Professional Documents
Culture Documents
Successful Use of Haemodialysis To Treat Phenobarbital Overdose
Uploaded by
Agustina ZairidaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Successful Use of Haemodialysis To Treat Phenobarbital Overdose
Uploaded by
Agustina ZairidaCopyright:
Available Formats
Novel treatment (new drug/intervention; established drug/procedure in new situation)
CASE REPORT
Successful use of haemodialysis to treat
phenobarbital overdose
Kimberley Hoyland,1 Michael Hoy,1 Richard Austin,1 Martyn Wildman2
1
Department of Intensive Care, SUMMARY The use of barbiturates in the West has rapidly
Lister Hospital, Stevenage, A 50-year-old woman presented with coma caused by a declined with the advent of benzodiazepines and
Hertfordshire, UK
2
Department of Intensive Care phenobarbital overdose, requiring intubation and newer antiepileptic drugs. Barbiturate toxicity
and Anaesthetics, Lister admission to critical care. She was an international results more readily as a result of both the general-
Hospital, Stevenage, visitor and had been prescribed the drug for night- ity of barbiturate binding and the direct opening of
Hertfordshire, UK sedation. Phenobarbital is a long-acting barbiturate, the chloride channel by comparison with benzodia-
which in an overdose can cause central nervous system zepines. The key clinical feature distinguishing the
Correspondence to
Dr Kimberley Hoyland, depression, respiratory failure and haemodynamic patient with benzodiazepine intoxication from one
kimberley.hoyland@nhs.net instability; these patients can remain obtunded for many with a barbiturate overdose is the ability to quickly
days. After initial supportive therapy, she was dialysed to antagonise the effect with flumazenil, which com-
help in the elimination of the drug. Haemodialysis petes with the benzodiazepine at the GABA-A
resulted in a markedly reduced plasma level of receptor. These characteristics of benzodiazepines
phenobarbital, which decreased the length of intubation have contributed to their clinical popularity with
and stay in the critical care unit and aided full recovery. the correspondent decline in favour of barbiturates.
However, given their continued use elsewhere in
the World, the treatment of barbiturate toxicity
remains an important topic of interest and one
which has had relatively little attention paid to it of
BACKGROUND
late.
Barbiturates bind to the β-subunit of the
γ-aminobutyric acid A (GABA-A) receptor, increas-
ing the duration of the opening of the chloride ion CASE PRESENTATION
channel and potentiating the neuroinhibitory effect A 50-year-old woman visiting the UK from Eastern
of GABA. The channel kinetics of the GABA-A Europe was discovered unconscious after a sus-
receptor have been explained by a three-state pected overdose of 12.5 g of phenobarbital, taken
model with chloride channel open-time constants at an unknown point within the preceding 24 h.
of 1, 4 and 11 ms—opening more frequently and On presentation to the emergency department, the
moving from a lower to a greater state as GABA patient had a Glasgow Coma Scale (GCS) of 3,
concentration increases.1 Barbiturates promote the although she remained haemodynamically stable.
opening of GABA-A receptors in their longer lived The initial phenobarbital level was 143 mg/L
state and at a higher frequency. It has been shown (therapeutic range for treatment of epilepsy
that in higher doses, barbiturates directly stimulate 10–30 mg/L)—the other toxicology screen was
GABA-A receptors outside of the presence of negative. The patient was intubated, ventilated and
GABA itself.2 The net effect of barbiturates is one transferred to intensive care. The patient had ini-
of neuroinhibition, and as such they have evolved tially been prescribed phenobarbital to help with
multiple clinical applications, including as anxio- insomnia by her regular doctor in Romania. In
lytic, sedative, antiepileptic and anaesthetic agents. light of the patient’s long-term barbiturate usage
Phenobarbital is a long-acting barbiturate, with a and likely tolerance with potentially enhanced
narrow therapeutic index and a wide interindivi- metabolism and clearance, we initially opted for
dual variability in the rate of metabolism. This supportive management.
narrow therapeutic range 10–30 mg/L means that
levels required for relieving anxiety and producing
sedative effects are very close to those associated TREATMENT
with toxicity. A phenobarbital overdose can cause Following 96 h of supportive care, the patient
central nervous system depression, along with remained on GCS 3, and despite the incremental
respiratory failure and haemodynamic instability.3 reductions in serial levels, her phenobarbital level
Furthermore, given the reported half life of 5 days, remained at 115 mg/L. Given the lack of progress
these patients can remain obtunded for some time.4 in her neurological status, we opted to trial venove-
Historical treatment of a barbiturate overdose is nous haemodialysis (dialysate flow 500 mL/min;
based on supportive care, activated charcoal and pump speed 200 mL/min; T 35.5) for a period of
To cite: Hoyland K, Hoy M,
Austin R, et al. BMJ Case
urinary alkalinisation along with the application of 2 h on two separate occasions, in an attempt to
Rep Published online: extracorporeal treatments such as charcoal haemo- enhance clearance of the drug. The patient’s
[please include Day Month perfusion or haemodialysis. There is, however, a phenobarbital levels reduced from 115 to 84 mg/L
Year] doi:10.1136/bcr-2013- notable paucity of recent evidence supporting one following the first dialysis and from 78 to 55 mg/L
010011 approach over another. following the second cycle (figure 1).
Hoyland K, et al. BMJ Case Rep 2013. doi:10.1136/bcr-2013-010011 1
Novel treatment (new drug/intervention; established drug/procedure in new situation)
of phenobarbital, with volumes of distribution reported at
0.54–0.9 L/kg.3 4
Haemodialysis has been shown in this case, as well as others
reported in the literature, to be an effective treatment in high-
dose phenobarbital overdose. Plasma clearance of phenobarbital
by high-flux haemodialysis has been shown to be 30 times that
of hepatic clearance, and 10 times greater than the rate achieved
with activated charcoal.8 This, combined with the fact that
haemodialysis is less expensive and more widely available than
haemoperfusion, makes it an appealing choice for this group of
patients.9
Figure 1 Graph demonstrating the elimination of phenobarbital over We would support the use of haemodialysis to diminish the
time. Haemodialysis performed at points indicated by arrows. prolonged effects of phenobarbital and reduce the length of stay
in intensive care units with all the attendant risks of prolonged
ventilation such as ventilator-acquired pneumonia together with
the increased costs associated with level three critical care.
OUTCOME AND FOLLOW-UP
In summary, this case presents a female patient with a pheno-
At a phenobarbital level of approximately 55 mg/L, the patient
barbital overdose resulting in coma that was treated successfully
spontaneously opened her eyes and was appropriate for extuba-
with two sessions of haemodialysis. We have presented a review
tion within hours. The patient was fit for discharge from critical
of similar cases of successful treatment of phenobarbital over-
care within 24 h and went on to make a full recovery. A full psy-
dose with haemodialysis. We conclude that haemodialysis may
chiatric assessment was made before discharge from hospital.
have a place in reducing the adverse effects of phenobarbital
overdose. However, further investigation into the use of haemo-
dialysis as a treatment for phenobarbital overdose is necessary
DISCUSSION to determine a protocol. What dialysis regime is most effective?
The reported lethal dose of phenobarbital is in the range of Should haemodialysis be used in all cases of phenobarbital over-
6–10 g,5 with concentrations of 80 mg/L reported as fatal.6 Our dose, or should there be a specific phenobarbital level to
patient ingested a higher dose than that reported as fatal, and dialyse? Further cases of phenobarbital overdose treated with
was haemodynamically stable, potentially due to the long-term haemodialysis are required in order to answer these questions.
tolerance of the drug. Haemodialysis produced a rapid reduc-
tion in the phenobarbital levels and accelerated the clinical
recovery of this patient, and has also shown similar success in Learning points
other cases reported in the literature.
Balme et al7 presented a case in 1962, whereby a patient pre-
senting with a barbitone level of 60 mg/100 mL was treated ▸ Phenobarbital remains an important drug that is open to
with haemodialysis for 8 h and responded similarly, with a abuse and overdose with significant potential for morbidity
return of reflexes and appropriate responses sufficient to be and mortality.
extubated. ▸ Haemodialysis is widely available in the critical care setting
Quan and Winter8 reported a case of a patient with a pheno- and increases the elimination of phenobarbital.
barbital level of 163 mg/L on presentation. Similar to our case, ▸ Haemodialysis can significantly reduce the length of
the patient showed no improvement for 3 days, and thus was intubation in patients with overdose.
treated with high-flux haemodialysis on two separate days for ▸ Haemodialysis can significantly reduce the length of critical
2–2.5 h each time, showing remarkable improvement.8 care stay in patients with overdose.
Furthermore, Palmer3 reported another case of a comatose
patient presenting following a phenobarbital overdose. The
patient had a phenobarbital level of 143 mg/mL and failed to
Contributors KH and MH gave the idea and concept for the writing of the
respond to repeated doses of activated charcoal.3 However, manuscript, and were also involved in the writing of the manuscript. RA and MW
high-flux dialysis for 4 h resulted in dramatic improvement with participated in the editing of the manuscript.
the patient responding appropriately by the end of the dialysis Competing interests None.
session.3
Patient consent Obtained.
Although cases of phenobarbital overdose treated successfully
Provenance and peer review Not commissioned; externally peer reviewed.
by haemodialysis have been reported in the literature, there
appears to be a lack of consensus regarding whether haemodi-
alysis or haemoperfusion is superior in treating barbiturate over-
dose. Haemoperfusion was originally deemed to be superior REFERENCES
due to its effectiveness in removing highly protein bound drugs, 1 Harrison N, Mendelson WB, De Wit H. Barbiturates. Neuropsychopharmacology
2000. http://www.acnp.org/g4/gn401000173/ch169.html (accessed 18 Jan 2012).
such as phenobarbital which displays 40–60% protein binding.3
2 Löscher W, Rogawski MA. How theories evolved concerning the mechanism of action
However, the premise that haemoperfusion is superior was of barbiturates. Epilepsia 2012;53:12–25.
based on the comparison with low-efficiency dialysers with low 3 Palmer BF. Effectiveness of hemodialysis in the extracorporeal therapy of
blood flow rates.3 The advent of more superior haemodialysis phenobarbital overdose. Am J Kidney Dis 2000;36:640–3.
machines calls for a review of the use of haemodialysis as a 4 Mohammed Ebid AHI, Abdel-Rahman HM. Pharmacokinetics of phenobarbital during
certain enhanced elimination modalities to evaluate their clinical efficacy in
treatment modality for phenobarbital overdose. Haemodialysis management of drug overdose. Ther Drug Monit 2001;23:209–16.
is most effective for drugs with a low molecular weight, high 5 Lindberg MC, Cunningham A, Lindberg NH. Acute phenobarbital intoxication. South
water solubility and small volume of distribution, which is true Med J 1992;85:803–7.
2 Hoyland K, et al. BMJ Case Rep 2013. doi:10.1136/bcr-2013-010011
Novel treatment (new drug/intervention; established drug/procedure in new situation)
6 Berman LB, Jehgers H, Schreiner GE, et al. Hemodialysis, an effective therapy for 8 Quan DJ, Winter ME. Extracorporeal removal of phenobarbital by high-flux
acute barbiturate poisoning. JAMA 1956;161:820–7. hemodialysis. J Appl Ther Res 1997;2:75–9.
7 Balme RH, Lloyd-Thomas HG, Shead GV. Severe barbitone poisoning treated by 9 Zawada ET, Nappi J, Done G, et al. Advances in the hemodialysis management of
haemodialysis. Br Med J 1962;1:231–2. phenobarbital overdose. South Med J 1983;76:6–8.
Copyright 2013 BMJ Publishing Group. All rights reserved. For permission to reuse any of this content visit
http://group.bmj.com/group/rights-licensing/permissions.
BMJ Case Report Fellows may re-use this article for personal use and teaching without any further permission.
Become a Fellow of BMJ Case Reports today and you can:
▸ Submit as many cases as you like
▸ Enjoy fast sympathetic peer review and rapid publication of accepted articles
▸ Access all the published articles
▸ Re-use any of the published material for personal use and teaching without further permission
For information on Institutional Fellowships contact consortiasales@bmjgroup.com
Visit casereports.bmj.com for more articles like this and to become a Fellow
Hoyland K, et al. BMJ Case Rep 2013. doi:10.1136/bcr-2013-010011 3
You might also like
- Ch013 001-007 HypertensionDocument7 pagesCh013 001-007 Hypertensiond_94100% (5)
- Baclofen and Gamma-Hydroxybutyrate WithdrawalDocument4 pagesBaclofen and Gamma-Hydroxybutyrate WithdrawalImustaforgotNo ratings yet
- Barbiturates Toxicity GuideDocument12 pagesBarbiturates Toxicity GuideDayagNo ratings yet
- Iadt02i6p480 PDFDocument3 pagesIadt02i6p480 PDFVandanaNo ratings yet
- Drugs That Act On The CNSDocument27 pagesDrugs That Act On The CNSnur rachmad afandiNo ratings yet
- PR 2021 Hindawi ID-5559981 CaseReports-in-Medicine 1-4Document4 pagesPR 2021 Hindawi ID-5559981 CaseReports-in-Medicine 1-4aditya galih wicaksonoNo ratings yet
- CNS Depressants: Barbiturates, Benzodiazepines, Chloral HydrateDocument11 pagesCNS Depressants: Barbiturates, Benzodiazepines, Chloral Hydrateاسامه عمر عثمانNo ratings yet
- Selected Topics: Toxicology: Severe Carisoprodol Withdrawal After A 14-Year Addiction and Acute OverdoseDocument4 pagesSelected Topics: Toxicology: Severe Carisoprodol Withdrawal After A 14-Year Addiction and Acute OverdoseAhmad SyaukatNo ratings yet
- Sedative-Hypnotic Drugs: Department of Pharmacology Zhang YanmeiDocument30 pagesSedative-Hypnotic Drugs: Department of Pharmacology Zhang YanmeiKAVITA HOODANo ratings yet
- Cannabinoid Hyperemesis Syndrome: Marijuana Is Both Antiemetic and ProemeticDocument6 pagesCannabinoid Hyperemesis Syndrome: Marijuana Is Both Antiemetic and ProemeticSilesiaNo ratings yet
- Anticonvulsivantes e Antipsicóticos No Tratamento Do Transtorno BipolarDocument7 pagesAnticonvulsivantes e Antipsicóticos No Tratamento Do Transtorno BipolarAzerax PLAYNo ratings yet
- Sedative-Hypnotic DrugsDocument30 pagesSedative-Hypnotic DrugsdrfatimarizNo ratings yet
- Acute Phenobarbital Administration Induces HyperalDocument9 pagesAcute Phenobarbital Administration Induces HyperalAldaNo ratings yet
- 29880020: Antiepileptic Drugs in Critically Ill PatientsDocument12 pages29880020: Antiepileptic Drugs in Critically Ill PatientsEward Rod SalNo ratings yet
- BARBITURATESDocument21 pagesBARBITURATESHamza DossaNo ratings yet
- A Case Report On Faropenem Induced Focal SeizuresDocument3 pagesA Case Report On Faropenem Induced Focal SeizuresInternational Journal of Innovative Science and Research Technology100% (1)
- Gabapentin Oi DesDocument11 pagesGabapentin Oi DesLuis Felipe Arteaga ArredondoNo ratings yet
- Psychoactive DrugsDocument24 pagesPsychoactive DrugsIshaani GargNo ratings yet
- IV Anesthesia - Barbiturates: ThiopentalDocument9 pagesIV Anesthesia - Barbiturates: ThiopentalClara Amanda SchramNo ratings yet
- Barbiturate Coma 2Document5 pagesBarbiturate Coma 2Carlos Perez CastroNo ratings yet
- Pini Lupo2001 Article Anti EpilepticDrugsInThePrevenDocument7 pagesPini Lupo2001 Article Anti EpilepticDrugsInThePrevenPutu Gede SudiraNo ratings yet
- Oct 12 El Intoxicado Grave Skolnik 2020Document16 pagesOct 12 El Intoxicado Grave Skolnik 2020lfc2086No ratings yet
- Combined Alternative Meds MemoDocument62 pagesCombined Alternative Meds MemoFDRHPO North Country EMS Program AgencyNo ratings yet
- Jurnal Presentasi 22 SeptDocument21 pagesJurnal Presentasi 22 Septliashuban29No ratings yet
- Hosp Ops II Week 2 Questions 1Document3 pagesHosp Ops II Week 2 Questions 1api-650133203No ratings yet
- Keta y Benzo en OhDocument6 pagesKeta y Benzo en OhVictor CarrenoNo ratings yet
- Dapsone-Induced Methemoglobinemia: Case ReportDocument4 pagesDapsone-Induced Methemoglobinemia: Case ReportHala HaylaNo ratings yet
- Drug StudyDocument7 pagesDrug StudyRalph Elvin MacanlalayNo ratings yet
- GBL Lukas 2006 ZeitungDocument3 pagesGBL Lukas 2006 ZeitungAnonymous LLtBH6AwiNo ratings yet
- Activity and Onset of Action of Reboxetine and Effect of Combination With Sertraline in An Animal Model of DepressionDocument10 pagesActivity and Onset of Action of Reboxetine and Effect of Combination With Sertraline in An Animal Model of DepressionIsaac Saucedo FloresNo ratings yet
- Effect of benfotiamine and pregabalin on carpal tunnel syndromeDocument6 pagesEffect of benfotiamine and pregabalin on carpal tunnel syndromeHomer SimpsonNo ratings yet
- Atípica AntipsychoticsDocument10 pagesAtípica AntipsychoticsRoberto Alexis Molina CampuzanoNo ratings yet
- Bipolar Disorders and Carbamazepine PharmacokinetiDocument6 pagesBipolar Disorders and Carbamazepine PharmacokinetiluthfiahNo ratings yet
- Jurnal 8Document7 pagesJurnal 8Fatma BaagilNo ratings yet
- Diclofenac - Martindale 36edDocument4 pagesDiclofenac - Martindale 36edSvetlana Maiochi LodovicoNo ratings yet
- Pharmacology of AntiepilepticDocument36 pagesPharmacology of AntiepilepticManWol JangNo ratings yet
- What Is New in Management of Pediatric Tuberculosis ?Document8 pagesWhat Is New in Management of Pediatric Tuberculosis ?VijayyyNo ratings yet
- Bipolar Disorders and Carbamazepine PharmacokinetiDocument5 pagesBipolar Disorders and Carbamazepine PharmacokinetiAgr YuroNo ratings yet
- Anticonvulsant Part2Document35 pagesAnticonvulsant Part2Rameez ShamounNo ratings yet
- Standards of Laboratory Practice: Antiepileptic Drug MonitoringDocument11 pagesStandards of Laboratory Practice: Antiepileptic Drug MonitoringDiegoAndrésYiZapataNo ratings yet
- RECENT ADVANCES IN UNDERSTANDING AND MANAGEMENT OF CANNABIS, BENZODIAZEPINE AND TOBACCO DEPENDENCEDocument54 pagesRECENT ADVANCES IN UNDERSTANDING AND MANAGEMENT OF CANNABIS, BENZODIAZEPINE AND TOBACCO DEPENDENCEstpeter_agraNo ratings yet
- Pyrantel EmbonateDocument1 pagePyrantel EmbonateLaily IlmiNo ratings yet
- Cannabinoid Replacement TherapyDocument4 pagesCannabinoid Replacement TherapyastrogliaNo ratings yet
- Pregabalin Abuse of Benzodiazepine and Alcohol Addicted PatientDocument2 pagesPregabalin Abuse of Benzodiazepine and Alcohol Addicted PatientSandro AlcobaçaNo ratings yet
- Hood Hulse 2014 FlumazenilDocument10 pagesHood Hulse 2014 FlumazenilDavid KevosNo ratings yet
- Pharmacology of CNS: Prajogo Wibowo Faculty of Medicine Hang Tuah UniversityDocument37 pagesPharmacology of CNS: Prajogo Wibowo Faculty of Medicine Hang Tuah UniversityIda Bagus Putu SwabawaNo ratings yet
- Bupropion 1Document22 pagesBupropion 1Robert MovileanuNo ratings yet
- Asma Felino TratamientoDocument7 pagesAsma Felino TratamientoRenzo Alessandro Pacherres NietoNo ratings yet
- Barbiturate Poisoning: Diagnosis, Treatment and ManagementDocument17 pagesBarbiturate Poisoning: Diagnosis, Treatment and ManagementRaymond ManjengwaNo ratings yet
- CNS Drugs Acting on GABA and Sodium ChannelsDocument27 pagesCNS Drugs Acting on GABA and Sodium Channelsashokvishnoi29pNo ratings yet
- A. BarbituratesDocument62 pagesA. BarbituratesMelanie LimNo ratings yet
- DRUG ACTIONDocument3 pagesDRUG ACTIONGwyn RosalesNo ratings yet
- Phenytoin-Diazepam Interaction: Objective Case SummaryDocument5 pagesPhenytoin-Diazepam Interaction: Objective Case SummaryNavisa HaifaNo ratings yet
- Kologi 1Document6 pagesKologi 1Ida BagusGede Dwi AmbaraNo ratings yet
- Discinesia e SNM Litio e Antipsicotico InicioDocument4 pagesDiscinesia e SNM Litio e Antipsicotico InicioBárbara LimaNo ratings yet
- Phenytoin Auto InductionDocument2 pagesPhenytoin Auto InductionNur MukminNo ratings yet
- Cebergoline Induced Psychotic Exacerbation in Schizophrenic PatientsDocument3 pagesCebergoline Induced Psychotic Exacerbation in Schizophrenic PatientsMaria Del GuercioNo ratings yet
- Long-Term Stabilisation of Myeloma With Curcumin: Abbas Zaidi, Maggie Lai, Jamie CavenaghDocument3 pagesLong-Term Stabilisation of Myeloma With Curcumin: Abbas Zaidi, Maggie Lai, Jamie CavenaghNisa TaslimNo ratings yet
- 12 2014 JHOP - SympManDocument4 pages12 2014 JHOP - SympManAhmed AliNo ratings yet
- NIH Public Access: Effect of Sedation On Pain PerceptionDocument21 pagesNIH Public Access: Effect of Sedation On Pain PerceptionAgustina ZairidaNo ratings yet
- Thermal Behaviour of Procaine and Benzocaine Part II: Compatibility Study With Some Pharmaceutical Excipients Used in Solid Dosage FormsDocument10 pagesThermal Behaviour of Procaine and Benzocaine Part II: Compatibility Study With Some Pharmaceutical Excipients Used in Solid Dosage FormsAgustina ZairidaNo ratings yet
- Arp2012 546409Document11 pagesArp2012 546409Agustina ZairidaNo ratings yet
- Thermal Behaviour of Procaine and Benzocaine Part II: Compatibility Study With Some Pharmaceutical Excipients Used in Solid Dosage FormsDocument10 pagesThermal Behaviour of Procaine and Benzocaine Part II: Compatibility Study With Some Pharmaceutical Excipients Used in Solid Dosage FormsAgustina ZairidaNo ratings yet
- National Use of Prescription Medications For Insomnia: NHANES 1999-2010Document10 pagesNational Use of Prescription Medications For Insomnia: NHANES 1999-2010Agustina ZairidaNo ratings yet
- Diagnosis and Management of Headache in Adults PDFDocument88 pagesDiagnosis and Management of Headache in Adults PDFFungky AnthonyNo ratings yet
- WJCC 3 20Document15 pagesWJCC 3 20api-394361077No ratings yet
- Dic 212257Document10 pagesDic 212257Agustina ZairidaNo ratings yet
- Arp2012 546409Document11 pagesArp2012 546409Agustina ZairidaNo ratings yet
- 280 Patients Refractory Chronic Pain - Neural TherapyDocument9 pages280 Patients Refractory Chronic Pain - Neural TherapyAngel MalzoneNo ratings yet
- Mycobacterium Leprae Alters Classical Activation of Human Monocytes in VitroDocument5 pagesMycobacterium Leprae Alters Classical Activation of Human Monocytes in VitroAgustina ZairidaNo ratings yet
- Bacillus Anthracis B. CereusDocument8 pagesBacillus Anthracis B. CereusAgustina ZairidaNo ratings yet
- Bacillus Anthracis B. CereusDocument8 pagesBacillus Anthracis B. CereusAgustina ZairidaNo ratings yet
- Approach To Short Stature: Guest Editor: Bhim S. PandhiDocument9 pagesApproach To Short Stature: Guest Editor: Bhim S. PandhiAldy WaveNo ratings yet
- Lila U GirlsDocument1 pageLila U GirlsNay Ebeye NubaseNo ratings yet
- 5 Adjective Clauses TranslateDocument12 pages5 Adjective Clauses TranslateIndah95No ratings yet
- NEUROPATHY DM 2Document14 pagesNEUROPATHY DM 2Agustina ZairidaNo ratings yet
- Ahwan-Bank Air Susu IbuDocument13 pagesAhwan-Bank Air Susu IbuAgustina ZairidaNo ratings yet
- Ahwan-Bank Air Susu IbuDocument13 pagesAhwan-Bank Air Susu IbuAgustina ZairidaNo ratings yet
- I Will Always Love YouDocument1 pageI Will Always Love YouPrila POenya KaMoeNo ratings yet
- Sex, Sleep or Scrabble? by DR Phil Hammond ExtractDocument36 pagesSex, Sleep or Scrabble? by DR Phil Hammond ExtractBlack & White PublishingNo ratings yet
- Fallacy of The Fundal HeightDocument3 pagesFallacy of The Fundal Heightمحمد النويجمNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument8 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- WHO Assessment RiskDocument90 pagesWHO Assessment RiskJuliana VelosoNo ratings yet
- Does Premenstrualsyndrome Induces Change in The ANSDocument1 pageDoes Premenstrualsyndrome Induces Change in The ANSSailaja NandennagariNo ratings yet
- Afinidad, Jiezl A: Davao Doctors College Nursing ProgramDocument4 pagesAfinidad, Jiezl A: Davao Doctors College Nursing ProgramJiezl Abellano AfinidadNo ratings yet
- Iodine SDSDocument8 pagesIodine SDSKike PadillaNo ratings yet
- Acupuncture For Low Back Pain TraditionalDocument7 pagesAcupuncture For Low Back Pain Traditionalobecalp812100% (1)
- #44 Ravanera, Adiel A. CED 11-201A MissionDocument4 pages#44 Ravanera, Adiel A. CED 11-201A MissionAdielNo ratings yet
- TYPHOID FEVER and HEPATITIS ADocument25 pagesTYPHOID FEVER and HEPATITIS AMaelleNo ratings yet
- Syllabus Foodservice-2Document15 pagesSyllabus Foodservice-2Arienda RKNo ratings yet
- PLT College Course Syllabus for Dispensing and Medication CounselingDocument5 pagesPLT College Course Syllabus for Dispensing and Medication Counseling;'SiLeNt';100% (1)
- Pure Performance Base Oil 70N, 80N - SDSDocument7 pagesPure Performance Base Oil 70N, 80N - SDSAvyan KelanNo ratings yet
- Understanding Transient Tachypnea of the Newborn (TTNDocument3 pagesUnderstanding Transient Tachypnea of the Newborn (TTNReviana Citra NataliaNo ratings yet
- A Position Paper On The Covid 19 VaccineDocument2 pagesA Position Paper On The Covid 19 VaccineLyza MateoNo ratings yet
- 3 - CHAT PilotDocument12 pages3 - CHAT PilotAda NwamemeNo ratings yet
- Assessment and Interpretation of Vitamin and Trace.34Document9 pagesAssessment and Interpretation of Vitamin and Trace.34ntnquynhproNo ratings yet
- Serum VEGF Levels in The Early Diagnosis and Severity Assessment of Non-Small Cell Lung CancerDocument10 pagesSerum VEGF Levels in The Early Diagnosis and Severity Assessment of Non-Small Cell Lung CanceryasserNo ratings yet
- Urological EmergenciesDocument35 pagesUrological EmergenciesAkhmad MustafaNo ratings yet
- Worksheet - Public Health Nutrition - Revision QuestionsDocument5 pagesWorksheet - Public Health Nutrition - Revision Questionsstar “Hjaljimmer” platinumNo ratings yet
- To Err Is Human A Case Study of Error Prevention in Process IsolationsDocument6 pagesTo Err Is Human A Case Study of Error Prevention in Process Isolationsairbuk doeingNo ratings yet
- Animal Testing Essential To Medical ProgressDocument7 pagesAnimal Testing Essential To Medical ProgressLayalNo ratings yet
- Assistive Technologies For Visually Impaired MarketDocument4 pagesAssistive Technologies For Visually Impaired Marketryan2021cmrNo ratings yet
- Commercial Index - SV - CarlislecDocument308 pagesCommercial Index - SV - CarlislecRobert RangstanNo ratings yet
- Fundamentals Exam 3Document2 pagesFundamentals Exam 3JackieNo ratings yet
- 7 Main Questions About Tummy TuckDocument3 pages7 Main Questions About Tummy TuckTandon ClinicNo ratings yet
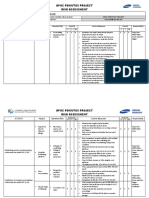
- APOC RISK ASSESSMENT FORMAT - SESA-BFIM-RA-INS-002.Rev02Document7 pagesAPOC RISK ASSESSMENT FORMAT - SESA-BFIM-RA-INS-002.Rev02Abdul WasayNo ratings yet
- Updated PS7 Speciality HospitalsDocument116 pagesUpdated PS7 Speciality HospitalsAyaanNo ratings yet
- Student Exploration: Disease Spread: Vocabulary: Disease, Epidemic, Infect, Infectious Disease, PathogenDocument5 pagesStudent Exploration: Disease Spread: Vocabulary: Disease, Epidemic, Infect, Infectious Disease, PathogenVijay Shankar PrasadNo ratings yet
- Levels of Evidence Flow Chart Rev May 2019Document3 pagesLevels of Evidence Flow Chart Rev May 2019Karl RobleNo ratings yet