Professional Documents
Culture Documents
Pelvic Inflammatory Disease - 3
Uploaded by
fatqur28Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pelvic Inflammatory Disease - 3
Uploaded by
fatqur28Copyright:
Available Formats
Pelvic Inflammatory Disease Workup: Approach Considerations, Labora... https://emedicine.medscape.
com/article/256448-workup#showall
This site is intended for healthcare professionals
Pelvic Inflammatory
Disease Workup
Updated: May 03, 2019
Author: Kristi A Tough DeSapri, MD; Chief Editor: Nicole W Karjane, MD more...
WORKUP
Approach Considerations
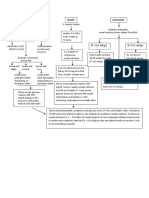
A number of procedures can be performed to improve the diagnosis of pelvic inflammatory disease
(PID) and its complications. These procedures are not necessary, nor are they indicated, in the
management of every case of PID. However, because of the difficulty of definitive clinical diagnosis
and the number of surgical and gynecologic emergencies that may have similar presentations, the
clinician should be aware of these modalities.
Procedures that may be appropriate for some patients, along with the corresponding findings
specific for PID, are as follows:
Laparoscopic confirmation
Transvaginal ultrasonographic scanning or magnetic resonance imaging (MRI) showing
thickened, fluid-filled tubes with or without free pelvic fluid or tubo-ovarian abscess (TOA)
Endometrial biopsy showing endometritis
Laparoscopy is the criterion standard for the diagnosis of PID, but the diagnosis of PID in
emergency departments and clinics is often based on clinical criteria, with or without additional
laboratory and imaging evidence. [60] No single test is highly specific and sensitive for PID, but
laboratory tests, imaging studies, and procedures may be used to increase the specificity of the
diagnosis.
Additional criteria that improve diagnostic specificity include the following:
Oral temperature higher than 38.3° C (101° F)
Abnormal cervical or vaginal mucopurulent discharge
Abundant white blood cells (WBCs) on saline microscopy of vaginal secretions
Elevated erythrocyte sedimentation rate (ESR) (≥40 mm/h)
Elevated C-reactive protein (CRP) level (≥ 60 mg/L)
Laboratory evidence of cervical infection with N gonorrhoeae or C trachomatis (via culture or
DNA probe)
In addition, obtaining a sample from the urethra in women with suspected PID can increase the
1 dari 8 19/05/2021 23.28
Pelvic Inflammatory Disease Workup: Approach Considerations, Labora... https://emedicine.medscape.com/article/256448-workup#showall
diagnostic yield for gonorrhea and chlamydial infection. This step is recommended only if the more
sensitive nucleic acid amplification test (NAAT) is unavailable. [11]
Laboratory Studies
Perform a pregnancy test. If the results are positive, the possibility of ectopic pregnancy must be
addressed. Pregnancy also directly influences selection of an antibiotic regimen and consideration
of the patient for admission.
On a complete blood count (CBC), fewer than 50% of women with acute PID have a WBC count
higher than 10,000/µL. Because of its poor sensitivity and specificity, an elevated WBC count is not
among the diagnostic criteria for PID formulated by the Centers for Disease Control and Prevention
(CDC). Blood cultures are not helpful in the diagnosis of PID.
In fact, no single test is highly specific and sensitive for PID; however, a number of tests may be
used to increase the specificity of the clinical diagnosis. Vaginal secretions that have been treated
with saline and potassium hydroxide can be examined for leukorrhea (>10 WBC/high-power field;
>1 WBC/epithelial cell), trichomoniasis, and clue cells. [16, 61] The presence of leukorrhea was
found to be the most sensitive, laboratory indicator of upper tract infection, though not a specific
one; the absence of leukorrhea is a negative predictor of PID.
Gonorrhea DNA probes and cultures are generally used to support the diagnosis and to provide
epidemiologic data for public health departments. However, they are frequently negative in later
stages of PID. [62]
Chlamydial vulvovaginal or endocervical DNA probes and cultures are generally used to support
the diagnosis and to provide epidemiologic data for public health departments, though recovery
rates from the cervix vary widely (5-56%). [63] Quantitative culture for Chlamydia identifies rapidly
replicating bacteria that appear to be associated with active disease. However, DNA probe and
culture results are often not available to the emergency physician at the time of initial evaluation.
One study suggested that women with high titers of immunoglobulin G (IgG) chlamydial antibodies,
acute pelvic pain, and a clinical picture suggestive of PID were more likely to have salpingitis than
adhesions alone. [64] Those patients with high titers and chronic pelvic pain but with a clinical
picture that did not suggest PID were more likely to have adhesions alone. In the investigators’
view, their limited data suggested that serologic testing might help establish the diagnosis.
Although the 2015 CDC guidelines mention Mycoplasma genitalium contributing to milder forms of
PID, there is no clear consensus on the value of testing for this organism. [95]
Other tests that may be considered include the following:
Rapid protein reagin (RPR) test for syphilis (the incidence of which is again increasing in the
United States)
Hepatitis virus and HIV
Urinalysis to help exclude urinary tract infections – Note, however, that a positive urinalysis
does not exclude PID, because any inflammatory process in the contiguous pelvis can
2 dari 8 19/05/2021 23.28
Pelvic Inflammatory Disease Workup: Approach Considerations, Labora... https://emedicine.medscape.com/article/256448-workup#showall
produce WBCs in the urine
Transvaginal Ultrasonography
Ultrasonographic scanning may be performed for cases of suspected PID in which clinical findings
are nondiagnostic. Transvaginal ultrasonography is superior to transabdominal ultrasonography for
diagnosing PID, as well as endometrial abnormalities and pelvic masses (see the images below).
[61] This modality is readily available and noninvasive and can be performed at the patient’s
bedside.
Transabdominal ultrasonogram shows anechoic tubular structures in adnexa; finding is compatible with hydrosalpinx.
Endovaginal ultrasonogram reveals tubular structure with debris in left adnexa; finding is compatible with pyosalpinx.
3 dari 8 19/05/2021 23.28
Pelvic Inflammatory Disease Workup: Approach Considerations, Labora... https://emedicine.medscape.com/article/256448-workup#showall
Ultrasonogram shows markedly heterogeneous and thickened endometrium; finding is compatible with endometritis.
Ultrasonogram reveals bilateral complex masses in patient who had pyometrium; finding is compatible with tubo-ovarian
abscess.
Transabdominal ultrasonogram demonstrates echogenic region within endometrium with dirty shadowing; finding is
compatible with air in endometrium and endometritis. Additionally, bilateral complex masses are present; finding is
compatible with tubo-ovarian masses.
There are no large randomized trials addressing the specificity and sensitivity of bedside
ultrasonography for the diagnosis of PID. The literature demonstrates that the accuracy of this
technique depends on the criteria used to indicate PID, the quality of the equipment, and the
4 dari 8 19/05/2021 23.28
Pelvic Inflammatory Disease Workup: Approach Considerations, Labora... https://emedicine.medscape.com/article/256448-workup#showall
experience of the individual operator performing the test.
Transvaginal ultrasonography has poor sensitivity (81%) and specificity (78%) in mild or atypical
PID. [61] Helpful findings include thickened (>5 mm), fluid-filled fallopian tubes; thickened cilia;
indistinct endometrial borders; ovaries with multiple small cysts; and moderate-to-large amounts of
free pelvic fluid in acute, severe PID. [65] Small amounts of free pelvic fluid have not been shown to
be a discriminatory finding. These findings alone are not sufficiently specific to permit a definitive
diagnosis of PID.
In the patient who appears toxic or has asymmetric pelvic findings, ultrasonographic scanning is an
important diagnostic tool for the identification of a TOA. Pelvic abscesses may be seen as complex
adnexal masses with multiple internal echoes. The modality has been shown to demonstrate as
many as 70% of adnexal masses missed on physical examination.
Pelvic ultrasonographic scanning is also useful in evaluating the possibility of ectopic pregnancy in
patients whose differential diagnosis includes both that condition and PID. The modality can also
be helpful in evaluating other disorders in the differential diagnosis, including hemorrhagic ovarian
cyst, ovarian torsion, endometrioma, and appendicitis. (At some adult academic medical centers,
however, ultrasonography is considered adequate as a solo imaging modality to rule out
appendicitis.)
Ultrasonographic results in patients with PID may be normal or nonspecific because salpingitis
alone is not usually associated with imaging findings. [66] Positive ultrasonographic findings in PID
may include the following:
The uterus may be ill defined because of inflammation; however, inflammation of the uterus is
an unusual finding
Endometritis may result in central-endometrial-cavity echo thickening and heterogeneity
Hydrosalpinx is depicted as a fluid-filled fallopian tube – If the fallopian tube walls are
thickened and if debris is present within the tube, pyosalpinx should be considered in the
differential diagnosis, but a pyosalpinx may be imaged as an echoless tube, whereas an
imaged echo-filled tube may be from proteinaceous but noninfected fluid in a hydrosalpinx
Oophoritis results in enlarged ovaries with ill-defined margins that often appear adherent to
the uterus; adjacent free fluid may be present in the adnexa or cul-de-sac
TOAs are depicted as complex adnexal masses with thickened walls and central fluid
Pelvic infection, with findings of tubal inflammation and hydrosalpinx detected by Doppler
studies, is one of the most specific criteria in diagnosing PID [6]
Thickening of the endometrium is nonspecific for PID because this finding may also be seen with
endometrial hyperplasia, polyps, or cancer. Knowledge of the patient’s clinical findings and other
signs of infection can help in the differential diagnosis.
Hydrosalpinx and pyosalpinx can usually be readily distinguished from pelvic veins and bowel by
visualizing the color flow within the patent blood vessels and peristalsis within the bowel.
Imaging findings in TOAs are usually nonspecific and must be distinguished from the following:
5 dari 8 19/05/2021 23.28
Pelvic Inflammatory Disease Workup: Approach Considerations, Labora... https://emedicine.medscape.com/article/256448-workup#showall
Endometriomas
Ectopic pregnancies
Hemorrhagic cysts
Ovarian tumors
Abscesses from adjacent organs
Laparoscopy
Laparoscopy is the criterion standard for the diagnosis of PID. It is significantly more specific and
sensitive than are clinical criteria alone. The minimum criteria for diagnosing PID laparoscopically
include tubal wall edema, visible hyperemia of the tubal surface, and the presence of exudate on
the tubal surfaces and fimbriae.
Pelvic masses consistent with TOA or ectopic pregnancy can be directly visualized. Hepatic
abscess exudate or adhesions may be visible. Material can be obtained for definitive culture and
histologic studies.
The main drawbacks of laparoscopy are that the procedure is expensive and invasive, exhibits
interobserver variability, and requires an operating room and anesthesia. [57] In addition, findings on
laparoscopy do not necessarily correlate with the severity of illness, in that only the surfaces of
structures are visible through the scope. In as many as 20% of cases, laparoscopy may not define
PID fully.
Computed Tomography
Computed tomography (CT) may also be used as the initial diagnostic study for the investigation of
nonspecific pelvic pain in a female, and PID may be found incidentally. Because of concerns about
radiation exposure, ultrasonography is preferred to CT as the triaging tool in a female child or
adolescent with right lower quadrant or pelvic pain.
In cases of PID in which no evidence of an abscess is found, CT scan findings are nonspecific.
Inflammation obliterates the pelvic fat planes, with thickening of the fascial planes. Endometritis
manifests as enlargement of the uterine cavity. If hydrosalpinx is present, a fluid-filled tubular
structure may be seen in the adnexa.
Typically, a TOA is visualized as a mass; the mass may have regular margins and contain debris
similar to that seen in endometriomas or hemorrhagic cysts. The margins may be thick and
irregular. There may also be an associated low-attenuation area that may represent an adjacent or
contained fluid-filled fallopian tube. [67] Many adult centers prefer CT to ultrasonography when a
diagnosis of appendicitis is in question.
Tubular, fluid-filled, nonvascular structures in the pelvis that are associated with an adnexal mass
are suggestive of dilated fallopian tubes that correlate with cases of PID. A finding of an adjacent or
6 dari 8 19/05/2021 23.28
Pelvic Inflammatory Disease Workup: Approach Considerations, Labora... https://emedicine.medscape.com/article/256448-workup#showall
surrounding complex mass confirms the diagnosis of TOA.
Magnetic Resonance Imaging
Although MRI has relatively high specificity (95%) and sensitivity (95%) in this setting, [61] it is costly
and is rarely indicated in cases of acute PID.
Hydrosalpinx is visualized on MRI as a tubular structure with low signal intensity on T1-weighted
scans and high signal intensity on T2-weighted images. If the walls are thickened, pyosalpinx
should be considered in the differential diagnosis. [68] Oophoritis may be evidenced by enlarged,
polycystic-appearing ovaries with ill-defined margins and adjacent fluid.
TOAs often appear as thick-walled masses with low signal intensity on T1-weighted images and
high signal intensity on T2-weighted images. Occasionally, TOAs may be isointense or
hyperintense on T1-weighted images and may have heterogeneous signal intensity on T2-weighted
images.
Culdocentesis
Culdocentesis can be performed rapidly in the emergency department. With the advent of
transvaginal ultrasonographic scanning, culdocentesis is rarely performed today, but it remains
valuable in settings where current technology is unavailable.
For the procedure, an 18-gauge spinal needle attached to a 20-mL syringe is inserted
transvaginally into the cul-de-sac. Normally, this yields only 2-4 mL of clear to straw-colored free
pelvic fluid; purulent fluid indicates an infectious or inflammatory process.
The potential positive findings of leukocytes and bacteria are nonspecific: They may indicate PID,
or they may be a product of another infectious or inflammatory process in the pelvis (eg,
appendicitis or diverticulitis), or they may result from contamination with vaginal contents. A yield of
more than 2 mL of nonclotting blood is consistent with ectopic pregnancy.
Endometrial Biopsy
Endometrial biopsy can be used to determine the histopathologic diagnosis of endometritis, a
condition that is uniformly associated with salpingitis. Endometrial biopsy is approximately 90%
specific and 90% sensitive. The procedure is performed with an endometrial suction pipette or
curette and is well tolerated. Specimens for culture may also be obtained during the procedure, but
these are frequently contaminated with vaginal flora.
Current CDC guidelines recommend endometrial biopsy in women undergoing laparoscopy who
have no visible signs of salpingitis, on the grounds that endometritis may be the only sign of PID. [6]
Diagnostic use of endometrial biopsy in the emergency department is limited; significant operator
training is required, and the results of the procedure are not immediately available to the clinician.
7 dari 8 19/05/2021 23.28
Pelvic Inflammatory Disease Workup: Approach Considerations, Labora... https://emedicine.medscape.com/article/256448-workup#showall
Endometrial biopsy findings usually confirm the presence of infection but rarely identify the
causative organism. Chronic endometritis is more commonly seen than acute endometritis.
Treatment & Management
TOP PICKS FOR YOU
8 dari 8 19/05/2021 23.28
You might also like
- Pelvic Inflammatory Disease - 4Document7 pagesPelvic Inflammatory Disease - 4fatqur28No ratings yet
- Pelvic Inflammatory Disease - 2Document2 pagesPelvic Inflammatory Disease - 2fatqur28No ratings yet
- Pelvic Inflammatory Disease - 1Document8 pagesPelvic Inflammatory Disease - 1fatqur28No ratings yet
- Pelvic Inflammatory Disease - 5Document5 pagesPelvic Inflammatory Disease - 5fatqur28No ratings yet
- Fixed Drug EruptionDocument4 pagesFixed Drug EruptionpriscilliafeybeNo ratings yet
- ThoracosintesisDocument37 pagesThoracosintesisfatqur28No ratings yet
- Jurnal Plasenta Akreta PDFDocument5 pagesJurnal Plasenta Akreta PDFfatqur28No ratings yet
- Management of AscitesDocument60 pagesManagement of AscitesAnonymous 5ePPbFyNo ratings yet
- Committee Opinion: Placenta AccretaDocument5 pagesCommittee Opinion: Placenta AccretaagungNo ratings yet
- Iv Fluids Insulin Potassium: 5,3 Meq/LDocument1 pageIv Fluids Insulin Potassium: 5,3 Meq/Lfatqur28No ratings yet
- Herpes Zoster: Nurul Iska Ulmarika Idrisc111 10 831 Ruth Faustine J. Rayo C 1 1 1 1 0 1 8 0Document26 pagesHerpes Zoster: Nurul Iska Ulmarika Idrisc111 10 831 Ruth Faustine J. Rayo C 1 1 1 1 0 1 8 0fatqur280% (1)
- ThoracosintesisDocument37 pagesThoracosintesisfatqur28No ratings yet
- Reti No Blast OmaDocument5 pagesReti No Blast Omafatqur28No ratings yet
- PregabalinDocument12 pagesPregabalinAngelica VergaraNo ratings yet
- Case Report Herpes Zoster Regio Th11 - L5Document37 pagesCase Report Herpes Zoster Regio Th11 - L5fatqur28No ratings yet
- Case Report Bangsal TeachingDocument11 pagesCase Report Bangsal Teachingfatqur28No ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Siemens Acuson Sc2000 Interventional FlyerDocument6 pagesSiemens Acuson Sc2000 Interventional Flyerbashir019No ratings yet
- Panvascular Disease - Diagnosis and Management: SciencedirectDocument9 pagesPanvascular Disease - Diagnosis and Management: SciencedirectAndikaputra Brahma WidiantoroNo ratings yet
- Aloka Prosound 2 Brochure and SpecificationsDocument12 pagesAloka Prosound 2 Brochure and SpecificationsKhwaja Maqsood100% (1)
- Acute Osteomyelitis in Children Journal Radiology PDFDocument15 pagesAcute Osteomyelitis in Children Journal Radiology PDFRegi ShabaraNo ratings yet
- Specifications For An Ultrasound MachineDocument2 pagesSpecifications For An Ultrasound MachineTony starkNo ratings yet
- DIPSI GuidelinesDocument7 pagesDIPSI GuidelinesvinaypharmNo ratings yet
- Ultrasonographic Differences Between Dogs and CatsDocument13 pagesUltrasonographic Differences Between Dogs and Catsludiegues752No ratings yet
- Flow MeasurementsDocument18 pagesFlow MeasurementsAbhishek SatheeshNo ratings yet
- Ultrasound in Acute Viral Hepatitis: Does It Have Any Role?: Original ArticleDocument5 pagesUltrasound in Acute Viral Hepatitis: Does It Have Any Role?: Original ArticleqalbiNo ratings yet
- 27 251s PDFDocument6 pages27 251s PDFDurgamadhaba MishraNo ratings yet
- Maternal Perception of Fetal Movements and Real-Time Ultrasound FindingsDocument6 pagesMaternal Perception of Fetal Movements and Real-Time Ultrasound FindingsDarian AngNo ratings yet
- The Significance of Septations in A Renal CystDocument3 pagesThe Significance of Septations in A Renal CystJenina Clarisse B. PascuaNo ratings yet
- Ultrasonic Testing Level 1Document9 pagesUltrasonic Testing Level 1Ashraf TrescaNo ratings yet
- Global Innovation by Design Toshiba - A History of LeadershipDocument6 pagesGlobal Innovation by Design Toshiba - A History of LeadershipkritonNo ratings yet
- Emergency Sonography For Trauma FAST Protocol 2010 PDFDocument101 pagesEmergency Sonography For Trauma FAST Protocol 2010 PDFChavo Delocho100% (9)
- 2jkv6ONYEwVsovvq PDFDocument304 pages2jkv6ONYEwVsovvq PDFSyarif AlfathNo ratings yet
- 9157 US ACUSON Juniper 1 5 Datasheet K8 HOOD05162003101293Document28 pages9157 US ACUSON Juniper 1 5 Datasheet K8 HOOD05162003101293Andres Mauricio Arturo Vargas100% (1)
- Medical Imaging Equipment Theory - Richard AstonDocument145 pagesMedical Imaging Equipment Theory - Richard Astongennaro0% (1)
- Small Group Discussion #4: A Case of A 22-Yr Old Nullipara Who Consulted For Left Lower Quadrant PainDocument36 pagesSmall Group Discussion #4: A Case of A 22-Yr Old Nullipara Who Consulted For Left Lower Quadrant PainRose Ann RaquizaNo ratings yet
- Mirror 5 Exp User's Manual (English)Document208 pagesMirror 5 Exp User's Manual (English)Eng.Mohamed HamedNo ratings yet
- A Practical Approach To Clinical Echocardiography (2014) (PDF) PDFDocument423 pagesA Practical Approach To Clinical Echocardiography (2014) (PDF) PDFDiana Loloiu67% (3)
- Sonoace X8 Technical SpecificationDocument22 pagesSonoace X8 Technical SpecificationjhonsrNo ratings yet
- Ultrasound - A GuideDocument9 pagesUltrasound - A GuideDebasish KunduNo ratings yet
- NDT20 Course NotesDocument278 pagesNDT20 Course Noteshazzleraflet100% (11)
- Acoustic Lens Improves Superficial In-Plane Ultrasound-Guided ProceduresDocument6 pagesAcoustic Lens Improves Superficial In-Plane Ultrasound-Guided ProceduresHarm ScholtenNo ratings yet
- Yan 2007Document3 pagesYan 2007Agustin LindaNo ratings yet
- Philips: URGENT - Medical Device CorrectionDocument2 pagesPhilips: URGENT - Medical Device CorrectionNirav BarotNo ratings yet
- Clarius Ultrasound Scanner User ManualDocument114 pagesClarius Ultrasound Scanner User Manualfgjruiz37No ratings yet
- Ultrasound 1Document65 pagesUltrasound 1Joana Bless PereyNo ratings yet
- MyLab - X75 - Customer PresentationDocument22 pagesMyLab - X75 - Customer PresentationIshaan JindalNo ratings yet