Professional Documents
Culture Documents
Pharmacoeconomical Evaluationof Oral Hypoglycemic Agents
Uploaded by
NamithaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharmacoeconomical Evaluationof Oral Hypoglycemic Agents
Uploaded by
NamithaCopyright:
Available Formats
Tamilselvan et al., IJPSR, 2017; Vol.
8(5): 2243-2248 E-ISSN: 0975-8232; P-ISSN: 2320-5148
IJPSR (2017), Vol. 8, Issue 5 (Research Article)
Received on 27 October, 2016; received in revised form, 27 December, 2016; accepted, 31 December, 2016; published 01 May, 2017
PHARMACOECONOMICAL EVALUATION OF ORAL HYPOGLYCEMIC AGENTS FOR
TYPE-2 DIABETES MELLITUS IN A MULTISPECIALITY HOSPITAL
T. Tamilselvan *, T. Kumutha, Amrita Lekshmi V., Anju C. James, Juliya S. Reji and Namitha Cheriyan
Department of Pharmacy Practice, Swamy Vivekanandha College of Pharmacy, Elayampalyam - 637205,
India.
Keywords: ABSTRACT: The objective of the study was to determine the cost effective
Pharmacoeconomics, drug among oral hypoglycemic agents utilized in a multispeciality hospital to
Diabetes Mellitus, ICER, Metformin treat type-2 diabetes mellitus. The prospective cost effectiveness study was
Correspondence to Author: conducted for 6 months period in patients who were diagnosed with type-2
Dr. T. Tamilselvan diabetes mellitus and were receiving treatment specifically with oral
hypoglycemic agent(s). The data obtained was introduced to Incremental
Professor and Head,
Department of Pharmacy Practice, Cost Effectiveness Ratio determination to arrive at the most cost effective
Swamy Vivekanandha College of drug and the prescription pattern and drug related problems in the patients
Pharmacy, Elayampalayam - 637205, were monitored. A total of 141 patients were included in the study. Glipizide
Tiruchengode, Tamilnadu, India. among monotherapy (p<0.01), Glimepiride as add on therapy to Metformin
(p<0.001), fixed dose triple combination of Glimepiride, Pioglitazone and
E-mail: tamilrx@gmail.com Metformin (p<0.01) and fixed dose combination of Glimepiride and
Metformin (p<0.001) were found to be more effective using statistical
analysis. Most of the patients were receiving fixed dose combinations
(43.6%) out of which Glimepiride and Metformin combination (34.42%) was
predominant over the others. Serious drug interactions (12) and adverse drug
reactions (5) were monitored. For Type 2 Diabetes Mellitus, Metformin
among monotherapy, Glimepiride as an add on to Metformin, fixed dose
triple combination of Glimepiride, Pioglitazone and Metformin can be
considered as the best drug of choice with respect to cost effectiveness.
INTRODUCTION: Diabetes is a modern-day Prevalence of diabetes among adults has reached
epidemic and is rightly recognized as a global approximately 20% in urban and approximately
public health issue. India leads the world with the 10% in rural populations in India 1. The disease
largest number of diabetic subjects earning the title appears to be more prevalent in the south of the
termed the “Diabetes capital of the world”. country as compared to the northern and eastern
According to the Indian Council of Medical parts 2.
Research (ICMR), in a national diabetes study,
India currently has 62.4 million people with In a developing country like India, 85% of total
diabetes. health expenditures are financed by house-hold out-
of–pocket expenditure. Many poor people
QUICK RESPONSE CODE frequently face a choice between buying medicines
DOI:
10.13040/IJPSR.0975-8232.8(5).2243-48 or buying food or other necessities due to limited
resources and high pricing of drug. The cost
effective analysis of the oral hypoglycemic agents
Article can be accessed online on:
www.ijpsr.com will reduce the healthcare burden on patients with
Diabetes mellitus and reduces the total health
DOI link: http://dx.doi.org/10.13040/IJPSR.0975-8232.8 (5).2243-48 expenditure of the country 3-5.
International Journal of Pharmaceutical Sciences and Research 2243
Tamilselvan et al., IJPSR, 2017; Vol. 8(5): 2243-2248 E-ISSN: 0975-8232; P-ISSN: 2320-5148
Pharmacoeconomics determine the costs and The data was interpreted using ICER quadrant
outcomes associated primarily with plane and the report was developed using ICER
pharmaceuticals address different decision decision matrix.
problems, including cost–utility analysis (CUA),
cost-effectiveness analysis (CEA), cost Statistical Analysis: The statistical analysis was
minimization analysis (CMA) and cost–benefit done using Graph Pad Prism version 6.07. The
analysis (CBA). Pharmacoeconomics is now more HbA1C level before and after the drug treatment
than ever before at the leading edge of thinking in was expressed as Mean ± SD. Paired student t- test
terms of securing the most rational and efficient use was used to analyze the statistical difference
of scarce health-care resources for diabetes 6, 7. The between the HbA1C reductions with various oral
aim of this study was to determine the most cost- hypoglycemic agents. p<0.05 was considered as
effective drug among oral hypoglycemic agents statistically significant.
utilized in a multi-specialty hospital. Other
RESULTS:
objectives of the study were to monitor prescription
Patient demographics: The data collected from
pattern and drug related problems with oral
141 diabetic patients were analyzed and
hypoglycemic agents.
categorized according to the patient demographics.
MATERIALS AND METHODS: This The mean age of the study population was 57.36 ±
Prospective Cost Effective Study was conducted 11.49 years (range 20-80 years), where the
for 6 months in both inpatients and outpatients of maximum number 47 (33.3%) of patients were in
Cardiology, General Medicine and Nephrology the age group of 61-70 years. The male patients 77
Departments with Type 2 Diabetes Mellitus in a (54.6%) were more predominant than female
300 bedded multispecialty hospital located at patients 64 (45.4%). (Table 1)
Elayampalayam. The study was approved by the
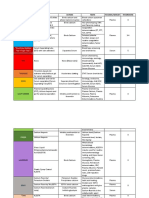
TABLE 1: PATIENT DEMOGRAPHICS
Institutional Ethical Committee of Vivekanandha
No of
Medical Care Hospital. About 383 Type 2 DM Demographics Percentage
Patients
patients were interviewed and based on inclusion (%)
(n=141)
and exclusion criteria, 141 patients were recruited Gender
Males 77 54.6%
in our study after getting the patient consent and Females 64 45.4%
the required data were collected in specially 20-30 Years 01 0.7%
31-40 Years 13 9.0%
designed data entry form. 41-50 Years 21 14.8%
Age
51-60 Years 45 31.9%
The study was included with patients of age 61-70 Years 47 33.3%
between 20 – 80 years in both genders, having 71-80 Years 14 9.9%
Type 2 Diabetes Mellitus prescribed with oral Mean Age 57.36 ± 11.49 Years
hypoglycemic agents. We excluded patients with
age < 20 and > 80 years, Pregnancy and Lactation, Co- Morbidity Assessment: The patients having
patients on insulin therapy, patients with lifestyle normal Body Mass Index (BMI) 68 (48.2%) were
modification alone and patients not willing to more predominant than overweight 48(34.1%) and
repeat glucose monitoring from the study. The underweight 11(7.8%) patients. About 48 (34.05%)
collected data were analyzed and the adherence of patients in the study were having prior family
level of the patients was categorized into low, history of diabetes. The co-morbidities like
medium and high adherence by using Morisky 8– hypertension, hyperlipidemia, Congestive Heart
Item Medication Adherence Scale. failure and Chronic Kidney Disease co-exist with
Diabetes Mellitus, out of which Hypertension
The drug interactions in the prescriptions were (47.5%) was more predominant. Among the other
checked out by using LEXICOMP Software. The co-morbidities hypothyroidism 13 (32.5%) was the
adverse drug reactions were monitored and major followed by Chronic Obstructive Pulmonary
assessed using Naranjo Causality Assessment Disease 9 (22.5%). (Table 2)
Scale.
International Journal of Pharmaceutical Sciences and Research 2244
Tamilselvan et al., IJPSR, 2017; Vol. 8(5): 2243-2248 E-ISSN: 0975-8232; P-ISSN: 2320-5148
TABLE 2: CO- MORBIDITY ASSESSMENT (67.37%) of the patients selected for the study were
No of patients Percentage affected by diabetes for more than 4 years. Only
Co - Morbidity
(n=141) (%)
102 (72.34%) of the patients in the study were
Hypertension 67 47.5%
Hyperlipidemia 11 7.8% strictly adapted to their lifestyle modifications.
Coronary heart disease 6 4.3% 61(43.26%) of the patients were prescribed with
Chronic kidney disease 17 12.1% fixed dose combinations, followed by monotherapy
Hypothyroidism 13 32.5% 35 (24.82%). Highly prescribed oral hypoglycemic
Asthma 8 20% agents in the selected patients in our study was
Angina 6 15%
COPD 9 22.5% Metformin among monotherapy in 11 (31.42%)
Depression 4 10% patients, Glimepiride as an add on to Metformin
Others 40 28.3% among add on therapy in 15 (45.45%) patients,
COPD – Chronic Obstructive Pulmonary Disease Glimepiride + Voglibose + Metformin among fixed
dose triple combinations in 7(58.33 %) patients,
Pharmacist Workup on Drug Therapy: Out of Glimepiride + Metformin among fixed dose
141 patients selected for the study, 124 (87.94%) of combinations in 21 (34.42 %) patients.
patients were outpatients and remaining were
inpatients 17 (12.05%). According to Morisky 8 – About 226 drug interactions were monitored in the
Item Medication Adherence Scale, about 72 (51.08 prescriptions, 71.68% were moderate, 23% were
%) of the diabetic patients in the study were highly minor and 5.3% were major interactions (Fig. 2).
adherent to the drug therapy, 41 (29.07 %) were During the study, 5 adverse drug reactions were
moderately adherent and remaining 28 (19.85 %) monitored, out of which 4 were Probable and an
were having low adherence. About 116 (82.26%) ADR was Definite with respect to Naranjo Adverse
number of the patients were in regular follow up of Drug Reaction Probability Scale. (Table 3)
diabetic treatment. Out of 141 patients, 95
TABLE 3: PHARMACIST WORKUP ON DRUG THERAPY
Characteristics No:of patients (n=141) Percentage (%)
Low 28 19.85%
Adherence level Medium 41 29.05%
High 72 51.1%
Yes 116 82.26%
Regular follow-up
No 25 17.73%
<1 year 15 10.63%
1-2 years 16 11.3%
Duration of therapy
3-4 years 15 10.63%
>4 years 95 67.37%
Yes 102 72.34%
Lifestyle Modifications
No 39 27.66%
Major 12 5.32%
Drug Interactions Moderate 162 71.68%
Minor 52 23%
Probable 8 5.67%
Adverse Drug Reactions
Definite 1 0.7%
Incremental Cost Effectiveness Ratio (ICER) statistical analysis shows that there was a highly
Analysis: The incremental cost effectiveness ratio significant difference between the HbA1C level of
was calculated using ICER formula and the result patients before and after the Glipizide treatment
was based on ICER quadrant plane and ICER (p<0.01) and hence found to be the most effective
decision matrix 8. Metformin shows the maximum drug when compared with other drugs among
HbA1C reduction among monotherapy. The monotherapy.
International Journal of Pharmaceutical Sciences and Research 2245
Tamilselvan et al., IJPSR, 2017; Vol. 8(5): 2243-2248 E-ISSN: 0975-8232; P-ISSN: 2320-5148
TABLE 4: COMPARISON OF ICER OF MONOTHERAPY
Drugs Cost of therapy Mean ± SD of HbA1C Reduction IC IE ICER
for 6 months (Rs) Baseline EOS of HbA1C
Glipizide 126.00 9.3 ± 0.99 8.8 ± 1.01** 0.5 - - -
Metformin 650.16 8.2 ± 1.82 7.1 ± 1.7* 1.1 524.16 0.6 873.6
Glimepiride 628.20 8.8 ± 1.5 8 ± 1.5* 0.9 - 21.96 - 0.2 109.8
Gliclazide 1800.00 7.8 ± 1.6 7.0 ± 1.2* 0.8 1171.8 -0.1 -11718
Pioglitazone 918.00 8.7 ± 1.5 8.1 ± 1.1 0.6 - 882 -0.2 4410
Voglibose 5832.00 9.4 ± 2.2 8.9 ± 1.9 0.5 4914 -0.1 -49140
Sitagliptin 4041 9.6 ± 2.5 9.1 ± 1.8 0.5 - 1791 - -
EOS - End of Study IC- Incremental Cost IE- Incremental Effect
ICER - Incremental Cost Effectiveness Ratio **p < 0.01 * p < 0.05
Considering HbA1c reduction, Glibenclamide as an since there was statistically significant difference
add on to Metformin, shows the maximum HbA1c between the HbA1C level before and after the drug
reduction. The most effective drug was found to be treatment.
Glimepiride as an add on to Metformin (p<0.001)
TABLE 5: COMPARISON OF ICER OF ADD ON THERAPY
Drugs Cost of Mean ± SD of HbA1C Reduction IC IE ICER
therapy for 6 Baseline EOS of HbA1C
months (Rs)
Metformin + 749.16 9.1 ± 1.6 7.9 ± 1.63** 1.2 - - -
Glibenclamide
Metformin + 1278.36 8.5 ± 1.3 7.5 ± 1.27*** 1.4 529.2 0.2 2646
Glimepiride
Metformin + 2178.36 8 ± 2.15 7.1 ± 2.10 0.2 900 - 1.2 -750
Gliclazide
Voglibose + 6750.00 9.1 ± 1.9 8.5 ± 1.2 0.63 4571.64 0.43 10631.72
Pioglitazone
Metformin + 4691.16 8.9 ± 2.4 8.1 ± 2.12 0.5 -2058.84 -0.13 15837.23
Sitagliptin
EOS - End of Study IC- Incremental Cost IE- Incremental Effect
ICER - Incremental Cost Effectiveness Ratio, *** p < 0.001 **p < 0.01
Fixed dose triple combination of Glimepiride, the HbA1C levels of the patient tested before and
Pioglitazone and Metformin, shows the maximum after the Glimepiride + Pioglitazone + Metformin
HbA1C reduction. The statistical analysis shows (p<0.01) treatment, which was found to be more
that there was highly significant difference between effective.
TABLE 6: COMPARISON OF ICER OF FIXED DOSE TRIPLE COMBINATIONS
Drugs Cost of therapy for 6 Mean ± SD of HbA1C Reduction IC IE ICER
months (Rs) of HbA1C
Baseline EOS
Glimepiride + 221.40 0.8 - - -
Voglibose + 11.3 ± 1.57 10.5 ± 1.95*
Metformin
Glimepiride + 4176.00 1.4 3954.6 0.6 6591
Pioglitazone + 9.8 ± 1.2 8.4 ± 1.58**
Metformin
Metformin + 4691.16 8.9 ± 2.4 8.1 ± 2.12 0.5 -2058.84 -0.13 15837.23
Sitagliptin
EOS - End of Study IC- Incremental Cost IE- Incremental Effect
ICER - Incremental Cost Effectiveness Ratio, **p < 0.01 * p < 0.05
DISCUSSION: Diabetes mellitus is a It is a chronic illness, which in most cases is treated
multifactorial metabolic disorder. The main defects for life; hence the cost associated with it is
include insulin resistance and insulin deficiency 9. enormous 17.
International Journal of Pharmaceutical Sciences and Research 2246
Tamilselvan et al., IJPSR, 2017; Vol. 8(5): 2243-2248 E-ISSN: 0975-8232; P-ISSN: 2320-5148
Few data exists as regards its cost to the patient and our result was Glibenclamide and Metformin.
the society in developing countries. These data may These findings are supported by Christian Diaz de
help to make a suitable policy in selection of Leon Castaneda et.al which performed Cost
formulations, decision taking and motivation for effectiveness study of oral hypoglycemic agents in
adherence to the therapy 10, 11. the treatment of outpatients with type-2 diabetes
attending a public primary care clinic in Mexico
The study was comprised of 141 patients, out of City 16.
which, most of the patients (33.3%) were in the age
group of 61-70 years. In the study, the male The drug interactions were monitored in the
patients (54.6 %) were more predominant in prescriptions and there were 12 (5.30%) major
number than the female patients. González-Ortiz M interactions. About 71.68% of moderate and 23%
et al performed a study on Efficacy of minor drug interactions were also present in the
Glimepiride/Metformin combination versus study. The interaction between Dalteparin and
Glibenclamide/Metformin in patients with Clopidogrel was the majorly identified drug
uncontrolled type 2 diabetes mellitus 12. Their interaction (1.42%), in which there will be an
findings substantiate the result in our study which enhanced risk of hemorrhage.
also concluded that Metformin/Glimepiride is more
effective in reducing HbA1C (p<0.001) than other About 5 Adverse Drug Reactions were identified in
fixed dose combinations. the study, out of which one was Definite and the
remaining 4 were Probable. The definite ADR was
Among monotherapy, Glipizide (p < 0.01) was Furosemide induced Hyponatremia and Vomiting
found to be the most effective anti diabetic drug in with Naranjo Score of nine.
reducing HbA1C in our study. It was supported by
the study performed by Diana Sherfali et.al which CONCLUSION: Economic evaluation of therapy
performed the effect of oral Antidiabetic drugs on should be encouraged to ensure cost effective
A1C levels and concluded that Thiazolidinediones therapy for diabetic patients. For the initial
and Sulphonylureas are most effective in HbA1C treatment of Type 2 Diabetes Mellitus, Metformin
reduction 13. A meta-analysis of Comparison of may be considered as cost-effective monotherapy.
different drugs as add-on treatments to Metformin If blood glucose is inadequately controlled with
in type 2 diabetes was performed by Monami M monotherapy, Glimepiride may be suggested in
et.al which concluded that sulphonylureas are more terms of cost effectiveness, as an add on to
effective in HbA1C reduction when given as add Metformin. For uncontrolled Type 2 Diabetes
on to Metformin 14. These findings are resemblance Mellitus, fixed dose combination of Glimepiride
to our study which shows that Glimepiride as an and Metformin can be considered as the best drug
add to Metformin (p<0.001) was the most effective of choice with respect to cost effectiveness.
among the add-on-therapy. Patients who do not obtain optimal glycemic
control with a fixed dose combination of oral
In our study, among add-on-therapy, Glimepiride hypoglycemic agents can be considered with fixed
was most cost effective in reducing HbA1C. These dose triple combinations, out of which combination
findings are similar to those reported by Scott of Glimepiride, Metformin and Pioglitazone was
Klarenbach et.al, which performed a prospective found to be the best choice.
analysis on Cost effectiveness of second line anti-
hyperglycemic therapy in patients with type-2 The use of multiple drugs by patients can
diabetes mellitus inadequately controlled on contribute to various drug interactions, which may
Metformin. They concluded that Sulphonylureas as sometimes be severe. This can be prevented by
a second line agent are most cost effective in close monitoring of drug therapy and avoiding use
glycemic control when added to Metformin of multiple drugs for less severe indications.
monotherapy 15.
ACKNOWLEDGEMENT: I would like to
Considering the HbA1C reduction, the most cost acknowledge Dr. S. Arthananreeswaran, Executive
effective drug among fixed dose combinations in
International Journal of Pharmaceutical Sciences and Research 2247
Tamilselvan et al., IJPSR, 2017; Vol. 8(5): 2243-2248 E-ISSN: 0975-8232; P-ISSN: 2320-5148
Director, Vivekanandha Medical Care Hospital, hospitalized adults. Am J Health Syst Pharm. 2015; 72 (7):
525-535.
Tiruchengode, Tamilnadu, India for giving me an 9. Giwa Abdulganiyu, Tayo Fola: Cost-effectiveness analysis
opportunity and guiding our research work. of anti-diabetic therapy in a university teaching hospital.
International Journal of Pharmacy and Pharmaceutical
Sciences.2014; 6(2): 82-91.
DECLARATION OF INTEREST: The author 10. Asrul Akmal Shafie, Vishal Gupta, Ranya Baabbad, Eva
has declared no conflict of interest. Hammerby et al: An analysis of the short- and long-term
cost-effectiveness of starting biphasic insulin aspart 30 in
insulin-naıve people with poorly controlled type 2
REFERENCES: diabetes. Diabetes Res Clin Prac. 2012; 2:11-14.
11. Andrea C Tricco, Huda M Ashoor, Jesmin Antony, Joseph
1. Suresh Purohit, Dev Priya, B.L.Pandey, Prabhat Beyene et al: Safety, effectiveness, and cost effectiveness
Upadhyay: A Review on Study of Drug Prescribing of long acting versusintermediate acting insulin for
Pattern in Diabetes in India. British Journal of Medical and patients with type 1 diabetes: systematic review and
Health Research. 2015; 2(10): 12-15. network meta-analysis. BMC Health Services Research.
2. Seema Abhijeet Kaveeshwar and Jon Cornwall: The 2014; 2:73.
current state of diabetes mellitus in India. Australasian 12. González-Ortiz M, Guerrero-Romero JF, Violante-Ortiz R,
Medical Journal. 2014; 7(1): 45-48. Wacher-Rodarte N et al: Efficacy of Glimepiride/
3. Abdelaziz MSL, Shobha Rani H, Ravindranath S, Ramjan Metformin combination versus Glibenclamide/Metformin
shaik et al: Pharmacoeconomic evaluation of oral- in patients with uncontrolled Type 2 Diabetes Mellitus. J
hypoglycemic agents at hospital in Bangalore. IOSR Diabetes Complications.2009; 23(6):376-379.
Journal of Pharmacy and Biological Sciences. 2015; 13. Diana Sherifali, RN, Kara Nerenberg, Eleanor
10(5):46-50. Pullenayegum, Ji Emmy Cheng et al: The Effect of Oral
4. Charalampos Tzanetakos, Andreas Melidonis, Antidiabetic Agents on A1C Levels. Diabetic Care. 2010;
Christos Verras, Georgia Kourlaba et al: Cost- 33(8):1859 – 1864.
effectiveness analysis of Liraglutide versus Sitagliptin or 14. Monami M, Caterina Lamanna, Niccolò Marchionni,
Exenatide in patients with inadequately controlled Type 2 Edoardo Mannucc: Comparison of different drugs as add-
diabetes on oral antidiabetic drugs in Greece. BMC Health on treatments to metformin in type 2 diabetes: A meta-
Services Research. 2014; 14:419. analysis. Diabetes Res Clin Prac. 2008; 79(2):196-203.
5. M. Charokopou, Postema R, Townsend R, Roudaut M et 15. Scott Klarenbach, Chris Cameron, Sumeet Singh, UR:
al: Cost-effectiveness of Dapagliflozin versus DPP-4 Cost-effectiveness of second-line antihyperglycemic
inhibitors as an add-on to Metformin in the Treatment of therapy in patients with type 2 diabetes mellitus
Type 2 from a UK Healthcare System Perspective. BMC inadequately controlled on metformin. Canadian Medical
Health Services Research. 2015; 15:496. Association Journal.2011; 183(16):1213-1220.
6. Marcelo Eidi Nita, Freddy G. Eliaschewitz, Eliane Ribeiro, 16. Christian Diaz de Leon Castaneda, Marina Altagracia-
Elio Asano et al: Cost-effectiveness and budget impact of Martínez, Jaime Kravzov-Jinich, Ma del Rosario
saxagliptin as additional therapy to metformin for the Cárdenas-Elizalde et al: Cost-effectiveness study of oral
treatment of diabetes mellitus type 2 in the Brazilian hypoglycemic agents in the treatment of outpatients with
private health system. Applied Microbiology and type 2 diabetes attending a public primary care clinic in
Biotechnology. 2012; 58(3):294-301. Mexico City. Clinicoecon Outcomes Res. 2012; 4: 57–65.
7. Pedro Mezquita Raya, Antonio Pérez, Antonio Ramírez de 17. Irina Odnoletkova, Geert Goderis, Lore Pil, Frank Nobels
Arellano, Teresa Briones et al: Incretin Therapy for Type 2 et al: Cost-effectiveness of therapeutic education to
Diabetes in Spain: A Cost-Effectiveness Analysis of prevent the development and progression of type 2
Liraglutide Versus Sitagliptin. Journal of Diabetes diabetes: systematic review. Journal of Diabetes &
Therapy. 2013; 4(2): 417-430. Metabolism. 2014; 5:9.
8. Singh K, Ansari MT, Patel RV, Bedard M et al:
Comparative efficacy and safety of insulin analogs in
How to cite this article:
T Tamilselvan, Kumutha T, Lekhmi VA, James AC, Reji JS and Cheriyan N: Pharmacoeconomical evaluation of oral hypoglycemic
agents for type-2 diabetes mellitus in a multispeciality hospital. Int J Pharm Sci Res 2017; 8(5): 2243-48.doi: 10.13040/IJPSR.0975-
8232.8(5).2243-48.
All © 2013 are reserved by International Journal of Pharmaceutical Sciences and Research. This Journal licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License.
This article can be downloaded to ANDROID OS based mobile. Scan QR Code using Code/Bar Scanner from your mobile. (Scanners are available on Google
Playstore)
International Journal of Pharmaceutical Sciences and Research 2248
You might also like
- Pharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyFrom EverandPharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyRating: 4.5 out of 5 stars4.5/5 (3)
- Nicotine - It May Have A Good Side - Harvard HealthDocument3 pagesNicotine - It May Have A Good Side - Harvard HealthzimkoNo ratings yet
- Ka 1Document6 pagesKa 1DHIVYANo ratings yet
- 21 Iajps21102017 PDFDocument9 pages21 Iajps21102017 PDFBaru Chandrasekhar RaoNo ratings yet
- Ismail 2013Document6 pagesIsmail 2013Nawang WulanNo ratings yet
- Drug Prescribing Patterns in Elderly Patients in A Tertiary Level HospitalDocument6 pagesDrug Prescribing Patterns in Elderly Patients in A Tertiary Level Hospitalsangita sukumaranNo ratings yet
- Drug Utilization Pattern of Anti-Diabetic Drugs Among Diabetic Outpatients in A Tertiary Care HospitalDocument3 pagesDrug Utilization Pattern of Anti-Diabetic Drugs Among Diabetic Outpatients in A Tertiary Care HospitalTazkiyatan IsriaNo ratings yet
- Patient adherence to oral hypoglycemic medications in Saudi ArabiaDocument5 pagesPatient adherence to oral hypoglycemic medications in Saudi ArabiamajedNo ratings yet
- Laporan Esktrak KERSENDocument4 pagesLaporan Esktrak KERSENMetiiNo ratings yet
- Article Wjpps 1469869064Document10 pagesArticle Wjpps 1469869064Lucia SibiiNo ratings yet
- Prescribing Patterns of Drugs in Outpatient Department of Paediatrics in Tertiary Care HospitalDocument12 pagesPrescribing Patterns of Drugs in Outpatient Department of Paediatrics in Tertiary Care HospitalAleena Maria KurisinkalNo ratings yet
- Selfcare and Related Factors in Patients With Type 2 DiabetesDocument5 pagesSelfcare and Related Factors in Patients With Type 2 DiabetesCM GabriellaNo ratings yet
- 2699 PDFDocument4 pages2699 PDFSeptya widhiafniNo ratings yet
- Literature ReviewDocument53 pagesLiterature ReviewJEMY JOSENo ratings yet
- Medication Adherence in Type 2 Diabetes PatientsDocument7 pagesMedication Adherence in Type 2 Diabetes PatientsCMargs ConceptsNo ratings yet
- Cost-Effective Analysis in Treating Diabetes Mellitus With ComorbidityDocument5 pagesCost-Effective Analysis in Treating Diabetes Mellitus With ComorbidityMONISH NAYARNo ratings yet
- REVIEWDocument20 pagesREVIEWSanjeet DuhanNo ratings yet
- 673 FullDocument7 pages673 FullAq IfahNo ratings yet
- Assessment On Prevalence of Polypharmacy in Geriatric Patients With Cardiovascular DiseasesDocument12 pagesAssessment On Prevalence of Polypharmacy in Geriatric Patients With Cardiovascular DiseasesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Drug-Related Problems in Hypertensive Patients With Multiple ComorbiditiesDocument8 pagesDrug-Related Problems in Hypertensive Patients With Multiple ComorbiditiesHIDAYATNo ratings yet
- Jurnal Interaksi Haloperidol Dan TrihexyphenidylDocument8 pagesJurnal Interaksi Haloperidol Dan TrihexyphenidylIka LismayaniNo ratings yet
- JMCP 2023 29 1 58Document11 pagesJMCP 2023 29 1 58Javier Martin Bartolo GarciaNo ratings yet
- JJJGJHGJHGHDocument6 pagesJJJGJHGJHGHTaufik NurohmanNo ratings yet
- WNL 2022 201574Document10 pagesWNL 2022 201574triska antonyNo ratings yet
- Impact of Pharmaceutical Care On The Health-RelateDocument14 pagesImpact of Pharmaceutical Care On The Health-RelatealfinadyaNo ratings yet
- KetorolacDocument16 pagesKetorolacniken retnoNo ratings yet
- Potentially Inappropriate Prescribing and Cost Outcomes For Older People: A National Population StudyDocument10 pagesPotentially Inappropriate Prescribing and Cost Outcomes For Older People: A National Population Studybiotech_vidhyaNo ratings yet
- Jurnal Baru 4Document8 pagesJurnal Baru 4FIRDA RIDHAYANINo ratings yet
- Refractory Epilepsy Diagnosis and Management: Local Experience at National Guard Hospital in Jeddah, KSADocument18 pagesRefractory Epilepsy Diagnosis and Management: Local Experience at National Guard Hospital in Jeddah, KSAOmar MohammedNo ratings yet
- Drug Prescribing Pattern in Surgical Wards of A TeDocument6 pagesDrug Prescribing Pattern in Surgical Wards of A TeNiranjan ChapagainNo ratings yet
- Department of Pharmacology and Pharmacy Practice, KVSR Siddhartha College of Pharmaceutical Sciences, Siddhartha Nagar, Vijayawada-520010Document1 pageDepartment of Pharmacology and Pharmacy Practice, KVSR Siddhartha College of Pharmaceutical Sciences, Siddhartha Nagar, Vijayawada-520010Ishana SNo ratings yet
- 1161-Article Text-4602-1-10-20211228Document6 pages1161-Article Text-4602-1-10-20211228amar prasadNo ratings yet
- 1161 Jphi QCRDDocument6 pages1161 Jphi QCRDamar prasadNo ratings yet
- Drug Utilization Evaluation of Antidiabetic Drugs Among Type 2 Diabetes Patients of Tamil NaduDocument4 pagesDrug Utilization Evaluation of Antidiabetic Drugs Among Type 2 Diabetes Patients of Tamil NaduMelly MV HutasoitNo ratings yet
- PHAR Article 73597 en 1Document7 pagesPHAR Article 73597 en 1AhmadNo ratings yet
- The Study of Drug Usage Patterns in Pediatric Patients at MGM Hospital, Navi MumbaiDocument10 pagesThe Study of Drug Usage Patterns in Pediatric Patients at MGM Hospital, Navi Mumbairajesh sumanNo ratings yet
- Comparison of Modified-NUTRIC, NRS-2002 and MUST Scores in Iranian Critically Ill Patients Admitted en CONTRADocument20 pagesComparison of Modified-NUTRIC, NRS-2002 and MUST Scores in Iranian Critically Ill Patients Admitted en CONTRAwguzmanNo ratings yet
- Complementary Therapies Used by Diabetes Patients in IndonesiaDocument17 pagesComplementary Therapies Used by Diabetes Patients in IndonesiariyanrestuNo ratings yet
- Prevalence of Diabetic Retinopathy in Type II Diabetic Patients in A Health Facility in Karachi, PakistanDocument8 pagesPrevalence of Diabetic Retinopathy in Type II Diabetic Patients in A Health Facility in Karachi, PakistanJaveria RphNo ratings yet
- Abughosh Et Al 2017 A Motivational Interviewing Intervention by Pharmacy Students To Improve Medication AdherenceDocument12 pagesAbughosh Et Al 2017 A Motivational Interviewing Intervention by Pharmacy Students To Improve Medication AdherenceKat HerNo ratings yet
- Jurnal DiabetesDocument7 pagesJurnal DiabetesIid Zii' Killmz ClaserNo ratings yet
- A Study of Prescription Pattern of Antibiotics in Pediatric In-Patients of Mc-Gann Teaching Hospital Shivamogga Institute of Medical Sciences (SIMS), Shivamogga, Karnataka.Document5 pagesA Study of Prescription Pattern of Antibiotics in Pediatric In-Patients of Mc-Gann Teaching Hospital Shivamogga Institute of Medical Sciences (SIMS), Shivamogga, Karnataka.International Organization of Scientific Research (IOSR)No ratings yet
- 1 PBDocument11 pages1 PBUsman SyaroniNo ratings yet
- Evaluation of Antidiabetic Drug Use in Type 2 Diabetes Mellitus Patients With Chronic Kidney Disease at Dr. M. Djamil Hospital PadangDocument5 pagesEvaluation of Antidiabetic Drug Use in Type 2 Diabetes Mellitus Patients With Chronic Kidney Disease at Dr. M. Djamil Hospital PadangInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Journal LL LL PediatriDocument4 pagesJournal LL LL PediatriIndra PermanaNo ratings yet
- PICU DDIsDocument8 pagesPICU DDIsFAHAD KHANNo ratings yet
- Clinical Epidemiology and Global Health: Original ArticleDocument4 pagesClinical Epidemiology and Global Health: Original Articleinnani wildaniaNo ratings yet
- Submitted 30 July 2021, Accepted 18 October 2022 AbstractDocument7 pagesSubmitted 30 July 2021, Accepted 18 October 2022 Abstractfahrunsiddik5No ratings yet
- Chakelba 2013Document9 pagesChakelba 2013Nawang WulanNo ratings yet
- AntidiabeticDrugsPJMR 20153p96 98Document4 pagesAntidiabeticDrugsPJMR 20153p96 98Tayyaba RahatNo ratings yet
- Adverse Effects of Oral Hypoglycemic Agents and Adherence To Them Among Patients With Type 2 Diabetes Mellitus in NepalDocument7 pagesAdverse Effects of Oral Hypoglycemic Agents and Adherence To Them Among Patients With Type 2 Diabetes Mellitus in NepalZH. omg sarNo ratings yet
- Giardia 2Document6 pagesGiardia 2Martha SánchezNo ratings yet
- CAD DDIsDocument9 pagesCAD DDIsFAHAD KHANNo ratings yet
- Beers Criteria Journal of Applied Pharmaceutical ScienceDocument8 pagesBeers Criteria Journal of Applied Pharmaceutical Sciencenurul.kusumawardani nurul.kusumawardaniNo ratings yet
- Adherence and Quality of Life Among Diabetic Patients With HypertensionDocument6 pagesAdherence and Quality of Life Among Diabetic Patients With HypertensionIJPHSNo ratings yet
- Prescribing Patterns and Pharmacoeconomic Analysis of Drugs Used in Pediatric Asthma Patients at Tertiary Care HospitalDocument18 pagesPrescribing Patterns and Pharmacoeconomic Analysis of Drugs Used in Pediatric Asthma Patients at Tertiary Care Hospitalrajesh sumanNo ratings yet
- The Impact of Clinical Pharmacists InterDocument7 pagesThe Impact of Clinical Pharmacists Interahmed1fkwnNo ratings yet
- Reducing Inappropriate Polypharmacy The Process of DeprescribingDocument8 pagesReducing Inappropriate Polypharmacy The Process of DeprescribingThiago SartiNo ratings yet
- Assessment of Patient's Knowledge, Attitude and Practice Regarding HypertensionDocument6 pagesAssessment of Patient's Knowledge, Attitude and Practice Regarding HypertensionScintya NasutionNo ratings yet
- Homeopathic Preparations For Preventing and Treating Acute Upper Respiratory Tract Infections in Children: A Systematic Review and Meta-AnalysisDocument10 pagesHomeopathic Preparations For Preventing and Treating Acute Upper Respiratory Tract Infections in Children: A Systematic Review and Meta-AnalysisCarlos Arturo Vera VásquezNo ratings yet
- KonstipasivgfvhDocument16 pagesKonstipasivgfvhrharaNo ratings yet
- PL - Grosir - 12-08-2023Document29 pagesPL - Grosir - 12-08-2023Fanteri Aji DharmaNo ratings yet
- Improving The Concept of Medication Vending MachineDocument4 pagesImproving The Concept of Medication Vending MachineHaritNo ratings yet
- GepantsDocument14 pagesGepantsmatheus galvãoNo ratings yet
- Blood Tube Additives and TestsDocument3 pagesBlood Tube Additives and TestsDanluidQMalintadNo ratings yet
- Bilastine AntihistamineDocument9 pagesBilastine AntihistamineteddypolNo ratings yet
- Scientific and Ethical Issues in The Use of Placebo Controls in Clinical TrialsDocument20 pagesScientific and Ethical Issues in The Use of Placebo Controls in Clinical TrialsNicusor OnaciuNo ratings yet
- Price List PT BMP: Nama Obat Satuan Stok Harga Nett++ (RP)Document98 pagesPrice List PT BMP: Nama Obat Satuan Stok Harga Nett++ (RP)apriantiNo ratings yet
- ANEXA1 Lista Medicamente Decontate de CASDocument39 pagesANEXA1 Lista Medicamente Decontate de CASVas RetNo ratings yet
- Zopiclone Report Sep09Document21 pagesZopiclone Report Sep09Iona KalosNo ratings yet
- The most likely diagnosis is: 1. Cardiac amyloidosis 2. Hypertrophic cardiomyopathy 3. Dilated cardiomyopathy 4. Restrictive cardiomyopathyDocument289 pagesThe most likely diagnosis is: 1. Cardiac amyloidosis 2. Hypertrophic cardiomyopathy 3. Dilated cardiomyopathy 4. Restrictive cardiomyopathyadnan shwNo ratings yet
- 2007 08/31 DR Gokhale DischargeDocument4 pages2007 08/31 DR Gokhale Dischargeapi-26176155No ratings yet
- AyuCaRe Vol 1 Issue 1Document52 pagesAyuCaRe Vol 1 Issue 1Priyanka SharmaNo ratings yet
- Rajini Final Merged ThesisDocument89 pagesRajini Final Merged ThesispadminiNo ratings yet
- Drug Study BAIAEDocument5 pagesDrug Study BAIAEDAOman09No ratings yet
- Nursing On ProcessDocument6 pagesNursing On Processsabecaw762brownalNo ratings yet
- Cannabis May Have Medical Benefits Says University MagazineDocument4 pagesCannabis May Have Medical Benefits Says University MagazineNeil MontgomeryNo ratings yet
- EvaluatePharma World Preview 2020 - 0Document32 pagesEvaluatePharma World Preview 2020 - 0solej100% (1)
- Pharmacology OpioidanalgesicsDocument6 pagesPharmacology OpioidanalgesicsJe SantosNo ratings yet
- Magnesium Sulfate Dosage Indications ContraindicationsDocument2 pagesMagnesium Sulfate Dosage Indications ContraindicationsEmma G. Guillermo RMNo ratings yet
- SERENACE Injection: What Is in This LeafletDocument5 pagesSERENACE Injection: What Is in This LeafletningrumNo ratings yet
- HYPERTHYROIDISMDocument48 pagesHYPERTHYROIDISMManoj Ghimire100% (1)
- Dwnload full Saunders Nursing Drug Handbook Pdf pdfDocument73 pagesDwnload full Saunders Nursing Drug Handbook Pdf pdfashley.duffy742100% (13)
- Anesthesiology Core Review 1st EditionDocument588 pagesAnesthesiology Core Review 1st EditionVeronica ChavezNo ratings yet
- All Category Name DescDocument286 pagesAll Category Name DescWeb SpringNo ratings yet
- Emergency Pediatric AidsDocument29 pagesEmergency Pediatric AidsRana SalemNo ratings yet
- Publications-2012-2017 Department of Pharmacognosy Faculty of Pharmacy and Pharmaceutical Sciences University of Karachi 2017 - 27 Research PapersDocument20 pagesPublications-2012-2017 Department of Pharmacognosy Faculty of Pharmacy and Pharmaceutical Sciences University of Karachi 2017 - 27 Research PapersHira Enayatullah KhanNo ratings yet
- EPAR FludarabineDocument8 pagesEPAR FludarabinerajugNo ratings yet
- GeraniolDocument8 pagesGeraniolclaudiagonz2128No ratings yet