Professional Documents
Culture Documents
Jurnal 2
Uploaded by
rosianaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal 2
Uploaded by
rosianaCopyright:
Available Formats
British Journal of Clinical DOI:10.1111/j.1365-2125.2010.03717.
Pharmacology
Correspondence
Influences of different proton Dr Takahisa Furuta MD PhD, Center for
Clinical Research, Hamamatsu University
School of Medicine, 1-20-1. Handayama,
pump inhibitors on the Higashi-Ku, Hamamatsu 431-3192, Japan.
Tel.: +81 53 435 2850
Fax: +81 53 435 2851
anti-platelet function of E-mail: furuta@hama-med.ac.jp
----------------------------------------------------------------------
clopidogrel in relation to Keywords
clopidogrel, CYP2C19, drug–drug
interaction, genotype, platelet function,
CYP2C19 genotypes proton pump inhibitor
----------------------------------------------------------------------
Received
Takahisa Furuta,1 Takayuki Iwaki2 & Kazuo Umemura2 13 January 2010
1
Accepted
Center for Clinical Research and 2Department of Pharmacology, Hamamatsu University School of 21 April 2010
Medicine, Hamamatsu 431-3192, Japan
WHAT IS ALREADY KNOWN ABOUT
THIS SUBJECT
• Active metabolism of clopidogrel is mainly AIMS
mediated by CYP2C19. There are genetic The efficacy of clopidogrel is influenced by CYP2C19 genotypes and
substrates of CYP2C19, such as proton pump inhibitors (PPIs). We
differences in the activity of CYP2C19.
assessed the influence of three different PPIs on the anti-platelet
Therefore, active metabolism of clopidogrel function of clopidogrel in relation to CYP2C19 genotype status.
is affected by CYP2C19 genotypes.
• The main metabolizing enzyme of proton METHODS
pump inhibitors (PPIs) is CYP2C19. Thirty-nine healthy volunteers with different CYP2C19 genotypes took
Therefore, the anti-platelet function of clopidogrel 75 mg with or without omeprazole 20 mg, lansoprazole
30 mg or rabeprazole 20 mg in the morning for 7 days. The influence
clopidogrel is attenuated by concomitant
of the three PPIs on the anti-platelet function of clopidogrel was
use of PPIs. determined. A less than 30% inhibition of platelet aggregation (IPA)
• There are differences in the metabolic during clopidogrel dosing was defined as a ‘low responder’. We also
disposition among different PPIs. Affinity to examined whether evening dosing of omeprazole could prevent the
CYP2C19 differs among different PPIs. interaction with clopidogrel dosed in the morning.
RESULTS
In rapid metabolizers (RMs, *1/*1, n = 15) of CYP2C19, omeprazole and
WHAT THIS STUDY ADDS rabeprazole significantly attenuated the anti-platelet function of
• Whether a PPI attenuates the efficacy of clopidogrel. In decreased metabolizers (DMs, carriers of *2 and/or *3,
clopidogrel depends on CYP2C19. n = 24), there was a large variation in IPA and there was a trend but no
Individuals who are decreased metabolizers, significant decrease in IPA when placed on a concomitant PPI. Some
DMs became ‘low-responders’ when placed on a concomitant PPI.
i.e. carriers the allele of CYP2C19 *2 and/or
Evening omeprazole dose in RMs did not seem to cause a significant
*3, are more likely to convert from decrease in IPA in contrast to morning dosing, but did so in DMs.
‘responder’ to ‘non-responder’ to clopidogrel
when placed on a concomitant PPI. CONCLUSIONS
• We found that rabeprazole, whose affinity to The three PPIs affected the efficacy of clopidogrel to different degrees.
CYP2C19 has been considered lower, Both omeprazole and rabeprazole significantly decreased IPA in RMs
but not DMs, although there was a trend towards lower IPA in DMs.
attenuated the efficacy of clopidogrel.
Morning and evening dosing of omeprazole were both associated with
• We tested whether the separate dosing of a lower IPA in DMs.
PPI and clopidogrel decreased the risk of
attenuation of clopidogrel efficacy. We
unfortunately found that separate dosing
did not avoid the problematic interaction
between clopidogrel and a PPI in subject’s
with CYP2C19 *2 and/or CYP2C19 *3.
© 2010 The Authors Br J Clin Pharmacol / 70:3 / 383–392 / 383
Journal compilation © 2010 The British Pharmacological Society
T. Furuta et al.
Introduction affinity to CYP2C19 among different PPIs results in differ-
ent effects on the anti-platelet function of clopidogrel.
Anti-platelet therapy is now widely used in patients with Another problem with clopidogrel is interindividual
stroke, myocardial infarction or peripheral arterial disease. difference in its anti-platelet activity among the different
Clopidogrel and aspirin are the most important corner- CYP2C19 genotype groups [11]. Patients with intermediate
stone agents in this therapy. To prevent stent thrombosis or poor metabolizer genotype of CYP2C19 are at a higher
after implantation of bare metal and drug-eluting stents, risk of stent thrombosis and re-infarction because of
dual anti-platelet therapy with aspirin and clopidogrel is decreased active metabolism of clopidogrel [18–22].
now a standard therapy [1]. However, such antiplatelet However, no study has evaluated the influence of CYP2C19
therapy increases the risk of gastrointestinal bleeding genotype status and different PPIs on the anti-platelet
[2–7]. A proton pump inhibitor (PPI), therefore, is often pre- function of clopidogrel simultaneously.
scribed with anti-platelet agents. In 2008, the American Based on the backgrounds mentioned above, we pro-
College of Cardiology Foundation (ACCF), the American spectively examined the effect of three proton pump
College of Gastroenterology (ACG) and American Heart inhibitors, omeprazole, lansoprazole and rabeprazole, on
Association (AHA) published their statement on antiplate- the anti-platelet function of clopidogrel in relation to
let therapy which recommends the prescription of a PPI to CYP2C19 genotype status. In addition, we examined
patients with a risk of peptic ulcer and/or on two or more whether the interaction between a PPI and clopidogrel
antiplatelet agents [8–10]. could be avoided by administering the two drugs sepa-
The drug–drug interaction between clopidogrel and a rately instead of taking them concomitantly.
PPI has been receiving attention lately. Clopidogrel is
metabolized by CYP2C19 to form its active metabolites.
Therefore, the plasma concentration of the active metabo- Methods
lite of clopidogrel depends on the activity of CYP2C19
[11]. CYP2C19 is also the main metabolizing enzyme Subjects
of PPIs. Therefore, concomitant use of clopidogrel and a Thirty-nine healthy volunteers were enrolled in this study.
PPI induces a drug–drug interaction, resulting in the None had taken any drug and smoked for at least 2 weeks
decreased activation of clopidogrel, which attenuates its before and during this study. Written informed consent
the anti-platelet effect and could lead to an increased risk was obtained from each of the subjects before their par-
of re-infarction and/or stent thrombosis. PPIs per se are ticipation in the study. The protocol was approved in
recognized as inhibitors of CYP2C19 [12], which would advance by the Human Institutional Review Board of
also contribute to the attenuation of activation of clopi- Hamamatsu University School of Medicine, Hamamatsu,
dogrel. Juurlink et al. [13] reported that concomitant Japan. Clinical demographic characteristics of the subjects
therapy with a PPI other than pantoprazole was associ- are summarized in Table 1. The study was performed from
ated with an increased risk of re-infarction. Ho et al. [14] February 2009 to June 2009.
reported that concomitant use of clopidogrel and a PPI
was associated with an increased risk of adverse out-
comes compared with the use of clopidogrel alone. Toth Genotyping of CYP2C19
et al. [15] reported that the efficacy of clopidogrel can also DNA was extracted from blood samples obtained from
be reduced if patients are receiving concomitant therapy volunteers using a commercially available kit (Genomix,
with a PPI such as omeprazole. However, Siller-Matula
et al. [16] reported that the intake of pantoprazole or
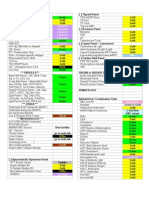
Table 1
esomeprazole is not associated with an impaired
Demographic clinical characteristics of subjects enrolled to the study
response to clopidogrel. Thus, the influence of PPIs on
clopidogrel efficacy seems controversial.
Interestingly, the influences of PPIs on CYP2C19 differ RMs DMs
among different PPIs. Omeprazole is a substrate with Parameters n = 15 n = 24 P values
strong affinity to CYP2C19. Lansoprazole is also a substrate CYP2C19 genotypes *1/*1: n = 15 *1/*2: n = 13
for CYP2C19 but with a weak affinity in comparison with *1/*3: n = 9
*2/*2: n = 0
omeprazole. The metabolism of rabeprazole has been
*2/*3: n = 2
thought to be less associated with CYP2C19 [17]. There *3/*3: n = 0
have been several reports on drug–drug interactions Male/Female 14/1 18/6 >0.2
between omeprazole and other drugs (e.g. warfarin, Age (years) 22.4 ⫾ 2.1 24.0 ⫾ 5.7 >0.2
Height (cm) 172.7 ⫾ 8.2 168.7 ⫾ 6.4 >0.2
phenytoin, diazepam), while incidences of drug–drug
BW (kg) 64.9 ⫾ 10.9 61.7 ⫾ 9.3 >0.2
interactions of rabeprazole and lansoprazole are not so BMI (kg m-2) 21.7 ⫾ 2.4 21.6 ⫾ 2.1 >0.2
many as observed with omeprazole [12]. However, it has
not been fully elucidated whether this difference in the DM, decreased metabolizer of CYP2C19; RM, rapid metabolizer of CYP2C19.
384 / 70:3 / Br J Clin Pharmacol
Influence of PPIs on clopidogrel and CYP2C19 genotypes
1st study 2nd study morning and by receiving a response from each subject
confirming the completion of taking the drugs.
Of 39 subjects, 30 participated in the second study, to
PPI 1 PPI 2 PPI 3 OPZ in the examine whether the separate dose of a PPI and clopi-
evening dogrel could prevent the drug–drug interaction between
PPI
them. They took 20 mg omeprazole at 20.00 h in the
Clopidogrel evening and 75 mg clopidogrel at 08.00 h the next
≥ 2 weeks ≥ 2 weeks ≥ 2 weeks ≥ 2 weeks
1 week 1 week 1 week 1 week 1 week
morning for 7 days. Platelet aggregation induced by 20 mM
of ADP was measured at 4 h after the last dose of clopi-
Platelet dogrel on the 7th day as noted above.
aggregation
Measurement of platelet aggregation
Figure 1 Platelet aggregation was measured as previously reported
Schematic demonstration of the study protocol. Firstly, all 39 subjects [11]. In brief, blood samples were collected in test tubes
took 75 mg clopidogrel at 08.00 h for 7 days. Next, all subjects took clopi- containing 1/10 volume of 3.2% trisodium citrate, and
dogrel 75 mg with a different PPI, 20 mg omeprazole, 30 mg lansoprazole platelet-rich and platelet-poor plasma were prepared by
or 20 mg rabeprazole. The order of the three PPIs was randomized. All
differential centrifugation at room temperature (150 g
medications were taken once daily at 08.00 h.There was a washout period
of at least 2 weeks between the two study periods. In the second study, 30 [900 rev min-1] for 15 min for platelet-rich plasma and
of 39 subjects took 20 mg omeprazole (OPZ) at 20.00 h and 75 mg clopi- 1710 g [3000 rev min-1] for 15 min for platelet-poor
dogrel at 08.00 h for 7 days. Platelet aggregation induced by 20 mM of ADP plasma). Maximum platelet aggregation (MPA) was deter-
was measured before the study and at 4 h after the last dose of clopi- mined in response to 20 mM ADP by light transmittance
dogrel on the 7th day of each study period
aggregometry using MCM hematracer 313-M (SSR engi-
neering Co. LTD., Tokyo, Japan). MPA was measured by an
expert technician who was unaware of any of information
Talent, Trieste, Italy). DNA samples were genotyped for
about the subjects. The inhibition of platelet aggregation
CYP2C19 as previously reported [23] to identify the
(IPA)(%) was calculated from the observed MPA value at
CYP2C19 wild type (*1) gene and two mutant alleles,
each scheduled time point with each treatment where:
CYP2C19 *2 (*2) in exon 5 and CYP2C19 *3 (*3) in exon 4.
Volunteers were then classified into three groups by geno- IPA = [(MPA baseline − MPA postdose )
type, namely rapid metabolizers (RMs) (*1/*1), intermedi- MPA baseline]×100%
ate metabolizers (IMs) (*1/*2 or *1/*3) and poor
metabolizers (PMs) (*2/*2, *3/*3, or *2/*3) [23]. The pres- IPA <30% was defined as a ‘low-responder’ [25, 26].
ence of the CYP2C19 *17 (*17) allele (ultra rapid metabo-
lizer) was also determined for all DNA samples as Data analysis
previously reported [24]. All numerical data are given as mean ⫾ standard deviation
(SD). Statistically significant differences in means of age
Study protocol and body weight between the two CYP2C19 genotype
This was the open-label single-arm crossover study. The groups were assessed by Student’s t-test.The male : female
schematic protocol is shown in Figure 1. Firstly, all 39 sub- ratios between the two genotype groups were assessed by
jects took 75 mg of clopidogrel at 08.00 h for 7 days. Plate- Fisher’s exact test. Statistically significant difference in
let aggregation induced by 20 mM of ADP was measured changes in IPA with different regimens between the two
before the first dose and 4 h (at 12.00 h) after the last dose CYP2C19 genotype groups were assessed by repeated
of clopidogrel for 7 days to calculate the baseline levels of measures ANOVA and Scheffe’s multiple comparison test.All
inhibition of platelet aggregation (IPA) (%), a representa- P values were two-sided and P < 0.05 indicated statistical
tive index of anti-platelet function of clopidogrel, as significance.
described later for each subject. Next, all subjects partici-
pated in a crossover study of 7 days dosing of clopidogrel
75 mg with a different PPI. They took 75 mg of clopidogrel Results
with 20 mg of omeprazole (Omepral®, AstraZeneca K.K.,
Osaka, Japan), 30 mg of lansoprazole (Takepuron®, Takeda CYP2C19 genotype and compliance
Pharmaceutical Co Ltd. Osaka, Japan) or 20 mg of rabepra- The study subjects consisted of 15 rapid metabolizers (RMs
zole (Pariet®, Eisai Co. Ltd, Tokyo, Japan). The order of the *1/*1), 22 intermediate metabolizers (IMs *1/*2: n = 13,
three PPIs was randomized. All medications were taken *1/*3: n = 9) and two poor metabolizers (PMs *2/*3: n = 2).
once daily at 08.00 h. There was a washout period of at There were no subjects who had the *17 allele. All subjects
least 14 days between different PPI dosings. Compliance completed the study protocol without any adverse events.
was confirmed by sending a reminder e-mail every Because the number of PMs was limited (only two), IMs and
Br J Clin Pharmacol / 70:3 / 385
T. Furuta et al.
A (n = 39) B
100 100
P = 0.825 P = 0.035
P = 0.724 P = 0.508
Inhibition of platelet aggregation (%)
Inhibition of platelet aggregation (%)
80 80
P = 0.015
P = 0.094
60 60
P < 0.001
P = 0.003
P < 0.001
P < 0.001
40 40
20 20
P = 0.443
P = 0.951
P =0.635
0 0
Clopidogrel + + + + + + + +
PPI – OPZ LPZ RPZ – OPZ LPZ RPZ
Figure 2
Changes in the inhibition of platelet aggregation (IPA) by clopidogrel with different PPIs in the whole group (A) and in different CYP2C19 genotype groups
(B). The grey zone indicates the low-responders. The anti-platelet function of clopidogrel was not influenced by any of the three PPIs, omeprazole (OPZ),
lansoprazole (LPZ) or rabeprazole (RPZ), in the whole group (A). When separately analyzed according to CYP2C19 genotype groups, statistically significant
differences in the inhibition of platelet aggregation by clopidogrel were found (B). This difference was maintained during the concomitant dosing with
different PPIs. Omeprazole (OPZ) and rabeprazole (RPZ) significantly attenuated the inhibition of platelet aggregation by clopidogrel in rapid metabolizers
(RMs) of CYP2C19 (B). (B): Rapid metabolizer (n = 15) ( ); Decreased metabolizer (n = 24) ( )
PMs were combined into one group, named as the tively. In RMs, omeprazole and rabeprazole significantly
decreased metabolizers (DMs) of CYP2C19, who had *2 decreased the mean IPA induced by clopidogrel. On the
and/or *3 allele (Table 1). other hand, in DMs, the IPA appeared to be decreased by
omeprazole, but the difference did not reach statistical
Effect of concomitant dose of PPIs on significance due to the wide distribution of IPA values.
anti-platelet function of clopidogrel The incidence of ‘responder’ (IPA ⱖ30%) and ‘low
The mean IPAs induced by clopidogrel alone, clopidogrel responder’ (IPA <30%) in different regimens as a function
with omeprazole, clopidogrel with lansoprazole and clopi- of CYP2C19 status is summarized in Table 2. The incidence
dogrel with rabeprazole were 45.0%, 40.2% (P = 0.094 vs. of low-responders in the RM group (n = 15) were 0 (0%), 0
clopidogrel alone), 44.2% (P = 0.724) and 44.4% (P = 0.825), (0%), 0 (0%) and 1 (7%) in the regimens with clopidogrel
respectively. The mean of IPA induced by clopidogrel was alone, clopidogrel and omeprazole, clopidogrel and lanso-
not significantly decreased by any of the three PPIs. The prazole, and clopidogrel and rabeprazole, respectively.
effect of omeprazole did not reach the statistical signifi- Those in the DM group (n = 24) were 8 (33%), 10 (42%),
cance. (Figure 2A). 6 (25%) and 6 (25%), respectively.
When data were stratified based on CYP2C19 genotype Changes in IPA by different PPIs in individual subjects in
status to RMs and DMs, the IPA of RMs was significantly the RM and DM groups are shown in Figure 3A, B, respec-
higher than in DMs in any of the study regimen (Figure 2B). tively. The IPA did not decrease to the levels of ‘low-
The mean IPA induced by clopidogrel alone, clopidogrel responder’ in RMs except in one case when rabeprazole
with omeprazole, clopidogrel with lansoprazole and clopi- was dosed (Figure 3A) as noted above, although the mean
dogrel with rabeprazole in RMs was 58.3%, 51.2% (P = IPA was significantly decreased by omeprazole and
0.015, vs. clopidogrel alone), 56.5% (P = 0.508) and 53.5% rabeprazole in RMs. On the other hand, the mean IPA at
(P = 0.035), respectively, and that in DMs was 36.6%, 33.3% baseline in DMs was close to the threshold line of <30%
(P = 0.443), 36.4% (P = 0.951) and 38.7% (P = 0.635), respec- and eight of the 24 DMs (30%) were in the ‘low-responder’
386 / 70:3 / Br J Clin Pharmacol
Influence of PPIs on clopidogrel and CYP2C19 genotypes
Table 2
Incidence of ‘responder’ and ‘low responder’ to clopidogrel in different regimens
Responder/Non-responder (n)
Regimen Clopidogrel alone Clopidogrel + OPZ Clopidogrel + LPZ Clopidogrel + RPZ
CYP2C19 RM 15/0 (100%/0%) 15/0 (100%/0%) 15/0 (100%/0%) 14/1 (93%/7%)
DM 16/8 (67%/33%) 14/10 (58%/42%) 18/6 (75%/25%) 18/6 (75%/25%)
DM, decreased metabolizer of CYP2C19 who has *2 and/or *3 allele of CYP2C19; LPZ, lansoprazole; OPZ, omeprazole; RM, rapid metabolizer of CYP2C19 (*1/*1); RPZ, rabeprazole.
A Rapid metabolizer B Decreased metabolizer
100 (n = 15) 100 (n = 24)
Inhibition of platelet aggregation (%)
Inhibition of platelet aggregation (%)
80 80
60 60
40 40
Low-responder
20 20
0 0
Clopidogrel + + + + + + + +
PPI – OPZ LPZ RPZ – OPZ LPZ RPZ
Figure 3
Individual changes in inhibition of platelet aggregation by clopidogrel with or without different PPIs. The connecting lines should be used to trace the IPA
values for each subject. The order of three PPIs was randomized. In the rapid metabolizers of CYP2C19 (RM), omeprazole (OPZ) and lansoprazole (LPZ)
influenced the efficacy of clopidogrel, but did not decrease it to the level of low-responders except in one case. In the decreased metabolizers (DM), there
was a wide distribution in the degree of inhibition of platelet aggregation by clopidogrel. Of 24 decreased metabolizers, 16 were not in the low-responder
group. PPIs affected the efficacy of clopidogrel. Of the 16 subjects not in the low-responder group, five, one and two became non-responders after
concomitant dosing with omeprazole, lansoprazole or rabeprazole (RPZ), respectively. Dotted lines indicate the IPA of poor metabolizers (*2/*3)
group before concomitant PPI dosing. When clopidogrel 7%)) (P = 0.083). On the other hand, six of eight DMs (75%)
was dosed with a PPI, IPA showed a wide variability and who were in the ‘low-responder’ group with clopidogrel
some subjects who were in the ‘responder’ group during alone converted to ‘responders’ when either of three PPIs
the dosing of clopidogrel alone became ‘low-responders’ was concomitantly dosed. Thus, the concomitant use of
after receiving PPIs. Of the 16 DMs who were judged as a PPI made the effect of clopidogrel widely variable,
‘responders’ during the dosing with clopidogrel alone, 5 especially in DMs.
(31%), 1 (6%) and 2 (13%) became ‘low-responders’ after
receiving a concomitant omeprazole, lansoprazole or Effect of separate doses of PPIs on the
rabeprazole, respectively. (Figure 3B). Although Table 2 anti-platelet function of clopidogrel
suggests that the incidence of low responders did not Of the 39 subjects, 30 completed the second study. IPA
change so much with the concomitant use of a PPI, in fact induced by clopidogrel alone in the morning, clopidogrel
only 10 of them remained in the‘responder group’irrespec- plus omeprazole in the morning, clopidogrel in the
tive of PPI dosing and six of 16 became ‘low responders’ morning plus omeprazole in the evening were 49.5%,
when dosed with either of three PPIs. This conversion rate 41.5% (P = 0.014 vs. clopidogrel alone) and 43.4% (P =
(6/16, 38%) in DMs appeared higher than that in RMs (1/15, 0.044), respectively. As a whole, the effect of clopidogrel
Br J Clin Pharmacol / 70:3 / 387
T. Furuta et al.
A B
100 100
(n = 30)
P = 0.044 P = 0.229
Inhibition of platelet aggregation (%)
Inhibition of platelet aggregation (%)
80 80
P = 0.014 P = 0.392 P = 0.021 P = 0.131
60 60
40 40
20 20
P = 0.066
P = 0.922
P = 0.070
0 0
Clopidogrel Mor Mor Mor Mor Mor Mor
Omeprazole – Mor Eve – Mor Eve
Figure 4
The effect of morning (Mor) or evening (Eve) dose of omeprazole on the efficacy of clopidogrel in the whole group (A) and in different CYP2C19 genotype
groups (B). Decreased efficacy of clopidogrel by the concomitant dosing of omeprazole was not restored by the separate dosing of omeprazole as a whole
(A). When separately analyzed according to CYP2C19 genotype, the decreased efficacy of clopidogrel with concomitant dosing with omeprazole was
restored by a separate dosing of omeprazole in the rapid metabolizers (RMs) of CYP2C19. In the decreased metabolizers (DM), omeprazole appeared to
decrease the efficacy of clopidogrel, which seemed not to be restored by the separate dosing of omeprazole. (B): Rapid metabolizer (n = 14) ( ); Decreased
metabolizer (n = 16) ( )
was significantly attenuated by a concomitant dose Discussion
of omeprazole, which could not be improved when
omeprazole was dosed separately in the evening We evaluated the influences of PPIs on the effect of clopi-
(Figure 4A). dogrel in relation to CYP2C19 genotypes and found that
The data were analyzed according to CYP2C19 any of three PPIs (i.e. omeprazole 20 mg, lansoprazole
genotype status. In RMs of CYP2C19 (n = 14), the effect of 30 mg and rabeprazole 20 mg) could cause attenuation of
clopidogrel was attenuated by co-administration of ome- the anti-platelet function of clopidogrel. We observed that
prazole (from 59.1% to 51.8%: P = 0.021) but appeared to the influence of a PPI on the effect of clopidogrel differed
be improved when omeprazole was dosed separately in between the CYP2C19 genotype groups and that drug–
the evening (56.2%: P = 0.229 vs. clopidogrel alone). drug interactions between clopidogrel and PPIs resulting
However, in the DM group (n = 16), the attenuated effect of in the decrease in IPA to the level of ‘low-responder’ were
clopidogrel by omeprazole dosed concomitantly did not likely to occur in DMs of CYP2C19, who are carrying the
appear to be improved by separate dosing of omeprazole decreased function allele of CYP2C19 (i.e. *2 and/or *3). We
in the evening (41.2%, 35.2%: P = 0.124 vs. clopidogrel also observed that separate dosing of a PPI (i.e. clopidogrel
alone, 32.2%: P = 0.096) (Figure 4B). in the morning and a PPI in the evening) did not prevent
In the RMs, regardless of whether omeprazole was the drug–drug interaction between clopidogrel and a PPI.
dosed concomitantly in the morning or separately in the Therefore, we have to reconsider the risk and benefit
evening, none was judged to be a ‘low-responder’ balance of the concomitant use of clopidogrel and a PPI
(Figure 5A). On the other hand, some of the DMs converted with reference to CYP2C19 genotype status.
to ‘responders’ after the separate dosing of omeprazole There appear to be differences in the effects on clopi-
and clopidogrel, while some DMs converted to ‘low dogrel among the different PPIs. Juurlink et al. [13] have
responders’ with the same regimen (Figure 5B). indicated that omeprazole, lansoprazole and rabeprazole,
388 / 70:3 / Br J Clin Pharmacol
Influence of PPIs on clopidogrel and CYP2C19 genotypes
A Rapid metabolizer B Decreased metabolizer
100 ( n = 14) 100 (n = 16)
Inhibition of platelet aggregation (%)
Inhibition of platelet aggregation (%)
80 80
60 60
40 40
Low-responder
20 20
0 0
Clopidogrel Mor Mor Mor Mor Mor Mor
Omeprazole – Mor Eve – Mor Eve
Figure 5
Individual changes in inhibition of platelet aggregation by clopidogrel with morning (Mor) or evening (Eve) dosing of omeprazole in different CYP2C19
genotype groups. The connecting lines should be used to trace the IPA of each subject. The order of three PPIs was randomized. In the rapid metabolizers
of CYP2C19 (RM), none became a low-responder (A). In the decreased metabolizers (DMs), four of seven subjects classified as low-responders during
concomitant dosing of clopidogrel and omeprazole become responders, but two subjects not classed as low-responders during concomitant dosing with
clopidogrel and omeprazole became low-responders after the separate dosing of clopidogrel and a PPI. The dotted line indicates the IPA of a poor
metabolizer (*2/*3)
but not pantoprazole, attenuate the clinical effect of clopi- In the present study, we tested omeprazole, lansopra-
dogrel in patients with cardiovascular disorders. Ho et al. zole and rabeprazole and found that the influence of three
[14] have reported that omeprazole and rabeprazole PPIs on the anti-platelet function of clopidogrel differed
attenuate the clinical effect of clopidogrel. Sibbing et al. among them. However, the levels of attenuation of clopi-
[27] reported that omeprazole impaired the anti-platelet dogrel by PPIs depended on CYP2C19 genotype status.
function of clopidogrel, but pantoprazole and esomepra- Although the efficacy of clopidogrel was decreased by a
zole did not. Gilard et al. [28] demonstrated that omepra- PPI in RMs of CYP2C19, the levels of anti-platelet function
zole impaired the anti-platelet function of clopidogrel of clopidogrel after attenuation by a PPI in this group were
[16, 27–29]. Small et al. [29] reported that lansoprazole mostly not problematic (i.e. rarely decreased to the levels
decreased the anti-platelet function of clopidogrel. Siller- of ‘low-responder’). Of 15 RMs, only one case became ‘low-
Matula et al. [16] reported that intake of pantoprazole or responder’after concomitant use of rabeprazole 20 mg. On
esomeprazole was not associated with impaired response the other hand, the efficacy of clopidogrel appeared to be
to clopidogrel. On the other hand, Zuern et al. [30] reported unstable with concomitant use of any of the PPIs used in
that co-administration of PPIs including pantoprazole and the present study especially in the DM group. Six of 16 DMs
esomeprazole significantly decreased the effect of clopi- who were judged as ‘responders’ during the dosing with
dogrel on platelet aggregation. Together, all PPIs used in clopidogrel alone became ‘low responders’ when clopi-
clinical practice appear to have the potential to attenuate dogrel was dosed with either of three PPIs, suggesting
the efficacy of clopidogrel. However, the recent report by that DMs could be at a higher risk of becoming a ‘low-
O’Donoghue et al. [31] demonstrated that a clinically prob- responder’ to clopidogrel and could easily become ‘low
lematic interaction was not observed between clopidogrel responders’ when clopidogrel was dosed with a PPI.There-
and a PPI, although the ex vivo study demonstrated that fore, we have to be careful with the concomitant use of
PPI use attenuated the anti-platelet effect of clopidogrel. clopidogrel and a PPI in DMs of CYP2C19 in particular.
Rassen et al. [32] did not observe any conclusive evidence The drug–drug interactions of PPIs with other drugs
of a clopidogrel–PPI interaction of major clinical relevance. through cytochrome P450s have not been considered so
Therefore, a drug–drug interaction between clopidogrel problematic. Several drug–drug interactions have been
and a PPI has been controversial. reported with omeprazole, but such reports on lansopra-
Br J Clin Pharmacol / 70:3 / 389
T. Furuta et al.
zole and rabeprazole have been rare [12]. However, recent dosed concomitantly with a PPI. Therefore, whichever
reports and our results have demonstrated that omepra- dosing scheme, concomitant or separate dosing of clopi-
zole as well as lansoprazole and rabeprazole attenuate the dogrel and a PPI, does not appear to be a problem in RMs.
efficacy of clopidogrel. The following explanations could On the other hand, in the DM group, the separate
be offered as the reason why the PPIs that had few reports dosing of clopidogrel and omeprazole could not prevent
on drug–drug interactions with many drugs influenced the attenuation of clopidogrel efficacy by omeprazole.
clopidogrel as shown in this study. The major metabolic Because the plasma half life and Cmax of omeprazole in the
route of clopidogrel is its metabolism by esterase to the DM group are increased in comparison with RMs [34] and
inactive metabolite (SR26334) and the active metabolism because activity of CYP2C19 to metabolize clopidogrel to
of clopidogrel by CYP2C19 is a minor route [33]. Moreover, its active metabolite is decreased in comparison with RMs,
CYP2C19 catalyzes the two step activation of clopidogrel omeprazole dosed in the evening could last for a long in
requires metabolism by CYP2C19 twice [33]. Therefore, in the systemic circulation and interfere with the efficacy of
the subjects with decreased activity of CYP2C19, such as clopidogrel dosed in the morning in DMs.
DMs, active metabolism of clopidogrel seemed to be easily The prophylactic use of a PPI for GI bleeding in patients
impaired by concomitant use of a PPI. Moreover, plasma undergoing anti-platelet therapy has been recommended
concentrations of PPIs in DMs of CYP2C19 are higher and [8–10]. However, our results indicate that prophylactic use
sustained longer in comparison with RMs [34–36], which of a PPI should be based on CYP2C19 genotype status. In
could further attenuate the active metabolism of the RMs, clopidogrel is extensively metabolized to its
clopidogrel. active metabolites, which indicates an increased risk of GI
However, in our study, some DMs, who were judged to bleeding with clopidogrel. Therefore a PPI should be used,
be ‘low responders’, converted to ‘responders’ when a PPI because the effect of a PPI on clopidogrel efficacy in this
was dosed. There is wide variation in the activity of group may be not so problematic. On the other hand, in
CYP2C19 in DMs of CYP2C19. The individuals who were the DMs of CYP2C19, efficacy of clopidogrel is decreased in
judged as the ‘low responders’ might have a lower activity comparison with RMs. Moreover, a PPI has a higher risk of
of CYP2C19. However, omeprazole is known to induce conversion from ‘responder’ to ‘low-responder’ in this
CYP1A2 in individuals with lower activity of CYP2C19 [37]. group.Therefore, we assume that the CYP2C19 genotyping
Therefore, the concomitant use of a PPI might induce test could be useful for the optimal prophylactic treatment
CYP1A2, which metabolized clopidogrel to the active for patients undergoing anti-platelet therapy.
metabolites, resulting in conversion of some ‘low- Recently, a histamine H2-receptor antagonist (H2RA)
responders’ to ‘responders’. Together, concomitant use of a was reported to be effective for the prevention of aspirin-
PPI with clopidogrel makes the effect of clopidogrel induced gastric injury [38]. Yasuda et al. [39] demonstrated
unstable. that an H2RA as well as a PPI completely prevented the GI
There were wide variation in the IPA in the DMs of bleeding and that an H2RA did not increase the risk of stent
CYP2C19, as demonstrated in our previous report [11]. We thrombosis or new lesions in coronary arteries in patients
cannot offer any appropriate explanation for the wide taking dual antiplatelet therapy after coronary stenting,
variation in clopidogrel efficacy in DMs. However, we are suggesting that an H2RA could replace a PPI as the prophy-
tempted to hypothesize that most of the DMs are het- lactic agent in patients taking dual antiplatelet therapy.
erozygous for a wild type allele and a mutated allele.Which However, this study is retrospective and no prospective
of the two alleles, a mutated allele or a wild type allele, is study has been performed. Therefore, which anti-secretory
dominant, may differ among different individuals. DMs in agent, a PPI or an H2RA, is better as the prophylactic agent
whom a mutated allele is dominant may show the lower in dual anti-platelet therapy must be verified from the
efficacy of clopidogrel and appear ‘low-responders’. On the points of view of safety and efficacy in a future prospective
other hand, DMs in whom the wild type allele is dominant, study.
where clopidogrel is extensively metabolized to the active Lastly, our results must be interpreted within the limi-
metabolites, appear ‘responders’. tations of the study. First of all, our study subjects were all
In the present study, we tested whether the separate healthy volunteers, not patients. Second, the sample size
dosing of a PPI (i.e. clopidogrel in the morning and ome- was small. However, we could not estimate the appropriate
prazole in the evening) could prevent the drug–drug inter- sample size because of lack of a preliminary study.Third, we
action between clopidogrel and a PPI. However, our study did not use aspirin, although many patients were treated
results indicated that separate dosing could not prevent with dual anti-platelet agents such as clopidogrel and
the drug–drug interaction between clopidogrel and a PPI. aspirin. Therefore, our study results should be considered
The results in the RM group suggested that the evening as preliminary. However, we would like to emphasize that
dosing of omeprazole could decrease the influence of the risk of attenuation of clopidogrel by a PPI depends on
omeprazole on the efficacy of clopidogrel dosed in the CYP2C19 genotype status. Therefore, we believe that the
morning. However, as shown in the present study, the RMs testing of CYP2C19 genotype could contribute to the
rarely became non-responders even if clopidogrel was development of tailored optimal anti-platelet therapy.
390 / 70:3 / Br J Clin Pharmacol
Influence of PPIs on clopidogrel and CYP2C19 genotypes
However, a further large scale study is necessary to verify Hlatky MA, Kaul S, Lindner JR, Moliterno DJ, Mukherjee D,
the clinical usefulness of CYP2C19 genotyping in anti- Schofield RS, Rosenson RS, Stein JH, Weitz HH, Wesley DJ.
platelet therapy. ACCF/ACG/AHA 2008 expert consensus document on
reducing the gastrointestinal risks of antiplatelet therapy
and NSAID use. Am J Gastroenterol 2008; 103: 2890–907.
Competing interests 10 Bhatt DL, Scheiman J, Abraham NS, Antman EM, Chan FK,
Furberg CD, Johnson DA, Mahaffey KW, Quigley EM,
Harrington RA, Bates ER, Bridges CR, Eisenberg MJ, Ferrari VA,
There are no competing interests to declare.
Hlatky MA, Kaul S, Lindner JR, Moliterno DJ, Mukherjee D,
This work was supported by a grant-in-aid from the Min- Schofield RS, Rosenson RS, Stein JH, Weitz HH, Wesley DJ.
istry of Education, Culture, Sports, Science and Technology of ACCF/ACG/AHA 2008 expert consensus document on
Japan (20590718). We thank the staff at the Translational reducing the gastrointestinal risks of antiplatelet therapy
Research Unit, Ms Takako Toyoda, Ms Yoko Akahori, Ms Yumi and NSAID use: a report of the American College of
Kiyama, Ms Keiko Arasawa, Ms Saori Oikawa and Ms Naomi Cardiology Foundation Task Force on Clinical Expert
Hashimoto for their help. Consensus Documents. J Am Coll Cardiol 2008; 52: 1502–17.
11 Umemura K, Furuta T, Kondo K. The common gene variants
of CYP2C19 affect pharmacokinetics and
pharmacodynamics in an active metabolite of clopidogrel in
healthy subjects. J Thromb Haemost 2008; 6: 1439–41.
REFERENCES
12 Stedman CA, Barclay ML. Review article: comparison of the
1 Cattaneo M. Aspirin and clopidogrel: efficacy, safety, and the pharmacokinetics, acid suppression and efficacy of proton
issue of drug resistance. Arterioscler Thromb Vasc Biol 2004; pump inhibitors. Aliment Pharmacol Ther 2000; 14: 963–78.
24: 1980–7.
13 Juurlink DN, Gomes T, Ko DT, Szmitko PE, Austin PC, Tu JV,
2 Derry S, Loke YK. Risk of gastrointestinal haemorrhage with Henry DA, Kopp A, Mamdani MM. A population-based study
long term use of aspirin: meta-analysis. BMJ 2000; 321: of the drug interaction between proton pump inhibitors
1183–7. and clopidogrel. CMAJ 2009; 180: 713–18.
3 Chan FK, Ching JY, Hung LC, Wong VW, Leung VK, Kung NN, 14 Ho PM, Maddox TM, Wang L, Fihn SD, Jesse RL, Peterson ED,
Hui AJ, Wu JC, Leung WK, Lee VW, Lee KK, Lee YT, Lau JY, Rumsfeld JS. Risk of adverse outcomes associated with
To KF, Chan HL, Chung SC, Sung JJ. Clopidogrel versus concomitant use of clopidogrel and proton pump inhibitors
aspirin and esomeprazole to prevent recurrent ulcer following acute coronary syndrome. JAMA 2009; 301:
bleeding. N Engl J Med 2005; 352: 238–44. 937–44.
4 Hallas J, Dall M, Andries A, Andersen BS, Aalykke C, 15 Toth PP, Armani A. Thienopyridine therapy and risk for
Hansen JM, Andersen M, Lassen AT. Use of single and cardiovascular events in secondary prevention. Curr
combined antithrombotic therapy and risk of serious upper Atheroscler Rep 2009; 11: 364–70.
gastrointestinal bleeding: population based case-control 16 Siller-Matula JM, Spiel AO, Lang IM, Kreiner G, Christ G,
study. BMJ 2006; 333: 726. Jilma B. Effects of pantoprazole and esomeprazole on
5 Awtry EH, Loscalzo J. Aspirin. Circulation 2000; 101: 1206–18. platelet inhibition by clopidogrel. Am Heart J 2009; 157: 148
e1–5.
6 Taha AS, Angerson WJ, Knill-Jones RP, Blatchford O. Upper
gastrointestinal haemorrhage associated with low-dose 17 Ishizaki T, Horai Y. Review article: cytochrome P450 and the
aspirin and anti-thrombotic drugs – a 6-year analysis and metabolism of proton pump inhibitors – emphasis on
comparison with non-steroidal anti-inflammatory drugs. rabeprazole. Aliment Pharmacol Ther 1999; 13 (Suppl. 3):
Aliment Pharmacol Ther 2005; 22: 285–9. 27–36.
7 Nakayama M, Iwakiri R, Hara M, Ootani H, Shimoda R, 18 Malek LA, Kisiel B, Spiewak M, Grabowski M, Filipiak KJ,
Tsunada S, Sakata H, Fujimoto K. Low-dose aspirin is a Kostrzewa G, Huczek Z, Ploski R, Opolski G. Coexisting
prominent cause of bleeding ulcers in patients who polymorphisms of P2Y12 and CYP2C19 genes as a risk factor
underwent emergency endoscopy. J Gastroenterol 2009; 44: for persistent platelet activation with clopidogrel. Circ J
912–18. 2008; 72: 1165–9.
8 Bhatt DL, Scheiman J, Abraham NS, Antman EM, Chan FK, 19 Simon T, Verstuyft C, Mary-Krause M, Quteineh L, Drouet E,
Furberg CD, Johnson DA, Mahaffey KW, Quigley EM. Meneveau N, Steg PG, Ferrieres J, Danchin N, Becquemont L.
ACCF/ACG/AHA 2008 expert consensus document on Genetic determinants of response to clopidogrel and
reducing the gastrointestinal risks of antiplatelet therapy cardiovascular events. N Engl J Med 2009; 360: 363–75.
and NSAID use: a report of the American College of 20 Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT,
Cardiology Foundation Task Force on Clinical Expert Walker JR, Antman EM, Macias W, Braunwald E, Sabatine MS.
Consensus Documents. Circulation 2008; 118: 1894–909. Cytochrome P-450 polymorphisms and response to
clopidogrel. N Engl J Med 2009; 360: 354–62.
9 Bhatt DL, Scheiman J, Abraham NS, Antman EM, Chan FK,
Furberg CD, Johnson DA, Mahaffey KW, Quigley EM, 21 Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT,
Harrington RA, Bates ER, Bridges CR, Eisenberg MJ, Ferrari VA, Walker JR, Antman EM, Macias WL, Braunwald E,
Br J Clin Pharmacol / 70:3 / 391
T. Furuta et al.
Sabatine MS. Cytochrome P450 genetic polymorphisms and on post-interventional residual platelet aggregation in
the response to prasugrel: relationship to pharmacokinetic, patients undergoing coronary stenting treated by dual
pharmacodynamic, and clinical outcomes. Circulation 2009; antiplatelet therapy. Thromb Res 2010; 125: e51–4.
119: 2553–60.
31 O’Donoghue ML, Braunwald E, Antman EM, Murphy SA,
22 Collet JP, Hulot JS, Pena A, Villard E, Esteve JB, Silvain J, Bates ER, Rozenman Y, Michelson AD, Hautvast RW,
Payot L, Brugier D, Cayla G, Beygui F, Bensimon G, Ver Lee PN, Close SL, Shen L, Mega JL, Sabatine MS,
Funck-Brentano C, Montalescot G. Cytochrome P450 2C19 Wiviott SD. Pharmacodynamic effect and clinical efficacy of
polymorphism in young patients treated with clopidogrel clopidogrel and prasugrel with or without a proton-pump
after myocardial infarction: a cohort study. Lancet 2009; 373: inhibitor: an analysis of two randomised trials. Lancet 2009;
309–17. 374: 989–97.
23 Furuta T, Sagehashi Y, Shirai N, Sugimoto M, Nakamura A,
32 Rassen JA, Choudhry NK, Avorn J, Schneeweiss S.
Kodaira M, Kenmotsu K, Nagano M, Egashira T, Ueda K,
Cardiovascular outcomes and mortality in patients using
Yoneyama M, Ohashi K, Ishizaki T, Hishida A. Influence of
clopidogrel with proton pump inhibitors after percutaneous
CYP2C19 polymorphism and Helicobacter pylori genotype
coronary intervention or acute coronary syndrome.
determined from gastric tissue samples in response to triple
Circulation 2009; 120: 2322–9.
therapy for H. pylori Infection. Clin Gastroenterol Hepatol
2005; 3: 564–73. 33 Hagihara K, Kazui M, Kurihara A, Yoshiike M, Honda K,
24 Sim SC, Risinger C, Dahl ML, Aklillu E, Christensen M, Okazaki O, Farid NA, Ikeda T. A possible mechanism of the
Bertilsson L, Ingelman-Sundberg M. A common novel differences in efficiency and variability of active metabolite
CYP2C19 gene variant causes ultrarapid drug metabolism formation from thienopyridine antiplatelet agents, prasugrel
relevant for the drug response to proton pump inhibitors and clopidogrel. Drug Metab Dispos 2009; 37: 2145–52.
and antidepressants. Clin Pharmacol Ther 2006; 79: 103–13. 34 Furuta T, Ohashi K, Kosuge K, Zhao XJ, Takashima M,
25 Geisler T, Langer H, Wydymus M, Gohring K, Zurn C, Kimura M, Nishimoto M, Hanai H, Kaneko E, Ishizaki T.
Bigalke B, Stellos K, May AE, Gawaz M. Low response to CYP2C19 genotype status and effect of omeprazole on
clopidogrel is associated with cardiovascular outcome after intragastric pH in humans. Clin Pharmacol Ther 1999; 65:
coronary stent implantation. Eur Heart J 2006; 27: 2420–5. 552–61.
26 Hoshino K, Horiuchi H, Tada T, Tazaki J, Nishi E, Kawato M, 35 Shirai N, Furuta T, Xiao F, Kajimura M, Hanai H, Ohashi K,
Ikeda T, Yamamoto H, Akao M, Furukawa Y, Shizuta S, Ishizaki T. Comparison of lansoprazole and famotidine for
Toma M, Tamura T, Saito N, Doi T, Ozasa N, Jinnai T, gastric acid inhibition during the daytime and night-time in
Takahashi K, Watanabe H, Yoshikawa Y, Nishimoto N, different CYP2C19 genotype groups. Aliment Pharmacol
Ouchi C, Morimoto T, Kita T, Kimura T. Clopidogrel resistance Ther 2002; 16: 837–46.
in Japanese patients scheduled for percutaneous coronary
intervention. Circ J 2009; 73: 336–42. 36 Sugimoto M, Furuta T, Shirai N, Kajimura M, Hishida A,
Sakurai M, Ohashi K, Ishizaki T. Different dosage regimens of
27 Sibbing D, Morath T, Stegherr J, Braun S, Vogt W, rabeprazole for nocturnal gastric acid inhibition in relation
Hadamitzky M, Schomig A, Kastrati A, von Beckerath N. to cytochrome P450 2C19 genotype status. Clin Pharmacol
Impact of proton pump inhibitors on the antiplatelet effects Ther 2004; 76: 290–301.
of clopidogrel. Thromb Haemost 2009; 101: 714–19.
37 Diaz D, Fabre I, Daujat M, Saint Aubert B, Bories P, Michel H,
28 Gilard M, Arnaud B, Cornily JC, Le Gal G, Lacut K, Le Calvez G,
Maurel P. Omeprazole is an aryl hydrocarbon-like inducer of
Mansourati J, Mottier D, Abgrall JF, Boschat J. Influence of
human hepatic cytochrome P450. Gastroenterology 1990;
omeprazole on the antiplatelet action of clopidogrel
99: 737–47.
associated with aspirin: the randomized, double-blind OCLA
(Omeprazole CLopidogrel Aspirin) study. J Am Coll Cardiol 38 Taha AS, McCloskey C, Prasad R, Bezlyak V. Famotidine for
2008; 51: 256–60. the prevention of peptic ulcers and oesophagitis in patients
29 Small DS, Farid NA, Payne CD, Weerakkody GJ, Li YG, taking low-dose aspirin (FAMOUS): a phase III, randomised,
Brandt JT, Salazar DE, Winters KJ. Effects of the proton pump double-blind, placebo-controlled trial. Lancet 2009; 374:
inhibitor lansoprazole on the pharmacokinetics and 119–25.
pharmacodynamics of prasugrel and clopidogrel. J Clin
39 Yasuda H, Yamada M, Sawada S, Endo Y, Inoue K, Asano F,
Pharmacol 2008; 48: 475–84.
Takeyama Y, Yoshiba M. Upper gastrointestinal bleeding in
30 Zuern CS, Geisler T, Lutilsky N, Winter S, Schwab M, Gawaz M. patients receiving dual antiplatelet therapy after coronary
Effect of comedication with proton pump inhibitors (PPIs) stenting. Intern Med 2009; 48: 1725–30.
392 / 70:3 / Br J Clin Pharmacol
You might also like
- Clopidogrel Pharmacogenetics: Metabolism and Drug InteractionsDocument7 pagesClopidogrel Pharmacogenetics: Metabolism and Drug InteractionsUmmuNo ratings yet
- Interaksi Obat Antara Klopidogrel Dan Proton Pump Inhibitor (PPI)Document5 pagesInteraksi Obat Antara Klopidogrel Dan Proton Pump Inhibitor (PPI)Xena Poetri Xaverya RenggaNo ratings yet
- Effect of Omeprazole On The Metabolism of Cilostazol: Ajit Suri and Steven L. BramerDocument7 pagesEffect of Omeprazole On The Metabolism of Cilostazol: Ajit Suri and Steven L. BramerNurul Kamilah SadliNo ratings yet
- The Relationship Between Clinical Pharmacokinetics of Aripiprazole and CYP2D6 Genetic Polymorphism: Effects of CYP Enzyme Inhibition by Coadministration of Paroxetine or FluvoxamineDocument9 pagesThe Relationship Between Clinical Pharmacokinetics of Aripiprazole and CYP2D6 Genetic Polymorphism: Effects of CYP Enzyme Inhibition by Coadministration of Paroxetine or FluvoxamineIulia CiocotisanNo ratings yet
- Clinical Application of CYP2C19 Pharmacogenetics Toward More Personalized MedicineDocument7 pagesClinical Application of CYP2C19 Pharmacogenetics Toward More Personalized MedicineGisela GloryNo ratings yet
- Review Article: Cytochrome P450 and The Metabolism of Proton Pump Inhibitors Ð Emphasis On RabeprazoleDocument10 pagesReview Article: Cytochrome P450 and The Metabolism of Proton Pump Inhibitors Ð Emphasis On RabeprazoleRoxana Magaly Chavez PillacaNo ratings yet
- Pengaruh Variasi Genetika Cyp2c19 Terhadap Efek Sedasi Midazolam IntravenaDocument8 pagesPengaruh Variasi Genetika Cyp2c19 Terhadap Efek Sedasi Midazolam Intravenasriokta dinaNo ratings yet
- Articles: Drug-Drug Interaction Between Clopidogrel and The Proton Pump InhibitorsDocument9 pagesArticles: Drug-Drug Interaction Between Clopidogrel and The Proton Pump InhibitorsLina WatilubisNo ratings yet
- Omeprazole PDFDocument8 pagesOmeprazole PDFRafael SyfuNo ratings yet
- Anticoagulacion 2Document9 pagesAnticoagulacion 2Annette ChavezNo ratings yet
- ClopidogrelDocument3 pagesClopidogrellorien86No ratings yet
- Inaba 2010Document11 pagesInaba 2010Eduardo GirónNo ratings yet
- Clopidogrel X OmeprazolDocument10 pagesClopidogrel X OmeprazolFabiana SottamNo ratings yet
- Antiplatelet Therapy in Flow Diversion-2019Document6 pagesAntiplatelet Therapy in Flow Diversion-2019ariNo ratings yet
- Resistant Prolactinomas: Short ReviewDocument5 pagesResistant Prolactinomas: Short ReviewFelipe Scipiao MouraNo ratings yet
- Tardif Diskinesia PDFDocument9 pagesTardif Diskinesia PDFHandi SuntamaNo ratings yet
- Omeprazole and Clopidogrel: Should Clinicians Be Worried?: Current Drug TherapyDocument4 pagesOmeprazole and Clopidogrel: Should Clinicians Be Worried?: Current Drug TherapytriciapipayNo ratings yet
- Bupropion 4Document17 pagesBupropion 4Robert MovileanuNo ratings yet
- Effects of The Proton Pump Inhibitor Lansoprazole On The Pharmacokinetics and Pharmacodynamics ofDocument11 pagesEffects of The Proton Pump Inhibitor Lansoprazole On The Pharmacokinetics and Pharmacodynamics ofLuciana OliveiraNo ratings yet
- Pharmacodynamic Evaluation of Pantoprazole Therapy On Clopidogrel EffectsDocument7 pagesPharmacodynamic Evaluation of Pantoprazole Therapy On Clopidogrel EffectsOk bro I am doneNo ratings yet
- New Drugs and Technologies: PrasugrelDocument10 pagesNew Drugs and Technologies: PrasugrelDewi FitrianaNo ratings yet
- More Details Regarding EvaneotrimDocument6 pagesMore Details Regarding Evaneotrimsalwa meraNo ratings yet
- Mot Ilium TabDocument11 pagesMot Ilium TabChandra FatmaNo ratings yet
- Clinical Pharmacokinetics of Clomipramine: Drug DispositionDocument16 pagesClinical Pharmacokinetics of Clomipramine: Drug DispositionElinaNo ratings yet
- Pharmacogenomix SpsDocument31 pagesPharmacogenomix SpsShyamaprasad SahaNo ratings yet
- Pantosec 40mg HeteroDocument2 pagesPantosec 40mg Heteroopto careNo ratings yet
- Ability To Establish The Repercussions of Particularly Inhibiting PDK1 Action in A Temporal and Reversible Method.20130222.170241Document2 pagesAbility To Establish The Repercussions of Particularly Inhibiting PDK1 Action in A Temporal and Reversible Method.20130222.170241grouse4sudanNo ratings yet
- ANTIPYRETICSDocument20 pagesANTIPYRETICSJoshua VillarbaNo ratings yet
- Cardiovascular PharmacogenomicsDocument51 pagesCardiovascular PharmacogenomicsNemer EzzeddineNo ratings yet
- Night Time Gastric Acid Suppression by Tegoprazan Compared To Vonoprazan orDocument9 pagesNight Time Gastric Acid Suppression by Tegoprazan Compared To Vonoprazan orDhruvin KapadiaNo ratings yet
- FullDocument9 pagesFullbravohr98No ratings yet
- Clopidogrel-Drug Interactions: Eric R. Bates, MD, Wei C. Lau, MD, Dominick J. Angiolillo, MD, P DDocument13 pagesClopidogrel-Drug Interactions: Eric R. Bates, MD, Wei C. Lau, MD, Dominick J. Angiolillo, MD, P DAyu ApriliantiNo ratings yet
- Genetic Polymorphism of CYP2C19 & Therapeutic Response To Proton Pump InhibitorsDocument10 pagesGenetic Polymorphism of CYP2C19 & Therapeutic Response To Proton Pump Inhibitorsbravohr98No ratings yet
- Antiplatelet Pada ACSDocument22 pagesAntiplatelet Pada ACSRidyah Ning TyasNo ratings yet
- JCPH 95Document8 pagesJCPH 95Diva HapsariNo ratings yet
- PHARMACOGENOMICSDocument10 pagesPHARMACOGENOMICSNicole AguilarNo ratings yet
- Rena2013 Article MolecularMechanismOfActionOfMeDocument9 pagesRena2013 Article MolecularMechanismOfActionOfMeDian Fitri ChairunnisaNo ratings yet
- Weiss2009 PDFDocument7 pagesWeiss2009 PDFLuisAlbertoGtzMtzNo ratings yet
- Effects of Fluvoxamine On Lansoprazole Pharmacokinetics in Relation To CYP2C19 GenotypesDocument8 pagesEffects of Fluvoxamine On Lansoprazole Pharmacokinetics in Relation To CYP2C19 GenotypesLuciana OliveiraNo ratings yet
- Tegoprazan Vs Vonoprazan or Esomeprazole For Night Time Gastric Acid SuppressionDocument9 pagesTegoprazan Vs Vonoprazan or Esomeprazole For Night Time Gastric Acid SuppressionMeggy ParrenoNo ratings yet
- 1123 FullDocument6 pages1123 FullasmanNo ratings yet
- Important Questions of Pharmacology by Medical Study CenterDocument10 pagesImportant Questions of Pharmacology by Medical Study CenterLin YunNo ratings yet
- JPM 08 00001 v2Document31 pagesJPM 08 00001 v2احمد صباح مالكNo ratings yet
- Tramadol Pregabalin InteractionDocument9 pagesTramadol Pregabalin InteractionnicolaslolxNo ratings yet
- MainDocument8 pagesMainAry MadinaNo ratings yet
- Dias2009 Article PantoprazoleDocument10 pagesDias2009 Article PantoprazoleTan JayNo ratings yet
- Pharmacology A Pharmacogenomics SummaryDocument4 pagesPharmacology A Pharmacogenomics SummaryarvinkennethdelacruzNo ratings yet
- TCM PharmacologyDocument3 pagesTCM Pharmacologypj9066No ratings yet
- Metoprolol Shortage March 2009Document3 pagesMetoprolol Shortage March 2009Moisés PonceNo ratings yet
- Dopamine Agonists: Barrow Neurological Institute, Phoenix, Arizona, U.S.ADocument17 pagesDopamine Agonists: Barrow Neurological Institute, Phoenix, Arizona, U.S.Aelenac67No ratings yet
- Loperamide: Article OutlineDocument10 pagesLoperamide: Article OutlineRama Biomantara0% (1)
- NewInsights Into The Use of Empagliflozin-A Comprehensive ReviewDocument21 pagesNewInsights Into The Use of Empagliflozin-A Comprehensive ReviewLu MVNo ratings yet
- Final Draft EsomeprazoleDocument4 pagesFinal Draft EsomeprazoleHassan Raza GilalNo ratings yet
- Interaction Between Statins and Clopidogrel Is TheDocument12 pagesInteraction Between Statins and Clopidogrel Is TheAnisa ArmadaniNo ratings yet
- A Naturally Occurring Isoform-Specific Probe For Highly Selective and Sensitive Detection of Human Cytochrome P450 3A5Document10 pagesA Naturally Occurring Isoform-Specific Probe For Highly Selective and Sensitive Detection of Human Cytochrome P450 3A5陈梓强No ratings yet
- AMPT-induced Monoamine Depletion in Humans: Evaluation of Two Alternative (123I) IBZM SPECT ProceduresDocument7 pagesAMPT-induced Monoamine Depletion in Humans: Evaluation of Two Alternative (123I) IBZM SPECT ProceduresMihaela ToaderNo ratings yet
- Pharm Imp. ShakilDocument40 pagesPharm Imp. ShakilABCNo ratings yet
- Restoril™ (Temazepam) Capsules USP RX Only Warning: Risks From Concomitant Use With OpioidsDocument14 pagesRestoril™ (Temazepam) Capsules USP RX Only Warning: Risks From Concomitant Use With OpioidsLeslie CitromeNo ratings yet
- The First Time Design of Cancer Nutrition as Specific to Treatment with Its Mega Analysis, Potential, Benefits, and DrawbacksFrom EverandThe First Time Design of Cancer Nutrition as Specific to Treatment with Its Mega Analysis, Potential, Benefits, and DrawbacksNo ratings yet
- Nihms 746781Document8 pagesNihms 746781rosianaNo ratings yet
- SocialDocument20 pagesSocialrosianaNo ratings yet
- 1 s2.0 S1015958416302019 MainDocument6 pages1 s2.0 S1015958416302019 MainrosianaNo ratings yet
- Nihms 906783Document26 pagesNihms 906783rosianaNo ratings yet
- Nihms 709743Document30 pagesNihms 709743rosianaNo ratings yet
- Ijms 20 04564Document17 pagesIjms 20 04564rosianaNo ratings yet
- Paper Environmental Risk of Cancer (Lectura)Document7 pagesPaper Environmental Risk of Cancer (Lectura)Claudio ManríquezNo ratings yet
- Jurnal fk2Document17 pagesJurnal fk2rosianaNo ratings yet
- Faktor Io ElderlyDocument3 pagesFaktor Io ElderlyrosianaNo ratings yet
- Parenteral Drug InteractionDocument4 pagesParenteral Drug InteractionrosianaNo ratings yet
- The Causes of Prescribing Errors in English General PracticesDocument8 pagesThe Causes of Prescribing Errors in English General PracticesrosianaNo ratings yet
- Parenteral Drug InteractionDocument4 pagesParenteral Drug InteractionrosianaNo ratings yet
- Io Pediatric-PolifarmasiDocument18 pagesIo Pediatric-PolifarmasirosianaNo ratings yet
- Potential Risks of Pharmacy CompoundingDocument8 pagesPotential Risks of Pharmacy CompoundingElizabeth CollinsNo ratings yet
- Jurnal 6Document11 pagesJurnal 6rosianaNo ratings yet
- FDocument59 pagesFDiannelis UgasNo ratings yet
- Stabilitas Ampi-Lipid EmulsDocument12 pagesStabilitas Ampi-Lipid EmulsrosianaNo ratings yet
- Clinical Nutrition and Drug InteractionDocument10 pagesClinical Nutrition and Drug InteractionDhigna LuthfiyaniNo ratings yet
- Jurnal 5Document7 pagesJurnal 5rosianaNo ratings yet
- Ppi y 1Document11 pagesPpi y 1Nurul Kamilah SadliNo ratings yet
- Cipro-Parenteral NutrisiDocument13 pagesCipro-Parenteral NutrisirosianaNo ratings yet
- Jurnal 7Document9 pagesJurnal 7rosianaNo ratings yet
- Jurnal 6Document11 pagesJurnal 6rosianaNo ratings yet
- Bushra, 2010Document7 pagesBushra, 2010Citta ArastiNo ratings yet
- Foods: Food-Drug Interactions With Fruit JuicesDocument14 pagesFoods: Food-Drug Interactions With Fruit JuicesrosianaNo ratings yet
- Customised in Vitro Model To Detect Human Metabolism Dependent Idiosyncratic Drug Induced Liver InjuryDocument17 pagesCustomised in Vitro Model To Detect Human Metabolism Dependent Idiosyncratic Drug Induced Liver InjuryrosianaNo ratings yet
- Jurnal 2Document7 pagesJurnal 2rosianaNo ratings yet
- Role of Food Drug Interactions in Neurological and Psychological DiseasesDocument11 pagesRole of Food Drug Interactions in Neurological and Psychological DiseasesSiscaNo ratings yet
- Individualized Medicine: Sex, Hormones, Genetics, and Adverse Drug ReactionsDocument9 pagesIndividualized Medicine: Sex, Hormones, Genetics, and Adverse Drug ReactionsrosianaNo ratings yet
- Reverse TsaDocument4 pagesReverse Tsaprwill00No ratings yet
- History of Powerlifting Warpeha 9-4-15Document19 pagesHistory of Powerlifting Warpeha 9-4-15Treinador Bruno FerreiraNo ratings yet
- AnemiaDocument40 pagesAnemiaRajaNo ratings yet
- Emergency Psychiatry Other Than Suicide: Dr. Pooja Singh, MD Assistant ProfessorDocument45 pagesEmergency Psychiatry Other Than Suicide: Dr. Pooja Singh, MD Assistant Professorpooja singhNo ratings yet
- Application Technique Traction PDFDocument25 pagesApplication Technique Traction PDFAZOZ 19No ratings yet
- GUY Et Al 1994 - Regulation of Colostrum Formation in Beef and Dairy CowsDocument6 pagesGUY Et Al 1994 - Regulation of Colostrum Formation in Beef and Dairy CowsMonique IndNo ratings yet
- Lavender Lavender Lavender Lavender Lavender Lavender: UrineDocument3 pagesLavender Lavender Lavender Lavender Lavender Lavender: UrineJonathan A. Sarmiento67% (6)
- Comparison of Two Approaches ofDocument96 pagesComparison of Two Approaches ofJacob OrtizNo ratings yet
- Arq AmberDocument4 pagesArq AmberMaqsood AnsariNo ratings yet
- List Alat OK Mayor Dan Minor 30 07 2022 20.12Document72 pagesList Alat OK Mayor Dan Minor 30 07 2022 20.12dehaaNo ratings yet
- Rosary Med BottleDocument2 pagesRosary Med BottlescrugglenampNo ratings yet
- Autonomic Nervous System: Rodina Rivera-Gorospe, M.DDocument44 pagesAutonomic Nervous System: Rodina Rivera-Gorospe, M.DPogo LocoNo ratings yet
- Effects of AntidepressantsDocument204 pagesEffects of AntidepressantsAMCArroyoNo ratings yet
- Mental Status ExamDocument10 pagesMental Status ExamSrini VoruNo ratings yet
- LT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewDocument3 pagesLT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewfatimaNo ratings yet
- Acog Embarazo Gemelar 2004 PDFDocument15 pagesAcog Embarazo Gemelar 2004 PDFEliel MarcanoNo ratings yet
- Carrubba Botanical Guide RDocument247 pagesCarrubba Botanical Guide Rafridikhanjan100% (3)
- Multidisciplinary Management of Female Pelvic Floor DisordersDocument336 pagesMultidisciplinary Management of Female Pelvic Floor DisordersJuan Jose Sardi100% (3)
- Final Abstract and Paper Edit 26 April 2020 อ เปรม แก้แล้ว PDFDocument22 pagesFinal Abstract and Paper Edit 26 April 2020 อ เปรม แก้แล้ว PDFchanakarn Vipusmith100% (2)
- BIODDocument5 pagesBIODJedan TopiagonNo ratings yet
- Tea CaffeineDocument3 pagesTea CaffeinedigitaltextNo ratings yet
- Get in Shape Month2Document5 pagesGet in Shape Month2Caroline Sandry100% (1)
- J&J CompanyDocument127 pagesJ&J CompanyRam TyagiNo ratings yet
- The Morrison Technique: A Free-Hand Method For Capturing Photomicrographs Using A SmartphoneDocument3 pagesThe Morrison Technique: A Free-Hand Method For Capturing Photomicrographs Using A SmartphoneGamal DawoodNo ratings yet
- Jurnal OnlineDocument5 pagesJurnal OnlineWireifnitedNo ratings yet
- Legg-Calvé-Perthes Disease: Roberto E. Novo, DVM, DACVSDocument2 pagesLegg-Calvé-Perthes Disease: Roberto E. Novo, DVM, DACVSEdi BackyNo ratings yet
- EMQDocument12 pagesEMQWaleed Mohamed AhmedNo ratings yet
- Home Private ServiceDocument4 pagesHome Private ServiceTubagus Adil AL AminNo ratings yet
- Multicare MC in ManualDocument28 pagesMulticare MC in ManualTom TamponNo ratings yet
- MBLEx Practice ExamsDocument268 pagesMBLEx Practice ExamsTrace Thuma100% (9)