in
the Premature Baby
Alessio Pini Prato1 Germana Casaccia1 Rossella Arnoldi1
1 Department of Pediatric Surgery, Alessandria Children Hospital, Address for correspondence Alessio Pini Prato, MD, Department of
Alessandria, Italy Pediatric Surgery, Alessandria Children Hospital, Spalto Marengo,
46, Alessandria 15100, Italy (e-mail: a.piniprato@gmail.com).
Eur J Pediatr Surg
Abstract Inguinal hernias in children occur with a prevalence ranging from 3 to 5%. The likelihood
of a symptomatic patent processus vaginalis is significantly higher in preterms, as
reported by most series. As a consequence, inguinal hernia represents the most
common condition requiring surgical repair in the neonate and preterm baby. Surgery
aims at avoiding and preventing intestinal and gonadal lesions related to incarceration.
Downloaded by: BIBLIOTHEQUE UNIV PARIS 5. Copyrighted material.
Nonetheless, hernia repair is technically demanding, with a relatively high risk of
complications including recurrence and testicular atrophy. This paper will address
Keywords some of most debated aspect of inguinal hernia management in preterms babies. The
► inguinal hernia authors will discuss anesthesiological implications, available surgical techniques,
► preterm optimal timing for surgery, and reasons for possible contralateral groin exploration.
► neonate The authors will also discuss literature evidences and will propose their own behavior to
► surgery provide an algorithm for the correct management of neonates and ex-preterms with
► laparoscopy inguinal hernia.
Introduction hernia in case of asymptomatic PPV has been estimated to be
more than 25%,5 there is still debate on what to do to prevent
Inguinal hernias in children occur with a prevalence ranging metachrony.
from 3 to 5%.1,2 It occurs as a consequence of a patent processus Based on previous epidemiological data, inguinal hernia
vaginalis (PPV) that can become symptomatic due to the represents the most common condition requiring surgical
sliding of bowel loops, ovary, omentum, or other intra-abdom- repair in the neonate and preterm baby. Even so, the procedure
inal organ in its contest. The likelihood of a symptomatic PPV is in preterms can be technically demanding with a potential risk
significantly higher in preterms who can experience inguinal for severe complications. This is the reason why inguinal
hernias in approximately 20% of cases, as reported in most herniotomy in neonates and preterms is considered a major
series.3 As for the general pediatric population, gender dis- procedure that is performed only by consultants or senior
tribution shows a strong male preponderance, and right-sided resident/registrars.6
hernias predominate over left-sided ones. Bilateral hernias Although most surgeons would advocate early repair,1,6
have a higher incidence in neonates and preterms. Of note, given the lack of definitive data, optimal timing for inguinal
previous studies, such as those by Holcomb et al, demonstrated herniotomy in neonates and preterms remains debatable.
that asymptomatic PPVs can be detected in nearly 60% of Surgical repair aims at avoiding or preventing intestinal and
patients with unilateral symptomatic groin hernias, with an gonadal sequelae related to incarceration, whose risk de-
inverse relationship with patients’ age.1,2,4 Roughly 80% of creases during growth but can be as high as 60% before
neonates, over 60% of infants, 30% of children younger than 1, 6 months of age.1,6 These risks must be balanced against the
and 15% of those younger than 5 years carry an asymptomatic risk for potential operative and anesthetic complications. In
PPV.1 Although the risk of developing a subsequent inguinal fact, surgery is not harmless nor it is anesthesia. This paper will
received © Georg Thieme Verlag KG DOI https://doi.org/
October 26, 2017 Stuttgart · New York 10.1055/s-0037-1608802.
accepted ISSN 0939-7248.
October 30, 2017
Timing and Management of Inguinal Hernia in the Premature Baby Pini Prato et al.
discuss anesthesiological implications, available surgical tech- over neurodevelopment.16 Of note, recent evidences even
niques, debate regarding timing for surgery, and reasons for suggest a possible superiority of RA over GA for postopera-
possible contralateral groin exploration. The authors will tive management of neonates and infants undergoing ingu-
discuss literature evidences and will propose their own beha- inal hernia repair.17 Although carrying a potential risk for
vior to provide an algorithm for the correct management of cerebrospinal fluid leak and bleeding,18 RA should be at least
neonates and ex-preterms with inguinal hernia. considered a valid alternative to GA for neonates or preterms
requiring early inguinal herniotomy.
Considerations regarding Anesthesia
Surgical Treatment
Surgical trauma and stress responses lead to inflammatory
activation that can interfere with neurodevelopment. In 2013, General Considerations
Sanders et al performed a systematic review of available Hernia repair in preterms and neonates can be approached
studies regarding effects of surgery and general anesthesia with the “classic” open surgery or with minimally invasive
(GA) over development and suggested that metabolic stress laparoscopic approaches that are gaining importance and
responses, as those occurring in case of surgery, can lead to wider use in recent years.19–27 Nonetheless, the real preva-
glial activation and neuronal hyperexcitability in cortical and lence of surgeons resorting to the latter approach and the
subcortical areas, thus stimulating apoptosis and damage benefits of minimally invasive surgery for hernia repair remain
during well-defined vulnerable time periods.7 Other authors undetermined to date.1
Downloaded by: BIBLIOTHEQUE UNIV PARIS 5. Copyrighted material.
suggested that GA can interfere per se with neurodevelopment Inguinal hernia repair in neonates and infants can be a
and that this risk is higher if children are operated early.8,9 But technically demanding procedure even in experienced hands,
what should be considered the age limit for GA to determine with a relatively high risk of postoperative complications. They
negative effects? Zhang et al performed a meta-analysis of are reported to occur with a frequency from 6% to more than
paper published over a 10-year period focusing on neurode- 10% and include bleeding, wound infection, recurrence, post-
velopmental outcome following GA. The authors concluded operative persistent hydrocele, testicular ascent, and testicular
that children who underwent GA up to the age of 3 have a atrophy.28–30 These complications have a threefold higher
moderately higher risk of neurodevelopmental disorders being incidence when compared with older children. A retrospective
those operated on at a later age basically unaffected.10 Though analysis by Baird et al confirmed a higher rate of complications
mostly retrospective, other studies confirmed this aspect. In in infants aged less than 43 weeks of postconceptual age at
particular, Dwyer et al performed an observational study on surgery. They speculated that thinner and friable PPV as well as
patients who underwent major surgery in the neonatal period fragile cord structures predispose to failure and other
and reported a neurodevelopmental effect of early surgery þ complications.31
GA. The authors reported mild delay, particularly in the area of Given the increased risk of testicular atrophy, which has
cognition, receptive language, and fine motor development.11 been reported to be as high as up to 10%,32 we recently looked
Based on in vitro and in vivo reports in animal models for preoperative risk factors and demonstrated in a unicentric
underlying the potential detrimental effects of anesthetic experience on more than 180 herniotomies in neonates and
agents over neurodevelopment, a recent randomized con- ex-preterm that preoperative incarceration significantly in-
trolled trial by Davidson et al compared regional anesthesia creases the likelihood of such a complication.6 This is not new
(RA) and GA in neonates, infants, and ex-preterms undergoing as other authors already suggested such a relationship33,34 but
inguinal hernia repair to determine the effects of GA in stresses the importance of correct timing for surgery with
neonates and ex-preterm. This trial failed to demonstrate adequate preoperative clinical surveillance.
major effects as neurodevelopment assessed by the age of 2
was not significantly affected by the chosen anesthetic plan.12
Available Surgical Techniques
Even so, the trial is still ongoing and we are still waiting the
results of 5-year neurodevelopmental assessment that could “Classic” Open Repair
better clarify this issue. On the other hand, in a secondary The classic skin incision at the inguinal crease leads to the
outcome analysis, the same study confirmed the higher risk of inguinal canal. Some surgeons will open the roof of the canal by
postoperative apnea related to GA administration and its dividing the external oblique fascia, as for older children,
potentially fatal effects if undetected.13 On the ground of these whereas others will go straight to the PPV distal to the external
considerations, this topic is still a matter of debate without inguinal ring. Extrainguinal approach is faster but requires
definitive answers reported so far. more experienced surgeons and theoretically increases the
Whether GA is harmful or not is thus yet to be determined. risk of recurrence due to the persistence of a patent stump that
Anyway, alternative options do exist and include RA (spinal can lead to recurrence or persistence in the medium-to-long
or caudal) without sedation. Many papers addressed this term. Other technical variations including external inguinal
issues, and many centers worldwide confirmed its feasibility, ring opening, twisting of the sac, and double ligation did not
with particular regard to inguinal hernia repair, even in show superior results when compared with a classic proce-
urgent cases.14,15 Furthermore, Williams et al in 2014, dure.35 As indicated previously, the risk of complication can be
reviewing 265 students who underwent RA in infancy, as high as 10%, with testicular atrophy being reported with a
confirmed that RA does not determine detrimental effects frequency ranging from 1 to 10%.6,28–30
European Journal of Pediatric Surgery
Timing and Management of Inguinal Hernia in the Premature Baby Pini Prato et al.
Open Repair and Diagnostic Laparoscopy relatively high risk of incarceration in the very first months of
Minimally invasive surgery is becoming increasingly popular life,6 surgery should be scheduled based on this aspect. Chen
even for newborns and preterms. Since the late 1990s, laparo- et al in 2009 reported a retrospective multicentric analysis on
scopy was used for diagnostic purposes to check the other side infants with inguinal hernia and concluded that waiting longer
of the groin to prevent the risk for metachronous hernias.36,37 than 14 days after diagnosis of inguinal hernia does increase the
risk of incarceration and subsequent complications.33 Similarly,
Laparoscopic Herniorrhaphy Vaos et al performed a retrospective analysis on infants with
Later on, laparoscopy was also introduced for the surgical inguinal hernia and concluded that waiting longer than 1 week
treatment.19,20 A provisional multicentric experience in 2002 significantly increases this risk.34 Lautz et al reported in 2011
by Schier et al reported good results of laparoscopic hernior- that surgery delayed beyond 40 weeks of postconceptual age
rhaphy, with 3.4% recurrence rate and only one case of testi- increases the risk of incarceration to more than 20% and that
cular atrophy over a series of 933 children aged on average this risk is further increased to nearly 30% when surgery is even
3 years.21 Since 2010, various authors have reported laparo- more delayed.38 A paper from Misra dating back to 2001
scopic inguinal hernia repair in neonates and ex-preterms. suggested to treat preterms before discharge to avoid incarcera-
Turial et al reported a series of 148 babies weighting less than tion but not as early as others previously suggested. The authors
5 kg with a reasonable recurrence rate (2%), no testicular stressed the importance of a strict clinical follow-up to avoid the
atrophy, and overall 6% reoperation rate due to recurrence or risks of testicular atrophy related to difficult dissection and vas
testicular ascent.22 The same authors focused on preterms and vessels manipulation.39
Downloaded by: BIBLIOTHEQUE UNIV PARIS 5. Copyrighted material.
babies and reported a higher but still reasonable recurrence Gholoum et al in 2010 addressed the issue of incarceration
rate (3.6%), a relatively high testicular ascent rate (nearly 10%), basing on ICD (International Classification of Diseases) coding
and no testicular atrophy. Noticeably, the authors reported a 7% and concluded that only a minority of infants with inguinal
incidence of anesthesiological issues.23 Esposito et al reported a hernia experience incarceration preoperatively and that a
series of neonates and ex-preterm weighting less than 3 kg at reasonable waiting time may not alter the outcome.40 In
surgery, with 4.4% recurrence rate, no testicular atrophy, and 2011, Lee et al reported a series of nearly 130 ex-preterms
15% of testicular ascent.24 The high rate of testicular ascent who underwent elective herniotomy after hospital discharge
with its subsequent need for orchiopexy prompted Shono et al and reported a zero incarceration rate in the waiting period.41
to focus on this issue. They concluded that the adherent sac can Based on these results, they supported the delay of hernia
somehow reduce the potential for testicular descent, thus repair in infants.
leading to subsequent need for orchiopexy,25 and that a strict When addressed within 5 to 6 kg, patients’ weight at
follow-up is mandatory to promptly identify this issue. surgery seem not to significantly interfere with complication
rates.6,28 Hughes et al published a series of more than 400
Percutaneous Internal Ring Suturing babies weighting on average less than 6 kg and reported that no
Although based on the same principles and risks of conven- significant differences in term of complication were observed
tional laparoscopic treatment, in 2006, Patkowski et al reported when comparing terms and ex-preterms, regardless of the
an innovative minimally invasive technique for inguinal hernia higher incidence of incarceration observed in the latter. These
repair called percutaneous internal ring suturing. The proce- results could suggest that incarceration does not interfere with
dure was adopted even in neonates and consisted of knot-tying the outcome, but these authors reported that nearly 50% of the
the internal ring through a 14-gauge needle under direct patients were lost on follow-up. Nevertheless, the authors
laparoscopic vision.26 The authors operated on 140 hernias, confirmed the higher likelihood of preterms to experience
with only three intraoperative complications and an impressive preoperative incarceration.28
success rate. In the long term, 2% recurrence and 4% hydrocele Of note, two surveys of the American Academy of Pediatrics
were reported. in 1993 and 2005 demonstrated a clear trend over early hernia
repair in neonates and ex-preterm with 63% of surgeons that in
Specific Anesthesiological Issues for Minimally 2005 declared that they would correct the hernia before dis-
Invasive Approach charge from neonatale intensive care unit (NICU) in order to
In a specific assessment of anesthesiological issues following avoid the consequences of preoperative incarceration. Only
laparoscopic hernia repair, Burgmeier and Schier reported a minority of pediatric surgeons would differ surgery to a later
5% anesthesiological issues in term babies and over 20% in stage.1
preterms. The authors speculated that specific preexisting
comorbidities can represent risk factors for cardiorespiratory What about Contralateral Exploration?
issues in case of laparoscopy.27 Nonetheless, laparoscopic In case laparoscopic approach is chosen, bilateral exploration
hernia repair is now being used worldwide,24,27 and many is straightforward and subsequent treatment can be under-
centers adopt the minimally invasive approach as the first taken during the same procedure. In case open approach is
choice for groin hernia repair in neonates. chosen, contralateral exploration implies doubling the risk of
vas and vessels traumatism. In 2016, Weaver et al assessed a
Timing for Repair series of 308 patients with an asymptomatic PPV detected
Given the linear relationship between preoperative incarcera- during a nonhernia laparoscopy and reported a very low
tion, and the subsequent risk for testicular atrophy and the incidence of subsequent clinically evident hernia (13%) after
European Journal of Pediatric Surgery
Timing and Management of Inguinal Hernia in the Premature Baby Pini Prato et al.
a mean 8-year follow-up. Those hernias presented within • Either open or minimally invasive approaches can be used to
9 months from laparoscopic detection and required surgical treat inguinal hernia in neonates and preterms. In case of
treatment.42 These results downgrade the risk of a PPV turning open surgery, the risk of cord manipulation and damage
symptomatic toward adulthood from 25 to 50% to less than should be taken into consideration. The same applies to the
15%.1,29 The likelihood of a contralateral PPV ranges from 20% risk of postoperative testicular ascent observed in case
to up to 70% according to literature.1,29,42 To conclude, when of minimally invasive approaches that may require subse-
approaching unilateral hernias with a classic open skin crease quent groin or testicular manipulation. The rationale of open
incision, we should explore up to 20 cords to avoid a single surgery is represented by the possibility to adopt RA,
metachronous hernia. In case of laparoscopy, we should per- whereas laparoscopy implies GA, which can be better ap-
form 5 useless closures of the internal inguinal ring in order to plied to patients without co-existing comorbidities.27
avoid a clinically evident metachronous hernia. As we have • As testicular atrophy correlates mostly with preopera-
already stated in a paper of ours that specifically addressed the tive incarceration, timing seems to be crucial. Literature
issue of metachronous hernias,6 routine contralateral explora- data demonstrate that no clear-cut indications regarding
tion has a negative risk–benefit ratio in males and should be timing for repair in neonates, infants, and ex-preterm
therefore avoided. In fact, the risk of surgical complications is exist. The majority of literature data suggest to operate
higher compared to that of potential complications related to a preterms and neonates, whose inguinal hernia was de-
contralateral patent PPV. tected during hospital stay, before discharge and those
who received a later diagnosis within 2 weeks from
Downloaded by: BIBLIOTHEQUE UNIV PARIS 5. Copyrighted material.
diagnosis, with adequate parent education regarding
Discussion and Recommendations
the risk of preoperative incarceration and appropriate
On the ground of literature review and previous considerations, surgical follow-up.
we can draw the following conclusions and recommendations: • Routine contralateral open cord exploration should be
• RA and GA are equally effective for the treatment of avoided. In case of laparoscopic approach, there is still
inguinal hernia in neonates and preterms babies, the debate regarding what to do with the contralateral PPV. If
latter being particularly prone to receive RA due to it is asymptomatic, it seems that a “wait-and-see” ap-
possible comorbidities contraindicating GA. proach should be preferred. In females, these options
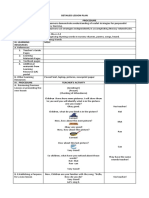
Fig. 1 Algorithm for neonatal inguinal hernia at Alessandria Children Hospital. Open surgery is used for most cases unless hernia is incarcerated
or recurrent (laparoscopy is used in those cases). Patients younger than 60 postconceptual weeks did require continuous overnight monitoring.
Metachronicity is considered only in case of females with unilateral left inguinal hernia. GA, general anesthesia; NICU, neonatal intensive care
unit; PCA, postconceptual age (weeks); RA, regional anesthesia.
European Journal of Pediatric Surgery
Timing and Management of Inguinal Hernia in the Premature Baby Pini Prato et al.
could be reassessed given the lower risk of complications 11 Dwyer GM, Walker K, Baur L, Badawi N. Developmental outcomes
and physical activity behaviour in children post major surgery: an
related to inguinal hernia repair. In fact, even in case of
observational study. BMC Pediatr 2016;16:123
open surgery, most of surgeons would operate bilaterally
12 Davidson AJ, Disma N, de Graaff JC, et al; GAS consortium.
in case of left-sided hernia given the higher likelihood of a Neurodevelopmental outcome at 2 years of age after general
contralateral PPV (left processus vaginalis obliterates ear- anaesthesia and awake-regional anaesthesia in infancy (GAS):
lier, thus increasing the risk of contralateral patency). an international multicentre, randomised controlled trial. Lancet
2016;387(10015):239–250
13 Davidson AJ, Morton NS, Arnup SJ, et al; General Anesthesia
Authors’ Preferred Approach compared to Spinal anesthesia (GAS) Consortium. Apnea after
awake regional and general anesthesia in infants: the general
In our Children Hospital, we adopt open approach for inguinal
anesthesia compared to spinal anesthesia study–comparing ap-
herniotomy (►Fig. 1). Whenever feasible, surgery is performed nea and neurodevelopmental outcomes, a randomized controlled
under RA. Laparoscopic approach is limited to patients with trial. Anesthesiology 2015;123(01):38–54
incarceration or recurrence, always under GA. We do schedule 14 Lambertz A, Schälte G, Winter J, et al. Spinal anesthesia for inguinal
preterms or neonates for herniotomy before discharge from hernia repair in infants: a feasible and safe method even in
emergency cases. Pediatr Surg Int 2014;30(10):1069–1073
NICU or within 2 weeks from diagnosis in case of outpatient
15 Maitra S, Baidya DK, Pawar DK, Arora MK, Khanna P. Epidural
diagnosis. We never explore the contralateral side in males, but anesthesia and analgesia in the neonate: a review of current
we explore it only in females with unilateral symptomatic left- evidences. J Anesth 2014;28(05):768–779
sided hernia. 16 Williams RK, Black IH, Howard DB, et al. Cognitive outcome after
Downloaded by: BIBLIOTHEQUE UNIV PARIS 5. Copyrighted material.
Postoperatively, in case of GA, we keep neonates and spinal anesthesia and surgery during infancy. Anesth Analg 2014;
preterms up to 60 postconceptual week overnight with 119(03):651–660
17 Gurria J, Kuo P, Kao A, Christensen L, Holterman A. General
continuous monitoring. Those patients receiving RA are
endotracheal vs. non-endotracheal regional anesthesia for elec-
discharged within 12 hours from surgery, provided no sur- tive inguinal hernia surgery in very preterm neonates: a single
gical issues of discomfort are reported. institution experience. J Pediatr Surg 2017;52(01):56–59
18 Allee JI, Goins KM, Berde CB, McCann ME. A case of cerebrospinal
fluid leak in an infant after spinal anesthesia. J Clin Anesth 2013;
Conflict of Interest 25(03):217–219
None. 19 Schier F. Laparoscopic herniorrhaphy in girls. J Pediatr Surg 1998;
33(10):1495–1497
20 Schier F. Laparoscopic surgery of inguinal hernias in children–
References initial experience. J Pediatr Surg 2000;35(09):1331–1335
1 Wang KS; Committee on Fetus and Newborn, American Academy 21 Schier F, Montupet P, Esposito C. Laparoscopic inguinal hernior-
of Pediatrics; Section on Surgery, American Academy of Pedia- rhaphy in children: a three-center experience with 933 repairs.
trics. Assessment and management of inguinal hernia in infants. J Pediatr Surg 2002;37(03):395–397
Pediatrics 2012;130(04):768–773 22 Turial S, Enders J, Krause K, Schier F. Laparoscopic inguinal hernior-
2 Grosfeld JL. Current concepts in inguinal hernia in infants and rhaphy in babies weighing 5 kg or less. Surg Endosc 2011;25(01):
children. World J Surg 1989;13(05):506–515 72–78
3 Harper RG, Garcia A, Sia C. Inguinal hernia: a common problem of 23 Turial S, Enders J, Krause K, Schier F. Laparoscopic inguinal
premature infants weighing 1,000 grams or less at birth. Pedia- herniorrhaphy in premature infants. Eur J Pediatr Surg 2010;20
trics 1975;56(01):112–115 (06):371–374
4 Holcomb GW III, Brock JW III, Morgan WM III. Laparoscopic 24 Esposito C, Turial S, Escolino M, et al. Laparoscopic inguinal hernia
evaluation for a contralateral patent processus vaginalis. J Pediatr repair in premature babies weighing 3 kg or less. Pediatr Surg Int
Surg 1994;29(08):970–973, discussion 974 2012;28(10):989–992
5 McGregor DB, Halverson K, McVay CB. The unilateral pediatric 25 Shono T, Izaki T, Nakahori R, Yoshimaru K. Testicular ascent after
inguinal hernia: should the contralateral side by explored? J Pediatr laparoscopic percutaneous extraperitoneal closure for inguinal
Surg 1980;15(03):313–317 hernias. Eur J Pediatr Surg 2015;25(01):105–108
6 Pini Prato A, Rossi V, Mosconi M, et al. Inguinal hernia in neonates 26 Patkowski D, Czernik J, Chrzan R, Jaworski W, Apoznański W.
and ex-preterm: complications, timing and need for routine Percutaneous internal ring suturing: a simple minimally invasive
contralateral exploration. Pediatr Surg Int 2015;31(02):131–136 technique for inguinal hernia repair in children. J Laparoendosc
7 Sanders RD, Hassell J, Davidson AJ, Robertson NJ, Ma D. Impact of Adv Surg Tech A 2006;16(05):513–517
anaesthetics and surgery on neurodevelopment: an update. Br J 27 Burgmeier C, Schier F. Cardiorespiratory complications after
Anaesth 2013;110(Suppl 1):i53–i72 laparoscopic hernia repair in term and preterm babies. J Pediatr
8 Block RI, Thomas JJ, Bayman EO, Choi JY, Kimble KK, Todd MM. Are Surg 2013;48(09):1972–1976
anesthesia and surgery during infancy associated with altered 28 Hughes K, Horwood JF, Clements C, Leyland D, Corbett HJ.
academic performance during childhood? Anesthesiology 2012; Complications of inguinal herniotomy are comparable in term
117(03):494–503 and premature infants. Hernia 2016;20(04):565–569
9 DiMaggio C, Sun LS, Kakavouli A, Byrne MW, Li G. A retrospective 29 Rosenberg J. Pediatric inguinal hernia repair-a critical appraisal.
cohort study of the association of anesthesia and hernia repair Hernia 2008;12(02):113–115
surgery with behavioral and developmental disorders in young 30 Takahashi A, Toki F, Yamamoto H, Otake S, Oki Y, Kuwano H.
children. J Neurosurg Anesthesiol 2009;21(04):286–291 Outcomes of herniotomy in premature infants: recent 10 year
10 Zhang H, Du L, Du Z, Jiang H, Han D, Li Q. Association between experience. Pediatr Int 2012;54(04):491–495
childhood exposure to single general anesthesia and neurodeve- 31 Baird R, Gholoum S, Laberge JM, Puligandla P. Prematurity, not age
lopment: a systematic review and meta-analysis of cohort study. at operation or incarceration, impacts complication rates of
J Anesth 2015;29(05):749–757 inguinal hernia repair. J Pediatr Surg 2011;46(05):908–911
European Journal of Pediatric Surgery
Timing and Management of Inguinal Hernia in the Premature Baby Pini Prato et al.
32 Fette AM, Höllwarth ME. Special aspects of neonatal inguinal 38 Lautz TB, Raval MV, Reynolds M. Does timing matter? A national
hernia and herniotomy. Hernia 2001;5(02):92–96 perspective on the risk of incarceration in premature neonates
33 Chen LE, Zamakhshary M, Foglia RP, Coplen DE, Langer JC. Impact with inguinal hernia. J Pediatr 2011;158(04):573–577
of wait time on outcome for inguinal hernia repair in infants. 39 Misra D. Inguinal hernias in premature babies: wait or operate?
Pediatr Surg Int 2009;25(03):223–227 Acta Paediatr 2001;90(04):370–371
34 Vaos G, Gardikis S, Kambouri K, Sigalas I, Kourakis G, Petoussis G. 40 Gholoum S, Baird R, Laberge JM, Puligandla PS. Incarceration rates
Optimal timing for repair of an inguinal hernia in premature in pediatric inguinal hernia: do not trust the coding. J Pediatr Surg
infants. Pediatr Surg Int 2010;26(04):379–385 2010;45(05):1007–1011
35 Ibrahim M, Ladan MA, Abdussalam US, et al. Open inguinal herniot- 41 Lee SL, Gleason JM, Sydorak RM. A critical review of premature
omy: analysis of variations. Afr J Paediatr Surg 2015;12(02):131–135 infants with inguinal hernias: optimal timing of repair, incarcera-
36 Rescorla FJ, West KW, Engum SA, Scherer LR III, Grosfeld JL. The tion risk, and postoperative apnea. J Pediatr Surg 2011;46(01):
“other side” of pediatric hernias: the role of laparoscopy. Am Surg 217–220
1997;63(08):690–693 42 Weaver KL, Poola AS, Gould JL, Sharp SW, St Peter SD, Holcomb
37 Chou TY, Chu CC, Diau GY, Wu CJ, Gueng MK. Inguinal hernia in GW III. The risk of developing a symptomatic inguinal hernia in
children: US versus exploratory surgery and intraoperative con- children with an asymptomatic patent processus vaginalis.
tralateral laparoscopy. Radiology 1996;201(02):385–388 J Pediatr Surg 2017;52(01):60–64
Downloaded by: BIBLIOTHEQUE UNIV PARIS 5. Copyrighted material.
European Journal of Pediatric Surgery
You might also like
- Incarceratedpediatric Hernias: Sophia A. Abdulhai,, Ian C. Glenn,, Todd A. PonskyDocument17 pagesIncarceratedpediatric Hernias: Sophia A. Abdulhai,, Ian C. Glenn,, Todd A. PonskyPhytoplankton DiatomsNo ratings yet
- Laparoscopic Hernia Repair in Neonates, Infants and ChildrenDocument9 pagesLaparoscopic Hernia Repair in Neonates, Infants and ChildrenErick OematanNo ratings yet
- Cesarean Scar Defect: A Prospective Study On Risk Factors: GynecologyDocument8 pagesCesarean Scar Defect: A Prospective Study On Risk Factors: Gynecologynuphie_nuphNo ratings yet
- Morini 2021Document14 pagesMorini 2021machalliNo ratings yet
- Inguinal and Scrotal Disorders: Diagnosis and TreatmentDocument11 pagesInguinal and Scrotal Disorders: Diagnosis and TreatmentPablo GuamanNo ratings yet
- Anesthetic Management in Pediatric General Surgery: Evolving and Current ConceptsFrom EverandAnesthetic Management in Pediatric General Surgery: Evolving and Current ConceptsSusan T. VergheseNo ratings yet
- Ijcm 2014071513394601 PDFDocument9 pagesIjcm 2014071513394601 PDFnurulrezqiaNo ratings yet
- Esposito 2016Document9 pagesEsposito 2016Krishna CaitanyaNo ratings yet
- ErniaDocument37 pagesErniaOskar MaNo ratings yet
- Anoplastia Percutanea 2022Document11 pagesAnoplastia Percutanea 2022Sandra Cárdenas HilasacaNo ratings yet
- Ding 2020Document6 pagesDing 2020Ridha Aswina DalimuntheNo ratings yet
- New Developments in Anal Surgery Congenital Ano RectalDocument5 pagesNew Developments in Anal Surgery Congenital Ano RectalOctavianus KevinNo ratings yet
- Current Postnatal Management of Antenatally Diagnosed HydronephrosisDocument8 pagesCurrent Postnatal Management of Antenatally Diagnosed HydronephrosisIoannis ValioulisNo ratings yet
- Fistula in AnoDocument5 pagesFistula in AnoIoannis ValioulisNo ratings yet
- Knowledge, Attitude and Practice of General Surgeons Regarding Paediatric Inguinal Hernia and HydroceleDocument5 pagesKnowledge, Attitude and Practice of General Surgeons Regarding Paediatric Inguinal Hernia and HydroceleriezanurdinsyahNo ratings yet
- Hernia InguinalDocument18 pagesHernia InguinalisabellaNo ratings yet
- Jurnal BedahDocument6 pagesJurnal Bedahyosep andrianu lorenNo ratings yet
- 2018, J, (Prevalensi) 1-S2.0-S2405857217300931-MainDocument8 pages2018, J, (Prevalensi) 1-S2.0-S2405857217300931-MainAyashopia AyaNo ratings yet
- Transverse Lie : Predisposing Factors, Maternal and Perinatal OutcomeDocument4 pagesTransverse Lie : Predisposing Factors, Maternal and Perinatal OutcomeErlangga DayudNo ratings yet
- Factores de Riesgo Asociados A Recidiva en Pacientes Con Antecedente de Plastia de Hernia Incisional en Centro Medico NavalDocument7 pagesFactores de Riesgo Asociados A Recidiva en Pacientes Con Antecedente de Plastia de Hernia Incisional en Centro Medico NavalIJAR JOURNALNo ratings yet
- Episiotomía Desgarro PerinealDocument9 pagesEpisiotomía Desgarro PerinealjigagomezNo ratings yet
- Burden of Adhesions in Abdominal and Pelvic SurgeryDocument15 pagesBurden of Adhesions in Abdominal and Pelvic SurgeryDian AdiNo ratings yet
- Contoversia de Hernia InguinalDocument13 pagesContoversia de Hernia InguinalOSCAR AUGUSTO QUESADA VEGANo ratings yet
- Meconium-Stained Amniotic Fluid: A Risk Factor For Postpartum HemorrhageDocument5 pagesMeconium-Stained Amniotic Fluid: A Risk Factor For Postpartum HemorrhagelaniNo ratings yet
- The Art of FetosDocument3 pagesThe Art of FetosDr Aprajita SinghNo ratings yet
- Laparoscopic Versus Open Inguinal Hernia Repair in Pediatric Patients: A Systematic ReviewDocument9 pagesLaparoscopic Versus Open Inguinal Hernia Repair in Pediatric Patients: A Systematic ReviewAbdul RahmanNo ratings yet
- Errores Defecto de ParedDocument7 pagesErrores Defecto de ParedAlan La TorreNo ratings yet
- Advancesinsurgeryfor Abdominalwalldefects: Gastroschisis and OmphaloceleDocument12 pagesAdvancesinsurgeryfor Abdominalwalldefects: Gastroschisis and OmphaloceleSitti HazrinaNo ratings yet
- Unukovych 2016Document7 pagesUnukovych 2016jdavies231No ratings yet
- Congenital Diaphragmatic Hernia Evidence ReviewDocument5 pagesCongenital Diaphragmatic Hernia Evidence ReviewElisabeth Agnes SidabutarNo ratings yet
- Cute Appendicitis in Children: Emergency Department Diagnosis and ManagementDocument13 pagesCute Appendicitis in Children: Emergency Department Diagnosis and ManagementMusyawarah MelalaNo ratings yet
- Hidronefrosisi 1Document12 pagesHidronefrosisi 1Zwinglie SandagNo ratings yet
- Laparoschisis: About A Case Report and Literature ReviewDocument10 pagesLaparoschisis: About A Case Report and Literature ReviewIJAR JOURNALNo ratings yet
- International Journal of Surgery: Humphrey G.M. Walker, Ahmad Al Samaraee, Sarah J. Mills, M. Reza KalbassiDocument7 pagesInternational Journal of Surgery: Humphrey G.M. Walker, Ahmad Al Samaraee, Sarah J. Mills, M. Reza KalbassiJason CalvinNo ratings yet
- Fetal Medicine Past, Present, and Future - LancetDocument1 pageFetal Medicine Past, Present, and Future - LancetlariialvezNo ratings yet
- Umbilical Cord ClampingDocument10 pagesUmbilical Cord ClampingTika WulandariNo ratings yet
- Indications and Risks of Vacuum Assisted Deliveries.: OriginalDocument2 pagesIndications and Risks of Vacuum Assisted Deliveries.: OriginalgagagigoNo ratings yet
- 10 1016@j Jpedsurg 2020 02 024Document6 pages10 1016@j Jpedsurg 2020 02 024Rizka Desti AyuniNo ratings yet
- Journal of Pediatric Surgery Case ReportsDocument3 pagesJournal of Pediatric Surgery Case ReportsKhaidar Ismail JuWiNo ratings yet
- Seminars in Pediatric Surgery: Progress in Anesthesia and Management of The Newborn Surgical PatientDocument5 pagesSeminars in Pediatric Surgery: Progress in Anesthesia and Management of The Newborn Surgical PatientAsif KhanNo ratings yet
- Mon 2018Document7 pagesMon 2018Nadieda Ayu MarthalitasariNo ratings yet
- Umbilical Hernia: When and How: Raquel A. Maia, Hrishikesh P. Salgaonkar, Davide Lomanto, Lynette LooDocument8 pagesUmbilical Hernia: When and How: Raquel A. Maia, Hrishikesh P. Salgaonkar, Davide Lomanto, Lynette LooZauzaa NabilaNo ratings yet
- Screening For Placenta Accreta at 11-14 Weeks of GestationDocument6 pagesScreening For Placenta Accreta at 11-14 Weeks of Gestationjuljim01No ratings yet
- Hernias e HidrocelesDocument8 pagesHernias e HidrocelesisabellaNo ratings yet
- Fetal Surgery - The Ochsner Experience With in Utero Spina Bifida RepairDocument6 pagesFetal Surgery - The Ochsner Experience With in Utero Spina Bifida RepairJusten ThompsonNo ratings yet
- 984 Pediatric Hernias and Hydrocele Pediatric SurgeryDocument27 pages984 Pediatric Hernias and Hydrocele Pediatric SurgeryVijay KumarNo ratings yet
- Cranial Ultrasound Findings in Late Preterm Infants and Correlation With Perinatal Risk FactorsDocument7 pagesCranial Ultrasound Findings in Late Preterm Infants and Correlation With Perinatal Risk FactorsM Ibnu Rahman SyahNo ratings yet
- Regional Anesthesia in Pediatric Orthopedics A CL 2022Document9 pagesRegional Anesthesia in Pediatric Orthopedics A CL 2022Alejandra SanchezNo ratings yet
- VP shunt and complicationDocument5 pagesVP shunt and complicationFabiola VaniaNo ratings yet
- Fetoscopic Endoluminal Tracheal Occlusion and ReesDocument9 pagesFetoscopic Endoluminal Tracheal Occlusion and ReesnNo ratings yet
- What's New in Pediatric Orthopaedics: J Bone Joint Surg AmDocument10 pagesWhat's New in Pediatric Orthopaedics: J Bone Joint Surg AmYariel AraujoNo ratings yet
- Lateral ColposuspentionDocument24 pagesLateral ColposuspentionMohammad QuayyumNo ratings yet
- Factors for Successful Nonsurgical Treatment of Pediatric Peritonsillar AbscessDocument4 pagesFactors for Successful Nonsurgical Treatment of Pediatric Peritonsillar AbscessruthameliapNo ratings yet
- Jurnal 2018Document9 pagesJurnal 2018aulNo ratings yet
- Inguinal Hernias and Hydroceles ExplainedDocument7 pagesInguinal Hernias and Hydroceles ExplainedEmma AssagafNo ratings yet
- 2010 TEPTSemin Pediatr Surg 2010 May 19296106Document12 pages2010 TEPTSemin Pediatr Surg 2010 May 19296106Riyan DarundryoNo ratings yet
- Acute Appendicitis in Childhood and Adulthood: MedicineDocument15 pagesAcute Appendicitis in Childhood and Adulthood: MedicineTran DuongNo ratings yet
- Editorial: Ureteropelvic Junction Obstruction (Upjo) in InfantsDocument2 pagesEditorial: Ureteropelvic Junction Obstruction (Upjo) in InfantssandyNo ratings yet
- Thesis On Ectopic Pregnancy in IndiaDocument7 pagesThesis On Ectopic Pregnancy in Indiaynwtcpwff100% (2)
- JournalDocument6 pagesJournalYosuaNo ratings yet
- Proportions and Reasons For Breast Conservation Surgery and Modified Radical Mastectomy in Early Breast CarcinomaDocument6 pagesProportions and Reasons For Breast Conservation Surgery and Modified Radical Mastectomy in Early Breast CarcinomaRENATA ULI AVIOLANo ratings yet
- Comparison of Breast-Conserving Surgery With Mastectomy in Locally Advanced Breast Cancer After Good Response To Neoadjuvant ChemotherapyDocument9 pagesComparison of Breast-Conserving Surgery With Mastectomy in Locally Advanced Breast Cancer After Good Response To Neoadjuvant ChemotherapyRENATA ULI AVIOLANo ratings yet
- Acute Mesenteric Ischemia: Guidelines of The World Society of Emergency SurgeryDocument11 pagesAcute Mesenteric Ischemia: Guidelines of The World Society of Emergency SurgeryUleonelNo ratings yet
- Diagnostic Accuracy of Hematological Parameters in Acute Mesenteric T Ischemia-A Systematic ReviewDocument10 pagesDiagnostic Accuracy of Hematological Parameters in Acute Mesenteric T Ischemia-A Systematic ReviewRENATA ULI AVIOLANo ratings yet
- When Not To Start Antibiotics - Avoiding Antibiotic Overuse in The Intensive Care Unit'Document6 pagesWhen Not To Start Antibiotics - Avoiding Antibiotic Overuse in The Intensive Care Unit'RENATA ULI AVIOLANo ratings yet
- Wjo 10 1Document14 pagesWjo 10 1RENATA ULI AVIOLANo ratings yet
- Yujm 2020 00031Document8 pagesYujm 2020 00031RENATA ULI AVIOLANo ratings yet
- Wjo 10 1Document14 pagesWjo 10 1RENATA ULI AVIOLANo ratings yet
- Yujm 2020 00031Document8 pagesYujm 2020 00031RENATA ULI AVIOLANo ratings yet
- EAU 2019 Full GuidelinesDocument1,475 pagesEAU 2019 Full Guidelinesrudirafian100% (4)
- When Not To Start Antibiotics - Avoiding Antibiotic Overuse in The Intensive Care Unit'Document6 pagesWhen Not To Start Antibiotics - Avoiding Antibiotic Overuse in The Intensive Care Unit'RENATA ULI AVIOLANo ratings yet
- F2 Chapter 4 Human HealthDocument6 pagesF2 Chapter 4 Human HealthJue Hazea GoldshopNo ratings yet
- GM Screen v3Document4 pagesGM Screen v3Mark HuntNo ratings yet
- Summer Internship (Imhrc)Document56 pagesSummer Internship (Imhrc)deepthirlsnNo ratings yet
- B. Choose The Word That Has Different Stress From Others.: Test 6 Part I: Phonetics: (2Pt)Document3 pagesB. Choose The Word That Has Different Stress From Others.: Test 6 Part I: Phonetics: (2Pt)Ngọc VươngNo ratings yet
- CryogenicsDocument5 pagesCryogenicsapi-502533045No ratings yet
- Internship Journal Week 4Document2 pagesInternship Journal Week 4api-609630655No ratings yet
- Excavation Risk AssessmentDocument3 pagesExcavation Risk Assessmentkhalef100% (1)
- OCTOBER 15, 2020: - Host Parent of A FLEX StudentDocument2 pagesOCTOBER 15, 2020: - Host Parent of A FLEX StudentIryna AbdellaNo ratings yet
- Study Protocol For A Randomized Controlled Trial To Test For Preventive Effects of Diabetic Foot Ulceration by Telemedicine That Includes Sensor-Equipped Insoles Combined With Photo DocumentationDocument12 pagesStudy Protocol For A Randomized Controlled Trial To Test For Preventive Effects of Diabetic Foot Ulceration by Telemedicine That Includes Sensor-Equipped Insoles Combined With Photo DocumentationAna GalvãoNo ratings yet
- Cardiocap 5 Manual UsuarioDocument228 pagesCardiocap 5 Manual UsuarioJonathan Scott100% (1)
- Bài tậpDocument2 pagesBài tậpminhphuongnmh14No ratings yet
- LESSON: The Discipline of Counseling ObjectivesDocument6 pagesLESSON: The Discipline of Counseling ObjectivesREYMARK PERALTANo ratings yet
- Hilti Firestop Submittal - Balamand UniversityDocument32 pagesHilti Firestop Submittal - Balamand UniversitybasbousrNo ratings yet
- IWR LAS Q2 WEEK 6 Shintoism Learning Activity Sheet WEEK 5Document11 pagesIWR LAS Q2 WEEK 6 Shintoism Learning Activity Sheet WEEK 5Suzcigrace Alma P. BelardoNo ratings yet
- Seaweed Biorefinery PDFDocument54 pagesSeaweed Biorefinery PDFJavier Andres Davila RinconNo ratings yet
- Theories of Juris - American JurisprudenceDocument5 pagesTheories of Juris - American JurisprudenceERICKSKIE23No ratings yet
- Laikou FBDDocument2 pagesLaikou FBDFarhanas Unique CollectionNo ratings yet
- Member Engagement Survey Results: Hemel East Catholic Parish, Hemel Hempstead, UK - Gallup ME25 2022Document8 pagesMember Engagement Survey Results: Hemel East Catholic Parish, Hemel Hempstead, UK - Gallup ME25 2022jacobNo ratings yet
- Petroleum Engineering Handbook For The Practicing Engineer Vol. 1 by M. A.Document5 pagesPetroleum Engineering Handbook For The Practicing Engineer Vol. 1 by M. A.ashishNo ratings yet
- Animal Testing Multimodal EssayDocument6 pagesAnimal Testing Multimodal Essayapi-535566007No ratings yet
- Detailed Lesson Plan I. Objectives ProcedureDocument5 pagesDetailed Lesson Plan I. Objectives ProcedureAngelaNo ratings yet
- Arunangshu Chakraborty, Balakrishnan Ashokka - A Practical Guide To Point of Care Ultrasound (POCUS) - Springer (2022)Document202 pagesArunangshu Chakraborty, Balakrishnan Ashokka - A Practical Guide To Point of Care Ultrasound (POCUS) - Springer (2022)Mohammad Louay100% (2)
- Post TermDocument17 pagesPost Termadane ararsoNo ratings yet
- (ENG) Huntleigh-BD4000 - BrochureDocument4 pages(ENG) Huntleigh-BD4000 - BrochureValentina Giraldo BetancourtNo ratings yet
- Method of Statement For Survey & Setting Out MakkahDocument17 pagesMethod of Statement For Survey & Setting Out MakkahToufeeq.HSE AbrarNo ratings yet
- Language Disorders: Causes, Symptoms and TreatmentDocument2 pagesLanguage Disorders: Causes, Symptoms and TreatmentLovielyn TubogNo ratings yet
- Predictors ATLS FailureDocument6 pagesPredictors ATLS FailureKing DonNo ratings yet
- Advanced Trauma Life Support: I. History/IntroductionDocument2 pagesAdvanced Trauma Life Support: I. History/IntroductionNAGARAJNo ratings yet
- End Stage Renal DiseaseDocument9 pagesEnd Stage Renal DiseaseShantanu DixitNo ratings yet
- Dehradun Distributor RetailersDocument238 pagesDehradun Distributor RetailersAmit DesaiNo ratings yet