Professional Documents
Culture Documents
ABSA2020 Covid 19 Dr3
ABSA2020 Covid 19 Dr3
Uploaded by
Wisiva Tofriska P.0 ratings0% found this document useful (0 votes)
7 views1 pageCopyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views1 pageABSA2020 Covid 19 Dr3
ABSA2020 Covid 19 Dr3
Uploaded by
Wisiva Tofriska P.Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
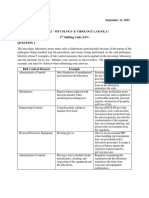
The Association for Biosafety and Biosecurity
Considerations for Handling Potential SARS-CoV-2 Samples
Bench work BSL2 BSL2 with BSL3 practices BSL3
• Whole blood, serum and urine • Using automated instruments and analyzers (if aerosol containment • practices
Aliquoting and/or diluting specimens Virus isolation in cell culture and initial
• Rapid respiratory testing performed is a feature) some devices might be older and not contained • Inoculating bacterial or mycological culture media characterization of viral agents recovered in
at the point of care (no nucleic acid • Staining and microscopic analysis of fixed smears • Performing diagnostic tests that do not involve propagation of viral cultures of SARS-CoV-2 specimens
isolation) • Examination of bacterial cultures agents in vitro or in vivo
• Pathologic examination and processing of formalin-fixed or • Nucleic acid extraction procedures involving potentially infected
Additional procedures
Laboratory Practices and • FACS/High Speed Cell Sorting
Technique otherwise inactivated tissues specimens
– Inactivation methods should be validated • Preparation and chemical- or heat-fixing of smears for microscopic • Transfer of inactivated samples
• Good (Standard) Microbiological outside BSL3
• Molecular analysis of extracted nucleic acid preparations analysis
Practices
• Final packaging of specimens for transport to diagnostic laborato- * CDC Source • Inactivation by validated methods
Primary Barriers and Personal ries for additional testing
Protective Equipment (PPE) • Specimens should already be in a sealed, decontaminated primary
Additional procedures Laboratory Practices and Technique
container • Respiratory samples and secretions • Good (Standard) Microbiological Practices
• PPE: lab coat, single gloves, surgical
• Stool*** – Follow BSL3 practices and procedures
mask, eye protection, face shield • Using inactivated specimens, such as specimens in
• Cytometry – non-fixed samples according to CDC BMBL 5th ed.
• Work behind plexiglass screen in an • Nucleic acid extraction buffer
• Inactivated virus lysate • Laboratory personnel must receive
isolated designated area (minimum) • Performing electron microscopic studies with glutaraldehyde- fixed
• Work with ANY sample that may produce an aerosol specific training in handling pathogenic
• Notify others in the lab grids and poten-tially lethal agents and must be
• Work with samples done over a * CDC Source supervised by scientists competent in
plastic-backed benchtop pad
Additional procedures Laboratory Practices and Technique handling infec-tious agents and associated
• Surface decontamination at every procedures.
step using EPA List N disinfectants • Cytometry – fixed samples • Good (Standard) Microbiological Practices
and contact times. • Primary & Secondary Barriers and PPE
Laboratory Practices and Technique Primary & Secondary Barriers
• Potentially infectious materials must • PPE: surgical mask (blood)/N-95 (respiratory secretions), double and PPE
be placed in a durable, leak proof • Good (Standard) Microbiological Practices
gloves, impervious gown, eye protection with side shields • All procedures involving the manipulation
container during collection, handling, • Access to the laboratory is restricted when work is being conducted
processing, storage, or transport • All procedures in which infectious aerosols or splashes may be • All samples opened inside the BSC in case of spills/leakage. If BSC of infectious materials must be conducted
within a facility. created are conducted in BSCs or other physical containment is not available, don N95 and face shield and work behind plexi-glass within a BSC, or other physical contain-
equipment. screen in an isolated designated area, notify other laboratori-ans, ment devices.
Administrative Controls: work with samples done over a plastic-backed benchtop pad • Respiratory protection is required (N95 or
• Use safety cups whenever possible to avoid exposure to aerosols. • Surface decontamination at every step using EPA List N disinfec- PAPR/CAPR)
Training and competency verification
on donning and doffing required PPE tants and contact times.
Primary & Secondary Barriers and PPE • Autoclave waste before disposal
* CDC Guidance for Laboratory https:// Administrative Controls: • Facility exhaust system must have HEPA
• PPE: surgical mask, single gloves, gown/lab coat, eye protection
www.cdc.gov/coronavirus/2019-nCoV/ filtration**
lab/lab-biosafe-ty-guidelines.html • BSCs, if available, are properly maintained and certified • Scheduled time for handling SARS-CoV-2 samples (best practice)
** WHO Laboratory Guidance https:// • Mechanical ventilation systems that provide an inward flow of air • Two-person rule for minimizing withdrawing hands from BSC Transfer of samples outside BSL3-
apps.who.int/iris/bitstream/ without recirculation to spaces outside of the laboratory based on risk assessment by
• Centrifuging of blood specimens is in safety cups or sealed rotor,
handle/10665/331138/WHO-WPE- biosafety officer
• A method for decontaminating all laboratory wastes should be loaded and unloaded in a BSC
GIH-2020.1-eng.pdf • Ensure lids are tight
available in the facility • Training and competency verification on donning and doffing
*** The Lancet https:// required PPE • Decontaminate outside of tubes
www.thelancet.com/journals/langas/ Administrative Controls: Wrap sample with absorbent material
• Specific training on use of N95 respirators, if applicable •
article/ • Training and competency verification for each procedure (includes pulmonary function, medical clearance, and fit testing)
PIIS2468-1253(20)30089-3/fulltext • Individually place into zip-lock bag
performed
These considerations do not supersede • Laboratory personnel have specific training in handling pathogenic • Seal zip-lock bag and change gloves
any regulatory or country-specific agents and are supervised by scientists competent in handling • Add all wrapped samples into second bag
requirements in your locale. infectious agents and associated procedures • Wrap bagged samples in ample packaging
• Occupational health and place into designated carrier, firmly
-mandatory reporting of any symptoms, any laboratory exposure attach lid
Laboratory practices, techniques, and
administrative controls build upon the -consider baseline blood, baseline questionnaire, emergency wallet
previous level. Additional controls are card
indicated at each level. • Demonstrated competency on working in a BSC (if available)
Last revision 4/13/2020 • Prepared by ABSA International Emerging Infectious Diseases Consortium • Please direct inquiries to info@absa.org
You might also like
- Handbook On The Participation of The CSO in The Local Budget ProcessDocument44 pagesHandbook On The Participation of The CSO in The Local Budget ProcessDBM CALABARZON93% (14)
- 3 2 Solving Quadratic Equations by GraphingDocument76 pages3 2 Solving Quadratic Equations by GraphingHasan Eser100% (1)
- CAP Accreditation Checklists - 2021 Edition: Checklists Subdisciplines Description of ContentsDocument7 pagesCAP Accreditation Checklists - 2021 Edition: Checklists Subdisciplines Description of ContentsMARGITNo ratings yet
- Rushil Decor LTDDocument47 pagesRushil Decor LTDtwinkalNo ratings yet
- Guidelines For Design of Earth DamsDocument13 pagesGuidelines For Design of Earth Damsrvkumar3619690100% (1)
- Ema's Charsheet, D&D 3.5 Ranger Spell SheetDocument5 pagesEma's Charsheet, D&D 3.5 Ranger Spell SheetSszveinNo ratings yet
- BioCapt Single UseMKTRev2 20150902 PDFDocument2 pagesBioCapt Single UseMKTRev2 20150902 PDFyuly yaniNo ratings yet
- Lab Math Lec (Prelims)Document7 pagesLab Math Lec (Prelims)Merra VenzuelaNo ratings yet
- Pre-Analytic Issues in Laboratory MedicineDocument9 pagesPre-Analytic Issues in Laboratory MedicineanggaririnNo ratings yet
- Portable Real-Time PCR Shenzhen Shineway v2Document26 pagesPortable Real-Time PCR Shenzhen Shineway v2Ale WengerNo ratings yet
- Lesson-27 Quality Control in CytologyDocument5 pagesLesson-27 Quality Control in CytologySasa AbassNo ratings yet
- Basic Rules of BiosafetyDocument3 pagesBasic Rules of BiosafetyBen ClydeNo ratings yet
- Auditing of Microbilogical Laboratory by P.hemaDocument31 pagesAuditing of Microbilogical Laboratory by P.hemaHema Pepakayala100% (2)
- 9433 - Sterlity Test Medical Devices - Web ReadyDocument4 pages9433 - Sterlity Test Medical Devices - Web ReadyZETTYNo ratings yet
- Microbiological Best Lab Practice&Environmental Monitoring-DikonversiDocument26 pagesMicrobiological Best Lab Practice&Environmental Monitoring-DikonversiNurul Hardiyanthi SadikinNo ratings yet
- Microbial Environment MonitoringDocument4 pagesMicrobial Environment MonitoringankziiNo ratings yet
- Sartorius Bio Aseptic SamplingDocument9 pagesSartorius Bio Aseptic SamplingTimNo ratings yet
- Lesson 13Document7 pagesLesson 13Abdelraouf ElmanamaNo ratings yet
- Pmls1 Lesson 2Document4 pagesPmls1 Lesson 2Kyla TabilasNo ratings yet
- Asama PosterDocument1 pageAsama Postershuvojit moulikNo ratings yet
- Kolgotrg Ovarian Cancer Biobak KolkataDocument1 pageKolgotrg Ovarian Cancer Biobak Kolkatashuvojit moulikNo ratings yet
- Who Wpe Gih 2021.1 EngDocument12 pagesWho Wpe Gih 2021.1 Engnydiacastillom2268No ratings yet
- DNA ExtractionDocument9 pagesDNA Extractionمحمود صالح محمود عليNo ratings yet
- Standard Operating Procedure (SOP) Niacin TestDocument5 pagesStandard Operating Procedure (SOP) Niacin TestSuci IrianiNo ratings yet
- Chem LecDocument11 pagesChem LecBeautyand ThebeastNo ratings yet
- Whitepaper Benefits DNA Sequencing Microbial Identification Pharma Analytics June 2022Document5 pagesWhitepaper Benefits DNA Sequencing Microbial Identification Pharma Analytics June 2022JohnNo ratings yet
- AST Testing MethodsDocument42 pagesAST Testing Methodstanty_ukNo ratings yet
- Trans-Molbio-Lab-Act 1Document6 pagesTrans-Molbio-Lab-Act 1janekieannearlosNo ratings yet
- Laboratory Biosafety Guidance Related To Coronavirus Disease 2019 (COVID-19)Document13 pagesLaboratory Biosafety Guidance Related To Coronavirus Disease 2019 (COVID-19)Holly Smith100% (1)
- 4 CCHM Trans LecDocument8 pages4 CCHM Trans LecCRUZ, ANNA MARIELLENo ratings yet
- DIB - Week 01 - 02 - Anatomy & Physiology PDFDocument99 pagesDIB - Week 01 - 02 - Anatomy & Physiology PDFFaisal MujibNo ratings yet
- Manufacturing Finals ExamDocument39 pagesManufacturing Finals ExamShawn Vaughn Allen SilorioNo ratings yet
- Quantitative Analysis (CHEM 201) What Do You Need?: Fall 2007, SH-C162 T &TH: 11:40 Am - 1 PMDocument11 pagesQuantitative Analysis (CHEM 201) What Do You Need?: Fall 2007, SH-C162 T &TH: 11:40 Am - 1 PMCheNo ratings yet
- Cytiva BuyDocument25 pagesCytiva BuyKalpita NathNo ratings yet
- MolBio Lab-Act #2-Laboratory Operations-Design and EquipmentDocument8 pagesMolBio Lab-Act #2-Laboratory Operations-Design and EquipmentJhenica D. NonanNo ratings yet
- Bosch Vivalytic Sti Cartiladge and QC IFU Update 17-3 Last UpdateDocument7 pagesBosch Vivalytic Sti Cartiladge and QC IFU Update 17-3 Last UpdateMohammed AlshnqityNo ratings yet
- Diagnosing: Jericko MagistradoDocument25 pagesDiagnosing: Jericko MagistradoJericko MagistradoNo ratings yet
- Biosafety Training 3Document16 pagesBiosafety Training 3senyoradomitillamercadejasNo ratings yet
- Comprehensive Genomic Profiling at IlluminaDocument23 pagesComprehensive Genomic Profiling at IlluminaSaulius BarauskasNo ratings yet
- Lecture 15 Cell BlockingDocument4 pagesLecture 15 Cell BlockingChef der Personal und Verwaltung ReichskanzleiNo ratings yet
- 3C Domingo Shifting1ALaboratoryDocument4 pages3C Domingo Shifting1ALaboratoryJC DomingoNo ratings yet
- Cytopreparatory Technique: Ama AfrahDocument49 pagesCytopreparatory Technique: Ama Afrahreuben kwotaNo ratings yet
- Cc1 Lec MergeDocument54 pagesCc1 Lec MergeMariaerika JordanNo ratings yet
- Lab Technologist Key Accountabilities & DutiesDocument1 pageLab Technologist Key Accountabilities & DutiessamNo ratings yet
- Cleaning Validation & Regulatory Compliance - Part4Document8 pagesCleaning Validation & Regulatory Compliance - Part4sasirkumar1No ratings yet
- Covid-19 One-Step RT-PCR Kit - IFUDocument2 pagesCovid-19 One-Step RT-PCR Kit - IFUHarun GanićNo ratings yet
- Bioburden TestDocument4 pagesBioburden TestMujeeb Ullah KhanNo ratings yet
- 1 Preparation of Laboratory Food SamplesDocument15 pages1 Preparation of Laboratory Food Samplesahmed alaaNo ratings yet
- Diagnostic Procedures: R. C. B. SlackDocument8 pagesDiagnostic Procedures: R. C. B. Slacknour achkarNo ratings yet
- HistopathDocument37 pagesHistopathFait HeeNo ratings yet
- Eurofins Genomics Europe Synthesis GMBH: Viroboar 4.0 RT-PCR Kit (Sars-Cov-2) User ManualDocument2 pagesEurofins Genomics Europe Synthesis GMBH: Viroboar 4.0 RT-PCR Kit (Sars-Cov-2) User ManualBatoNo ratings yet
- Ex Vivo Platform: ExpertiseDocument2 pagesEx Vivo Platform: ExpertiseMazhar KayaNo ratings yet
- Bitesize Bio NEB NAP EbookDocument22 pagesBitesize Bio NEB NAP EbookIdamelis Rodríguez GarcíaNo ratings yet
- Water - ISPE PDFDocument24 pagesWater - ISPE PDFmanojdhamne5802100% (1)
- Molecular Biology: Laboratory Safety and PrecautionDocument7 pagesMolecular Biology: Laboratory Safety and PrecautionSamantha100% (1)
- 0056-0060 (61) Microbiological Examination of Nonsterile Products - Microbial Enumeration TestsDocument5 pages0056-0060 (61) Microbiological Examination of Nonsterile Products - Microbial Enumeration TestsMerrene Bright Divino JudanNo ratings yet
- 62 The Basics of Bioburden TestingDocument2 pages62 The Basics of Bioburden Testinghitham shehataNo ratings yet
- Cascadion 2018 EU 24i Godwin - Tetteh 96413 PosterDocument1 pageCascadion 2018 EU 24i Godwin - Tetteh 96413 Posteralexandre larmagnacNo ratings yet
- Cell Counting ProformaDocument5 pagesCell Counting ProformadonaNo ratings yet
- Quality Control in Histopathology - PPTX Edited - PPTX No 1Document30 pagesQuality Control in Histopathology - PPTX Edited - PPTX No 1Medicine 0786No ratings yet
- WHO WPE GIH 2020.2 Eng PDFDocument11 pagesWHO WPE GIH 2020.2 Eng PDFMaicon MarquesNo ratings yet
- Peranan Mikrobiologi Dalam Diagnosis Penyakit Infeksi: Dr. Agus Eka Darwinata, PH.DDocument43 pagesPeranan Mikrobiologi Dalam Diagnosis Penyakit Infeksi: Dr. Agus Eka Darwinata, PH.DKomang YuniNo ratings yet
- Usp 61 Microbiological Examination of Nonsterile Products Microbial Enumeration TestsDocument5 pagesUsp 61 Microbiological Examination of Nonsterile Products Microbial Enumeration TestsyuniarwindiNo ratings yet
- Lab Diagnosis of TBDocument73 pagesLab Diagnosis of TBMigori ArtNo ratings yet
- Lady Lazarus AnnotationsDocument2 pagesLady Lazarus Annotationsapi-511521252No ratings yet
- Desktop Support Engineer Interview QuestionsDocument3 pagesDesktop Support Engineer Interview QuestionsjosephNo ratings yet
- Quiz Track1 1Document4 pagesQuiz Track1 1windleaNo ratings yet
- Factories and Works Act 15:04 RGN 264: Building, Structural and Excavation WorkDocument19 pagesFactories and Works Act 15:04 RGN 264: Building, Structural and Excavation WorkCourageNo ratings yet
- One Pager 1Document1 pageOne Pager 1api-557165715No ratings yet
- Test 3 TronwellDocument8 pagesTest 3 Tronwellpablopez30No ratings yet
- Gran Armada de 1588Document5 pagesGran Armada de 1588samuraijack7No ratings yet
- VAVEDocument39 pagesVAVEprakash_20305No ratings yet
- ESEM 5554 Reflection 4Document3 pagesESEM 5554 Reflection 4nitiyahsegarNo ratings yet
- Juice Sulphitation Process - Methods of Sugar Cane Juice SulphitationDocument6 pagesJuice Sulphitation Process - Methods of Sugar Cane Juice SulphitationYounas Sardar0% (1)
- Island Society ActivityDocument2 pagesIsland Society Activityapi-240157347No ratings yet
- Industry Oriented Training Synopsis ReportDocument23 pagesIndustry Oriented Training Synopsis Reportsanyam dhawan0% (1)
- Technical Textile and Its Area of Application - PDF Version 1Document6 pagesTechnical Textile and Its Area of Application - PDF Version 1k sNo ratings yet
- 3 2 - Thursday - Kitty Lesson PlanDocument6 pages3 2 - Thursday - Kitty Lesson Planapi-326382783100% (1)
- Ijest NG Vol3 No7 pp1 14 PDFDocument14 pagesIjest NG Vol3 No7 pp1 14 PDFRahul SethiNo ratings yet
- Glazing and Curtain Wall Prices Philippines - PHILCON PRICESDocument1 pageGlazing and Curtain Wall Prices Philippines - PHILCON PRICESjohn reyesNo ratings yet
- Xbox 360 Error CodesDocument6 pagesXbox 360 Error CodesTOM2-TOM20% (3)
- Alma Redemptoris Mater PDFDocument2 pagesAlma Redemptoris Mater PDFJoeNo ratings yet
- AUTOSAR SRS GatewayDocument31 pagesAUTOSAR SRS Gatewaymahmooudhelmyy1No ratings yet
- Modul - Bahasa Inggris 1 - UNIT 5 Rev 2019 - PDFDocument12 pagesModul - Bahasa Inggris 1 - UNIT 5 Rev 2019 - PDFFreeze AndrewNo ratings yet
- 04 Catalogo Intifernal Records - AbrilDocument2 pages04 Catalogo Intifernal Records - AbrilGabriel RiosNo ratings yet
- Φ630 Cantilever frame Single-twist Cabling MachineDocument3 pagesΦ630 Cantilever frame Single-twist Cabling Machinetees220510No ratings yet
- Russell's Criticism of Logical PositivismDocument33 pagesRussell's Criticism of Logical PositivismDoda BalochNo ratings yet
- ZUBXDocument14 pagesZUBXAtika SeharNo ratings yet
- Midlife Crisis - Signs, Causes, and Coping TipsDocument13 pagesMidlife Crisis - Signs, Causes, and Coping TipsMonyesmaNo ratings yet