Professional Documents
Culture Documents
AJR Clinical PET MRI 2018 Update
Uploaded by
alfred benedict bayanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AJR Clinical PET MRI 2018 Update
Uploaded by
alfred benedict bayanCopyright:
Available Formats
N u c l e a r M e d i c i n e a n d M o l e c u l a r I m a g i n g • R ev i ew
Broski et al.
Update on Clinical PET/MRI
Nuclear Medicine and Molecular Imaging
Review
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
FOCUS ON:
Clinical PET/MRI: 2018 Update
Stephen M. Broski1 OBJECTIVE. The purpose of this article is to provide an update on clinical PET/MRI, in-
Ajit H. Goenka1 cluding current and developing clinical indications and technical developments.
Bradley J. Kemp1 CONCLUSION. PET/MRI is evolving rapidly, transitioning from a predominant re-
Geoffrey B. Johnson1,2 search focus to exciting clinical practice. Key technical obstacles have been overcome, and
further technical advances promise to herald significant advancements in image quality. Fur-
Broski SM, Goenka AH, Kemp BJ, Johnson GB ther optimization of protocols to address challenges posed by this hybrid modality will ensure
the long-term success of PET/MRI.
ET/MRI has steadily transi- new opportunities. Recent developments have
P tioned from a predominant re-
search focus to exciting clinical
practice at a number of medical
offered an exciting glimpse into the potential
of simultaneous PET/MRI to characterize tu-
mor heterogeneity, perform complex motion
centers [1]. Here, we review recent changes correction, leverage advanced data mining
in the field of PET/MRI, including indica- and bioinformatics, and integrate biomarkers
tions and protocols where PET/MRI appears to better evaluate disease processes, cancer
to have a clear foothold in clinical practice. evolution, and therapy response [3].
This article will focus primarily on clinical
PET/MRI and adult diseases. We review Instrumentation Update
some key recent technical advances and clin- The core basic design of clinical and
ical data that support these areas of growth. commercially available PET/MRI systems
Finally, we touch on indications that show has remained unchanged for several years.
potential for success in the very near future. Currently, there are two vendors producing
PET/MRI has undergone rapid evolution PET/MRI systems: Siemens Healthcare and
in recent years. An article in 2016 by Spick GE Healthcare. Both the Siemens Healthcare
Keywords: cancer, inflammation, PET/MRI and colleagues [2] combining data from mul- Biograph mMR [4] and the GE Healthcare
tiple studies and over 2300 patients showed Signa [5] are fully integrated PET/MRI sys-
doi.org/10.2214/AJR.18.20001 the equivalency of 18F-FDG PET/CT and tems in which solid-state PET detectors re-
Received April 12, 2018; accepted after revision April 30, PET/MRI in oncologic evaluation. A prior side within a 3-T MRI gantry, allowing si-
2018. fixation on finding a single best application to multaneous PET and MRI acquisition. The
justify investing in PET/MRI has given way important characteristics of both PET/MRI
Supported by research funding from GE Healthcare to to a multitude of clinically useful applications. systems are listed in Table 1.
B. J. Kemp and G. B. Johnson.
The initial enormous hurdle of developing a
1
Department of Radiology, Mayo Clinic, Charlton 1, 200 PET detector system that could function in an Attenuation Correction
First St SW, Rochester, MN 55905. Address correspon- MRI magnetic field was overcome with ava- Once a major challenge to the field, MRI-
dence to G. B. Johnson (johnson.geoffrey@mayo.edu). lanche photodiode solid-state PET detectors. based attenuation correction is no longer
2
More recently, faster silicon photomultiplier viewed as a significant impediment to clini-
Department of Immunology, Mayo Clinic, Rochester, MN.
detectors have been introduced, advancing cal adoption of PET/MRI. However, attenu-
Supplemental Data PET performance to a new state of the art. The ation correction must be taken into account
Available online at www.ajronline.org. field is also addressing and overcoming core when reading PET/MRI in a similar manner
issues with MRI-based attenuation correction. to the many other factors that are known to
AJR 2018; 211:295–313 Long scan times required for body PET/MRI affect standardized uptake value (SUV) in
0361–803X/18/2112–295
result in patient dissatisfaction; however, PET data. A detailed review of the numerous
more-rapid and robust MRI sequences prom- MRI-based attenuation correction techniques
© American Roentgen Ray Society ise to improve the patient experience and open is beyond the scope of this article (see [6] for
AJR:211, August 2018 295
Broski et al.
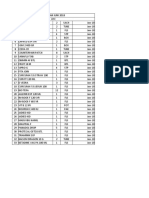
TABLE 1: Design and Performance Characteristics of the Biograph mMR reconstruction of activity and attenuation algo-
(Siemens Healthcare) and Signa (GE Healthcare) PET/MRI Systems rithm [18]. By incorporating time-of-flight in-
Characteristic Biograph mMR Signa
formation, the activity and attenuation distribu-
tions can be determined up to a constant [19].
MRI component Deep convolutional neural networks have been
Magnet 3-T superconductor 3-T superconductor developed for noise reduction and segmenta-
tion of medical images [20, 21]. A deep convo-
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
Bore diameter (cm) 60 60
lutional neural network has been developed to
Gradient coil
overcome some of the limitations of maximum
Amplitude (mT/m) 45 44 likelihood reconstruction of activity and atten-
Slew rate (T/m/s) 200 200 uation [22], and a deep convolutional neural
Transaxial FOV (cm) 50 50 network has been trained to transform Dixon
MRI and zero-TE sequences of the pelvis into
Axial FOV (cm) 50 50
a quantitatively accurate attenuation map [23].
PET component
Crystal material Lutetium oxyorthosilicate Lutetium-based scintillator Motion Correction
Crystal size (mm3) 4.0 × 4.0 × 20 4.0 × 5.3 × 25 Diaphragmatic motion correction on both
body MRI and PET are routine practice in cur-
Transaxial FOV (cm) 60 60
rent clinical PET/MRI. More exciting is the
Axial FOV (cm) 25.8 25.0 developing practice of correcting PET images
Detector type Avalanche photodiode Silicon photomultiplier for multiple types of motion simultaneously.
Timing resolution (ps) 2930 386 Simultaneous PET/MRI can be corrected for
respiratory, cardiac, and bulk patient motion
PET performance specifications
using simultaneously acquired MR images.
PET sensitivity (cps/kBq) 15.0 23.3 As a result, the PET images have reduced mo-
PET spatial resolution at 1 cm (mm) 4.3 4.4 tion artifacts, decreased blurring, improved
PET peak noise equivalent count rate 184 at 23.1 218 at 17.8 colocalization of PET and MRI anatomy, and
(kcps) at kBq/mL more accurate SUV measurements. These
Note—The system design characteristics have been described elsewhere [4, 5]. The National Electrical
techniques may improve PET beyond what
Manufacturers’ Association PET performance specifications have been described elsewhere [4, 160]. is currently available in PET/CT. There have
been several publications showing the effec-
an excellent summary). As opposed to the required special attention. The Signa sys- tiveness of these promising techniques (see
straightforward attenuation correction used tem uses an atlas-based approach (an average [24] for a good review), but to date there are
with CT, MRI-based attenuation correction skull is inserted in to the MRI-based attenua- no commercially available algorithms.
involves various components: patient attenu- tion correction map) to compensate for skull
ation correction, bed and coil hardware atten- attenuation [14]. A zero-TE MRI sequence Oncologic Body Applications
uation correction, and truncation correction has recently been introduced to produce a General Considerations
[3]. To identify artifacts, it remains important patient-specific skull attenuation map [15, Integrated PET/MRI has several technical
that MRI-based attenuation correction maps 16] (Fig. S1 can be viewed in the AJR elec- advantages over PET/CT that are particularly
and non–attenuation-corrected images be dis- tronic supplement to this article, available relevant for body applications. With PET/CT,
played and reviewed during interpretation [7]. at www.ajronline.org). The Biograph mMR most protocols are performed with nongated
For body MRI-based attenuation correc- system uses an ultrashort-TE sequence, and CT followed by nongated PET, which intro-
tion, vendors use a segmentation-based tech- an atlas-based approach (multipatient da- duces misregistration artifacts due to respira-
nique in which in-phase, out-of-phase, water, tabase of matched MR and CT images) has tory motion, particularly in the upper abdom-
and fat images obtained using Dixon se- recently been introduced as well. In a com- inal organs. In contrast, integrated PET/MRI
quences [8] are separated into soft tissue, fat, parison of MRI-based attenuation correction protocols routinely use respiratory gating, and
lung, and air [9] (Fig. 1). On both systems, algorithms applied to a large cohort of pa- recently even the MRI-based attenuation cor-
bone is incorrectly assigned as soft tissue, tient studies acquired on the Biograph mMR, rection can be gated. Therefore, there is a high
which will generally underestimate uptake it was shown that methods that specifically degree of temporal and spatial coregistration,
in lesions within or adjacent to bone [10, 11]. account for bone achieved low global and lo- which results in superior image fusion. Anoth-
Attenuation correction for objects outside cal bias and variance [17]. er clear advantage of PET/MRI is the length of
the body has improved. More coil hardware Other MRI-based attenuation correction ap- time PET data can be collected while simulta-
can now be locked to the table, and software proaches under development, but not yet com- neously collecting MRI data, which generates
can therefore better account for attenuation, mercially available, include those using joint PET images with decreased noise that are more
and coils that are less dense and attenuate estimation and deep learning. In joint estima- sensitive for subtle lesions. Newer radiotracers
fewer PET photons are being used [12, 13]. tion, the PET emission data are used to pro- targeting neuroendocrine tumors (NETs) (e.g.,
Bone attenuation in the head is much more vide an estimate of the attenuation informa- the recently U.S. Food and Drug Adminis-
significant than in most of the body and has tion. This method is the maximum likelihood tration [FDA]–approved 68Ga-DOTATATE)
296 AJR:211, August 2018
Update on Clinical PET/MRI
68Ga-DOTATATE [1,4,7,10-tetraazocyclodo- or remained stable at follow-up imaging. A potential to affect management of patients with
decane-1,4,7,10-tetraacetic acid–octreotide]) free-breathing ultrashort-TE sequence (not GEP NET, and this has rapidly gained traction
and prostate cancer (e.g., 11C-choline, the re- yet clinically available) or incorporation of a in our own practice.
cently FDA-approved 18F-fluciclovine, and 3D contrast-enhanced T1-weighted thoracic
non–FDA-approved 68Ga-prostate-specific sequence in the PET/MRI protocol may im- Pancreatic Adenocarcinoma
membrane antigen [PSMA]) may be especially prove the detection of solid pulmonary nod- FDG PET/CT has not been widely adopt-
well suited for PET/MRI. Cancers that occur ules at MRI down to 6 mm [30]. It is important ed for the evaluation of pancreatic ductal ad-
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
in body locations where MRI is clearly supe- to note that the nondiagnostic CT component enocarcinoma (PDAC), likely in part because
rior to CT, such as colon cancer and especially of PET/CT is also inferior to diagnostic CT for of the low level of FDG activity of these tu-
rectal cancer, have dominated the clinical prac- the detection of pulmonary nodules. There- mors [37]. However, the higher sensitivity of
tice so far. fore, additional diagnostic chest CT may be silicon photomultipliers combined with respi-
considered as part of cancer staging. ratory gating and longer PET acquisition that
Hepatobiliary Cancer is possible with simultaneous PET/MRI may
PET/MRI has been shown to be particular- Neuroendocrine Tumors be particularly beneficial for the evaluation of
ly helpful for assessment of liver metastases A novel class of somatostatin analogs la- PDAC. In a small study, PET/MRI has shown
and, therefore, has utility in evaluating malig- beled with the positron-emitting radionu- better performance than multiphase CT to de-
nancies with a propensity for hepatic spread clide 68Ga have become part of standard tect liver metastases in patients with PDAC
(Fig. 2). A recent study found that multipa- evaluation of NETs. Of the available agents, [38]. However, CT and PET/MRI are comple-
rametric FDG PET/MRI had comparatively 68Ga-DOTATATE is approved in the United mentary to each other in PDAC evaluation;
higher accuracy for the detection of liver me- States for this indication. Molecular imag- CT is the preferred imaging modality for lo-
tastases from nonmucinous colorectal tumors ing with 68Ga-DOTATATE PET allows ac- coregional assessment, whereas PET/MRI
when compared with the individual modali- curate delineation of disease extent, identifi- is mainly used to evaluate distant metastatic
ties (PET and MRI) [25]. Hepatobiliary phase cation of a primary tumor that may be occult disease and response to neoadjuvant therapy
liver imaging after administration of hepato- on cross-sectional imaging, and noninvasive in patients with borderline resectable PDAC
cyte-specific contrast agent, such as gadox- characterization of tumor receptor status and [37]. Imaging biomarkers from integrated
etate, has critical advantages for the detection heterogeneity [31, 32]. On the other hand, PET/MRI may also predict prognosis [38,
of hepatic metastases. Navigated hepatobi- MRI is considered a robust anatomic mo- 39]. In one study, the ratio of metabolic tu-
liary phase imaging using gadoxetate aligns dality for liver imaging. In particular, DWI mor volume to minimum apparent diffusion
well with respiratory-compensated list mode and the hepatobiliary-specific MRI contrast coefficient (ADC) was found to correlate with
liver PET data [26]. PET/MRI overlay of met- agent gadoxetate disodium have shown a tumor aggressiveness, clinical stage, and pro-
abolic information on the hepatobiliary phase very high sensitivity for the detection of he- gression-free survival in patients with PDAC
images adds to the ability to detect active ver- patic metastases (Fig. 3) from gastroentero- or periampullary cancer [39].
sus inactive cancer and improves reader diag- pancreatic (GEP) NETs [33–35]. Because
nostic confidence [27]. many patients with GEP NETs undergo dedi- Prostate Cancer
The field still lacks standardized PET/MRI cated liver MRI and PET during routine stag- Multiparametric MRI has a well-established
protocols [1], allowing some novel approaches ing and after therapy, a combined PET/MRI role in the evaluation of prostate cancer at the
to develop. For example, an adaptive PET/MRI approach offers the promise to provide one time of initial staging but can have variable re-
protocol with whole-body PET/MRI followed comprehensive study for GEP NETs (Fig. 3). sults depending on the protocol, tumor grade,
by dedicated MRI of organs with positive PET In a study that used a single-injection and tumor size. Integrated PET/MRI using
findings has been applied to colorectal cancer, dual-imaging protocol, PET/MRI using prostate-specific PET probes has been evalu-
adding clinical value compared with contrast- 68Ga-DOTATOC (1,4,7,10-tetraazocyclodo- ated to improve performance of the individ-
enhanced CT, especially in lymph nodes and decane-1,4,7,10-tetraacetic acid-D-Phy1-Tyr3- ual modalities for staging; however, this is an
liver lesions [28]. The improved characteriza- octreotide) correctly identified more NET off-label indication in the United States but is a
tion of these lesions with PET/MRI was mainly lesions than did 68Ga-DOTATOC PET/CT relatively common use of PET/MRI in Europe
the result of the information provided by MRI. and provided superior lesion conspicuity. A [1]. In one study, 68Ga-PSMA-11 PET/MRI
In 21.6% (11/51) of patients, treatment strategy strong correlation was observed in the max- showed incremental gain in diagnostic perfor-
was changed because of additional information imum SUVs from the two modalities [36]. mance over the individual modalities (multipa-
provided by PET/MRI. However, PET/MRI However, the MRI component of the imag- rametric MRI and PET) for localization of pri-
had inferior performance for detection of pul- ing protocol was performed with gadobutrol, mary prostate cancer [40]. These results have
monary metastases (detection rate of 52.9%). which is an extracellular contrast agent. An- the potential to improve the performance of
The inferior performance of PET/MRI other single-injection dual-imaging protocol targeted fusion image–guided biopsy. In theo-
compared with CT for the detection of pul- PET/MRI study that used a hepatobiliary-spe- ry, integrated PET/MRI also has the potential
monary metastases is primarily due to known cific contrast agent, gadoxetate, found an in- to improve detection of regional lymph node
limitations of the MRI component. However, creased detection rate for hepatic metastases and distant metastases at the time of initial
a study examining pulmonary nodules missed on the hepatobiliary phase imaging [27]. Thus, staging. However, there have been limited and
at PET/MRI in a heterogeneous cohort of pa- a synergistic combination of 68Ga-peptide PET contradictory preliminary data about the use-
tients with cancer [29] found that most missed with optimized multiphase MRI, including a fulness of 68Ga-PSMA PET for this indication
non–FDG-avid nodules either disappeared hepatobiliary-specific contrast agent, has the [40–42], necessitating further research.
AJR:211, August 2018 297
Broski et al.
Another potential use of PET/MRI is in be performed at a significantly lower radia- improve accuracy when considered in addition
the investigation of biochemical recurrence tion dose than can PET/CT, which is especial- to multiparametric MRI (which included con-
of prostate cancer. In general, MRI is consid- ly important in young patients needing serial trast-enhanced imaging, DWI, ADC, PWI, and
ered superior for the detection of local recur- imaging evaluation. In one prospective pilot MRS) [63]. A recent prospective study exam-
rence, compared with 11C-choline and 18F-flu- study in patients with ulcerative colitis, hybrid ining integrated FDG PET/MRI showed a bet-
ciclovine PET/CT, whereas PET using these PET/MRI metrics were more accurate than ter overall performance of PWI compared with
approved prostate-specific probes is consid- serum biomarkers for assessing subclinical PET in differentiating low- from high-grade
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
ered the modality of choice for the detection inflammation, and the combination of serum gliomas and also recurrent tumor from treat-
of nodal and distant metastases [43]. There- biomarkers plus PET/MRI was even more ac- ment effect. Interestingly, there was poor corre-
fore, the combination of the two modalities curate than either alone [53]. lation between perfusion measures and SUVs,
can offer a one-stop shop for the evaluation of which the authors attributed to these parameters
prostate cancer biochemical recurrence (Fig. Oncologic Neurology Applications showing different aspects of tumor biology [64].
4). Initial studies using the single-injection Primary Brain Tumors Similarly, a recent study examining integrated
dual-imaging protocol have shown equivalent Neurooncologic PET/MRI uses targeted ra- 18F-FET PET/MRI in predicting glioma grade
performance of PET/MRI and PET/CT for diotracers to evaluate different aspects of tu- showed that 18F-FET PET and PWI differenti-
the detection of nodal and osseous metastases mor function and behavior, including glucose ated low- from high-grade gliomas with similar
from recurrent prostate cancer [44, 45]. metabolism (FDG), amino acid transport, accuracy, but that regional abnormalities were
protein synthesis (11C-methionine, 18F-fluo- often incongruent between PET and PWI, likely
Gynecologic Cancer roethyl-L-tyrosine [FET], and 18F-fluoro-L-3, indicating different pathophysiologic phenome-
Both MRI and PET have well-defined and 4-dihydroxyphenylalanine [DOPA]), DNA na [65]. Simultaneous FET PET/MRI has been
independent utility in the evaluation of gyne- synthesis (18F-fluorothymidine), and hypoxia shown to be useful in evaluation of patients with
cologic malignancies. The major gynecologic (18F-fluoromisonidazole). In the United States, suspected recurrent glioma [66], including dif-
applications of PET/MRI have been in the pri- the use of these agents, with the exception of ferentiation of recurrence from radiation necro-
mary staging of cervical and endometrial ma- FDG, is mainly in the research domain. sis [67]. Integrated 18F-DOPA PET/MRI has
lignancies, planning of radiotherapy in cervi- FDG PET has proven utility in differenti- been shown to have excellent accuracy for as-
cal cancer, evaluation of response to therapy ating radiation necrosis from recurrent tumor sessing striatal involvement in pediatric glioma
in ovarian cancer, and detection of recurrence [54], correlates with tumor grade [55], and [68]. Given these results, amino acid PET/MRI
in these malignancies [46–49]. In many of may show transformation from low- to high- is expected to have a significant effect for pa-
these studies, combined PET/MRI showed in- grade glioma [55, 56]. However, FDG inter- tients with glioma in the United States once it is
cremental benefits in accuracy compared with pretation is hampered by high intrinsic uptake clinically available.
PET and MRI individually. However, it should of FDG in normal brain parenchyma, result- Primary CNS lymphoma (PCNSL) and glio-
be noted that Medicare in the United States ing in inferior differentiation of tumor mar- blastoma multiforme (GBM) can have overlap-
limits the approved use of FDG PET in initial gins compared with amino acid tracers such ping imaging features at MRI, including cor-
staging of cervical cancer to patients with evi- as 18F-FET PET [57] and 18F-DOPA [58]. pus callosum involvement. Several studies have
dence of distant metastases. These tracers have greater signal-to-back- shown the utility of FDG PET to differentiate
ground noise ratio and specificity for tumor- PCNSL (which typically is more FDG avid)
Nononcologic Body Applications: al tissue compared with FDG and have been from GBM (which typically is less FDG avid)
Inflammatory Bowel Disease shown to be the PET agents of choice for glio- [63, 69] (Fig. 5). FDG PET has also shown
In patients with Crohn disease and ulcer- ma assessment [59, 60]. benefit in PCNSL treatment response evalua-
ative colitis, FDG PET/MRI may hold prom- Advanced MRI techniques, including DWI, tion [70] and offers prognostic information for
ise. There are two potential indications: dif- perfusion-weighted imaging (PWI), diffusion- these patients [71]. Makino and colleagues [72]
ferentiation of predominantly fibrotic from tensor imaging, and MR spectroscopy (MRS), examined the added benefit of FDG uptake
predominantly inflammatory strictures and have now become an integral part of brain tu- and quantitative ADCs to conventional MRI
assessment of systemic disease activity [50, mor management [61]. For example, the com- to differentiate between PCNSL and GBM
51]. Both CT enterography and MR enterog- bination of functional MRI and diffusion-ten- and found increased accuracy by inclusion of
raphy have shown inconsistent results for sor imaging can show the spatial relationship metabolic data (95% vs 75%) but no diagnos-
differentiation of fibrotic and inflammatory between intracranial lesions and white matter tic effect from the inclusion of ADC data. In
strictures because of their reliance on con- tracts, which is highly useful for preoperative contrast, larger and more recent studies have
trast enhancement for this distinction. In one planning and risk assessment [62]. shown the utility of both PWI and DWI in dif-
PET/MRI study, the product of maximum The unprecedented multiparametric func- ferentiating PCNSL and GBM [73, 74]. There
SUV and ADC showed a trend toward bet- tional, anatomic, and metabolic capability of have yet to be any studies detailing the perfor-
ter performance than did individual PET and integrated PET/MRI seems well suited for pri- mance of integrated PET/MRI for this purpose.
MRI metrics for the identification of predomi- mary CNS lesion evaluation, but initial reports
nantly fibrotic enteric strictures [50]. Integrat- have been conflicting. A recent retrospective Intracranial Metastases
ed PET/MRI has also shown higher accura- study of 60 gliomas evaluated with FDG PET Although there has been tremendous re-
cy for the detection of active inflammation in and multiparametric MRI showed that PET de- search into the roles of PET and MRI in eval-
patients with Crohn disease than either MRI lineated between high- and low-grade gliomas uation of primary CNS tumors, intracranial
or PET alone [52]. Moreover, PET/MRI can with accuracy similar to that of MRI but did not metastatic disease occurs up to 10 times more
298 AJR:211, August 2018
Update on Clinical PET/MRI
commonly than does primary CNS tumor [75]. structural lesions and to show specific atro- have detailed early success with both FDG
Simultaneous brain PET/MRI may be acquired phy patterns, such as atrophy of the medial and amyloid PET/MRI in patients with AD,
to assess the presence of intracranial metastatic temporal lobes in patients with Alzheimer dementia with Lewy bodies, vascular de-
disease from sources outside the CNS, includ- disease (AD) [84], one of the best-established mentia, frontotemporal dementia, and logo-
ing advanced lung cancer [76] (Fig. 6) and high- neuroimaging biomarkers of AD. Moreover, penic aphasia [93–95].
risk melanoma [77]. Complete staging in a sin- MRI can detect specific patterns of atrophy
gle examination increases patient convenience and signal abnormality in less-common neu-
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
Epilepsy
and is a key advantage of integrated PET/MRI rodegenerative processes, such as selective FDG PET/MRI has been successful in
compared with separate PET/CT and brain midbrain atrophy in progressive supranucle- helping to bring more patients with intrac-
MRI in patients at risk for brain metastases. ar palsy and pontocerebellar atrophy with table epilepsy to surgery for cure. FDG is
cruciform T2 hyperintensity in multiple sys- the most commonly applied PET radiotracer
Head-and-Neck Cancer tem atrophy [85, 86]. for these patients, because epileptogenic foci
Head-and-neck cancer represents anoth- PET has a well-proven ability to detect typically show hypometabolism on interictal
er exciting avenue for PET/MRI use given pathologic abnormalities at a molecular level, imaging [96]. Focal FDG hypometabolism
the widespread use of PET/CT and MRI for long before the structural and signal changes may correspond to subtle abnormalities iden-
radiation and preoperative planning. FDG occur at MRI. There are several available ra- tified at MRI, thus increasing confidence, or
PET/CT has a well-established role in head diotracers in clinical use for imaging of patients when the MRI appears normal, FDG PET
and neck squamous cell carcinoma, includ- with dementia, including FDG and several am- can independently suggest a target for sur-
ing staging, detection of occult primary ma- yloid PET agents, including 18F-florbetapir, 18F- gical resection [58] (Fig. 7). For example, a
lignancies, assessment of chemoradiothera- florbetaben, and 18F-flutemetamol. FDG PET significant portion of patients with focal cor-
peutic response, and differentiation of local has high accuracy in distinguishing AD from tical dysplasia and negative MRI have posi-
recurrence from treatment effect [78]. other neurodegenerative disorders, such as tive PET findings [97, 98].
Huang et al. [79] found that fused PET/MR frontotemporal dementia [87]. Although FDG Studies have shown that fusion of FDG
images had a higher coefficient of correla- PET is FDA approved only for distinguishing PET with separately acquired MRI improves
tion with pathologic tumor size than did con- AD from frontotemporal dementia, distinc- the diagnosis of focal cortical dysplasia com-
trast-enhanced CT, MRI, or PET/CT. Com- tive patterns of cerebral hypometabolism have pared with each modality on its own. It has
bined gadolinium-enhanced PET/MRI has been described in many other neurodegenera- been found to be especially helpful in pa-
been shown to yield similar radiation treat- tive conditions [85, 86, 88]. The typical pattern tients with normal MRI scans and subtle cas-
ment gross tumor volumes compared with CT of AD hypometabolism is considered an imag- es of cortical dysplasia [99] and allows more
in patients with primary oropharyngeal cancer ing biomarker [89]. Amyloid PET has emerged limited cortical resection in select patients
[80], although the authors noted cases in which as an invaluable tool for noninvasive evalua- [100]. A study of 29 patients with refractory
PET/MRI substantially altered the gross tu- tion of amyloid burden [90]. Patients with amy- epilepsy undergoing PET/MRI showed that
mor volume and, therefore, radiation plan. Re- loid-positive findings at PET tend to experience PET/MRI increased the diagnostic accuracy
searchers from Zurich have found improved faster cognitive decline, greater likelihood of of localizing an epileptogenic focus compared
performance of contrast-enhanced PET/MRI mild cognitive impairment progression to AD, with separate MRI and PET/CT [101]. Addi-
versus contrast-enhanced PET/CT in 85 pa- and faster rates of brain atrophy than do control tional pilot data have indicated a clear role for
tients with head-and-neck cancer undergoing subjects with amyloid-negative findings [91]. PET/MRI in patients with refractory epilepsy
sequential PET/CT and PET/MRI on a trimo- As such, positive cortical amyloid binding is [102]. Combination high-sensitivity electroen-
dality system, noting increased diagnostic con- also considered a biomarker of AD pathology cephalography and PET with functional MRI
fidence for accurate lesion detection (especial- and has been implemented into the diagnostic evaluation has been shown to achieve reliable
ly in the nasopharynx or larynx), infiltration criteria of mild cognitive impairment and AD- interictal data with better efficiency, reduced
of adjacent structures, and perineural spread related dementia [92]. bias, and decreased cost [103].
of tumor [81]. This is especially critical given Given the ability of PET/MRI to depict
the higher risk of local recurrence, metastat- biomarkers of β-amyloid plaque deposition Oncologic Musculoskeletal PET/MRI
ic disease, and decreased survival in patients (cortical amyloid PET binding) and neuronal Bone and Soft-Tissue Sarcomas
with perineural metastasis [82]. An additional degeneration and injury (MRI temporal lobe MRI is the reference standard for assessing
study examining integrated PET/MRI evalua- atrophy and FDG PET hypometabolism), in- the T stage of bone sarcomas and soft-tissue
tion of 16 patients with pathologically proven tegrated PET/MRI offers the possibility of a sarcomas (STSs), given its ability to show the
laryngeal cancer reported on the usefulness of complete neuroimaging assessment in one tumor’s relationship to neurovascular struc-
PET/MRI for staging, noting a significant cor- convenient session. A recent study of simul- tures, joints, and muscular compartments [77,
relation between PET/MRI findings and en- taneous amyloid PET/MRI in 100 subjects 104–106]. The addition of novel MRI tech-
doscopic or histologic evaluation and also a with suspected mild cognitive impairment, niques, such as DWI, ADC, dynamic contrast
significant effect on patient management [83]. AD, or frontotemporal dementia who un- enhancement, and MRS, may improve diag-
derwent simultaneous PET/MRI with 18F- nostic accuracy compared with conventional
Nononcologic Neurology Applications florbetaben or 11C-labeled Pittsburgh com- MRI [105, 107, 108]. Combining these tech-
Dementia pound B found feasibility and high patient niques with metabolic measures, such as SUV,
MRI plays an important role in dementia or caregiver and referrer acceptance of this total lesion glycolysis, and metabolic tumor
evaluation. It is useful to exclude treatable new one-stop imaging test [92]. Other studies volume, provides powerful multiparametric
AJR:211, August 2018 299
Broski et al.
evaluation. Combined metabolic and MRS MRI can detect marrow signal changes of nary, infiltrative, and inflammatory diseas-
evaluation on FDG PET/MRI has already myelomatous lesions before osseous destruc- es [1, 146, 147]. Coronary ischemia repre-
been explored in STS [109], and a radiomics tion is seen at CT. MRI also has proven superi- sents the most common indication for cardiac
model examining FDG PET/MRI texture fea- ority in detecting diffuse bone marrow involve- PET/MRI. Recent work has shown benefit in
tures has been used to predict the presence of ment compared with whole-body low-dose CT combining complementary coregistered coro-
pulmonary metastases in 51 patients with ex- or PET/CT [127–129]. Incorporation of DWI nary blood flow and myocardial flow reserve
tremity STS [110]. results in greater lesion conspicuity compared as assessed by PET, with simultaneous func-
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
The addition of focused PET assessment with conventional MRI [130, 131], and ADC tional imaging and infarct- or scar-related de-
of primary bone sarcoma and STS provides values have excellent accuracy to differentiate layed enhancement as assessed by MRI [147].
prognostic information and can help guide diseased from normal marrow [132, 133]. FDG Improvements in complex respiratory and
biopsy. Baseline FDG activity in STS and PET/CT performs equally well to MRI in de- cardiac motion correction take advantage of
bone sarcoma has been correlated with sur- tecting focal lesions but, again, is inferior for simultaneous PET/MRI acquisition to im-
vival in several studies [111, 112]. Dedicat- detecting diffuse disease [127–129, 134, 135]. prove image resolution, colocalization, and
ed PET evaluation of sarcomas may also Both MRI and PET are beneficial in eval- diagnostic confidence, thus making PET/MRI
allow sampling of the most FDG-avid high- uating treatment response. Giles and col- superior to PET/CT plus MRI for evaluating
est-grade areas of tumor [113, 114]. This can leagues [136] showed that increased ADC these cardiac conditions [148–151].
be especially important in large or high- has excellent accuracy in determining posi- There is growing excitement about the role
grade sarcomas, which may be prone to non- tive treatment response, which has also been of cardiac PET/MRI, particularly in the eval-
diagnostic biopsy or undersampling given supported by other studies [137]. The role uation of inflammatory and infiltrative cardio-
significant heterogeneity (Fig. 8). of FDG PET/CT in assessing treatment re- myopathies, such as sarcoidosis and amyloido-
In 2017, Platzek et al. [115] assessed the role sponse was well seen in a recent meta-anal- sis [1, 152]. MRI has long been a mainstay in
of FDG PET/MRI in staging 29 patients with ysis including 690 patients with myeloma the evaluation of patients with infiltrative car-
bone sarcoma and STS. They found identical from 10 studies [138]. PET/CT may show diomyopathies. In cardiac sarcoidosis, MRI al-
T, M, and N staging for PET/MRI and conven- disease response earlier than MRI, because lows accurate diagnosis and assessment of car-
tional imaging in 28 of 29 patients. PET/MRI resolution of FDG activity is typically seen diac injury and function, whereas PET adds the
had a slightly increased sensitivity for detecting before MRI signal normalization. ability to detect active inflammation and assess
distant metastases (97.8% vs 94.4% for conven- Shortt and colleagues [141] found that, al- whether further antiinflammatory treatment is
tional imaging), but this was insignificant (p = though whole-body MRI outperformed FDG needed [153]. PET/MRI allows simultaneous
0.51). A number of small case series and pilot PET/CT in assessment of active multiple my- assessment of all of these cardiac factors, mak-
studies have also shown potential benefit of eloma, adding FDG PET information to MRI ing it a potential modality of choice for imaging
PET/MRI in STS staging [116–118]. improved the results of MRI alone. Sachpe- [154]. A recent joint Society of Nuclear Medi-
The utility of FDG PET for response as- kidis et al. [142] showed the equivalency of cine and Molecular Imaging and American
sessment after chemotherapy has been PET/CT and PET/MRI for the detection of Society of Nuclear Cardiology expert consen-
shown for patients with STS [119, 120] and myeloma lesions in 30 patients using a sin- sus statement suggests that FDG PET/CT can
bone sarcoma [121, 122]. Quantitative ADC gle-injection PET/CT and PET/MRI proto- be used for follow-up of patients with cardiac
maps have been used to assess STS response col. PET/MRI missed rib lesions identified sarcoidosis to assess for treatment response
at MRI [107, 108]. Combined PET and MRI at PET/CT evaluation, which is unsurprising and that specialized coronary blood flow imag-
evaluation would therefore seem synergistic given that MRI has known limitations in eval- ing with 82Rb or 13N-ammonia plus FDG car-
in evaluating chemotherapeutic response, but uation of the ribs, skull, and clavicles [143]. diac and body imaging should be used [155].
several studies have shown discordant results In our experience, PET/MRI has been help- When appropriate, this same method has been
between PET and MRI measures [123, 124] ful in cases of diffuse myelomatous disease, applied to PET/MRI. Recent data suggest that
after neoadjuvant therapy. However, a recent which is better seen with MRI than PET (Fig. 9), radiotracers such as Ga-DOTATOC (not FDA
study found superior diagnostic accuracy of and also in depicting resolution of FDG activ- approved) or Ga-DOTATATE (FDA approved,
integrated FDG PET/MRI compared with ity in responding lesions before normalization of but off-label for cardiac imaging), which target
stand-alone MRI for identification of locally signal abnormality at MRI (Fig. 10). There are somatostatin receptors, could also be used to
recurrent STSs, and PET/MRI also conferred conflicting data on the importance of osteolysis image cardiac and systemic sarcoidosis with-
higher confidence levels for delineating ma- at PET/CT, but despite this, the updated Inter- out the need for hard-to-follow special dietary
lignant lesions [125]. Future prospective national Myeloma Working Group guidelines preparations [156].
studies are expected to define the role of in- necessitate the presence of osteolysis to make PET/MRI has great potential in evaluating
tegrated PET/MRI in the posttherapy setting. the diagnosis of active disease at PET/CT [126]. myocardial deposition of light-chain and amy-
This is an additional advantage of integrated loidogenic transthyretin (ATTR) amyloid. In the
Multiple Myeloma FDG PET/MRI, to depict intramedullary le- right clinical setting, bone radiotracer imaging,
The diagnosis of multiple myeloma can be sions at MRI that are occult at CT, thereby in- such as pyrophosphate planar and SPECT/CT,
made on the basis of clinical and laboratory creasing sensitivity for active disease (Fig. 10). is specific enough as to have been suggested to
measures alone [126]. However, advanced im- potentially remove the need for more invasive
aging can play a key role in better diagnosing Cardiac Applications diagnostic procedures, such as endomyocardial
active versus inactive disease, prognosticat- Cardiac PET/MRI has been advancing into biopsy, for diagnosing ATTR in some patients
ing, and assessing early response to therapy. clinical practice for the evaluation of coro- [157]. More recently, the use of 18F-NaF (FDA
300 AJR:211, August 2018
Update on Clinical PET/MRI
approved, but off-label for use in the heart) PET 4. Delso G, Furst S, Jakoby B, et al. Performance telmans L, Suetens P. Simultaneous maximum a
for the detection of ATTR using PET/MRI has measurements of the Siemens mMR integrated posteriori reconstruction of attenuation and activity
been proposed [157]. The use of SPECT-based whole-body PET/MR scanner. J Nucl Med 2011; distributions from emission sinograms. IEEE
bone scan agents is already becoming the stan- 52:1914–1922 Trans Med Imaging 1999; 18:393–403
dard of care to diagnose ATTR cardiomyopathy 5. Levin CS, Maramraju SH, Khalighi MM, Deller 19. Defrise M, Rezaei A, Nuyts J. Time-of-flight PET
[156], and 18F-NaF allows this strategy to move TW, Delso G, Jansen F. Design features and mu- data determine the attenuation sinogram up to a
to PET and PET/MRI. Another exciting option tual compatibility studies of the time-of-flight constant. Phys Med Biol 2012; 57:885–899
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
is to use FDA-approved radiotracers designed to PET capable GE SIGNA PET/MR system. IEEE 20. Chartrand G, Cheng PM, Vorontsov E, et
target β-amyloid in the brain (FDA approved, Trans Med Imaging 2016; 35:1907–1914 al. Deep learning: a primer for radiologists.
but off-label for use in the heart), including flo- 6. Chen Y, An H. Attenuation correction of RadioGraphics 2017; 37:2113–2131
rbetapir, flutemetamol, and florbetaben for tar- PET/MR imaging. Magn Reson Imaging Clin N 21. Zaharchuk G, Gong E, Wintermark M, Rubin D,
geting either amyloidosis or ATTR in the heart Am 2017; 25:245–255 Langlotz CP. Deep learning in neuroradiology.
[158]. These techniques promise to directly bind 7. Keller SH, Holm S, Hansen AE, et al. Image arti- AJNR 2018 Feb 1 [Epub ahead of print]
to amyloidosis in the heart and, when used in facts from MR-based attenuation correction in 22. Hwang D, Kim KY, Kang SK, et al. Im-
combination with blood-flow analysis, may be clinical, whole-body PET/MRI. MAGMA 2013; proving accuracy of simultaneously reconstructed
able to quantify amyloid burden. Given these 26:173–181 activity and attenuation maps using deep learning.
promising new therapies, there is excitement 8. Dixon WT. Simple proton spectroscopic imag- J Nucl Med 2018 Feb 15 [Epub ahead of print]
that this imaging method may allow therapy as- ing. Radiology 1984; 153:189–194 23. Leynes AP, Yang J, Wiesinger F, et al. Direct
sessment at follow-up. 9. Wollenweber S, Ambwani S, Lonn A, et al. Com- pseudoCT generation for pelvis PET/MRI attenu-
parison of 4-class and continuous fat/water methods ation correction using deep convolutional neural
Conclusion for whole-body, MR-based PET attenuation correc- networks with multi-parametric MRI: zero echo-
Clinical PET/MRI is in a dynamic period, tion. IEEE Trans Nucl Sci 2013; 60:3391–3398 time and Dixon Deep pseudoCT (ZeDD-CT).
and the future appears bright. Critical issues 10. Aznar MC, Sersar R, Saabye J, et al. Whole-body J Nucl Med 2017; 59:852–858
have been overcome, and the unique advantages PET/MRI: the effect of bone attenuation during 24. Fayad H, Lamare F, Merlin T, Visvikis D.
of simultaneous PET/MRI are being harnessed MR-based attenuation correction in oncology im- Motion correction using anatomical information
to better diagnose disease. Comparison with aging. Eur J Radiol 2014; 83:1177–1183 in PET/CT and PET/MR hybrid imaging. Q J
PET/CT is generally no longer needed. MRI- 11. Samarin A, Burger C, Wollenweber SD, et al. Nucl Med Mol Imaging 2016; 60:12–24
based attenuation correction is adequate for PET/MR imaging of bone lesions: implications 25. Brendle C, Schwenzer NF, Rempp H, et al. As-
clinical use and is rapidly advancing. Complex for PET quantification from imperfect attenua- sessment of metastatic colorectal cancer with hy-
motion correction and advances in silicon pho- tion correction. Eur J Nucl Med Mol Imaging brid imaging: comparison of reading perfor-
tomultipliers and image reconstruction prom- 2012; 39:1154–1160 mance using different combinations of
ise to bring significant improvements in image 12. Eldib M, Bini J, Faul DD, Oesingmann N, anatomical and functional imaging techniques in
quality. Imaging of certain diseases, such as liv- Tsoumpas C, Fayad ZA. Attenuation correction PET/MRI and PET/CT in a short case series.
er metastases, uniquely benefits from PET/MRI. for magnetic resonance coils in combined Eur J Nucl Med Mol Imaging 2016; 43:123–132
Several new radiotracers are and will be used to PET/MR imaging: a review. PET Clin 2016; 26. Hope TA, Pampaloni MH, Nakakura E, et al. Si-
better advantage on PET/MRI compared with 11:151–160 multaneous 68Ga-DOTA-TOC PET/MRI with
PET/CT. Faster and more robust MRI protocols 13. Paulus DH, Tellmann L, Quick HH. Towards im- gadoxetate disodium in patients with neuroendo-
allow more-complete scans with improved pa- proved hardware component attenuation correc- crine tumor. Abdom Imaging 2015; 40:1432–1440
tient satisfaction. Continued efforts to standard- tion in PET/MR hybrid imaging. Phys Med Biol 27. Kirchner J, Sawicki LM, Deuschl C, et al. 18 F-
ize protocols across institutions and develop in- 2013; 58:8021–8040 FDG PET/MR imaging in patients with suspect-
novative solutions for the challenges posed by 14. Wollenweber SD, Ambwani S, Delso G, et al. ed liver lesions: value of liver-specific contrast
this hybrid modality will be critical to the long- Evaluation of an atlas-based PET head attenua- agent gadobenate dimeglumine. PLoS One 2017;
term success of PET/MRI. tion correction using PET/CT & MR patient data. 12:e0180349
IEEE Trans Nucl Sci 2013; 60:3383–3390 28. Kang B, Lee J, Song Y, et al. Added value
References 15. Sekine T, Ter Voert EE, Warnock G, et al. Clini- of integrated whole-body PET/MRI for evalua-
1. Fendler WP, Czernin J, Herrmann K, Beyer T. cal evaluation of zero-echo-time attenuation cor- tion of colorectal cancer: comparison with con-
Variations in PET/MRI operations: results from rection for brain 18F-FDG PET/MRI: comparison trast-enhanced MDCT. AJR 2016; 206:[web]
an international survey among 39 active sites. with atlas attenuation correction. J Nucl Med W10–W20
J Nucl Med 2016; 57:2016–2021 2016; 57:1927–1932 29. Raad RA, Friedman KP, Heacock L, Ponzo F,
2. Spick C, Herrmann K, Czernin J. 18F-FDG 16. Wiesinger F, Sacolick LI, Menini A, et al. Zero Melsaether A, Chandarana H. Outcome of small
PET/CT and PET/MRI perform equally well in TE MR bone imaging in the head. Magn Reson lung nodules missed on hybrid PET/MRI in pa-
cancer: evidence from studies on more than Med 2016; 75:107–114 tients with primary malignancy. J Magn Reson
2,300 patients. J Nucl Med 2016; 57:420–430 17. Ladefoged CN, Law I, Anazodo U, et al. A multi- Imaging 2016; 43:504–511
3. Bailey DL, Pichler BJ, Guckel B, et al. Combined centre evaluation of eleven clinically feasible 30. Burris NS, Johnson KM, Larson PE, et al.
PET/MRI: global warming—summary report of brain PET/MRI attenuation correction tech- Detection of small pulmonary nodules with ultra-
the 6th International Workshop on PET/MRI, niques using a large cohort of patients. Neuroim- short echo time sequences in oncology patients
March 27-29, 2017, Tubingen, Germany. Mol Im- age 2017; 147:346–359 by using a PET/MR system. Radiology 2016;
aging Biol 2018; 20:4–20 18. Nuyts J, Dupont P, Stroobants S, Benninck R, Mor- 278:239–246
AJR:211, August 2018 301
Broski et al.
31. Baumann T, Rottenburger C, Nicolas G, Wild D. static prostate cancer detected by 68Ga-PSMA- diagnosis: a meta-analysis. AJNR 2013; 34:944–
Gastroenteropancreatic neuroendocrine tumours positron emission tomography/computerized 950
(GEP-NET): imaging and staging. Best Pract Res tomography. Prostate 2015; 75:1934–1940 55. Padma MV, Said S, Jacobs M, et al. Prediction of
Clin Endocrinol Metab 2016; 30:45–57 43. Kitajima K, Murphy RC, Nathan MA, et al. Detec- pathology and survival by FDG PET in gliomas.
32. Deroose CM, Hindié E, Kebebew E, et al. tion of recurrent prostate cancer after radical pros- J Neurooncol 2003; 64:227–237
Molecular imaging of gastroenteropancreatic tatectomy: comparison of C-11-choline PET/CT 56. De Witte O, Levivier M, Violon P, et al.
neuroendocrine tumors: current status and future with pelvic multiparametric MR imaging with en- Prognostic value positron emission tomography
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
directions. J Nucl Med 2016; 57:1949–1956 dorectal coil. J Nucl Med 2014; 55:223–232 with [18F]fluoro-2-deoxy-D-glucose in the low-
33. Giesel FL, Kratochwil C, Mehndiratta A, et al. 44. Freitag MT, Radtke JP, Hadaschik BA, et grade glioma. Neurosurgery 1996; 39:470–476;
Comparison of neuroendocrine tumor detection al. Comparison of hybrid 68Ga-PSMA PET/MRI discussion, 476–477
and characterization using DOTATOC-PET in and 68Ga-PSMA PET/CT in the evaluation of 57. Pauleit D, Stoffels G, Bachofner A, et al. Com-
correlation with contrast enhanced CT and de- lymph node and bone metastases of prostate can- parison of 18F-FET and 18F-FDG PET in brain
layed contrast enhanced MRI. Eur J Radiol 2012; cer. Eur J Nucl Med Mol Imaging 2016; 43:70–83 tumors. Nucl Med Biol 2009; 36:779–787
81:2820–2825 45. Souvatzoglou M, Eiber M, Takei T, et al. Com- 58. Miller-Thomas MM, Benzinger TL. Neu-
34. Mayerhoefer ME, Ba-Ssalamah A, Weber parison of integrated whole-body [11C]choline rologic applications of PET/MR imaging. Magn
M, et al. Gadoxetate-enhanced versus diffusion- PET/MR with PET/CT in patients with prostate Reson Imaging Clin N Am 2017; 25:297–313
weighted MRI for fused Ga-68-DOTANOC cancer. Eur J Nucl Med Mol Imaging 2013; 59. Albert NL, Weller M, Suchorska B, et al. Re-
PET/MRI in patients with neuroendocrine tu- 40:1486–1499 sponse Assessment in Neuro-Oncology Working
mours of the upper abdomen. Eur Radiol 2013; 46. Grueneisen J, Beiderwellen K, Heusch P, Group and European Association for Neuro-On-
23:1978–1985 et al. Simultaneous positron emission tomogra- cology recommendations for the clinical use of
35. Sankowski AJ, Ćwikla JB, Nowicki ML, et al. phy/magnetic resonance imaging for whole-body PET imaging in gliomas. Neuro Oncol 2016;
The clinical value of MRI using single-shot echo- staging in patients with recurrent gynecological 18:1199–1208
planar DWI to identify liver involvement in pa- malignancies of the pelvis: a comparison to 60. Dunet V, Pomoni A, Hottinger A, Nicod-
tients with advanced gastroenteropancreatic-neu- whole-body magnetic resonance imaging alone. Lalonde M, Prior JO. Performance of 18F-FET
roendocrine tumors (GEP-NETs), compared to Invest Radiol 2014; 49:808–815 versus 18F-FDG-PET for the diagnosis and grad-
FSE T2 and FFE T1 weighted image after i.v. 47. Grueneisen J, Schaarschmidt BM, Beiderwellen ing of brain tumors: systematic review and meta-
Gd-EOB-DTPA contrast enhancement. Med Sci K, et al. Diagnostic value of diffusion-weighted analysis. Neuro Oncol 2016; 18:426–434
Monit 2012; 18:MT33–MT40 imaging in simultaneous 18F-FDG PET/MR im- 61. Kimura M, da Cruz LCH Jr. Multiparametric MR
36. Sawicki LM, Deuschl C, Beiderwellen K, aging for whole-body staging of women with pel- imaging in the assessment of brain tumors. Magn
et al. Evaluation of 68Ga-DOTATOC PET/MRI vic malignancies. J Nucl Med 2014; 55:1930–1935 Reson Imaging Clin N Am 2016; 24:87–122
for whole-body staging of neuroendocrine tu- 48. Grueneisen J, Schaarschmidt BM, Heub- 62. Bailey PD, Zaca D, Basha MM, et al. Pre-
mours in comparison with 68Ga-DOTATOC ner M, et al. Integrated PET/MRI for whole-body surgical fMRI and DTI for the prediction of peri-
PET/CT. Eur Radiol 2017; 27:4091–4099 staging of patients with primary cervical cancer: operative motor and language deficits in primary
37. Yeh R, Dercle L, Garg I, Wang ZJ, Hough DM, preliminary results. Eur J Nucl Med Mol Imaging or metastatic brain lesions. J Neuroimaging 2015;
Goenka AH. The role of 18F-FDG PET/CT and 2015; 42:1814–1824 25:776–784
PET/MRI in pancreatic ductal adenocarcinoma. 49. Oldan JD, Shah SN, Rose TL. Applications of 63. Yoon JH, Kim JH, Kang WJ, et al. Grading of
Abdom Radiol (NY) 2018; 43:415–434 PET/MR imaging in urogynecologic and genito- cerebral glioma with multiparametric MR imag-
38. Chen BB, Tien YW, Chang MC, et al. urinary cancers. Magn Reson Imaging Clin N Am ing and 18F-FDG-PET: concordance and accura-
Multiparametric PET/MR imaging biomarkers 2017; 25:335–350 cy. Eur Radiol 2014; 24:380–389
are associated with overall survival in patients 50. Catalano OA, Gee MS, Nicolai E, et al. 64. Sacconi B, Raad RA, Lee J, et al. Concur-
with pancreatic cancer. Eur J Nucl Med Mol Im- Evaluation of quantitative PET/MR enterography rent functional and metabolic assessment of brain
aging 2018 Feb 23 [Epub ahead of print] biomarkers for discrimination of inflammatory tumors using hybrid PET/MR imaging. J Neu-
39. Chen BB, Tien YW, Chang MC, et al. PET/MRI strictures from fibrotic strictures in Crohn dis- rooncol 2016; 127:287–293
in pancreatic and periampullary cancer: correlat- ease. Radiology 2016; 278:792–800 65. Verger A, Filss CP, Lohmann P, et al. Comparison
ing diffusion-weighted imaging, MR spectrosco- 51. Fidler JL, Goenka AH, Fleming CJ, Andrews JC. of 18F-FET PET and perfusion-weighted MRI for
py and glucose metabolic activity with clinical Small bowel imaging: computed tomography en- glioma grading: a hybrid PET/MR study. Eur J
stage and prognosis. Eur J Nucl Med Mol Imag- terography, magnetic resonance enterography, Nucl Med Mol Imaging 2017; 44:2257–2265
ing 2016; 43:1753–1764 angiography, and nuclear medicine. Gastrointest 66. Jena A, Taneja S, Gambhir A, et al. Glioma
40. Eiber M, Weirich G, Holzapfel K, et al. Endosc Clin N Am 2017; 27:133–152 recurrence versus radiation necrosis: single-ses-
Simultaneous 68Ga-PSMA HBED-CC PET/MRI 52. Catalano OA, Wu V, Mahmood U, et al. Diagnos- sion multiparametric approach using simultane-
improves the localization of primary prostate tic performance of PET/MR in the evaluation of ous O-(2-18F-Fluoroethyl)-L-Tyrosine PET/MRI.
cancer. Eur Urol 2016; 70:829–836 active inflammation in Crohn disease. Am J Nucl Clin Nucl Med 2016; 41:e228–e236
41. Budäus L, Leyh-Bannurah SR, Salomon G, et al. Med Mol Imaging 2018; 8:62–69 67. Sogani SK, Jena A, Taneja S, et al. Potential for
Initial experience of 68Ga-PSMA PET/CT imag- 53. Shih IL, Wei SC, Yen RF, et al. PET/MRI for differentiation of glioma recurrence from radio-
ing in high-risk prostate cancer patients prior to evaluating subclinical inflammation of ulcerative necrosis using integrated 18F-fluoroethyl-L-tyro-
radical prostatectomy. Eur Urol 2016; 69:393–396 colitis. J Magn Reson Imaging 2018; 47:737–745 sine (FET) positron emission tomography/mag-
42. Hijazi S, Meller B, Leitsmann C, et al. Pel- 54. Nihashi T, Dahabreh IJ, Terasawa T. Di- netic resonance imaging: a prospective
vic lymph node dissection for nodal oligometa- agnostic accuracy of PET for recurrent glioma evaluation. Neurol India 2017; 65:293–301
302 AJR:211, August 2018
Update on Clinical PET/MRI
68. Morana G, Piccardo A, Puntoni M, et al. 80. Wang K, Mullins BT, Falchook AD, et al. Evalua- 93. Barthel H, Schroeter ML, Hoffmann KT, Sabri O.
Diagnostic and prognostic value of 18F-DOPA tion of PET/MRI for tumor volume delineation for PET/MR in dementia and other neurodegenera-
PET and 1H-MR spectroscopy in pediatric supra- head and neck cancer. Front Oncol 2017; 7:8 tive diseases. Semin Nucl Med 2015; 45:224–233
tentorial infiltrative gliomas: a comparative 81. Kuhn FP, Hullner M, Mader CE, et al. Contrast- 94. Vercher-Conejero JL, Rubbert C, Kohan AA,
study. Neuro Oncol 2015; 17:1637–1647 enhanced PET/MR imaging versus contrast-en- Partovi S, O’Donnell JK. Amyloid PET/MRI in
69. Yamashita K, Yoshiura T, Hiwatashi A, et al. Dif- hanced PET/CT in head and neck cancer: how the differential diagnosis of dementia. Clin Nucl
ferentiating primary CNS lymphoma from glio- much MR information is needed? J Nucl Med Med 2014; 39:e336–e339
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
blastoma multiforme: assessment using arterial 2014; 55:551–558 95. Moodley KK, Minati L, Barnes A, Dickson JC,
spin labeling, diffusion-weighted imaging, and 82. Paes FM, Singer AD, Checkver AN, Ell PJ, Chan D. Simultaneous PET/MRI in fron-
18F-fluorodeoxyglucose positron emission to- Palmquist RA, De La Vega G, Sidani C. Perineu- totemporal dementia. Eur J Nucl Med Mol Imag-
mography. Neuroradiology 2013; 55:135–143 ral spread in head and neck malignancies: clini- ing 2013; 40:468–469
70. Kawai N, Miyake K, Yamamoto Y, Nishiyama Y, cal significance and evaluation with 18F-FDG 96. Lee KK, Salamon N. [18F] fluorodeoxy-
Tamiya T. 18F-FDG PET in the diagnosis and PET/CT. RadioGraphics 2013; 33:1717–1736 glucose-positron-emission tomography and MR
treatment of primary central nervous system lym- 83. Cavaliere C, Romeo V, Aiello M, et al. Multipara- imaging coregistration for presurgical evaluation
phoma. BioMed Res Int 2013; 2013:247152 metric evaluation by simultaneous PET-MRI ex- of medically refractory epilepsy. AJNR 2009;
71. Kawai N, Zhen HN, Miyake K, Yamamaoto Y, amination in patients with histologically proven 30:1811–1816
Nishiyama Y, Tamiya T. Prognostic value of pre- laryngeal cancer. Eur J Radiol 2017; 88:47–55 97. Lerner JT, Salamon N, Hauptman JS, et al. As-
treatment 18F-FDG PET in patients with primary 84. Frisoni GB, Fox NC, Jack CR Jr, Schel- sessment and surgical outcomes for mild type I
central nervous system lymphoma: SUV-based tens P, Thompson PM. The clinical use of struc- and severe type II cortical dysplasia: a critical
assessment. J Neurooncol 2010; 100:225–232 tural MRI in Alzheimer disease. Nat Rev Neurol review and the UCLA experience. Epilepsia
72. Makino K, Hirai T, Nakamura H, et al. 2010; 6:67–77 2009; 50:1310–1335
Does adding FDG-PET to MRI improve the dif- 85. Broski SM, Hunt CH, Johnson GB, Morreale RF, 98. Halac G, Delil S, Zafer D, et al. Compati-
ferentiation between primary cerebral lymphoma Lowe VJ, Peller PJ. Structural and functional im- bility of MRI and FDG-PET findings with histo-
and glioblastoma? Observer performance study. aging in parkinsonian syndromes. RadioGraphics pathological results in patients with focal cortical
Ann Nucl Med 2011; 25:432–438 2014; 34:1273–1292 dysplasia. Seizure 2017; 45:80–86
73. Choi YS, Lee HJ, Ahn SS, et al. Primary central 86. Martin-Macintosh EL, Broski SM, Johnson GB, 99. Salamon N, Kung J, Shaw SJ, et al. FDG-PET/MRI
nervous system lymphoma and atypical glioblas- Hunt CH, Cullen EL, Peller PJ. Multimodality im- coregistration improves detection of cortical dys-
toma: differentiation using the initial area under aging of neurodegenerative processes. Part 2. plasia in patients with epilepsy. Neurology 2008;
the curve derived from dynamic contrast-en- Atypical dementias. AJR 2016; 207:883–895 71:1594–1601
hanced MR and the apparent diffusion coeffi- 87. Bohnen NI, Djang DS, Herholz K, Anzai Y, 100. Chassoux F, Rodrigo S, Semah F, et al. FDG-PET
cient. Eur Radiol 2017; 27:1344–1351 Minoshima S. Effectiveness and safety of improves surgical outcome in negative MRI Tay-
74. Kickingereder P, Wiestler B, Sahm F, et al. Pri- 18F-FDG PET in the evaluation of dementia: a lor-type focal cortical dysplasias. Neurology
mary central nervous system lymphoma and review of the recent literature. J Nucl Med 2012; 2010; 75:2168–2175
atypical glioblastoma: multiparametric differen- 53:59–71 101. Shin HW, Jewells V, Sheikh A, et al. Initial experi-
tiation by using diffusion-, perfusion-, and sus- 88. Martin-Macintosh EL, Broski SM, John- ence in hybrid PET-MRI for evaluation of refrac-
ceptibility-weighted MR imaging. Radiology son GB, Hunt CH, Cullen EL, Peller PJ. Multimo- tory focal onset epilepsy. Seizure 2015; 31:1–4
2014; 272:843–850 dality imaging of neurodegenerative processes. 102. Ding YS, Chen BB, Glielmi C, Friedman K,
75. Wray R, Solnes L, Mena E, Meoded A, Subrama- Part 1. The basics and common dementias. AJR Devinsky O. A pilot study in epilepsy patients us-
niam RM. 18F-flourodeoxy-glucose PET/comput- 2016; 207:871–882 ing simultaneous PET/MR. Am J Nucl Med Mol
ed tomography in brain tumors: value to patient 89. Brown RK, Bohnen NI, Wong KK, Minoshima S, Imaging 2014; 4:459–470
management and survival outcomes. PET Clin Frey KA. Brain PET in suspected dementia: pat- 103. Grouiller F, Delattre BM, Pittau F, et al. All-in-
2015; 10:423–430 terns of altered FDG metabolism. RadioGraphics one interictal presurgical imaging in patients
76. Lee SM, Goo JM, Park CM, et al. Preoperative 2014; 34:684–701 with epilepsy: single-session EEG/PET/(f)MRI.
staging of non-small cell lung cancer: prospec- 90. Johnson KA, Minoshima S, Bohnen NI, et Eur J Nucl Med Mol Imaging 2015; 42:1133–1143
tive comparison of PET/MR and PET/CT. Eur al. Appropriate use criteria for amyloid PET: a 104. Kransdorf MJ, Bridges MD. Current develop-
Radiol 2016; 26:3850–3857 report of the Amyloid Imaging Task Force, the ments and recent advances in musculoskeletal
77. Buchbender C, Heusner TA, Lauenstein TC, Society of Nuclear Medicine and Molecular Im- tumor imaging. Semin Musculoskelet Radiol
Bockisch A, Antoch G. Oncologic PET/MRI. Part aging, and the Alzheimer’s Association. Alzheim- 2013; 17:145–155
2. Bone tumors, soft-tissue tumors, melanoma, ers Dement 2013; 9:e1–e16 105. Kransdorf MJ, Murphey MD. Imaging of soft-
and lymphoma. J Nucl Med 2012; 53:1244–1252 91. Jack CR Jr, Albert MS, Knopman DS, et al. Intro- tissue musculoskeletal masses: fundamental con-
78. Szyszko TA, Cook GJR. PET/CT and PET/MRI duction to the recommendations from the National cepts. RadioGraphics 2016; 36:1931–1948
in head and neck malignancy. Clin Radiol 2018; Institute on Aging-Alzheimer’s Association work- 106. Manaster BJ. Soft-tissue masses: optimal imaging
73:60–69 groups on diagnostic guidelines for Alzheimer’s protocol and reporting. AJR 2013; 201:505–514
79. Huang SH, Chien CY, Lin WC, et al. A compara- disease. Alzheimers Dement 2011; 7:257–262 107. Ahlawat S, Fayad LM. Diffusion weighted imag-
tive study of fused FDG PET/MRI, PET/CT, 92. Schütz L, Lobsien D, Fritzsch D, et al. ing demystified: the technique and potential clin-
MRI, and CT imaging for assessing surrounding Feasibility and acceptance of simultaneous amy- ical applications for soft tissue imaging. Skeletal
tissue invasion of advanced buccal squamous cell loid PET/MRI. Eur J Nucl Med Mol Imaging Radiol 2018; 47:313–328
carcinoma. Clin Nucl Med 2011; 36:518–525 2016; 43:2236–2243 108. Fisher SM, Joodi R, Madhuranthakam AJ, Oz
AJR:211, August 2018 303
Broski et al.
OK, Sharma R, Chhabra A. Current utilities of SUVmax as an indicator of histopathologic re- fuse MR imaging pattern in patients with multi-
imaging in grading musculoskeletal soft tissue sponse after neoadjuvant chemotherapy in ex- ple myeloma. Radiology 2017; 282:484–493
sarcomas. Eur J Radiol 2016; 85:1336–1344 tremity osteosarcoma. Eur J Nucl Med Mol Im- 133. Messiou C, Collins DJ, Morgan VA, Bianchini D,
109. Zhang X, Chen YL, Lim R, Huang C, Chebib IA, aging 2013; 40:728–736 de Bono JS, de Souza NM. Use of apparent diffu-
El Fakhri G. Synergistic role of simultaneous 122. Hongtao L, Hui Z, Bingshun W, et al. 18F-FDG sion coefficient as a response biomarker in bone:
PET/MRI-MRS in soft tissue sarcoma metabo- positron emission tomography for the assessment effect of developing sclerosis on quantified val-
lism imaging. Magn Reson Imaging 2016; of histological response to neoadjuvant chemo- ues. Skeletal Radiol 2014; 43:205–208
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
34:276–279 therapy in osteosarcomas: a meta-analysis. Surg 134. Chantry A, Kazmi M, Barrington S, et al. Guide-
110. Vallières M, Freeman CR, Skamene SR, El Naqa Oncol 2012; 21:e165–e170 lines for the use of imaging in the management of
I. A radiomics model from joint FDG-PET and 123. Byun BH, Kong CB, Lim I, et al. Combination of patients with myeloma. Br J Haematol 2017;
MRI texture features for the prediction of lung 18F-FDG PET/CT and diffusion-weighted MR 178:380–393
metastases in soft-tissue sarcomas of the extremi- imaging as a predictor of histologic response to 135. Regelink JC, Minnema MC, Terpos E, et al.
ties. Phys Med Biol 2015; 60:5471–5496 neoadjuvant chemotherapy: preliminary results Comparison of modern and conventional imag-
111. Kubo T, Furuta T, Johan MP, Ochi M. Prognostic in osteosarcoma. J Nucl Med 2013; 54:1053–1059 ing techniques in establishing multiple myeloma-
significance of 18F-FDG PET at diagnosis in pa- 124. Schuler MK, Platzek I, Beuthien-Baumann B,
related bone disease: a systematic review. Br J
tients with soft tissue sarcoma and bone sarcoma; Fenchel M, Ehninger G, van den Hoff J. 18F-FDG Haematol 2013; 162:50–61
systematic review and meta-analysis. Eur J Can- PET/MRI for therapy response assessment in sar- 136. Giles SL, Messiou C, Collins DJ, et al. Whole-
cer 2016; 58:104–111 coma: comparison of PET and MR imaging re- body diffusion-weighted MR imaging for assess-
112. Li YJ, Dai YL, Cheng YS, Zhang WB, Tu CQ. sults. Clin Imaging 2015; 39:866–870 ment of treatment response in myeloma. Radiol-
Positron emission tomography 18F-fluorodeoxy- 125. Erfanian Y, Grueneisen J, Kirchner J, et al. Inte- ogy 2014; 271:785–794
glucose uptake and prognosis in patients with grated 18F-FDG PET/MRI compared to MRI 137. Messiou C, Collins DJ, Morgan VA, de Souza
bone and soft tissue sarcoma: a meta-analysis. alone for identification of local recurrences of NM. Optimising diffusion weighted MRI for im-
Eur J Surg Oncol 2016; 42:1103–1114 soft tissue sarcomas: a comparison trial. Eur J aging metastatic and myeloma bone disease and
113. Nanni C, Gasbarrini A, Cappelli A, et al. FDG Nucl Med Mol Imaging 2017; 44:1823–1831 assessing reproducibility. Eur Radiol 2011;
PET/CT for bone and soft-tissue biopsy. Eur J 126. Rajkumar SV, Dimopoulos MA, Palumbo A, et 21:1713–1718
Nucl Med Mol Imaging 2015; 42:1333–1334 al. International Myeloma Working Group up- 138. Caldarella C, Treglia G, Isgro MA, Treglia I, Gior-
114. Hain SF, O’Doherty MJ, BinghAm J, Chinyama dated criteria for the diagnosis of multiple my- dano A. The role of fluorine-18-fluorodeoxyglu-
C, Smith MA. Can FDG PET be used to success- eloma. Lancet Oncol 2014; 15:e538–e548 cose positron emission tomography in evaluating
fully direct preoperative biopsy of soft tissue tu- 127. Baur-Melnyk A, Buhmann S, Becker C, et al. the response to treatment in patients with multiple
mours? Nucl Med Commun 2003; 24:1139–1143 Whole-body MRI versus whole-body MDCT for myeloma. Int J Mol Imaging 2012; 2012:175803
115. Platzek I, Beuthien-Baumann B, Schramm G, et staging of multiple myeloma. AJR 2008; 139. Spinnato P, Bazzocchi A, Brioli A, et al. Contrast
al. FDG PET/MR in initial staging of sarcoma: 190:1097–1104 enhanced MRI and 18F-FDG PET-CT in the as-
initial experience and comparison with conven- 128. Zamagni E, Nanni C, Patriarca F, et al. A pro- sessment of multiple myeloma: a comparison of
tional imaging. Clin Imaging 2017; 42:126–132 spective comparison of 18F-fluorodeoxyglucose results in different phases of the disease. Eur J
116. Loft A, Jensen KE, Lofgren J, Daugaard S, Peters- positron emission tomography-computed tomog- Radiol 2012; 81:4013–4018
en MM. PET/MRI for preoperative planning in raphy, magnetic resonance imaging and whole- 140. Derlin T, Peldschus K, Munster S, et al. Compara-
patients with soft tissue sarcoma: a technical report body planar radiographs in the assessment of tive diagnostic performance of 18F-FDG PET/CT
of two patients. Case Rep Med 2013; 2013:791078 bone disease in newly diagnosed multiple my- versus whole-body MRI for determination of re-
117. Partovi S, Kohan AA, Zipp L, et al. Hybrid
eloma. Haematologica 2007; 92:50–55 mission status in multiple myeloma after stem cell
PET/MR imaging in two sarcoma patients: clini- 129. Waheed S, Mitchell A, Usmani S, et al. Standard transplantation. Eur Radiol 2013; 23:570–578
cal benefits and implications for future trials. Int and novel imaging methods for multiple myelo- 141. Shortt CP, Gleeson TG, Breen KA, et al. Whole-
J Clin Exp Med 2014; 7:640–648 ma: correlates with prognostic laboratory vari- body MRI versus PET in assessment of multiple
118. Schuler MK, Richter S, Beuthien-Baumann B, et ables including gene expression profiling data. myeloma disease activity. AJR 2009; 192:980–986
al. PET/MRI imaging in high-risk sarcoma: first Haematologica 2013; 98:71–78 142. Sachpekidis C, Hillengass J, Goldschmidt H, et
findings and solving clinical problems. Case Rep 130. Dutoit JC, Vanderkerken MA, Anthonissen J,
al. Comparison of 18F-FDG PET/CT and
Oncol Med 2013; 2013:793927 Dochy F, Verstraete KL. The diagnostic value of PET/MRI in patients with multiple myeloma.
119. Benz MR, Czernin J, Allen-Auerbach MS, et al. SE MRI and DWI of the spine in patients with Am J Nucl Med Mol Imaging 2015; 5:469–478
FDG-PET/CT imaging predicts histopathologic monoclonal gammopathy of undetermined sig- 143. Walker R, Barlogie B, Haessler J, et al. Magnetic
treatment responses after the initial cycle of neo- nificance, smouldering myeloma and multiple resonance imaging in multiple myeloma: diag-
adjuvant chemotherapy in high-grade soft-tissue myeloma. Eur Radiol 2014; 24:2754–2765 nostic and clinical implications. J Clin Oncol
sarcomas. Clin Cancer Res 2009; 15:2856–2863 131. Squillaci E, Bolacchi F, Altobelli S, et al. Pre- 2007; 25:1121–1128
120. Evilevitch V, Weber WA, Tap WD, et al. Reduc- treatment staging of multiple myeloma patients: 144. Siontis B, Kumar S, Dispenzieri A, et al. Positron
tion of glucose metabolic activity is more accu- comparison of whole-body diffusion weighted emission tomography-computed tomography in
rate than change in size at predicting histopatho- imaging with whole-body T1-weighted contrast- the diagnostic evaluation of smoldering multiple
logic response to neoadjuvant therapy in enhanced imaging. Acta Radiol 2015; 56:733–738 myeloma: identification of patients needing ther-
high-grade soft-tissue sarcomas. Clin Cancer Res 132. Koutoulidis V, Fontara S, Terpos E, et al. Quanti- apy. Blood Cancer J 2015; 5:e364
2008; 14:715–720 tative diffusion-weighted imaging of the bone 145. Zamagni E, Nanni C, Gay F, et al. 18F-FDG
121. Kong CB, Byun BH, Lim I, et al. 18F-FDG PET marrow: an adjunct tool for the diagnosis of a dif- PET/CT focal, but not osteolytic, lesions predict
304 AJR:211, August 2018
Update on Clinical PET/MRI
the progression of smoldering myeloma to active PET in simultaneous PET-MR imaging. PET sarcoid detection and therapy monitoring. J Nucl
disease. Leukemia 2016; 30:417–422 Clin 2017; 12:321–327 Cardiol 2017; 24:1741–1758
146. Abgral R, Dweck MR, Trivieri MG, et al. Clini- 152. Hanneman K, Kadoch M, Guo HH, et al. Initial 156. Lapa C, Reiter T, Kircher M, et al. Somatostatin
cal utility of combined FDG-PET/MR to assess experience with simultaneous 18F-FDG PET/MRI receptor based PET/CT in patients with the suspi-
myocardial disease. JACC Cardiovasc Imaging in the evaluation of cardiac sarcoidosis and myo- cion of cardiac sarcoidosis: an initial comparison
2017; 10:594–597 carditis. Clin Nucl Med 2017; 42:e328–e334 to cardiac MRI. Oncotarget 2016; 7:77807–77814
147. LaForest R, Woodard PK, Gropler RJ. Cardiovas- 153. Slart RHJA, Glaudemans AWJM, Lancellotti P,
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
157. Gillmore JD, Maurer MS, Falk RH, et al. Nonbi-
cular PET/MRI: challenges and opportunities. et al. A joint procedural position statement on im- opsy diagnosis of cardiac transthyretin amyloido-
Cardiol Clin 2016; 34:25–35 aging in cardiac sarcoidosis: from the Cardiovas- sis. Circulation 2016; 133:2404–2412
148. Munoz C, Neji R, Cruz G, et al. Motion-corrected cular and Inflammation & Infection Committees 158. Trivieri MG, Dweck MR, Abgral R, et al. F-
simultaneous cardiac positron emission tomography of the European Association of Nuclear Medi- 18-sodium fluoride PET/MR for the assessment
and coronary MR angiography with high acquisition cine, the European Association of Cardiovascular of cardiac amyloidosis. J Am Coll Cardiol 2016;
efficiency. Magn Reson Med 2018; 79:339–350 Imaging, and the American Society of Nuclear 68:2712–2714
149. Küstner T, Schwartz M, Martirosian P, et al. MR- Cardiology. J Nucl Cardiol 2018; 25:298–319 159. Osborne DR, Acuff SN, Stuckey A, Wall JS. A
based respiratory and cardiac motion correction for 154. Dweck MR, Abgral R, Trivieri MG, et al. Hybrid routine PET/CT protocol with streamlined calcu-
PET imaging. Med Image Anal 2017; 42:129–144 magnetic resonance imaging and positron emis- lations for assessing cardiac amyloidosis using
150. Wang X, Rahmim A, Tang J. MRI-assisted dual sion tomography with fluorodeoxyglucose to di- 18F-florbetapir. Front Cardiovasc Med 2015; 2:23
motion correction for myocardial perfusion de- agnose active cardiac sarcoidosis. JACC Cardio- 160. Grant AM, Deller TW, Khalighi MM, Maramra-
fect detection in PET imaging. Med Phys 2017; vasc Imaging 2018; 11:94–107 ju SH, Delso G, Levin CS. NEMA NU 2-2012
44:4536–4547 155. Chareonthaitawee P, Beanlands RS, Chen W, et performance studies for the SiPM-based ToF-
151. Rakvongthai Y, El Fakhri G. Magnetic reso-
al. Joint SNMMI-ASNC expert consensus docu- PET component of the GE SIGNA PET/MR sys-
nance-based motion correction for quantitative ment on the role of 18F-FDG PET/CT in cardiac tem. Med Phys 2016; 43:2334–2343
A B C D E F
Fig. 1—Patient undergoing FDG PET/MRI study.
A–F, Coronal in-phase (A), water (B), and fat (C) images are used to generate attenuation correction map (D), which is then used in attenuation correction of PET data
(FDG PET image, E; fused PET/MR image, F). Regions containing head, lung, abdomen, and pelvis are identified during acquisition setup to prescribe head versus body
attenuation correction modes and to assist segmentation of Dixon sequence images into various tissue classes. Note that there is no bone component in body and that
head portion of attenuation correction map (D) consists of atlas and head and neck coil.
AJR:211, August 2018 305
Broski et al.
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
A B C
D E F
Fig. 2—48-year-old man with newly diagnosed
pancreatoblastoma.
A–F, On MRI component of FDG PET/MRI, lesion was
well-circumscribed, lobulated, and T2 hyperintense
(arrow, A); showed progressive enhancement on
arterial (B), venous (C), and delayed (D) dynamic
contrast-enhanced images (arrows); and no diffusion
restriction (arrows) on DW image (E) and apparent
diffusion coefficient map (F), which are imaging
characteristics typical of hepatic hemangioma.
G and H, On PET component, however, hepatic lesion
(arrow, G) showed intense uptake, similar to that of
primary lesion (arrowhead, H). According to these
findings, liver lesion was reported to be of metastatic
cause, which was confirmed on hepatic wedge biopsy.
G H
Fig. 3—41-year-old woman with metastatic pancreatic neuroendocrine tumor undergoing staging
68 Ga-DOTATATE PET/MRI.
A–E, PET maximum intensity projection image (A) shows multiple hepatic metastases (circle) and right second
rib metastasis (arrowhead). Axial T2-weighted fat-saturated MRI (B) of liver shows no T2-hyperintense
hepatic metastases. However, DW image shows focus of restricted diffusion in right hepatic lobe (arrow,
C), with corresponding hypointensity on hepatobiliary phase contrast-enhanced image (arrow, D) and
DOTATATE uptake on fused PET/MR image (arrow, E), consistent with neuroendocrine hepatic metastasis.
Neuroendocrine tumor in pancreatic tail also shows intense DOTATATE uptake (solid arrowhead, E), and there
were DOTATATE-avid locoregional lymph node metastases (dashed arrowhead, E).
(Fig. 3 continues on next page)
A
306 AJR:211, August 2018
Update on Clinical PET/MRI
Fig. 3 (continued)—41-year-old woman with
metastatic pancreatic neuroendocrine tumor
undergoing staging 68Ga-DOTATATE PET/MRI.
A–E, PET maximum intensity projection image (A)
shows multiple hepatic metastases (circle) and
right second rib metastasis (arrowhead). Axial
T2-weighted fat-saturated MRI (B) of liver shows
no T2-hyperintense hepatic metastases. However,
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
DW image shows focus of restricted diffusion in
right hepatic lobe (arrow, C), with corresponding
hypointensity on hepatobiliary phase contrast-
enhanced image (arrow, D) and DOTATATE uptake
on fused PET/MR image (arrow, E), consistent with
neuroendocrine hepatic metastasis. Neuroendocrine
tumor in pancreatic tail also shows intense B C
DOTATATE uptake (solid arrowhead, E), and there
were DOTATATE-avid locoregional lymph node
metastases (dashed arrowhead, E).
D E
Fig. 4—71-year-old man with prostate carcinoma who underwent radical prostatectomy and radiation therapy
and later presented with slowly increasing prostate-specific antigen level, currently 0.8 ng/mL.
A–E, Carbon-11-choline PET/MRI maximum intensity projection image (A), T2-weighted MR images (B and D),
and fused PET/MR images (C and E) show choline-avid left seminal vesicle recurrence (circle, A; ovals, B and C)
and metastatic left internal iliac node (arrows, A, D, and E).
(Fig. 4 continues on next page)
A
AJR:211, August 2018 307
Broski et al.
Fig. 4 (continued)—71-year-old man with prostate
carcinoma who underwent radical prostatectomy
and radiation therapy and later presented with slowly
increasing prostate-specific antigen level, currently
0.8 ng/mL.
A–E, Carbon-11-choline PET/MR maximum intensity
projection image (A), T2-weighted MR images (B
and D), and fused PET/MR images (C and E) show
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
choline-avid left seminal vesicle recurrence (circle,
A; ovals, B and C) and metastatic left internal iliac
node (arrows, A, D, and E).
B C
D E
308 AJR:211, August 2018
Update on Clinical PET/MRI
Fig. 5—67-year-old man with primary CNS lymphoma undergoing restaging after chemotherapy.
A–F, FDG PET maximum intensity projection image (A) shows intense foci of intracranial activity, but no
evidence of systemic disease. PET/MR images show infiltrative lesion involving splenium of corpus callosum
with increased signal on T2-weighted FLAIR image (arrows, B), diffusion restriction with high signal on DW
image (arrows, C), low signal on apparent diffusion coefficient image (arrows, D), and intense FDG activity on
PET image (arrows, E) and fused PET/MR image (arrows, F). Fused PET/MRI examination enabled full diagnostic
brain MRI and torso PET in single session.
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
A B C
D E F
AJR:211, August 2018 309
Broski et al.
Fig. 6—61-year-old woman with right perihilar
pulmonary adenocarcinoma.
A–D, FDG PET/MRI maximum intensity projection
(A), PET (B), contrast-enhanced T1-weighted fat-
saturated (C), and fused PET/MR (D) images show
large FDG-avid pulmonary mass (arrowhead, A)
and small enhancing metastases in left cerebellar
hemisphere (arrows, B–D). Integrated PET/MRI
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
allowed complete staging in single session.
A B
C D
Fig. 7—33-year-old man with 10 years of nocturnal
general tonic-clonic seizures.
A–D, Initial MRI (A) was interpreted as negative.
Coronal 3D T1-weighted (B) and coronal FLAIR (C)
images are also shown. Subsequent interictal FDG
PET/MRI (D) shows hypometabolism throughout
anterior left temporal lobe (ovals, C and D). Placement
of left temporal grid confirmed seizure focus and
patient has been seizure-free since left temporal
resection.
(Fig. 7 continues on next page)
A B
310 AJR:211, August 2018
Update on Clinical PET/MRI
Fig. 7 (continued)—33-year-old man with 10 years of
nocturnal general tonic-clonic seizures.
A–D, Initial MRI (A) was interpreted as negative.
Coronal 3D T1-weighted (B) and coronal FLAIR (C)
images are also shown. Subsequent interictal FDG
PET/MRI (D) shows hypometabolism throughout
anterior left temporal lobe (ovals, C and D). Placement
of left temporal grid confirmed seizure focus and
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
patient has been seizure-free since left temporal
resection.
C D
Fig. 8—27-year-old woman undergoing staging FDG PET/MRI for pelvic sarcoma.
A–E, FDG PET maximum intensity projection image shows increased uptake in right pelvis (arrow, A) and no
evidence of regional or distant metastatic disease. Axial (B and C) and coronal (D and E) T2-weighted fat-
saturated (B and D) and fused PET/MR images (C and E) show locally advanced T2-hyperintense mass involving
right sacrum and ilium, with soft component. Note increased FDG activity in extraosseous component (arrows,
B–E). FDG-avid extraosseous component was subsequently targeted for biopsy, with pathologic analysis
showing chondroblastic osteosarcoma.
B C
A D E
AJR:211, August 2018 311
Broski et al.
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
A B C D
Fig. 9—54-year-old woman with multiple myeloma undergoing staging FDG PET/MRI.
A–D, Coronal (top) and sagittal (bottom) PET (A), STIR (B), and fused PET/STIR (C) images of spine and pelvis show diffuse T2-hyperintense marrow infiltration,
consistent with diffuse involvement by multiple myeloma, but no significantly increased FDG activity. PET maximum intensity projection image (D) shows relatively
normal FDG biodistribution, with exception of healing right rib fracture (arrow). Subsequent bone marrow biopsy showed involvement by 80–90% clonal plasma cells.
312 AJR:211, August 2018
Update on Clinical PET/MRI
Downloaded from www.ajronline.org by 152.32.99.177 on 11/01/20 from IP address 152.32.99.177. Copyright ARRS. For personal use only; all rights reserved
A B C
D E F
Fig. 10—Two patients with myeloma.
A and B, 43-year-old woman with myeloma undergoing restaging FDG PET/MRI after chemotherapy. Axial T1-weighted MR image (A) shows rounded T1-hypointense
marrow-replacing lesion in posterior right iliac bone (arrow). Corresponding fused T1-weighted fused PET/MR image (B) shows no FDG activity within lesion (arrow),
consistent with successfully treated lesion showing decreased FDG activity before normalized MRI signal.
C–F, 60-year-old man with history of multiple myeloma who underwent chemotherapy and had laboratory evidence of relapse. Restaging whole-body low-dose CT shows
subtle area of soft-tissue density in proximal left femoral shaft (arrow, C), without corresponding osteolysis (arrow, D). Subsequent FDG PET/MRI shows T1-hypointense
marrow-replacing lesion in same location (arrow, E) with increased FDG activity seen on fused PET/MR image (arrow, F), consistent with active disease.
F O R YO U R I N F O R M AT I O N
A data supplement for this article can be viewed in the online version of the article at: www.ajronline.org.
AJR:211, August 2018 313
You might also like
- 1066UE 2023-01 RANDOX Level 3Document92 pages1066UE 2023-01 RANDOX Level 3Dharmesh PatelNo ratings yet
- Best New Flaps and Tips For Success in MicrosurgeryDocument12 pagesBest New Flaps and Tips For Success in MicrosurgeryDwi WicaksonoNo ratings yet
- Effect of Hyperbaric Oxygen Therapy On Chronic Neurocognitive Deficits of Post-Traumatic Brain Injury Patients: Retrospective AnalysisDocument9 pagesEffect of Hyperbaric Oxygen Therapy On Chronic Neurocognitive Deficits of Post-Traumatic Brain Injury Patients: Retrospective AnalysisVinnie Juliana YonatanNo ratings yet
- Fusion 9.2.3.1 PDFDocument6 pagesFusion 9.2.3.1 PDFGowri ShankarNo ratings yet
- AJRAmJRoentgenol 2013Aug2012W206-14Document10 pagesAJRAmJRoentgenol 2013Aug2012W206-14asdfghjm.,nmnbvcxNo ratings yet
- Photobiomodulation in Endodontic, Restorative, and Prosthetic Dentistry: A Review of The LiteratureDocument18 pagesPhotobiomodulation in Endodontic, Restorative, and Prosthetic Dentistry: A Review of The LiteratureAbhishek NaikNo ratings yet
- Photobiomodulation in Endodontic, Restorative, and Prosthetic Dentistry: A Review of The LiteratureDocument18 pagesPhotobiomodulation in Endodontic, Restorative, and Prosthetic Dentistry: A Review of The LiteratureAbhishek NaikNo ratings yet
- Ceor 306138 Ultrasound Guided Pudendal Nerve Block in Patients UndergoinDocument8 pagesCeor 306138 Ultrasound Guided Pudendal Nerve Block in Patients UndergoinImdaad MownahNo ratings yet
- Lens Dose in Routine Head CTDocument8 pagesLens Dose in Routine Head CTAglaia T.No ratings yet
- Korea RTWDocument11 pagesKorea RTWLisa NurhasanahNo ratings yet
- Boom or Bust in OTDocument4 pagesBoom or Bust in OTSusan Ly VillalobosNo ratings yet
- Pickhardt 2020 Positive Oral Contrast Material For Abdominal CT Current Clinical Indications and Areas of ControversyDocument10 pagesPickhardt 2020 Positive Oral Contrast Material For Abdominal CT Current Clinical Indications and Areas of ControversyLucas ParretNo ratings yet
- Ot Dis Tribut E: Spectroscopic Sensing of Cancer and Cancer TherapyDocument9 pagesOt Dis Tribut E: Spectroscopic Sensing of Cancer and Cancer TherapyYerly Ramirez MuñozNo ratings yet
- Science, Medicine, and The Future: Functional Magnetic Resonance Imaging in NeuropsychiatryDocument5 pagesScience, Medicine, and The Future: Functional Magnetic Resonance Imaging in NeuropsychiatryVania RafeliaNo ratings yet
- MRI Safety Update 2008: Part 1, MRI Contrast Agents and Nephrogenic Systemic FibrosisDocument11 pagesMRI Safety Update 2008: Part 1, MRI Contrast Agents and Nephrogenic Systemic FibrosisDvina AudreyNo ratings yet
- 02-MARTINS 2020-Post - Operative - Pain - After - Using - Sodium.18Document8 pages02-MARTINS 2020-Post - Operative - Pain - After - Using - Sodium.18julio.bragaNo ratings yet
- The Performance of Compartmental And.20Document12 pagesThe Performance of Compartmental And.20Joanna GlezNo ratings yet
- Jospt.2008.2725 A Primer On Selected Aspects of EBP Relating To Questions of Treatment IIDocument17 pagesJospt.2008.2725 A Primer On Selected Aspects of EBP Relating To Questions of Treatment IIShilpika DhuriNo ratings yet
- 600 FullDocument18 pages600 Fulleric22hkNo ratings yet
- 21 - Piriformis SyndromeDocument11 pages21 - Piriformis SyndromewatiNo ratings yet
- Biomarkers, Screening and EthicsDocument4 pagesBiomarkers, Screening and Ethicsarif_amininNo ratings yet
- Botulinum Toxin in The Management of Children With Cerebral PalsyDocument21 pagesBotulinum Toxin in The Management of Children With Cerebral PalsyPolet OligNo ratings yet
- Systematic Review of Orthodontic Treatment ManagementDocument7 pagesSystematic Review of Orthodontic Treatment ManagementJuan AndradeNo ratings yet
- Physiotherapy After Traumatic Brain Injury: A Systematic Review of The LiteratureDocument9 pagesPhysiotherapy After Traumatic Brain Injury: A Systematic Review of The LiteratureVeronika AtaNo ratings yet
- Oral Health Related Quality of Life in Sur 2017 American Journal of OrthodonDocument2 pagesOral Health Related Quality of Life in Sur 2017 American Journal of Orthodondruzair007No ratings yet
- Tympanoplasty - News and New PerspectivesDocument21 pagesTympanoplasty - News and New PerspectivesMonik AlamandaNo ratings yet
- BMC Neuroscience: Requirements For A Lead Compound To Become A Clinical CandidateDocument7 pagesBMC Neuroscience: Requirements For A Lead Compound To Become A Clinical CandidatedasdeeNo ratings yet
- What The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyDocument8 pagesWhat The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyQonita Aizati QomaruddinNo ratings yet
- Clinical Protocol For Managing Acute Disc Displacement Without Reduction: A Magnetic Resonance Imaging EvaluationDocument8 pagesClinical Protocol For Managing Acute Disc Displacement Without Reduction: A Magnetic Resonance Imaging EvaluationAndhi DavidNo ratings yet
- Abstract 73748 2018111218314Document6 pagesAbstract 73748 2018111218314Yang LiuNo ratings yet
- Emerging Trends in Botulinum Neurotoxin A Resistance - An International Multidisciplinary Review and Consensus - Ho, 2022Document11 pagesEmerging Trends in Botulinum Neurotoxin A Resistance - An International Multidisciplinary Review and Consensus - Ho, 2022Rafael Autran Cavalcante AraújoNo ratings yet
- E030146 FullDocument7 pagesE030146 FullAURORA BADIALINo ratings yet
- 2022 BMJ Open - Models of Care For Low Back PainDocument7 pages2022 BMJ Open - Models of Care For Low Back PainMiguel Arévalo-CárdenasNo ratings yet
- Corticoterapia Na PACDocument15 pagesCorticoterapia Na PACksdposaNo ratings yet
- E000391 FullDocument10 pagesE000391 FullcogajoNo ratings yet
- Management of Acute Ischemic Stroke.13Document10 pagesManagement of Acute Ischemic Stroke.13Juan fernando Torres pavaNo ratings yet
- 2024 Focused Update Guidelines On Use Of.275Document15 pages2024 Focused Update Guidelines On Use Of.275Luis ReyesNo ratings yet
- Biomechanical Basis For Stability: Explanation To Enhance Clinical-UtilityDocument8 pagesBiomechanical Basis For Stability: Explanation To Enhance Clinical-UtilityADAMNo ratings yet
- Physical Rehabilitation in The ICU A Systematic.3Document14 pagesPhysical Rehabilitation in The ICU A Systematic.3Alan Calderón BerrioNo ratings yet
- Polymers 14 02751Document24 pagesPolymers 14 02751nader zirakNo ratings yet
- The Safety of Orthokeratology-A Systematic ReviewDocument8 pagesThe Safety of Orthokeratology-A Systematic ReviewBAYUNo ratings yet
- Medical Physics in The Future: SpectDocument5 pagesMedical Physics in The Future: SpectTsetsaNo ratings yet
- 논문원문Document10 pages논문원문Donghee LeeNo ratings yet
- Perioperative ERAS Approach Defining The Role of Desflurane - Slide Deck FinalDocument69 pagesPerioperative ERAS Approach Defining The Role of Desflurane - Slide Deck FinalHelmiHassanNo ratings yet
- Review-2015-Interactomics-toward Protein Function and RegulationDocument24 pagesReview-2015-Interactomics-toward Protein Function and Regulationcarlos ArozamenaNo ratings yet
- Agenda at A Glance PDF 1012Document4 pagesAgenda at A Glance PDF 1012Amit MalviyaNo ratings yet
- 2024 Focused Update Guidelines On Use Of.275Document15 pages2024 Focused Update Guidelines On Use Of.275nhunhuochachNo ratings yet
- Impairment-Based Rehabilitation Following Hip Arthroscopy: Postoperative Protocol For The Hip Arthroscopy International Randomized Controlled TrialDocument26 pagesImpairment-Based Rehabilitation Following Hip Arthroscopy: Postoperative Protocol For The Hip Arthroscopy International Randomized Controlled TrialFer NandoNo ratings yet
- Delatorrecanales 2019Document11 pagesDelatorrecanales 2019ELIAS DAVID NOBMAN ALVARADONo ratings yet
- Synopsis Levobupivacaine NewDocument10 pagesSynopsis Levobupivacaine NewsagarNo ratings yet
- Ijaem40005hospitals Now and BeforeDocument6 pagesIjaem40005hospitals Now and BeforeAntonette RayanNo ratings yet
- New SPECT and PET Radiopharmaceuticals For Imaging CardiovascularDocument26 pagesNew SPECT and PET Radiopharmaceuticals For Imaging CardiovascularKarnVimolvattanasarnNo ratings yet
- Misch S Contemporary Implant Dentistry.4Document2 pagesMisch S Contemporary Implant Dentistry.4Dadi SindhuNo ratings yet
- Cuts Poster JB Cfs 2Document1 pageCuts Poster JB Cfs 2api-465519286No ratings yet
- Abstract P29 A Novel Surgical Approach To The.212Document1 pageAbstract P29 A Novel Surgical Approach To The.212Ana HidalgoNo ratings yet
- Yang 2019Document6 pagesYang 2019KevinNo ratings yet
- FiltrationDocument16 pagesFiltrationjojokawayNo ratings yet
- TOPICAL REVIEW Progress in Applications of MagnetiDocument16 pagesTOPICAL REVIEW Progress in Applications of MagnetiSong BeeNo ratings yet
- Optic Neuritis.6Document29 pagesOptic Neuritis.6Juliana Valentina CedeñoNo ratings yet
- PET MRI Emerging Clinical Applications in OncologyDocument17 pagesPET MRI Emerging Clinical Applications in Oncologyalfred benedict bayanNo ratings yet
- PET MRI Vs PET CT in Oncology, Management and CostDocument10 pagesPET MRI Vs PET CT in Oncology, Management and Costalfred benedict bayanNo ratings yet
- Nuclear Medicine in The Philippines 2016Document6 pagesNuclear Medicine in The Philippines 2016alfred benedict bayanNo ratings yet
- PET in Neurological DisordersDocument12 pagesPET in Neurological Disordersalfred benedict bayanNo ratings yet
- Globocan 2020Document2 pagesGlobocan 2020alfred benedict bayanNo ratings yet
- Financial Ratios Are Mathematical Comparisons of Financial Statement Accounts or CategoriesDocument5 pagesFinancial Ratios Are Mathematical Comparisons of Financial Statement Accounts or Categoriesalfred benedict bayanNo ratings yet
- Dementia Asia Pacific 2014Document64 pagesDementia Asia Pacific 2014alfred benedict bayanNo ratings yet
- Doctrine of Res Ipsa LoquiturDocument3 pagesDoctrine of Res Ipsa Loquituralfred benedict bayanNo ratings yet
- Doctrine of Ostensible AgencyDocument2 pagesDoctrine of Ostensible Agencyalfred benedict bayanNo ratings yet
- LWT - Food Science and Technology: A A A A B BDocument8 pagesLWT - Food Science and Technology: A A A A B BMarton FruzsinaNo ratings yet
- Physiology AssignmentDocument4 pagesPhysiology Assignmentmaha khanNo ratings yet
- Rad 97Document188 pagesRad 97Ahmed BadranNo ratings yet
- Catch Up Fridays Lesson PlanDocument2 pagesCatch Up Fridays Lesson PlanJedison IlocsoNo ratings yet
- The New Integrated Pest Management Paradigm For The Modern AgeDocument9 pagesThe New Integrated Pest Management Paradigm For The Modern AgeRómulo Del ValleNo ratings yet
- Thesis StatementDocument15 pagesThesis StatementJos50% (2)
- Corelation of The Changes Between The Iridocorneal - Angle and Other Paramet E Rs at The Neovascular GlaucomaDocument25 pagesCorelation of The Changes Between The Iridocorneal - Angle and Other Paramet E Rs at The Neovascular GlaucomaAJVAZI100% (1)
- Dust Collector DesignDocument13 pagesDust Collector DesignAekJay50% (2)
- Pharmaceutical Sciences: Assessment of Vitamin B-12 Deficiency in Type-Ii Diabetics Using MetforminDocument5 pagesPharmaceutical Sciences: Assessment of Vitamin B-12 Deficiency in Type-Ii Diabetics Using MetforminMuhammad ZubairNo ratings yet
- Chapter 5 - The Research DesignDocument14 pagesChapter 5 - The Research DesignmarlianaNo ratings yet
- CECS ProtocolDocument6 pagesCECS ProtocolTsz Kwan CheungNo ratings yet
- From Dysthymia To Treatment-Resistant Depression: Evolution of A Psychopathological ConstructDocument7 pagesFrom Dysthymia To Treatment-Resistant Depression: Evolution of A Psychopathological ConstructApenasNo ratings yet
- PosterDocument1 pagePostermacNo ratings yet
- CervicothoracicSpine AssessmentDocument16 pagesCervicothoracicSpine AssessmentKanika SinhaNo ratings yet
- Weight Bearing As Tolerated: Knee Replacement Exercise BookletDocument33 pagesWeight Bearing As Tolerated: Knee Replacement Exercise BookletRAGHAVNo ratings yet
- HIIT Exercises ListDocument8 pagesHIIT Exercises ListJeanNo ratings yet
- Health-Preneurship: Why Does Public Health Need An Entrepreneur?Document11 pagesHealth-Preneurship: Why Does Public Health Need An Entrepreneur?LipatriNo ratings yet
- Manual Handling: Safe Work Practice Safe Work PracticeDocument4 pagesManual Handling: Safe Work Practice Safe Work PracticegouthamreddysNo ratings yet
- Axis III GMCDocument4 pagesAxis III GMCFasya GhaffarNo ratings yet
- Functioning in Schizophrenia: Comparison Between Six Health ProfessionsDocument1 pageFunctioning in Schizophrenia: Comparison Between Six Health ProfessionsMaite BarriosNo ratings yet
- Yash N Archi Critisis AnalysisDocument5 pagesYash N Archi Critisis AnalysisArchita DuttaNo ratings yet
- MTP 20 WeeksDocument4 pagesMTP 20 WeeksSurya S PNo ratings yet
- Assignment Interview LEADERSHIPDocument13 pagesAssignment Interview LEADERSHIPsjamilmdfauzieNo ratings yet
- Janson Medical Clinic: A Case Study in Quality ImprovementDocument7 pagesJanson Medical Clinic: A Case Study in Quality ImprovementAira Genille YaochingNo ratings yet
- Learn Fron MCQ Mba Net - Copy 1Document64 pagesLearn Fron MCQ Mba Net - Copy 1santosh kumarNo ratings yet
- Barang Ed DekatDocument12 pagesBarang Ed DekatAkhmad “Billy Rafi” HambaliNo ratings yet
- Ketones &ketone Urine Test - Purpose, Procedure, ResutlsDocument6 pagesKetones &ketone Urine Test - Purpose, Procedure, ResutlsEiann Jasper LongcayanaNo ratings yet
- Field Guide To Designing Health Comm Strategy 131 147Document17 pagesField Guide To Designing Health Comm Strategy 131 147yemimaNo ratings yet
- Aditek Catalogue Ed.04 - EnglishDocument64 pagesAditek Catalogue Ed.04 - EnglishhabeebNo ratings yet