Professional Documents
Culture Documents
New Technique For Obesity Surgery: Internal Gastric Plication Technique Using Intragastric Single-Port (Igs-Igp) in Experimental Model
Uploaded by
Radu MiricaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
New Technique For Obesity Surgery: Internal Gastric Plication Technique Using Intragastric Single-Port (Igs-Igp) in Experimental Model
Uploaded by
Radu MiricaCopyright:
Available Formats
ABCDDV/12
ABCD Arq Bras Cir Dig Original Article - Technique
2017;30(1):60-64
DOI: /10.1590/0102-6720201700010017
NEW TECHNIQUE FOR OBESITY SURGERY: INTERNAL GASTRIC
PLICATION TECHNIQUE USING INTRAGASTRIC SINGLE-PORT
(IGS-IGP) IN EXPERIMENTAL MODEL
Nova técnica para a cirurgia da obesidade: Plicatura Intragástrica Single Port Intragástrico (IGS-IGP) reduz em média 51% do
volume gástrico em modelo experimental
Verena MÜLLER1, Panagiotis FIKATAS1, Safak GÜL1, Maximilian NOESSER1, Kirs
ten FUEHRER1, Igor SAUER1, Johann PRATSCHKE1, Ricardo ZORRON1
From the 1Center for Innovative Surgery ABSTRACT – Background: Bariatric surgery is currently the most effective method to
(ZIC), Center for Bariatric and Metabolic ameliorate co-morbidities as consequence of morbidly obese patients with BMI over 35 kg/
Surgery, Department of General, Visceral m2. Endoscopic techniques have been developed to treat patients with mild obesity and
and Transplant Surgery, Campus Virchow ameliorate comorbidities, but endoscopic skills are needed, beside the costs of the devices.
Klinikum and Department of General, Aim: To report a new technique for internal gastric plication using an intragastric single port
Visceral, Vascular and Thoracic Surgery, device in an experimental swine model. Methods: Twenty experiments using fresh pig cadaver
Campus Mitte, Charité-Universitätsmedizin, stomachs in a laparoscopic trainer were performed. The procedure was performed as follow
Berlin, Germany. in ten pigs: 1) volume measure; 2) insufflation of the stomach with CO2; 3) extroversion of
the stomach through the simulator and installation of the single port device (Gelpoint
Applied Mini) through a gastrotomy close to the pylorus; 4) performance of four intragastric
handsewn 4-point sutures with Prolene 2-0, from the gastric fundus to the antrum; 5) after
the performance, the residual volume was measured. Sleeve gastrectomy was also performed
in further ten pigs and pre- and post-procedure gastric volume were measured. Results: The
internal gastric plication technique was performed successfully in the ten swine experiments.
The mean procedure time was 27±4 min. It produced a reduction of gastric volume of a
HEADINGS - Morbid obesity. Bariatric mean of 51%, and sleeve gastrectomy, a mean of 90% in this swine model. Conclusion: The
surgery. Laparoscopy. Endoscopic internal gastric plication technique using an intragastric single port device required few skills
sleeve gastroplasty. Intragastric sleeve to perform, had low operative time and achieved good reduction (51%) of gastric volume in
gastroplication an in vitro experimental model.
Correspondência: RESUMO – Racional: A cirurgia bariátrica é atualmente o método mais efetivo para melhorar
Ricardo Zorron as co-morbidades decorrentes da obesidade mórbida com IMC acima de 35 kg/m2.
E-mail: rzorron@gmail.com Técnicas endoscópicas foram desenvolvidas para tratar pacientes com obesidade leve
e melhorar as comorbidades, mas habilidades endoscópicas são necessárias, além dos
Fonte de financiamento: não há custos. Objetivo: Relatar uma nova técnica para a plicatura gástrica interna utilizando um
Conflito de interesse: não há. dispositivo intragástrico de portal único em modelo experimental de suínos. Métodos: Foram
realizados 20 experimentos utilizando estômagos de cadáver de porco fresco em um instrutor
Recebido para publicação: laparoscópico. O procedimento foi realizado da seguinte forma em dez porcos: 1) medida
Aceito para publicação: de volume; 2) insuflação do estômago com CO2; 3) extroversão do estômago através do
simulador e instalação do dispositivo de uma única via (Gelpoint Applied Mini) através de
uma gastrotomia próxima ao piloro; 4) realização de quatro suturas de quatro pontos intra-
gástricas com Prolene 2-0, desde o fundo gástrico até o antro; 5) medição do volume residual.
A gastrectomia vertical foi também realizada em mais dez suínos e o volume gástrico pré e
pós-procedimento foi medido. Resultados: A técnica de plicatura gástrica interna foi realizada
com sucesso nos dez experimentos com suínos. O tempo médio do procedimento foi de
27±4 min. Produziu redução do volume gástrico em média de 51%, e a gastrectomia vertical
em média de 90% neste modelo suíno. Conclusão: A técnica de plicatura gástrica interna,
DESCRITORES - Obesidade mórbida. utilizando um dispositivo intragástrico de uma única via, exigiu poucas habilidades para ser
Cirurgia bariátrica. Laparoscopia. realizada, teve baixo tempo operatório e obteve boa redução (51%) do volume gástrico em
Gastroplastia vertical. um modelo experimental in vitro.
INTRODUCTION
T
he increase of obesity to one third of the world population1 calls for more
than 370 million people who are currently suffering type 2 Diabetes Mellitus
(T2DM)2metabolic surgery has been shown to be more effective in reducing
mortality, improving hyperglycemia, hypertension and dyslipidemia in randomized clinical
trials among patients with obesity and type 2 diabetes. However, surgery also has the
risk for acute perioperative complications, long-term micronutrient deficiencies and
psychological problems. Weighing these risks against the benefits of significant weight
loss and improved glycemic control, metabolic surgery seems to be a promising treatment
option for obesity-associated type 2 diabetes. However, current guidelines and treatment
60 ABCD Arq Bras Cir Dig 2017;30(1):60-64
NEW TECHNIQUE FOR OBESITY SURGERY: INTERNAL GASTRIC PLICATION TECHNIQUE USING INTRAGASTRIC SINGLE-PORT (IGS-IGP) IN EXPERIMENTAL MODEL
algorithms for the treatment of type 2 diabetes either ignore or (Figure 5). Plastinate models were produced filling the alterated
underestimate the potential of metabolic surgery. In my opinion, specimens with cyanoacrylate to evaluate internal luminal
metabolic surgery should be considered earlier in the treatment anatomy for IGP and SG (Figure 6). A summary of the procedure
of type 2 diabetes and obesity and no longer be considered as can be reviewed in the video (video1).
the last therapeutic option for patients with obesity-associated
type 2 diabetes.. Conservative medical treatment for obesity
and/or T2DM does not seem to be successful. Multimodal
RESULTS
therapies such as exercises, dietary change and cognitive
therapy alone are little effective. Bariatric surgery is the most A total of 10 internal gastric plication procedures and 10
effective and sustainable treatment for obesity3. Roux-en-Y sleeve gastrectomy procedures were performed in an ex-vivo
gastric bypass (RYGB), sleeve gastrectomy (SG), adjustable gastric swine cadaver stomach model. Mean total procedure time for the
banding and the biliopancreatic diversion, in combination with plications was 27±4 min per stomach. The mean preoperative
cognitive therapy and internal medicine, are the most successful volume of the pig stomachs was 884 ml (510ml-1260ml). The
treatment options for morbid obesity4. Endoscopic methods mean volume after the plications was 341±169 ml. The mean
are recently evolving as a promising alternative for these volume after the sleeve gastrectomy was 63±23ml. The mean
patients. The endoscopically placed gastric balloon seems to percentage of the volume reduction for IGS was 51±25% (Table
be a safe transitional procedure for losing weight. The Apollo 1). The mean volume reduction after sleeve gastrectomy was
Overstich® is an endoscopic suturing device which has been 90±5%. There was a high significantly difference between
currently used to perform gastric volume reduction in the style postoperative gastric volume, after IGP and after SG (p<0.005).
of the sleeve gastrectomy without resection of the stomach5.
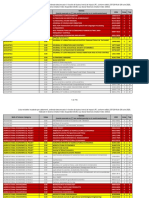
Another recent surgical procedure is the laparoscopic greater TABLE 1 - Intragastric water volume measure of specimens
gastric curvature plication (LGCP). It is a procedure that reduces before surgery and after IGS-IGP
the gastric volume using sutures that invaginates the greater
curvature, avoiding stapling or gastric resection, and aiming Volume Volume Volume reduction
Pig
preoperative in ml postoperative in ml in %
to reduce morbidity and costs for obesity surgery6,7. Although
1 800 740 8
with good excess weight loss in clinical series, it still causes
2 610 420 31
perioperative morbidity due to the gastric devascularisation 3 510 440 14
without gastric resection. 4 1000 350 65
Our group recently presented a new technique for 5 1000 340 66
intraluminal gastric surgery using an intragastric single port 6 710 240 66
device, the IGS-IGP technique, for a series of clinical application 7 510 200 61
for resection of intragastric benign tumors8. Adapting this access 8 510 250 51
for IGS-IGP can potentially produce a new bariatric restrictive 9 900 290 68
procedure with advantages over LGCP and the endoscopic 10 740 140 81
sleeve gastroplasty. Mean 683 ml Mean 341 ml Mean 51%
The objective of this study was to evaluate the effectiveness
of IGP in promoting gastric volume reduction in an experimental Plastinate models were produced filling the lumen of
set. procedural alterated specimens with colored cyanoacrylate
to evaluate internal luminal anatomy for IGP and SG. The
METHODS models showed the altered anatomy after the plication and
the disposition of the remaining cavities (Figure 6).
Between November and December 2015, 20 procedures
were performed in the experimental surgery at our institution. DISCUSSION
The experimental model consisted of ex-vivo fresh pig cadaver
stomachs installed in a laparoscopic single port trainer (Applied Bariatric surgery is the most effective and sustainable
Medical, Rancho Santa Margarida, CA, USA) (Figures 1-3). treatment for obesity3. When compared with each other, certain
The procedure was performed as follows in ten pigs: procedures resulted in greater weight loss and improvements
1) for measuring the initial pre-procedural gastric volume, in comorbidities than others. Outcomes were similar between
each stomach was filled with water to a pressure of 50 mmHG RYGB and SG, and both of these procedures had better outcomes
(0.06 Bar); 2) the stomach wall was then extroverted and fixed than adjustable gastric banding. Although with optimal results
to the laparoscopic trainer single port orifice, and opened a in reducing weight and ameliorating co-morbidities for these
2 cm anterior incision close to the pylorus; 3) the single port patients, RYGB and SG are associated with some complications
device (Gelpoint Applied Mini, Applied Medical, Rancho Santa due to the technical issues of stapling and anastomosing, with
Margarida, CA, USA) was inserted intragastrically through the a risk of leaks and fistulas reported in nearly 1% of the cases9.
2 cm gastrotomy (Figure 2 A-B); 4) the lumen was insufflated New less invasive methods have been developed to
inside the simulator with CO2 (1-2 mmHg), and a 30 degrees promote an effective therapy without the potential problems of
optic, a laparoscopic needle holder and a grasper were inserted penetrating or resecting the gastric wall. To reduce the capacity
through the single port; 5) four handsewing full-thickness of the stomach and allowing mechanical restriction to food
4-point sutures with Prolene 2-0 were performed from the intake is a known effective mechanism to promote weight loss
fundus to the antrum in each stomach (Figure 4 A-B); 6) after for morbidly obese patients9. At least three current bariatric and
finishing the procedure, the entrance defect was closed with metabolic procedures are based on gastric volume reduction,
Vicryl-0 running suture and the stomach was filled with water as the laparoscopic adjustable gastric banding (LAGB), SG and
under pressure again and the residual volume was measured laparoscopic greater curvature plication (LGCP).
(Figure 5). O’Brien et al10 described a 15 year follow up for patients
In further ten pigs, sleeve gastrectomy was performed by with adjustable gastric banding. They included 3227 patients,
stapling the antrum and greater curvature over a 36F bougie. with a mean body mass index of 43,8 kg/m2, and 714 had
Post-procedural gastric volume was also measured. As a result completed at least ten years of follow-up. They showed 47%
of the internal plication, the technique produced macroscopic of excess weight loss at 15 years. Angrisani et al compared the
alterations in the form and capacity of the plicated stomach laparoscopic adjustable gastric banding with the RYGB with 51
ABCD Arq Bras Cir Dig 2017;30(1):60-64 61
Original Article - Technique
FIGURE 4 – A) Internal laparoscopic view after the first suture
performed at the gastric fundus (FU) and the
resulting gastric sleeve tubular anatomy (GS)
is shown, as the gastric suture plication (GPL)
is performed along the greater curvature (GC),
leaving the lesser curvature (LC) intact; B) final
aspect of gastric reduction and altered anatomy
by intragastric greater curvature plication
FIGURE 1 - Schematic illustration for performing IGS-IGP for
gastric volume reduction as a new restrictive
bariatric procedure. A single port device is inserted
in the antral part of the stomach, and variable
laparoscopic instruments can be inserted for
intragastric surgery
FIGURE 5 – A) Final external aspect after concluding IGS internal
FIGURE 2 - Schematic illustration for performing IGS-IGP for sleeve plication; B) measuring the gastric volume
gastric volume reduction in an ex-vivo experimental after the anatomical modification, filling the
swine model: A) a single port device is inserted in stomach with high pressured (50 mmHg) of water
the antral part of the stomach, and laparoscopic
intragastric suturing is performed using four
interrupted sutures; B) intragastric greater
curvature plication is started from the fundus
region, progressing with further non-absorbable
sutures to the antrum and, finally, the entry incision
is closed with running suture
FIGURE 6 - Plastinate model with cyanoacrylate showing
differences in postoperative anatomy after IGS-
IGP (A) and sleeve gastrectomy (B)
FIGURE 3 - External view and team position at laparoscopic
trainer for single port intragastric surgery (IGS)
for internal sleeve plication
62 ABCD Arq Bras Cir Dig 2017;30(1):60-64
NEW TECHNIQUE FOR OBESITY SURGERY: INTERNAL GASTRIC PLICATION TECHNIQUE USING INTRAGASTRIC SINGLE-PORT (IGS-IGP) IN EXPERIMENTAL MODEL
patients in a period of five years11. Mean BMI before surgery The results of our study show that the IGP-IGS technique
was 43 kg/m2. The mean BMI at 12 months after surgery was is feasible and produces, ex-vivo, a significant reduction in the
35 for the RYGB and 39 for the LAGB, decreasing to 29 for the gastric volume by restricting its area of distension. It is possible
RYGB and 36 for the LAGB after three years and staying the to reduce the volume of the stomach without resecting or
same for the RYGB at 29 and still decreasing for the LAGB at bypassing it. It is also possible to perform a surgical gastric
35 after five years. Excess weight loss was significantly higher plication without devascularization, by acting intraluminally. The
in the RYGB group after five years (67% RYGB and 48% LAGB). entry wound in the antral region does not produces relevant
Himpens et al12 showed an excess weight loss of 73% three morbidity in our clinical experience with IGS for resection of
years after and 58% six years after SG, similar to the findings intragastric tumors. In studies, LGCP seems to be as effective
of Diamantis et al13, with an EWL of 62% at five years after and as the sleeve gastrectomy regarding EWL and ameliorating
54% at six years after SG. comorbidities. The IGP-IGS can potentially be as effective as that
Talebpour et al shared their 12 years experience in 800 with less operative time, as there is no need to entry the rest of
patients submitted to LGCP14. The mean BMI of their patients the peritoneal cavity nor to liberate the gastric vessels or vessel
was 42 kg/m2; the mean EWL was 20% after one month (n=779), ligation. Leaks, gastric necrosis or bleeding are improbable, as the
67% after 12 months (n=491), 70% after 24 months (n=356), 66% technique does not induce gastric ischemia. A shorter learning
after three years (n=251), 62% after four years (n=176) and 55% curve is expected, it is a procedure with only one incision and
after five years (n=134) following surgery. Severe complications only one technical step. It also is reversible by just cutting the
occurred in 1% of the patients, including gastric necrosis and suture lines, endoscopically, within the first weeks after the
enteric fistulae. They had to perform operative revisions because operation. As the endoscopic similar technique - endoscopic
of regain in 32 cases and failure in six cases. These findings show sleeve gastroplasty - it can be followed by surgical malabsorptive
in the literature similar effects in EWL of LGCP to the SG13,15. In methods as a second stage operation in cases with insufficient
a systematic review, the complication rate of the LGCP seems weight loss without any change to previous surgery.
to be higher16. There were minor complications with a rate of Survival studies have to be addressed to evaluate the
11%, such as nausea and vomiting and major complications feasibility and safety of the technique.
including bleeding, leaks, gastric obstruction and gastric fistula
in 4%. Still, the procedure has not gained much popularity due
to the possibility of these complications, compared to the low
CONCLUSION
rates in the literature for RYGB or SG.
Endoscopic alternatives were developed to fill the gap The consequences of this study cannot be applied yet in
between bariatric procedures with high effectiveness but the clinical practice, as experimental survival studies are needed
with more complications, and the conservative therapy, less to prove the feasibility and safety of IGP. Its evaluation as a
harmful but less efficient in obtaining sustainable weight valuable method for therapy of morbid obesity, in achieving
loss. The endoscopically placed gastric balloon seems to be sustainable weight loss, is the next step of our research.
a safe procedure for losing weight, but a metanalysis showed
that it is only a short-term effective treatment, but it is not
yet capable to maintain a weight loss over a long period of
ACKNOWLEDGEMENTS
time17. However, this therapy only seems to be successful in
very compliant patients and weight regain after removal of the The authors thank Applied Medical Germany for their
balloon is common17-20. research support providing simulators and disposable materials.
The novel endoscopic suturing device available in the
market, Apollo Overstich®, has been currently used to perform a REFERENCES
gastric volume reduction in the style of the SG without resection
of the stomach5. Abu Dayyeh et al used this device in 2013 in
1. Ng M, Fleming T, Robinson M, et al. Global, regional, and national
four patients with a mean BMI of 36 kg/m2. The procedure time prevalence of overweight and obesity in children and adults during
was 172 to 245 min and they placed 26 sutures5. Lopez-Nava et 1980–2013: a systematic analysis for the Global Burden of Disease Study
al used the Apollo overstitch as well in 50 patients21. The mean 2013. Lancet. 2014;6736(14):1-16.
procedure time was 66 min and they placed seven sutures on 2. Blüher M. [Insulin or surgery? : The perspective of a diabetologist]. Chirurg.
2014;85(11):957-962.
average with five stitches in each suture. They did not measure
3.CarlssonLMS,PeltonenM,AhlinS,etal.BariatricSurgeryandPreventionofType
the volume of the stomach pre- and post-intervention. Oral 2 Diabetes in Swedish Obese Subjects. N Engl J Med. 2012;367(8):695-704.
contrast studies in addition with an endoscopy were optional 4. Schauer PR, Kashyap SR, Wolski K, et al. Bariatric Surgery versus Intensive
for the patients at 24 h, three and six months. The mean BMI Medical Therapy in Obese Patients with Diabetes. N Engl J Med.
changed from 37.7±4,6 kg/m2 to 30.9±5,1 kg/m2 at one year 2012;366(17):1567-1576.
5. Abu Dayyeh BK, Rajan E, Gostout CJ. Endoscopic sleeve gastroplasty:
follow up. The indication of this therapy is currently applied to
a potential endoscopic alternative to surgical sleeve gastrectomy for
low-BMI patients5,21,22, but indication for superobese as a first step treatment of obesity. Gastrointest Endosc. 2013;78(3):530-535.
procedure for a 2nd stage strategy is recently described23,24. The 6. Bradnova O, Kyrou I, Hainer V, et al. Laparoscopic Greater Curvature
technique seems promising, but long-term results and studies Plication in Morbidly Obese Women with Type 2 Diabetes: Effects on
with larger series are needed to evaluate the effectiveness of Glucose Homeostasis, Postprandial Triglyceridemia and Selected Gut
Hormones. Obes Surg. 2014;24(5):718-726.
this method in the morbidly obese population.
7. Fried M, Dolezalova K, Buchwald JN, McGlennon TW, Sramkova P, Ribaric
The physiology of our proposed IGP technique is potentially G. Laparoscopic greater curvature plication (LGCP) for treatment of morbid
similar to the endoscopic gastric plication and not similar to the obesity in a series of 244 patients. Obes Surg. 2012;22(8):1298-1307.
laparoscopic gastric plication, where the greater curvature is 8.Intragastrische (IGS) Single-Port-Chirurgie bei großen gutartigen
denervated and devascularized, and the plicated stomach wall Magentumoren. R Zorron, C Bothe, M Holtmann, T Junghans. Zeitschrift
für Gastroenterologie 53 (08), KC096
is compressed to the lumen. In IGP, there is rather a delaying
9. Laparoscopic greater curvature plication: initial results of an alternative
in gastric emptying caused by the shortening of the stomach restrictive bariatric procedure. Ramos A, Galvao Neto M, Galvao M,
and the impaired motility due to the sutures. In fact, in a recent Evangelista LF, Campos JM, Ferraz A. Obes Surg. 2010 Jul;20(7):913-8.
study evaluating postoperative scintigraphic findings on patients 10. O’Brien PE, MacDonald L, Anderson M, Brennan L, Brown W. Long-term
submitted to endoscopic sleeve gastroplasty, Abu Dayyeh outcomes after bariatric surgery: fifteen-year follow-up of adjustable
gastric banding and a systematic review of the bariatric surgical literature.
reported a delayed gastric emptying, recognizing a complete
Ann Surg. 2013;257(1):87-94.
different mechanism of action of this therapy, if compared with
SG, where on the contrary a rapid gastric emptying is expected25.
ABCD Arq Bras Cir Dig 2017;30(1):60-64 63
Original Article - Technique
11. Angrisani L, Lorenzo M, Borrelli V. Laparoscopic adjustable gastric 19.Yasawy M, Al-Quorain A, Hussameddin A, Al-Sulaiman R, Yasawy Z.
banding versus Roux-en-Y gastric bypass: 5-year results of a prospective Obesity and gastric balloon. J Fam Community Med. 2014;21(3):196.
randomized trial. Surg Obes Relat Dis. 2007;3(2):127-132. 20. Milone L, Strong V, Gagner M. Laparoscopic sleeve gastrectomy is
12. Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic superior to endoscopic intragastric balloon as a first stage procedure
sleeve gastrectomy for obesity. Ann Surg. 2010;252(2):319-324. for super-obese patients (BMI ±50). Obes Surg. 2005;15:612-617.
13. Diamantis T, Apostolou KG, Alexandrou A, Griniatsos J, Felekouras E, 21. Lopez-Nava G, Galvão MP, Bautista-Castaño I, Jimenez-Baños A,
Tsigris C. Review of long-term weight loss results after laparoscopic Fernandez-Corbelle JP. Endoscopic Sleeve Gastroplasty: How I Do It?
sleeve gastrectomy. Surg Obes Relat Dis. 2014;10(1):177-183. Obes Surg. 2015;25(8):1534-1538. doi:10.1007/s11695-015-1714-7.
14. Talebpour M, Kalantar Motamedi HM, Talebpour A, Vahidi H. Twelve 22.Galvao MP, Grecco E, Souza TF, Quadros LG, Silva LB, Campos JM.
year experience of laparoscopic gastric plication in morbid obesity: Endoscopic sleeve gastroplasty- minnimally invasive therapy for primary
development of the technique and patient outcomes. Ann Surg Innov obesity treatment. ABCD Arch Bras Cir Dig 2016; 29 (1): 95-97.
Res. 2012;6(1):7. 23. Sharaiha RZ, Kedia P, Kumta N, DeFilippis EM, Gaidhane M, Shukla
15.Chouillard E, Schoucair N, Alsabah S, Alkandari B. Laparoscopic Gastric A, Aronne LJ, Kahaleh M. Initial experience with endoscopic sleeve
Plication ( LGP ) as an Alternative to Laparoscopic Sleeve Gastrectomy gastroplasty: technical success and reproducibility in the bariatric
( LSG ) in Patients with Morbid Obesity : A Preliminary , Short-Term , population. Endoscopy 2015; 47: 164-166.
Case-Control Study. 2015:4-9. 24. Zorron R, Galvão-Neto MP, Campos J, Branco AJ, Sampaio J, Junghans
16. Ji Y, Wang Y, Zhu J, Shen D. A systematic review of gastric plication for the T, Bothe C, Benzing C, Krenzien F., From Complex Evolving to Simple:
treatment of obesity. Surg Obes Relat Dis. 2014 Nov-Dec;10(6):1226-32. Current Revisional and Endoscopic Procedures following Bariatric Surgery,
17. Imaz I, Martínez-Cervell C, García-Álvarez EE, Sendra-Gutiérrez JM, Arq Bras Cir Dig. 2016; 29(1):128-133.
González-Enríquez J. Safety and effectiveness of the intragastric balloon 25. Abu Dayyeh BK, Acosta A, Camilleri M, Mundi MS, Rajan E, Topazian
for obesity. A meta-analysis. Obes Surg. 2008;18(7):841-846. MD, Gostout CJ. Endoscopic sleeve gastroplasty alters gastric physiology
18. Roman S, Napoléon B, Mion F, et al. Intragastric balloon for “non-morbid” and induces loss of body weight in obese individuals. Clin Gastroenterol
obesity: A retrospective evaluation of tolerance and efficacy. Obes Surg. Hepatol. 2015 Dec 31. pii: S1542-3565(15)01714-0. doi: 10.1016/j.
2004;14(4):539-544. cgh.2015.12.030. [Epub ahead of print] PMID:26748219
64 ABCD Arq Bras Cir Dig 2017;30(1):60-64
You might also like
- Laparoscopic Sleeve GastrectomyFrom EverandLaparoscopic Sleeve GastrectomySalman Al-SabahNo ratings yet
- Apollo 2 Años 2017Document3 pagesApollo 2 Años 2017angelrullNo ratings yet
- Impact of Sleeve Gastrectomy Volumes On Weight Loss Results: A Prospective StudyDocument6 pagesImpact of Sleeve Gastrectomy Volumes On Weight Loss Results: A Prospective StudyDavid Campos AvilaNo ratings yet
- Technical Modification For Sleeve GastrectomyDocument5 pagesTechnical Modification For Sleeve GastrectomyJorge SalazarNo ratings yet
- Study 4Document6 pagesStudy 4angelrullNo ratings yet
- Study 5Document4 pagesStudy 5angelrullNo ratings yet
- Changes in Gastric Volume and Their Implications For Weight Loss After Laparoscopic Sleeve GastrectomyDocument7 pagesChanges in Gastric Volume and Their Implications For Weight Loss After Laparoscopic Sleeve GastrectomyAndrés MaldonadoNo ratings yet
- Study 2Document7 pagesStudy 2angelrullNo ratings yet
- 1 Octombrie 2019Document4 pages1 Octombrie 2019Radu MiricaNo ratings yet
- 8 Mai 2020Document3 pages8 Mai 2020Radu MiricaNo ratings yet
- Case Report Effects of Cryolipolysis On Abdominal AdiposityDocument8 pagesCase Report Effects of Cryolipolysis On Abdominal AdiposityIcetrick StormNo ratings yet
- Initial Experience With Endoscopic Sleeve Gastroplasty in PolandDocument7 pagesInitial Experience With Endoscopic Sleeve Gastroplasty in PolandvictorNo ratings yet
- 2019 Simplified Minimally Invasive Surgical Approach For Prophylactic Laparoscopic Gastropexy in 21 CasesDocument8 pages2019 Simplified Minimally Invasive Surgical Approach For Prophylactic Laparoscopic Gastropexy in 21 CasesrizalakbarsyaNo ratings yet
- CholeL During BariatricDocument6 pagesCholeL During BariatriclucasakrNo ratings yet
- Surgical Endoscopy 6Document102 pagesSurgical Endoscopy 6Saibo BoldsaikhanNo ratings yet
- Acute Rehabilitation Program After Laparoscopic Colectomy Using Intravenous LidocaineDocument6 pagesAcute Rehabilitation Program After Laparoscopic Colectomy Using Intravenous LidocaineKu Badlisyah Ku AzizNo ratings yet
- Sleeve-Gastrectomy 2011 BrethauerDocument15 pagesSleeve-Gastrectomy 2011 BrethauerDavid Schnettler RodriguezNo ratings yet
- DRP2018 5276528Document9 pagesDRP2018 5276528cientifico FismatekNo ratings yet
- Laparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyDocument4 pagesLaparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Laparoscopic Vs Open Appendectomy: Which Way To Go?Document22 pagesLaparoscopic Vs Open Appendectomy: Which Way To Go?fahryzal_noteNo ratings yet
- Dietary Intake and Ghrelin and Leptin Changes After SleeveDocument8 pagesDietary Intake and Ghrelin and Leptin Changes After Sleevea12345644321No ratings yet
- Laparoscopic Sleeve Gastrectomy: Perioperative Outcomes, Weight Loss and Impact On Type 2 Diabetes Mellitus Over 2 YearsDocument5 pagesLaparoscopic Sleeve Gastrectomy: Perioperative Outcomes, Weight Loss and Impact On Type 2 Diabetes Mellitus Over 2 YearsYondri Mandaku TasidjawaNo ratings yet
- Ansu 265 466Document8 pagesAnsu 265 466BlayneNo ratings yet
- Technical Options For Malabsorption Issues After Single Anastomosis Duodenoileal Bypass With Sleeve GastrectomyDocument5 pagesTechnical Options For Malabsorption Issues After Single Anastomosis Duodenoileal Bypass With Sleeve GastrectomyAlexandraNo ratings yet
- 379 EnglishDocument7 pages379 EnglishDarshan SDNo ratings yet
- GASTROPEXI2Document5 pagesGASTROPEXI2taigorengNo ratings yet
- Initial Efficacy and Tolerability of Early Enteral Nutrition With Immediate or Gradual Introduction in Intubated PatientsDocument6 pagesInitial Efficacy and Tolerability of Early Enteral Nutrition With Immediate or Gradual Introduction in Intubated PatientsUCI COVID Pediátrico HNGAINo ratings yet
- Resultados Iniciales de Un Programa de Cirugía Hepato-Bilio-Pancreática Laparoscópica en El Hospital Regional de TalcaDocument9 pagesResultados Iniciales de Un Programa de Cirugía Hepato-Bilio-Pancreática Laparoscópica en El Hospital Regional de TalcaNicolás Javier Acevedo OjedaNo ratings yet
- Zorrilla-Nunez ProofDocument3 pagesZorrilla-Nunez ProofDr. Luis Fernando Zorrilla NúñezNo ratings yet
- Preliminary Information About Intraperitoneal Hypertermic Chemoterapy (Iphc) in Abdominal CancerDocument29 pagesPreliminary Information About Intraperitoneal Hypertermic Chemoterapy (Iphc) in Abdominal CancerViorica StoianNo ratings yet
- 10.1007@s11695 020 05012 2Document9 pages10.1007@s11695 020 05012 2Andrés MaldonadoNo ratings yet
- Short Term Volumetric Changes of The Stomach Following Laparoscopic Sleeve Gastrectomy Versus Laparoscopic Gastric PlicationDocument7 pagesShort Term Volumetric Changes of The Stomach Following Laparoscopic Sleeve Gastrectomy Versus Laparoscopic Gastric PlicationDrGeorge Saad AbdallaNo ratings yet
- Laparoscopic Sleeve Gastrectomy: A Radiological Guide To Common Postsurgical FailureDocument13 pagesLaparoscopic Sleeve Gastrectomy: A Radiological Guide To Common Postsurgical FailureAlexandraNo ratings yet
- 3 Potential Hormone Mechanisms of Bariatric SurgeryDocument13 pages3 Potential Hormone Mechanisms of Bariatric SurgeryJuan Luis RuizNo ratings yet
- Billroth I & IIDocument5 pagesBillroth I & IIRoxieparkerNo ratings yet
- 3.BASIC Pharmacologic PrinciplesDocument2 pages3.BASIC Pharmacologic PrinciplesBenjie Balisi0% (1)
- 20 Iunie 2017Document3 pages20 Iunie 2017Radu MiricaNo ratings yet
- Effects of Cryolipolysis On Lower Abdomen Fat ThicknessDocument8 pagesEffects of Cryolipolysis On Lower Abdomen Fat ThicknessAline soaresNo ratings yet
- Criolipolise X CavitaçãoDocument6 pagesCriolipolise X CavitaçãoPolyana AlencarNo ratings yet
- Bariatric Surgery: 1. Predominantly Malabsorptive ProceduresDocument9 pagesBariatric Surgery: 1. Predominantly Malabsorptive ProceduresmegangstaNo ratings yet
- Sap 0b013e31827e29e5Document5 pagesSap 0b013e31827e29e5randomaeiou7273No ratings yet
- World Journal of Surgical Oncology: Alternative Reconstruction After PancreaticoduodenectomyDocument4 pagesWorld Journal of Surgical Oncology: Alternative Reconstruction After PancreaticoduodenectomyPra YudhaNo ratings yet
- Cistectomia Radical Art08 PDFDocument7 pagesCistectomia Radical Art08 PDFJoshua GardnerNo ratings yet
- Magenstrasse GastroplastyDocument8 pagesMagenstrasse GastroplastyalaaNo ratings yet
- Bowel Exposure in Rectal Cancer IMRT Using Prone, Supine, or A Belly Board (2012)Document8 pagesBowel Exposure in Rectal Cancer IMRT Using Prone, Supine, or A Belly Board (2012)Michelle LEINo ratings yet
- 2018 Article 892-Dy7nDocument12 pages2018 Article 892-Dy7nCaroline Ruffo FogassaNo ratings yet
- Abdominoplasty With Customized Transverse Musculoaponeurotic PlicationsDocument9 pagesAbdominoplasty With Customized Transverse Musculoaponeurotic PlicationsМаратNo ratings yet
- LSG Vs LGB Vs RYGBDocument7 pagesLSG Vs LGB Vs RYGBRadu MiricaNo ratings yet
- One Anastomosis Gastric Bypass (OAGB) : The Story Behind A Name With 20 Years of HistoryDocument3 pagesOne Anastomosis Gastric Bypass (OAGB) : The Story Behind A Name With 20 Years of HistoryTan BulNo ratings yet
- Colonic Atresia Revision 1Document10 pagesColonic Atresia Revision 1HenggarAPNo ratings yet
- Gastric GIST Treatment by Laparoscopy Report of 49 Cases and Literature's ReviewDocument4 pagesGastric GIST Treatment by Laparoscopy Report of 49 Cases and Literature's ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Clavien Dildo Complications Assesment in Bariatric SurgeryDocument6 pagesClavien Dildo Complications Assesment in Bariatric SurgeryErlan SantosNo ratings yet
- CD3 Z X9 M Yqtpxfy 8 PY457 WC WJFNDocument4 pagesCD3 Z X9 M Yqtpxfy 8 PY457 WC WJFNWalaa AbuzaidNo ratings yet
- CreonDocument12 pagesCreonNikola StojsicNo ratings yet
- 23 August 2012Document6 pages23 August 2012Radu MiricaNo ratings yet
- Original Research ArticleDocument9 pagesOriginal Research ArticleAnand ShanmugaiahNo ratings yet
- Three Methods For HysterectomyDocument73 pagesThree Methods For HysterectomyAjeej0% (1)
- Treatmen 3Document6 pagesTreatmen 3Livia GudacNo ratings yet
- 01 HepatogastroDocument3 pages01 Hepatogastroyacine26No ratings yet
- Jurnal DindaDocument6 pagesJurnal Dindachiendo ymNo ratings yet
- Gastroesophageal Reflux Disease, Obesity and Laparoscopic Sleeve Gastrectomy - The Burning Questions PDFDocument10 pagesGastroesophageal Reflux Disease, Obesity and Laparoscopic Sleeve Gastrectomy - The Burning Questions PDFMateo TamayoNo ratings yet
- Medicina: Is It Safe To Combine A Fundoplication To Sleeve Gastrectomy? Review of LiteratureDocument7 pagesMedicina: Is It Safe To Combine A Fundoplication To Sleeve Gastrectomy? Review of LiteratureRadu MiricaNo ratings yet
- 15 Octombrie 2021Document13 pages15 Octombrie 2021Radu MiricaNo ratings yet
- 4 Decembrie 2021Document8 pages4 Decembrie 2021Radu MiricaNo ratings yet
- 8 Mai 2020Document3 pages8 Mai 2020Radu MiricaNo ratings yet
- 6 August 2019Document6 pages6 August 2019Radu MiricaNo ratings yet
- 1 Octombrie 2019Document4 pages1 Octombrie 2019Radu MiricaNo ratings yet
- 29 Noiembrie 2016Document4 pages29 Noiembrie 2016Radu MiricaNo ratings yet
- 23 August 2012Document6 pages23 August 2012Radu MiricaNo ratings yet
- 21 Septembrie 2017Document4 pages21 Septembrie 2017Radu MiricaNo ratings yet
- Ianuarie 2017Document6 pagesIanuarie 2017Radu MiricaNo ratings yet
- 7 Aprilie 2017Document8 pages7 Aprilie 2017Radu MiricaNo ratings yet
- Bariatric Surgery and Gastroesophageal Reflux Disease: Darius Ashrafi, Emma Osland, Muhammed Ashraf MemonDocument7 pagesBariatric Surgery and Gastroesophageal Reflux Disease: Darius Ashrafi, Emma Osland, Muhammed Ashraf MemonRadu MiricaNo ratings yet
- 3 Ianuarie 2021Document8 pages3 Ianuarie 2021Radu MiricaNo ratings yet
- 20 Iunie 2017Document3 pages20 Iunie 2017Radu MiricaNo ratings yet
- 18 Iunie 2013Document6 pages18 Iunie 2013Radu MiricaNo ratings yet
- 28 Septembrie 2015Document11 pages28 Septembrie 2015Radu MiricaNo ratings yet
- Review Article: To Sleeve or NOT To Sleeve in Bariatric Surgery?Document5 pagesReview Article: To Sleeve or NOT To Sleeve in Bariatric Surgery?Radu MiricaNo ratings yet
- Mai 2015Document5 pagesMai 2015Radu MiricaNo ratings yet
- Covid-19 Pandemic and Bariatric Surgery in ArgentinaDocument7 pagesCovid-19 Pandemic and Bariatric Surgery in ArgentinaRadu MiricaNo ratings yet
- 15 Aprilie 2011Document6 pages15 Aprilie 2011Radu MiricaNo ratings yet
- 23 August 2012Document6 pages23 August 2012Radu MiricaNo ratings yet
- Review Article: To Sleeve or NOT To Sleeve in Bariatric Surgery?Document5 pagesReview Article: To Sleeve or NOT To Sleeve in Bariatric Surgery?Radu MiricaNo ratings yet
- Bile Acids, FXR, and Metabolic Effects of Bariatric SurgeryDocument8 pagesBile Acids, FXR, and Metabolic Effects of Bariatric SurgeryRadu MiricaNo ratings yet
- Boan Et Al 2004 Bariatric SurgeryDocument8 pagesBoan Et Al 2004 Bariatric SurgeryRadu MiricaNo ratings yet
- If Clasamente2020Document716 pagesIf Clasamente2020Radu MiricaNo ratings yet
- Recommendations To Manage Patients For Bariatric Surgery in The COVID-19 Pandemic: Experience From ChinaDocument4 pagesRecommendations To Manage Patients For Bariatric Surgery in The COVID-19 Pandemic: Experience From ChinaRadu MiricaNo ratings yet
- AIS Clasamente2020Document651 pagesAIS Clasamente2020Radu MiricaNo ratings yet
- AIS Clasamente2020Document651 pagesAIS Clasamente2020Radu MiricaNo ratings yet
- Comparison of Percentage Excess Weight Loss After LaparoscopicDocument6 pagesComparison of Percentage Excess Weight Loss After LaparoscopicRadu MiricaNo ratings yet
- Legal Medicine FinalsDocument13 pagesLegal Medicine FinalsBo DistNo ratings yet
- Carnoy's Solution in The Management of Odontogenic KeratocystDocument4 pagesCarnoy's Solution in The Management of Odontogenic KeratocystlydiaNo ratings yet
- Foundation of Professional Nursing PracticeDocument15 pagesFoundation of Professional Nursing PracticeArnie Jude CaridoNo ratings yet
- Smith & Nephew Fast-Fix 360 CurvedDocument12 pagesSmith & Nephew Fast-Fix 360 CurvedTomi GunawanNo ratings yet
- 2018 Surgical Rescue in Medical PatientsDocument11 pages2018 Surgical Rescue in Medical PatientsgiseladlrNo ratings yet
- KingdomNomics Reflections Part 1Document45 pagesKingdomNomics Reflections Part 1adelani_oni100% (1)
- Vision & Mission: Healthc Are Solution GroupDocument16 pagesVision & Mission: Healthc Are Solution GroupFajar Pandu WijayaNo ratings yet
- Iso Medec PDFDocument98 pagesIso Medec PDFIkoy Setyawan Keren100% (1)
- CyberTherapy & Rehabilitation, Issue 3 (3), Winter 2010.Document52 pagesCyberTherapy & Rehabilitation, Issue 3 (3), Winter 2010.Giuseppe RivaNo ratings yet
- Principles of SurgeryDocument87 pagesPrinciples of SurgeryfiansisNo ratings yet
- UrethrocystographyDocument9 pagesUrethrocystographyyinyangdongNo ratings yet
- A Management Algorithm For Esophageal PerforationDocument4 pagesA Management Algorithm For Esophageal Perforationoscar chirinosNo ratings yet
- Lap Ok HisterektomiDocument4 pagesLap Ok HisterektomiHappy Martha NababanNo ratings yet
- Crucial Roles of Vascular Surgeons in OncovascularDocument8 pagesCrucial Roles of Vascular Surgeons in OncovascularMatias Jurado ChaconNo ratings yet
- An ABC Technical Algorithm To Mangled HandDocument10 pagesAn ABC Technical Algorithm To Mangled HandRoxana LungociNo ratings yet
- Sample Literature ReviewDocument8 pagesSample Literature Review67890ThNo ratings yet
- Anesthetic Care FR Amdominal Surgery - Anesthesiology ClinicsDocument237 pagesAnesthetic Care FR Amdominal Surgery - Anesthesiology ClinicsAbdullah QaziNo ratings yet
- The Lancet Practice by TelephoneDocument4 pagesThe Lancet Practice by TelephoneVincentDuclosNo ratings yet
- Teaching Plan Avninder Deol Norquest College NPRT 2102 Cathy Macdonald February 20, 2021Document10 pagesTeaching Plan Avninder Deol Norquest College NPRT 2102 Cathy Macdonald February 20, 2021Neena Deol100% (1)
- Endoscopic Excision of Antrochoanal PolypDocument3 pagesEndoscopic Excision of Antrochoanal PolypreginalisaNo ratings yet
- RPNDocument21 pagesRPNAruna Teja Chennareddy50% (8)
- Panduan Praktik Klinis (PPK) Prosedur Tindakan/Operasi Bedah Orthopedik Rsup Fatmawati Jakarta 2014 - 2016Document2 pagesPanduan Praktik Klinis (PPK) Prosedur Tindakan/Operasi Bedah Orthopedik Rsup Fatmawati Jakarta 2014 - 2016Arbianti AstutiNo ratings yet
- Consenso de Cirurgia em Retocolite Ulcerativa e D de Crohn 2023 GEDIIBDocument19 pagesConsenso de Cirurgia em Retocolite Ulcerativa e D de Crohn 2023 GEDIIBCarla MartinsNo ratings yet
- Colonic InertiaDocument5 pagesColonic InertiaEmilio SanchezNo ratings yet
- Health Development in PakistanDocument3 pagesHealth Development in PakistanMazher Hussain SyalNo ratings yet
- Wound-TypesDocument1 pageWound-TypesJamie W.No ratings yet
- MagiCore Catalog 2Document34 pagesMagiCore Catalog 2PabloNo ratings yet
- AHEL Investor Presentation Jun 21Document54 pagesAHEL Investor Presentation Jun 21Nihar DekaNo ratings yet
- Coding Modifiers TableDocument22 pagesCoding Modifiers TableArindamDuttaChoudhury100% (1)
- Settings Up of OTDocument10 pagesSettings Up of OTshivaguruNo ratings yet
- Relentless: From Good to Great to UnstoppableFrom EverandRelentless: From Good to Great to UnstoppableRating: 5 out of 5 stars5/5 (785)
- Aging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayFrom EverandAging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayNo ratings yet
- Chair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouFrom EverandChair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouRating: 3.5 out of 5 stars3.5/5 (5)
- Power of 10: The Once-A-Week Slow Motion Fitness RevolutionFrom EverandPower of 10: The Once-A-Week Slow Motion Fitness RevolutionRating: 3.5 out of 5 stars3.5/5 (11)
- The Yogi Code: Seven Universal Laws of Infinite SuccessFrom EverandThe Yogi Code: Seven Universal Laws of Infinite SuccessRating: 4.5 out of 5 stars4.5/5 (104)
- Peak: The New Science of Athletic Performance That is Revolutionizing SportsFrom EverandPeak: The New Science of Athletic Performance That is Revolutionizing SportsRating: 5 out of 5 stars5/5 (97)
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindFrom EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindRating: 4.5 out of 5 stars4.5/5 (1)
- Mind Your Body: 4 Weeks to a Leaner, Healthier LifeFrom EverandMind Your Body: 4 Weeks to a Leaner, Healthier LifeRating: 4.5 out of 5 stars4.5/5 (5)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingFrom EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingRating: 4.5 out of 5 stars4.5/5 (66)
- Muscle for Life: Get Lean, Strong, and Healthy at Any Age!From EverandMuscle for Life: Get Lean, Strong, and Healthy at Any Age!Rating: 4.5 out of 5 stars4.5/5 (22)
- Pranayama: The Yoga Science of BreathingFrom EverandPranayama: The Yoga Science of BreathingRating: 4.5 out of 5 stars4.5/5 (8)
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerFrom EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerRating: 4 out of 5 stars4/5 (5)
- Endure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceFrom EverandEndure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceRating: 4.5 out of 5 stars4.5/5 (237)
- Easy Strength: How to Get a Lot Stronger Than Your Competition-And Dominate in Your SportFrom EverandEasy Strength: How to Get a Lot Stronger Than Your Competition-And Dominate in Your SportRating: 4.5 out of 5 stars4.5/5 (17)
- Not a Diet Book: Take Control. Gain Confidence. Change Your Life.From EverandNot a Diet Book: Take Control. Gain Confidence. Change Your Life.Rating: 4.5 out of 5 stars4.5/5 (124)
- The Total Kettlebell Workout: Trade Secrets of a Personal TrainerFrom EverandThe Total Kettlebell Workout: Trade Secrets of a Personal TrainerRating: 5 out of 5 stars5/5 (1)
- Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandYamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (111)
- Enter The Kettlebell!: Strength Secret of the Soviet SupermenFrom EverandEnter The Kettlebell!: Strength Secret of the Soviet SupermenRating: 4 out of 5 stars4/5 (29)
- Roxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingFrom EverandRoxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingRating: 4.5 out of 5 stars4.5/5 (132)
- The Strength and Conditioning Bible: How to Train Like an AthleteFrom EverandThe Strength and Conditioning Bible: How to Train Like an AthleteNo ratings yet
- Tibetan Yoga: Magical Movements of Body, Breath, and MindFrom EverandTibetan Yoga: Magical Movements of Body, Breath, and MindRating: 5 out of 5 stars5/5 (1)
- The Yoga Sutras of Patanjali: The Final Guide for the Study and Practice of Patanjali's Yoga SutrasFrom EverandThe Yoga Sutras of Patanjali: The Final Guide for the Study and Practice of Patanjali's Yoga SutrasNo ratings yet
- Music For Healing: With Nature Sounds For Natural Healing Powers: Sounds Of Nature, Deep Sleep Music, Meditation, Relaxation, Healing MusicFrom EverandMusic For Healing: With Nature Sounds For Natural Healing Powers: Sounds Of Nature, Deep Sleep Music, Meditation, Relaxation, Healing MusicRating: 5 out of 5 stars5/5 (1)
- 80/20 Running: Run Stronger and Race Faster by Training SlowerFrom Everand80/20 Running: Run Stronger and Race Faster by Training SlowerRating: 4.5 out of 5 stars4.5/5 (97)
- 5-Minute Yoga: A More Energetic, Focused, and Balanced You in Just 5 Minutes a DayFrom Everand5-Minute Yoga: A More Energetic, Focused, and Balanced You in Just 5 Minutes a DayRating: 5 out of 5 stars5/5 (2)
- Strength Training Over 40: The Only Weight Training Workout Book You Will Need to Maintain or Build Your Strength, Muscle Mass, Energy, Overall Fitness and Stay Healthy Without Living in the GymFrom EverandStrength Training Over 40: The Only Weight Training Workout Book You Will Need to Maintain or Build Your Strength, Muscle Mass, Energy, Overall Fitness and Stay Healthy Without Living in the GymRating: 4 out of 5 stars4/5 (6)