Professional Documents
Culture Documents
Trans - Med 9a (Gram-Negative Bacteria I)
Uploaded by
Christille Lindy Joyce CaluyoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Trans - Med 9a (Gram-Negative Bacteria I)
Uploaded by
Christille Lindy Joyce CaluyoCopyright:
Available Formats
09/04/2019
9:30-12:00 W Introduction to Infectious Disease
7:30-10:00 F Medicine II
LDT Juan Ismael Sumagaysay, M.D.
OUTLINE o Increase antibiotic use increases risk of
infection by killing the normal flora
I. AnatB1 Introduction to Infectious Disease Treatment with immunosuppressive drug:
II. Enteric Gram-negative Rods important especially in fungal and immunocompromised patients
(Enterobacteriaceae)
III. Diseases Caused by Escherichia coli Host-Factor Interactions
INTRODUCTION TO INFECTIOUS DISEASE Geography: Dengue and Malaria are common in tropics
Environment
Not a system or part of the body Behavior
Broad, composes different disciplines
Anything caused by a microbe Specific factors that influence likelihood of infections:
1. Age: extreme of ages
Multi system involvement: outmost (skin) to innermost (bone)
2. Immunization history: common in children
Top most diseases
3. Prior illness
o Tuberculosis
4. Level of nutrition
o Diarrhea o Malnourished (prone to disease)
Second leading cause of death worldwide o More nourished (more prone to dengue)
5. Pregnancy: prone to disease
Host-Pathogen Interactions 6. Coexisting illnesses: diabetes, COPD, hepatitis, renal problem
7. Emotional state
Infectious disease: major cause of death and debility around the world o Emotionally stressed
Common in 3rd world due to: o Lack of sleep
o Poverty o Always starving
o Overcrowding
o Cultural differences
Tripod The Immune Response
o Etiologic agent
o Host Innate immunity
o Immune system o Defensins
Antibiotic resistance occurs at an alarming rate: microbes develop the o Simple peptide on the skin
ability to elude the best antimicrobials and develop new survival o Macrophages
strategies Adaptive immunity
There is resurgence of disease long thought to be eradicated o Cellular immunity
o Factor: migration from area of high incidence of disease to area of T lymphocytes
low incidence Macrophage
o Disease resurgence in recent times Natural killer cells
Tuberculosis: increased incidence in developing countries
Cholera
RA Approach to the Patient
West Nile Virus Encephalitis
Careful history taking
o Recently emerging newer disease pathogens o Paramount in the evaluation of a patient with a possible infectious
Ebola virus disease
Human metapneumovirus o Guides PE and initial diagnostic testing
Anaplasma phagocytophila infection o Focus on 2 areas
Retroviruses / HIV An exposure history that may identify microorganisms with
Helicobacter pylori infection which the patient may have come into contact
Zika virus infection Host-specific factors that may predispose to the development of
an infection
Infectious diseases don’t often occur in isolation (e.g. contaminated
H2O respiratory droplets) o History of infections or exposure to drug-resistant microbes
May alter the choice of antibiotics
Medical Care Factors
o Social history
Hospitalization Unsafe sexual behaviors (IV drug use)
o Prone to develop hospital acquired infection Hobby-associated exposures (avid gardening)
o Increase hospitalization, increase risk Occupational exposures (increased risk for MTB exposure in
Breach in the skin / mucosal membrane funeral service workers)
Introduction of foreign bodies: implant, valve o Dietary habits
Alteration of natural flora (antibiotic use) Shiga toxin-producing strains of E. coli and T. gondii:
o Chemotherapy consumption of raw or undercooked meat or raw seafood
CPU College of Medicine | Magnus Animus Medicus | 2021
S. typhimurium, L. monocytogenes, and M. bovis: unpasteurized o Specimens are collected before the administration of antimicrobial
milk therapy (blood, urine, sputum, pus from a wound)
Leptospira spp., parasites, and enteric bacteria: unpurified water o Allows identification of the etiologic agent, determination of the
Vibrio spp., norovirus, helminthes and protozoa: raw seafood antimicrobial susceptibility profile and isolate typing
Pathogen-specific testing
o Animal exposures: often vectors of infectious diseases o Serology, Antigen testing, PCR testing
o Travel history o Facilitate rapid turnaround that ultimately enhances patient care
Both international and domestic travel o PCRs identify organisms that currently are not cultivable and have
Fever in a patient who has recently returned from abroad
unclear relationships to disease
significantly broadens the differential diagnosis
Radiology
Careful review of systems o Allows evaluation for lymphadenopathy in regions that are not
Thorough Physical Examination externally accessible, assessment of internal organs for evidence of
o Vital signs: temperature, HR, PR, RR infection, and facilitation of image-guided percutaneous sampling of
o Lymphatics deep spaces
Infections are an important cause of lymphadenopathy o CT scan, MRI, Ultrasound, Nuclear medicine
Evaluation of lymph nodes in multiple regions
Location
Treatment
Size
Consistency
“Primum non nocere”: do no harm
Presence or absence of tenderness
Whether the nodes are matted (connected and moving Obtain relevant samples for culture prior to the administration of
together) antibiotics
Determining whether the patient has generalized versus localized Although a general maxim for antibiotic treatment is to use a regimen
lymphadenopathy with as narrow a spectrum as possible, empirical regimens are
necessarily somewhat broad, given that a specific diagnosis has not yet
o Skin: specific rashes are extremely helpful in narrowing the been made
diagnosis of an infection
o Foreign bodies Laboratory Diagnosis of Infectious Diseases
Maintenance of epithelial barriers is one of the most important
mechanisms in protection against infection Requires demonstration, either direct or indirect, of viral, bacterial,
Hospitalization of patient is often associated with branches of mycotic, or parasitic agents in tissues, fluids or excreta of the host
barriers: IV lines, surgical drains or tubes o Direct: microscopy, pathology (biopsy)
Allow microorganisms to localize in sites to which they o Indirect: PCR, serologic test
normally would not have access Detection of pathogenic agents by culture
o Specimen collection and transport
o Isolation of bacterial pathogens
Laboratory Investigations o Isolation of viral agents: cultured cell for cytopathic effect,
immunofluorescent detection of viral antigen
Must be directed towards establishing an etiologic diagnosis
Detection methods
Shortest possible time, lowest possible cost, least possible cost and least o Biologic signals: a material that can be reproducibly differentiated
possible discomfort to the patient
from other substances present in the same physical environment
Specimens must be appropriate and handled carefully Structural components of bacteria, fungi
o Must be based directly on the patient’s history and physical exam
findings Detection system: trained eye of the technologist
o Limited to those conditions that are reasonably likely and treatable, o Sensitive electronic instruments: immunofluorescence,
important in terms of public health considerations, and/or capable of chemiluminescence
providing a definitive diagnosis that will consequently limit other Amplification: culture of bacterium on an agar plate, PCR, enzyme
testing immunoassays
WBC count Direct detection
o Elevations in the WBC count are often associated with infection, o Microscopy
though many viral infections are associated with leukopenia o Staining: Gram’s stain, Acid fast stain, Fluorochrome stains,
o Important to access the WBC differential count Immunofluorescent stains
Bacteria: increase in polymorphonuclear neutrophils o Macroscopic antigen detection: Latex agglutination assays, Enzyme
Viruses: increase in lymphocytes Immunoassays
Certain parasites: increase in eosinophils Identification methods
Inflammatory markers o Classic Phenotyping
o Erythrocyte Sedimentation Rate o Gas-liquid chromatography
o C-reactive Protein o Nucleic acid probes
Analysis of CSF Susceptibility testing
o Critical for patient with suspected meningitis or encephalitis o Paper disk method
o Opening pressure should always be recorded, and fluid should o Broth tube method
routinely be sent for cell counts, Gram’s stain and culture and o Minimum Inhibitory Concentration (MIC)
determination of glucose and protein levels Principles of Immunization and Vaccination
Cultures
o Mainstay of infectious disease diagnosis
Universal immunization has invariably remained an unattained goal
Vaccination (Polio: only disease that it totally eradicated)
CPU College of Medicine | Magnus Animus Medicus | 2021 Page 2 of 6
Immunization Immunocompromised persons (HIV+, hematologic/generalized
o Process of inducing or providing immunity malignancy)
Passive: given as immunoglobulins o Should be immunized in the same manner as individuals with
Human tetanus Immunoglobulin normal immune system
Transplacental transfer of antibodies o Live attenuated vaccine is contraindicated, may lead to disseminated
Active: as toxoids promoting production of antibodies directly infection with the vaccine virus
(will take some time for the body to produce its own antibody)
ENTERIC GRAM-NEGATIVE RODS (ENTEROBACTERIACEAE)
Factors that can give rise to increase in vaccine-preventable disease
o Low rates of immunization that result in an accumulation of Large and heterogenous
susceptible people Facultative anaerobes and aerobes
o Changes in the infectious agent that permit it to escape vaccine- Often called Coliforms
induced protection Many produce toxins and virulence factors
o Waning of vaccine-induces immunity
Found in the intestinal tract of humans and animals
o Point-source introductions of large inoculate o Escherichia
o Shigella
Approaches to Immunization and Vaccination
o Salmonella
o Enterobacter
Vaccine: attenuated or live microorganisms/antigenic portion
o Klebsiella
Toxoid: modified bacterial toxin
o Serratia
Immune globulin: antibody containing protein
o Proteus
Antitoxin: antibody derived from serum of animals
o Citrobacter
Active immunization
o Morganella
o Live, attenuated: generally long-lasting immunity
o Providencia
o Inactivated: multiple doses or periodic boosters
o Cronobacter
Passive Immunization
o Edwardsiella
o Generally used to provide temporary immunity
o Treatment of certain diseases associated with toxins Among the most commonly cultured in laboratory and disease bacteria
Classifications
Route of administration
o Classified as to shape, growth, colony form, biochemical properties
o Determine the rapidity and nature of the vaccine
o Gram-negative rods
o Must determine the licensed route to ensure immunogenicity
o Motile or nonmotile
Orally
Intranasally o Grow on peptone and MacConkey’s agar
Intramuscular o Ferments glucose
o Catalase (+), Oxidase (-)
o Temperature and transport are factors that can affect the o Reduce nitrate to nitrite
effectiveness of vaccines o Typically short, gram-negative rods
Primary Response o Some have capsules: Klebsiella
o Measurable circulating antibody do not appear for 7-10 days o Most have convex, smooth, circular colonies
o Characterized by early appearing IgM antibodies
Secondary Response Escherichia coli
o Elicited by second exposure to the same antigen
o Usually occur within 4-5 days Indole +
o Characterized by marked proliferation of IgG antibodies Lysine decarboxylases
o Hypersensitivity reaction Produce gas from glucose
o Herd immunity Ferments mannitol
Constituents of Vaccines Hemolyzes blood agar
o Preservatives, stabilizers, antibiotics Iridescent sheen on culture media (Greenish-metallic Sheen)
o Adjuvants: enhance immune response
o Suspending fluids Klebsiella – Enterobacter - Serratia
Target Population and Timing of Immunization Mucoid growth
Large polysaccharide capsule
Demographic features of the populations at risk Lacks motility
Duration and character of the immunologic response
Influenza pandemic preparedness Proteus – Morganella – Providentia
Breast feeding: neither killed nor live vaccine affect the safety of breast
feeding for either mother or infant Deaminate phenylalanine
Pregnancy Motile: swarming on solid media
o Routine immunization should be avoided Grow on potassium cyanide medium
o Tetanus and diphtheria toxoid can be safely given Ferments xylose
o MMR, varicella should be withheld (has teratogenic effects Citrobacter
especially in the first trimester)
Hepatitis B vaccine: workers Citrate +
Rubella, Measles, varicella – Health caregivers Do not decarboxylase lysine
CPU College of Medicine | Magnus Animus Medicus | 2021 Page 3 of 6
Shigella 6 Distinct Types of Intestinal E. coli
1. Enterohemorrhagic E. coli (EHEC) / Shiga-toxin producing E. coli
Non-motile (STEC)
Do not ferment lactose 2. Enterotoxigenic E. coli (ETEC)
Produce acid but not gas 3. Enteropathogenic E. coli (EPEC)
Do not produce H2S 4. Enteroinvasive E. coli (EIEC)
5. Enteroaggregative E. coli (EAEC)
Salmonella 6. Diffusely adherent E. coli (DAEC)
Motile Enteropathogenic E. coli (EPEC)
Ferment glucose and mannose Primarily affecting young children
Most produce H2S: associated with typhoid fever Infants, Nurseries: Infantile diarrhea
Breastfeeding decreases its incidence
Antigenic Structure of Enterics Stools often contain mucus rather than blood
Rapid person-to-person spread
O Antigen (Somatic Antigen) Colonization of the bowel
o Most external part of the cell wall o Initial localized adherence to enterocytes via Type IV bundle-
o Resistant to host and alcohol forming pili
K Antigen (Capsular Antigen) Effacement of microvilli
o External to O antigen on some Cup-like actin-rich pedestals
o Associated with virulence
o Can be identified by capsular swelling in some Incubation period: 1 or 2 days (often self-limited, lasting 5-15 days)
H Antigen (Flagellar Antigen) Host cell modulation by Type III secretion system
o Located in flagella Diarrhea: accompanied by vomiting and fever
o Denatured by heat or alcohol Atypical EPEC
o Strains lacking bundle-forming pili
o Pathogens in all age groups
Colicins
o Can affects immunocompromised patients
Bacteriocins o Diarrheal stool contains mucus
Produce by certain enterics
Enterotoxigenic E. coli (ETEC)
Virus-like bactericidal substances which act against certain strain of
closely related species Traveler’s diarrhea and very important cause of diarrhea in infants
Used in typing of organisms Major cause of endemic diarrhea
o Children after weaning commonly experiences several episodes of
DISEASES CAUSED BY ESCHERICHIA COLI infection during first 3 years of life
Adherence of ETEC via colonization factors that causes net fluid
Escherichia coli: UTI
secretion in jejunum and ileum
o Heat-labile toxin (LT-1) activates adenylate cyclase
Escherichia coli Structurally and functionally similar to Cholera toxin
o Most common cause of UTI A and B subunit
o Accounts for approximately 90% of 1st UTI in young women Binding of B subunit to GM1 ganglioside leads to intracellular
translocation of A subunit
Signs and Symptoms
A Subunit: functions as ADP-ribosyltransferase
o Uncomplicated Cystitis: most common acute UTI syndrome
o Dysuria o Heat-stable toxin (STa) activates guanylate cyclase: increased
Initial intracellular secretions of CGMP
Terminal Usually self-limited: a large inoculum (106-1010 CFU) is needed to
Caused by cystitis, inflamed urinary bladder produce disease
Urethritis Incubation period: 12-72 hours
o Hematuria Although symptoms are usually self-limited (3-5 days), infection may
result in significant morbidity and mortality
o Pyuria
o Watery diarrhea accompanied by cramps
o Flank pain
o Mucus, blood and inflammatory cells in stool
Together with fever
o Fever
Suggests progression to pyelonephritis
o Disease spectrum ranges from a mild illness to a life-threatening
o Fever cholera-like syndrome
May take 5-7 days to resolve completely
Persistent or increasing fever and neutrophil counts should Enterohemorrhagic (EHEC) / Shiga toxin-producing E. coli (STEC)
prompt evaluation for intrarenal or perinephric abscess and/or
obstruction More common in developed countries where the consumption of
Prostatic infection is a potential complication of UTI in men processed food is more common
Symptom may suggest progression to pyelonephritis Several large outbreaks resulting from the consumption of fresh
produce (lettuce, spinach, sprouts) and of undercooked ground beef
E. coli Associated Diarrheal Disease O157:H7 strains are the fourth most commonly reported cause of
bacterial diarrhea in the US
CPU College of Medicine | Magnus Animus Medicus | 2021 Page 4 of 6
Less than 102 CFU can cause disease Diarrhea of more than 10 days: Giardia or Cryptosporidium
Incubation period: 3-4 days O157 STEC/EHEC: identified via culture
o Self-limited (5-10 days) o Screening for E. coli strains not fermenting sorbitol
Mode of transmission:
o Environmental contamination
o Person to person transmission Treatment
Produces verotoxin (Shiga toxin), associated with hemorrhagic colitis
with hemolytic uremic syndrome Appropriate fluid and electrolyte replacement: mainstay treatment
o Stx gene: present on chromosomally integrated prophages for all diarrheal syndromes
o Uncommon but feared complication is HUS, which occurs 2-14 Self-limited use of prophylactic antibiotic should be discouraged
Stool free of mucus and blood
days after diarrhea in 2-8% of cases
o Early patient initiation of treatment of traveler’s diarrhea with
o This complication is mediated by the systemic translocation of
fluoroquinolone or azithromycin to decrease duration of illness
Shiga toxins
Colonic edema and an initial non-bloody secretory diarrhea may
SOURCES
develop into the STEC/EHEC hallmark syndrome of grossly bloody
diarrhea
o Grossly bloody diarrhea: 90% of cases Upclass trans
o Absence of fever Doc’s ppt
o Significant abdominal pain: 70% of cases Recordings
o Fecal leukocytes: 70% of cases Harrison’s
HUS: 2 to 14 days after diarrhea
APPENDIX
o Most often in very young or elderly patients (STEC/EHEC)
o Non-elderly adults especially young women (ST-EAEC)
o Mediated by systemic translocation of Shiga toxin
Enteroaggregative (EAEC) and Diffusely Adherent E. coli (DAEC)
Acute and chronic diarrhea in children (>14 days)
Can cause traveler’s diarrhea
Associated with prolonged watery diarrhea
DAEC: diarrheal disease in children 2-6 years old
Large inoculum is required for infection
In vitro, the organisms exhibit a diffuse or “stacked-brick” pattern
of adherence to small intestine epithelial cells
Pathogenesis begins with intestinal adherence
o Stimulation of epithelial mucus production and bacterial biofilm
formation
o Inflammation from epithelial cell exfoliation
Enteroinvasive E. coli (EIEC)
Children and travelers
Uncommon cause of diarrhea
Produces diseases similar to shigellosis
Unlike shigella, it produces disease only at a large inoculum
o 108-1010 CFU
Incubation period: 1-3 days
Symptoms are usually self-limited (7-10 days)
o Colonization and invasion of the colonic mucosa -> replication
therein and cell-to-cell spread -> development of inflammatory
colitis
Fever
Abdominal pain
Tenesmus
Scant stool containing mucus, blood, and inflammatory cells
Can cause sepsis and meningitis
Diagnosis
Differentiation between inflammatory and non-inflammatory diarrhea
o Non-inflammatory: most commonly viral
o Inflammatory: usually bacterial
ETEC, EPEC, EAEC and DAEC are uncommon cause of non-
inflammatory diarrhea
ETEC causes majority of causes of non-inflammatory traveler’s diarrhea
CPU College of Medicine | Magnus Animus Medicus | 2021 Page 5 of 6
Recommended Immunization Schedule (Adult)
Vaccine 19-21 22-26 years 27-49 50-64 ≥65
years years years years
Influenza 1 dose annually
Tdap/Td 1 dose Tdap, then Td booster every 10 yrs
MMR 1 or 2 doses depending on indication (if
born in 1957 or later)
VAR 2 doses
RZV 2 doses
ZVL 1 dose
HPV- 2 or 3 doses depending
Female on age at series
initiation
HPV- 2 or 3 Depending
Male doses on age at
series
initiation
PCV13 1 dose
PPSV23 1 or 2 doses depending on indication 1 dose
HepA 2 or 3 doses depending on vaccine
HepB 3 doses
Men 1 or 2 doses depending on indication, then booster every 5
ACWY yrs if risk remains
MenB 2 or 3 doses depending on vaccine
Hib 1 or 3 doses depending on indication
CPU College of Medicine | Magnus Animus Medicus | 2021 Page 6 of 6
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Common HCC Codes and Diabetes Manifestations SheetDocument2 pagesCommon HCC Codes and Diabetes Manifestations SheetmeikaizenNo ratings yet
- Oration ExampleDocument1 pageOration ExampleChristille Lindy Joyce Caluyo74% (19)
- Questions:: Exercise 4. Bioethical Dilemma of Gene TherapyDocument2 pagesQuestions:: Exercise 4. Bioethical Dilemma of Gene Therapyrjay manaloNo ratings yet
- Community-Acquired Pneumonia - CPG 2016Document26 pagesCommunity-Acquired Pneumonia - CPG 2016Jamie SebastianNo ratings yet
- Trans - Clin Patho 1 (Pre-Analysis and Specimen Collection)Document6 pagesTrans - Clin Patho 1 (Pre-Analysis and Specimen Collection)Christille Lindy Joyce CaluyoNo ratings yet
- Abdomen XrayDocument82 pagesAbdomen Xraypriyasureddi8004100% (2)
- Neck Mass NewDocument9 pagesNeck Mass NewWahyu Permata LisaNo ratings yet
- Neck MassesDocument7 pagesNeck MassesSaad AbdullahNo ratings yet
- Endorsement Case Discussion JULY 29, 2020 Patient # 39 I. General DataDocument9 pagesEndorsement Case Discussion JULY 29, 2020 Patient # 39 I. General DataChristille Lindy Joyce CaluyoNo ratings yet
- SmallpoxDocument24 pagesSmallpoxChristille Lindy Joyce Caluyo100% (1)
- Journal in ZoologyDocument1 pageJournal in ZoologyChristille Lindy Joyce CaluyoNo ratings yet
- Australian Responses To Human Trafficking-ACRATH Feb2008Document21 pagesAustralian Responses To Human Trafficking-ACRATH Feb2008Christille Lindy Joyce CaluyoNo ratings yet
- HIV para Sa FilipinoDocument6 pagesHIV para Sa FilipinoChristille Lindy Joyce CaluyoNo ratings yet
- Sustainable DevelopmentDocument37 pagesSustainable DevelopmentSheetal RawatNo ratings yet
- UntitledDocument1 pageUntitledChristille Lindy Joyce CaluyoNo ratings yet
- High Dose Rate Interstitial Brachytherapy Using Two Weekly SessionsDocument1 pageHigh Dose Rate Interstitial Brachytherapy Using Two Weekly SessionsZuriNo ratings yet
- EBUS Kazuhiro YasufukuDocument27 pagesEBUS Kazuhiro YasufukuOrion JohnNo ratings yet
- TRS 987Document286 pagesTRS 987NGOTTANo ratings yet
- Public Health Microbiology - 4th EdDocument39 pagesPublic Health Microbiology - 4th EdaphethuxolomNo ratings yet
- Pharmaceutical Assasination (Partial)Document14 pagesPharmaceutical Assasination (Partial)jamie_clark_2100% (2)
- Basic Anaestetic DrugsDocument1 pageBasic Anaestetic DrugsLuthfi AfiatNo ratings yet
- G PsumatDocument22 pagesG PsumattimworkmakesthedreamworkNo ratings yet
- Enhanced Recovery After Surgery (Eras) Protocols vs. Standard Care in Patients With Peptic Ulcer PerforationDocument8 pagesEnhanced Recovery After Surgery (Eras) Protocols vs. Standard Care in Patients With Peptic Ulcer PerforationIJAR JOURNALNo ratings yet
- Biotechnology & Drug Discovery.Document35 pagesBiotechnology & Drug Discovery.IrsaNo ratings yet
- Importance of Mental HealthDocument2 pagesImportance of Mental HealthCp CsNo ratings yet
- Urinalysis Control - Level 2 (Urnal Control 2) : Cat. No. UC5034 Lot No. 737UC Size: Expiry: 2015-10Document6 pagesUrinalysis Control - Level 2 (Urnal Control 2) : Cat. No. UC5034 Lot No. 737UC Size: Expiry: 2015-10Meiliana ThanNo ratings yet
- Ventouse - FinalDocument10 pagesVentouse - FinalJasmine KaurNo ratings yet
- BupropionDocument3 pagesBupropionRJ HNo ratings yet
- Abstract Leftsidest SetDocument1,047 pagesAbstract Leftsidest Setpokharelriwaj82No ratings yet
- Textbook ReadingDocument275 pagesTextbook ReadingNovitasari EkaNo ratings yet
- 0812 Gelofusine PDFDocument2 pages0812 Gelofusine PDFMsglow WulanNo ratings yet
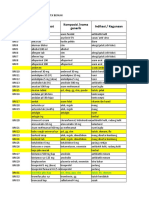
- Nama Obat Indikasi / Kegunaan Komposisi /nama Generik: Brochifar Plus Kap PCT, DMP, Ppa, CTM Batuk, Flu, DemamDocument52 pagesNama Obat Indikasi / Kegunaan Komposisi /nama Generik: Brochifar Plus Kap PCT, DMP, Ppa, CTM Batuk, Flu, Demamrio1995No ratings yet
- Diabetes Advisor - A Medical Expert System For Diabetes ManagementDocument5 pagesDiabetes Advisor - A Medical Expert System For Diabetes ManagementPrincess LunieNo ratings yet
- 2nd Semester Pe and Health 11Document3 pages2nd Semester Pe and Health 11Mae Ann Daganos100% (3)
- Seminar Conduction System of HeartDocument61 pagesSeminar Conduction System of HeartKirtishAcharyaNo ratings yet
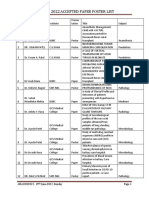
- Amacon2022-Accepted Paper Poster ListDocument35 pagesAmacon2022-Accepted Paper Poster ListViraj ShahNo ratings yet
- Rih - Lower Extremity Runoff Cta Ge Lightspeed 16 / Optima Ct580 ProtocolDocument1 pageRih - Lower Extremity Runoff Cta Ge Lightspeed 16 / Optima Ct580 ProtocolRafieLugassektiNo ratings yet
- Contractura 11 PDFDocument2 pagesContractura 11 PDFVillateAngelaNo ratings yet
- Juvenile Rheumatoid ArthritisDocument30 pagesJuvenile Rheumatoid ArthritisAnonymous dFSZ2k2IUNo ratings yet
- Essential Medicines Lists Punjab 2014Document65 pagesEssential Medicines Lists Punjab 2014Salman Nazir WattuNo ratings yet
- Bacteremia Fungemia, and Blood Cul Tures-V1Document53 pagesBacteremia Fungemia, and Blood Cul Tures-V1Alok MishraNo ratings yet
- DrugsDocument2 pagesDrugsJeff MarekNo ratings yet
- Individual Exercise: Date Frequency Intensity Time TypeDocument2 pagesIndividual Exercise: Date Frequency Intensity Time TypeMillcent GonzalesNo ratings yet