Professional Documents
Culture Documents
Hypothyroidism, The Main Thyroid Dysfunction in Iranian Patients With Myasthenia Gravis: A Case Serie
Uploaded by
Fitria ChandraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hypothyroidism, The Main Thyroid Dysfunction in Iranian Patients With Myasthenia Gravis: A Case Serie
Uploaded by
Fitria ChandraCopyright:
Available Formats
Iranian Journal Original Paper
of Neurology Ir J neurol 2011; 10(1-2): 22-25
Hypothyroidism, the main thyroid
dysfunction in Iranian patients with
myasthenia gravis: A case serie Received: 23 Aug 2010
Accepted: 26 Nov 2010
Mansoureh Mamarabadi1, Hadie Razjouyan1,2,3, Mehdi Moghaddasi1
1
Department of Neurology, Rasool-e-Akram Hospital, Tehran University of Medical Sciences, Tehran, Iran
2
Iranian Centre of Neurological Researches, Imam Khomeini Hospital, Tehran University of Medical Sciences, Tehran, Iran
3
Cancer Center, Howard University Hospital, Rm#522 2041 Georgia Ave., Washington DC 20059, USA
Keywords years (P: N.S.), respectively. In addition, once the MG
Thyroid Disease; Myasthenia Gravis; AChR Ab patients are younger than 50, female gender is
dominant while they are more than fifty, male is the
dominant gender.
Abstract Conclusion: Our results show that Iranian patients with
Background: Several concomitant disorders especially MG tend to be female and young. Before sixth decade of
thyroid abnormalities have been reported in patients with life, women are the most presenting patients thereafter,
myasthenia gravis (MG). We aimed to estimate the men are the predominant gender. About 7 percent of
frequency and pattern of thyroid disorders in Iranian them may suffer from concomitant thyroid problem
patients with MG. especially hypothyroidism.
Methods: All consecutive patients with MG referred to
neurology clinic of Rasool-e-Akram Hospital during 2006- Introduction
2007 were enrolled. All patients underwent clinical Myasthenia Gravis (MG) has been considered as a disease
assessment of thyroid gland as well as thyroid function test. once Thomas Willis described a woman with dysarthria in
AChR Ab titer was measured as well. Nerve conduction 1672, and is a prototype of both synaptic and autoimmune
study (NCS), Electromyography (EMG), and Repetitive Nerve disorders. In most patients, auto-antibodies against the
Stimulation (RNS) was done by a same neurologist. The nicotinic acetylcholine receptor (AChR) are the cause and
diagnosis of MG was made on the basis of clinical concentrate at the post-synaptic region of the
examinations, an edrophonium chloride test and neuromuscular junction [1].
electrophysiological studies. The diagnosis of thyroid Although MG is rare, epidemiological evidences
disorders were based on clinical presentation as well as suggest that frequency of MG is increasing over time,
thyroid function tests. likely due to either improvements in diagnosis or a true
Results: Fifty eight patients (mean age [SD]: 37.1 [16.9], increase of disease frequency. Recent prevalence rates for
range: 10-80; female: 65.5%) were enrolled in this 12-month MG approach 20/ 100,000 [2]. Earlier point prevalence
study. Four patients (6.9%) had abnormal thyroid function rates varied between 0.5 and 15 per 100,000 [3-5]. In
tests (Hypothyroidism: 3 [5.2%]; 4 females; 3 with western countries, a wide range of incidence has been
hypothyroidism and 1 with hyperthyroidism). The mean age reported with an estimate of about 2.0 to 10.4/million/year
(SD) in men and women were 41.4 (21.3) and 34.9 (13.8) in Virginia to 21.27/million/year in Barcelona, Spain [6,7].
Iranian Journal of Neurology Corresponding Author: Mehdi Moghaddasi, MD
Department of Neurology, Rasool-e-Akram Hospital, Tehran
Email: ijnl@tums.ac.ir University of Medical Sciences, Niayesh St., Sattar-Khan Ave.,
http://ijnl.tums.ac.ir Tehran 144561-3131, Iran
Email: moghaddasim@irimc.org
There has been proposed an interaction between MG and Materials and Methods
demographic features of the disease. Studies showed that All the subjects of present observational, descriptive,
the onset of MG is influenced by gender and age in a cross-sectional study were recruited consecutively from
bimodal fashion. For instance in patients younger than 40, Rasool-e-Akram hospital affiliated to Tehran University of
women gender predominates (female/male: 7/3). In the fifth Medical Sciences. All patients with MG referred to
decade, new cases of MG are evenly distributed between neurology clinic during 2006-2007 were enrolled and
men and women. After age 50, new cases of MG are detailed questionnaire including age, gender, thyroid
slightly more common in men with male/female ratio of 3/2 disease and MG presentation were filled out for each
(8-10). It seems that future prevalence of the disease will be subject. All of them underwent clinical assessment of
affected by the spontaneous remission rate (20%) and the thyroid gland as well as thyroid function test (Thyroid
fact that without treatment a further 20–30% will die within Stimulating Hormone, TSH; Free thyroxine, FT4;
10 years [4,5]. triiodothyronine, T3). AChR-Ab titer was measured in all
The thyroid gland is essential for normal human the patients at screening. Nerve conduction study (NCS),
development and maintenance. In most situations, however, Electromyography (EMG), and Repetitive Nerve
the presentations of thyroid disease are insidious, and include Stimulation (RNS) was done by a same neurologist. The
many neurological manifestations [11]. For the first time in study was approved by ethical committee of Tehran
1908 Rennie G. described the association of Graves’ disease, University of Medical Sciences and all patients were
GD with MG [12]. Since then, this association has often been informed of the study and provided their written consent
reported [11,13-17]. Although the pathogenic link between before participating in the study.
these two autoimmune diseases remains unclear, but an The diagnosis of MG was made on the basis of clinical
immunological cross-reactivity between neuromuscular examinations, an edrophonium chloride test where
junction and thyroid components was found in overlapping necessary, and electrophysiological studies. The diagnoses
GD and MG [18]. of thyroid disorder were based on clinical presentation as
Clinical and experimental findings from the 1970s well as thyroid function tests.
showed that MG can be an autoimmune disease, the ideas Quantitative variables were expressed as mean (SD).
that have been applied to other autoimmune disorders of the Chai-Square test and t-test were used for qualitative and
neuromuscular junction [19,20]. Patients with MG may have quantitative data, respectively. Non parametric tests were
evidence of coexisting autoimmune thyroid disease (AITD) used where appropriate. A P value of less than 0.05 was
[12,21-24] as well as other autoimmune disorders like type 1 considered significant. All calculations were performed
diabetes mellitus, primary hypogonadism, pernicious anemia, with the SPSS Version 16.0 for Windows (SPSS Inc.,
and adrenal insufficiency, generally referred as the Chicago, Illinois, USA).
polyglandular syndrome [26]. The rates of autoimmune
diseases association with MG in a Norwegian and Danish Results
studies were 22.9% and 9.4%, respectively [13,26]. The Fifty eight patients with mean age (SD) of 37.1 (16.9)
Danish study has also shown that AITDs such as Graves’ years were enrolled in this twelve- month study. Thirty
disease and Hashimoto’s thyroiditis are most frequently eight of them were women (65.5%). The clinical and
associated disease with MG [13]. Other epidemiological paraclinical findings of the enrolled patients are depicted
studies showed that AITD occur in approximately 5-10% of in table 1. Four patients (6.9 %) had abnormal thyroid
MG patients and GD is the commonest AITD associated with
function test among whom, 3 cases had hypothyroidism
MG and both GD and MG are more common in females [27,
(5.2%). All patients who had abnormal thyroid function
28]. In a series of consecutive Japanese patients with MG,
tests were female and the only one who had
associated autoimmune diseases were found in 19.7% of
hyperthyroidism was a 37 year old female.
them, among which GD (7.7%) and Hashimoto’s thyroiditis
The mean age (SD) of men and women were 41.4
(4.2%) were predominant [25].
(21.3) and 34.9 (13.8) years (P: N.S.), respectively.
The association of MG and hyperthyroidism has been
Distribution of patients’ gender regarding age
reported by many authors [11,12,25,29-37]. Various
classification is depicted in figure 1. There was a trend of
estimates place the incidence of hyperthyroidism at from 3 to
positive RNS findings as the ages increased (less than 20:
8 % in cases of MG [38]. It is generally believed that
71.4%, 20-30: 94.1%, 30-40: 93.3%, 40-50: 100%, 50-60:
hyperthyroidism is far more commonly associated with MG
100%, 60-70: 80%, ≥70: 33.3%; P value: 0.04). There was
than is hypothyroidism. However, no clear explanation has
no clinical or paraclinical presentation differences among
been offered to account for this difference. In present study
MG patients with and without thyroid function
we aimed to assess concomitant thyroid disorders in Iranian
abnormality. There was no age difference among patients
patients with MG as well understand the pattern of thyroid
with and without clinical presentations such as ocular,
abnormality in our patients
bulbar, extremities, respiratory system involvement.
Hypothyroidism and myasthenia gravis 23
Ir J neurol 2011; 10(1-2)
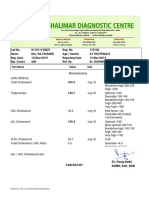
Table1. The clinical and paraclinical findings of study subjects. accordance with all studies [25,27-37] but with some [38].
In Iran legislation of salt iodization was established in
Number Percent
1994, however goiter and urinary iodine concentration
Thyroid Problem 4 6.9 remained elevated in many provinces of Iran. In 2006,
Clinic, Involvement Aminorroaya et al performed a population-based study to
Ocular 54 93.1
assess the prevalence of hypothyroidism in Isfahan, Iran.
Bulbar 50 86.2
They found that hypothyroidism was common (12.8% of
Extremities 50 86.2
Respiratory system 32 55.2 women and 4.7% of men) and probably due to
Paraclinic autoimmunity with no correlation to iodine intake [39]. It
EMG positive finding 38 65.5 seems that the higher frequency of concomitant
RNS positive finding 51 87.9 hypothyroidism may be due to endemy of hypothyroidism
NCS positive finding 0 0 in our country. However, whether this difference is due to
AchR- Ab 55 94.8 geographic distribution of thyroid problems or genetic or
environmental difference of MG among nations should be
Discussion elucidated in well structured ecologic studies.
Present study showed that mean age of the recruited MG Present study confirmed previous reports in which
patients was 37 years and women were the predominant female gender was described as the most frequent one
gender. The frequency of thyroid dysfunction was 6.9% among patients with MG [11,24,27,28,40]. In our study,
among MG patients. Moreover, hypothyroidism was the most the mean age of women with MG was lower than men
frequent thyroid dysfunction. Moreover, female gender was [35 vs. 41], however, was not statistically significant. Our
the predominant one among those who suffer from both MG study did not show gender difference in ages less than 20,
and Thyroid diseases. In addition, the predominance of however, till 60 years of age, female gender was the most
gender in ages less and more than sixty was female and male, frequent one among patients and thereafter, men were the
respectively. most common presenting gender, figure 1. These findings
Once MG disease was reported by an Oxford physician in are in accordance with previous studies [8,9,11,41,42].
1672 [1], several other case reports or series mentioned a wide Since 20-50 years is the reproductive period of women and
variety of concomitant disorders [11-17, 21-38]. Since 1970s, it before climacteric period, we hypothesize that the specific
has been proposed that MG has some autoimmune origin [10, hormonal balance may have a role in presentation of
24, 26-28]. Thereafter, several studies reported concomitant clinical features of MG patients possibly as an
diseases with autoimmune pathophysiology in MG patients exacerbating factor.
with a rate of 5 to 23% (26-28). Among them, the two Our study did not show any clinical presentation
prototypes of hypo- and hyper-thyroidism, Hashimoto and difference among MG patients with and without thyroid
Graves ’ disease, has been reported as the most common problem as well no paraclinical assessment (EMG, RNS,
concomitant disorder with MG [11,12,25,29-37]. AchR-Ab) difference was found between these two groups.
Interestingly, Hypothyroidism was the most frequent Whether these findings are pure clinical finding or a
thyroid problem among our patients. This finding is not in consequent of not having enough study subjects remain to
Female Male
80% 80.00%
75%
71.40% 67%
57.10% 70.60%
42.90%
28.60% 33%
29.40%
25%
20.00%
20%
<20 20-30 30-40 40-50 50-60 60-70 >70
Figure 1. Distribution of patients’ gender regarding their age range
24 Ir J neurol 2011; 10(1-2) Mamarabadi
be elucidated by future studies with more patients. This estimate can warn our neurologist to think of
In summary, Iranian patients with MG tend to be female concomitant thyroid disease in diagnosis and management
and young. Up to six decade of life, women are the most of patients suspicious to MG. The higher frequency of
presenting patients. Thereafter, men are the predominant hypothyroidism may be a clue to elucidate more the
gender. About 7 percent of MG patients may suffer from interaction of thyroid disorders with MG.
concomitant thyroid problem especially hypothyroidism.
References
1. Vincent A, Palace J, Hilton-Jones D. 15. Sahay BM, Blendis LM, Greene R. Relation inhibiting immunoglobulins in myasthenia
Myasthenia gravis. Lancet 2001 30; 357 between myasthenia gravis and thyroid gravis. Acta Endocrinol (Copenh) 1982;
(9274):2122-8. disease. British Medical Journal 1965; 1:762- 101:41-46.
2. Phillips LH 2nd: The epidemiology of 5. 28. Pacey SR, Belchetz PE. Grave’s disease
myasthenia gravis. Ann NY Acad Sci 2003; 16. Ohno M, Hamada N, Yamakawa J et al. associated with ocular myasthenia gravis and
998:407-412. Myasthenia gravis associated with Graves’ thymic cyst. J r Soc Med 1993; 86:297-298.
3. Oosterhuis HJ. Clinical aspects and disease in Japan. Japanese Journal of 29. Cohen, S. J., and King, F. H. Arch Neurol
epidemiology. In: Oosterhuis HJGH, ed. Medicine 1987; 26:2–6. Psychiat 1932; 28:1338.
Myasthenia gravis. Groningen: Groningen 17. Lakhal K, Blel Y, Fysekidis M, Mohammedi 30. Thorner MW. Relation of myasthenia gravis
Neurological Press 1997: 17–48. K, et al. Concurrent Graves’ disease to hyperthyroidism. Arch intern Med 1939;
4. Oosterhuis HJ. The natural course of thyrotoxicosis and myasthenia gravis: the 64:330-335.
myasthenia gravis: a long term follow up treatment of the former may dangerously 31. McEachern D, Parnell JL. Hyperthyroidism
study. J Neurol Neurosurg Psychiatry 1989; reveal the latter. Anaesthesia 2008; 63:876-9. and Myasthenia Gravis. J Clin Endocr 1948;
52:1121–27. 18. Mappouras DG, Philippou G, Haralambous 8:842-850.
5. Grob D. Natural history of myasthenia gravis. S, et al. Antibodies to acetylcholinesterase 32. Green R. Thyrotoxicosis, Exophthalmic
In: Engel AG, ed. Myasthenia gravis and cross-reacting with hyroglobulin in Ophthalmoplegia, Myasthenia Gravis and
myasthenic disorders. Oxford: Oxford myasthenia gravis and Graves’s disease. Vertigo. Proc Roy Soc Med 1949; 42:263-
University Press. Contemporary Neurology Clinical and Experimental Immunology 267.
Series, 1999:131–45. 1995; 100:336–43. 33. Bartels EC, Kingsley JW Jr. Hyperthyroidism
6. Phillips LH 2nd, Torner JC: Epidemiologic 19. Simpson JA. Myasthenia gravis: a new associated with myasthenia gravis. Lahey
evidence for a changing natural history of hypothesis. Scott Med J 1960; 5:419-39. Clin Bull 1949; 6:101-8.
myasthenia gravis. Neurology 1996; 20. Newsom-Davis J. Autoantibody-mediated 34. Levy G, Meadows WR, Gunnar RM. The
47:1233-1238. channelopathies at the neuromuscular association of grave's disease with
7. Aragones JM, Bolibar I, Bonfill X, et al: junction. Neuroscientist 1997; 3:337-46. myasthenia gravis, with a report of five cases.
Myasthenia gravis. A higher than expected 21. Garlepp MJ, Dawkins RI, Christiansen FT. Ann Intern Med 1951; 35:134-47.
incidence in the elderly. Neurology 2003; Autoimmunity in ocular and generalized 35. Millikan CH, Haines SF. The thyroid gland in
60:1024-1026. myasthenia gravis. J Neuroimmunol 1981; relation to neuromuscular disease. AMA
8. Grob D. Course and management of 1:325-332. Arch Intern Med 1953; 92:5-39.
myasthenia gravis. JAMA 1953; 153:529- 22. Drachman DB. Myasthenia gravis and the 36. Maclean B, Wilson JA. See-saw relationship
532. thyroid gland. N Engl J Med 1962; 15:330- between hyperthyroidism and myasthenia
9. Grob D, Brunner NG, Namba T. The natural 333. gravis. Lancet 1954; 266:950-3.
course of myasthenia gravis and effects of 23. Tola MR, Caniatti LM, Casetta I, et al. 37. Silver S, Osserman KE. Hyperthyroidism and
therapeutic measures. Ann NY Acad Sci Immunogenetic heterogeneity and associated myasthenia gravis. J Mt Sinai Hosp N Y
1981; 377:652-669. autoimmune disorders in myasthenia gravis: a 1957; 24:1214-20.
10. Juel VC, Massey JM. Myasthenia Gravis. population-based survey in the province of 38. Sahay BM, Blendis LM, Greene R. Relation
Orphanet J Rare Dis 2007; 2:44. Ferrara, Northern Italy. Acta Neurol Scand between myasthenia gravis and thyroid
11. Mistry N, Wass J, Turner MR. When to 1994; 90:318-323. disease. Br Med J 1965; 1:762-5.
consider thyroid dysfunction in the neurology 24. Bello-Sani F, Anumah FE, Bakari AG. 39. Aminorroaya A, Janghorbani M, Amini M,
clinic. Pract Neurol 2009; 9:145-56. Myasthenia gravis associated with Hovsepian S, Tabatabaei A, Fallah Z. The
12. Rennie G. Exophtalmic goiter combined with autoimmune thyroid disease: a report of two prevalence of thyroid dysfunction in an
myasthenia gravis. Review of Neurology and patients. Ann Afr Med 2008; 7:88-90. iodine-sufficient area in Iran. Arch Iran Med
Psychiatry 1908; 6:229-33. 25. Kanazawa M, Shimohata T, Tanaka K, et al. 2009; 12:262-70.
13. Christensen PB, Jensen TS, Tsiropoulos I, et Clinical features of patients with myasthenia 40. Vanderpump MP, Tunbridge WM, French
al. Associated autoimmune diseases in gravis associated with autoimmune diseases. JM, et al. The incidence of thyroid disorders
myasthenia gravis. A population based study. Eur J Neurol 2007; 14:1403-4. in the community: a twenty-year follow-up of
Acta Neurologica Scandinavica 1995; 26. Thorlacius S, Aarli JA, Riise T, et al. the Whickham Survey. Clin Endocrinol 1995;
91:192-5. Associated disorders in myasthenia gravis: 43:55-68.
14. Marino M, Ricciardi R, Pinchera A, et al. autoimmune diseases and their relation to 41. Somnier F. Myasthenia gravis. Dan Med Bull
Mild clinical expression of myasthenia gravis thymectomy. Acta Neurologica Scandinavica 1996; 43: 1–10.
associated with autoimmune thyroid diseases. 1989; 80:290-95. 42. Sanders DB, Andrews PI, Howard JF,
Journal of Clinical Endocrinology and 27. Kiessling WR, Finke R, Kotulla P, Massey JM. Seronegative myasthenia gravis.
Metabolism 1997; 82:438-43. Schleusener H. Circulating TSh-binding Neurology 1997; 48 (suppl 5): S40–S45.
Hypothyroidism and myasthenia gravis 25
Ir J neurol 2011; 10(1-2)
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Myasthenic Crisis Complicated With Myxedema PositiDocument4 pagesMyasthenic Crisis Complicated With Myxedema PositiFitria ChandraNo ratings yet
- Bilateral Cavernous Sinus Involvement by Perineural Spread of Inverted PapillomaDocument3 pagesBilateral Cavernous Sinus Involvement by Perineural Spread of Inverted PapillomaFitria ChandraNo ratings yet
- Mus 26717Document8 pagesMus 26717Fitria ChandraNo ratings yet
- JCSM 13 3 479Document26 pagesJCSM 13 3 479Fitria ChandraNo ratings yet
- Pulmonary Function Tests For The Generalist: A Brief ReviewDocument9 pagesPulmonary Function Tests For The Generalist: A Brief ReviewFitria ChandraNo ratings yet
- Evidence-Based Guideline Summary: Evaluation, Diagnosis, and Management of Facioscapulohumeral Muscular DystrophyDocument10 pagesEvidence-Based Guideline Summary: Evaluation, Diagnosis, and Management of Facioscapulohumeral Muscular DystrophyFitria ChandraNo ratings yet
- Lab ReportDocument2 pagesLab Reportmohit kumarNo ratings yet
- Anatomy & Function of The SkinDocument9 pagesAnatomy & Function of The Skinعبدالعزيز احمد علي عتشNo ratings yet
- Yang Dipake 3Document6 pagesYang Dipake 3Deaz CressendoNo ratings yet
- Diabetes Mellitus in Children (Pedi Clinics of N. America Vol 52, No 6) WW PDFDocument275 pagesDiabetes Mellitus in Children (Pedi Clinics of N. America Vol 52, No 6) WW PDFEliMihaelaNo ratings yet
- 7 1 Work FileDocument2 pages7 1 Work FileNeil BernardNo ratings yet
- Station 5 Cases 4Document73 pagesStation 5 Cases 4Sagit Nauman81100% (1)
- Asynchronous Activity Sheet FormsDocument8 pagesAsynchronous Activity Sheet FormsNur SanaaniNo ratings yet
- Renal FunctionDocument4 pagesRenal FunctionCoralene Rose SilverioNo ratings yet
- HyperthyroidismDocument2 pagesHyperthyroidismZane ZyraNo ratings yet
- HypothyridismDocument18 pagesHypothyridismanuu1404No ratings yet
- Medical Diagnosis (Hyperthyroidism)Document4 pagesMedical Diagnosis (Hyperthyroidism)Kenneth Smith IINo ratings yet
- Endocrinology: SECTION A: Read Each Question Carefully and Record The Answer "TRUE" or "FALSE"Document9 pagesEndocrinology: SECTION A: Read Each Question Carefully and Record The Answer "TRUE" or "FALSE"Alice TaylorNo ratings yet
- Questions 1 Through 10 Are Based On The Following Reading PassageDocument12 pagesQuestions 1 Through 10 Are Based On The Following Reading PassageSoonie Doongie DoryNo ratings yet
- Adrenal Gland DisordersDocument7 pagesAdrenal Gland Disorderscn351073No ratings yet
- CASE REPORT - CA Tiroid Aldi - ProofreadDocument11 pagesCASE REPORT - CA Tiroid Aldi - ProofreadAldy BimaNo ratings yet
- Metabolisme Tulang: Triawanti Bagian BiokimiaDocument50 pagesMetabolisme Tulang: Triawanti Bagian BiokimiaTrii SakttiNo ratings yet
- Pathophysiology of Gestational DMDocument3 pagesPathophysiology of Gestational DMAnonymous GtR96jCNo ratings yet
- Synevo Results 3001981811Document3 pagesSynevo Results 3001981811Edward MarinescuNo ratings yet
- 09-2013 UTpt EndoDocument44 pages09-2013 UTpt Endomina0% (1)
- Hyperthyroidism (Thyrotoxicosis) : 郑州大学第一附院内分泌科 王守俊 Wang shou junDocument133 pagesHyperthyroidism (Thyrotoxicosis) : 郑州大学第一附院内分泌科 王守俊 Wang shou junapi-19916399No ratings yet
- Metformin Use in Women With Polycystic Ovary Syndrome: Neil P. JohnsonDocument6 pagesMetformin Use in Women With Polycystic Ovary Syndrome: Neil P. JohnsonanyNo ratings yet
- Hormone Replacement Therapy (HRT)Document15 pagesHormone Replacement Therapy (HRT)LanaNo ratings yet
- An Introduction To EndocrinologyDocument47 pagesAn Introduction To EndocrinologyAmeng GosimNo ratings yet
- Terminologia LatinaDocument7 pagesTerminologia LatinaКонстантин ЗахарияNo ratings yet
- 592008000011: 59000720 03-Aug-20 08:49 AM: Mrs. Veena K Arora: 03-Aug-2020 08:49 AM: Dr. Self: 03-Aug-2020 12:47PM: 48 Y 06 M 12 D / F: 03-Aug-2020 01:12PMDocument2 pages592008000011: 59000720 03-Aug-20 08:49 AM: Mrs. Veena K Arora: 03-Aug-2020 08:49 AM: Dr. Self: 03-Aug-2020 12:47PM: 48 Y 06 M 12 D / F: 03-Aug-2020 01:12PMrajanarora72No ratings yet
- A Case Report On Hyponatremia Leading Sign of Hypopituitarism (Secondary To Adrenal Insufficiency)Document4 pagesA Case Report On Hyponatremia Leading Sign of Hypopituitarism (Secondary To Adrenal Insufficiency)International Journal of Innovative Science and Research TechnologyNo ratings yet
- مذكرة فارماكولوجي روعةDocument56 pagesمذكرة فارماكولوجي روعةKomang Gede Suwija Negara100% (1)
- Tubular Reabsorption and SecretionDocument29 pagesTubular Reabsorption and SecretionenriNo ratings yet
- Laboratory Tests of Renal FunctionDocument5 pagesLaboratory Tests of Renal Functiongiselle155204No ratings yet
- Cushing's SyndromeDocument24 pagesCushing's SyndromeUdtjeVanDerJeyk100% (1)