Professional Documents
Culture Documents
OPTH 129552 Vernal Keratoconjunctivitis 011018
OPTH 129552 Vernal Keratoconjunctivitis 011018
Uploaded by
Sugumar YathavanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
OPTH 129552 Vernal Keratoconjunctivitis 011018
OPTH 129552 Vernal Keratoconjunctivitis 011018
Uploaded by
Sugumar YathavanCopyright:
Available Formats
Clinical Ophthalmology Dovepress
open access to scientific and medical research
Open Access Full Text Article Review
Vernal keratoconjunctivitis
This article was published in the following Dove Press journal:
Clinical Ophthalmology
Clinical Ophthalmology downloaded from https://www.dovepress.com/ by 43.252.233.243 on 27-Aug-2021
Hampton Addis Abstract: Vernal keratoconjunctivitis (VKC) is a chronic allergic conjunctivitis that is most
Bennie H Jeng often seen in young, males. Although most types of allergic conjunctivitis do not affect vision,
Department of Ophthalmology
VKC is unusual in that damage to the cornea from the condition can result in vision loss.
and Visual Sciences, University Although it is typically seasonal, year-round symptoms can be seen, which can lead to uncertain
of Maryland School of Medicine, diagnoses being made. Although the pathophysiology of VKC is better understood in recent
Baltimore, MD, USA
years, allowing more targeted therapies, management of these patients can still be very chal-
lenging, and complications can occur. As such, aggressive management of VKC is necessary,
especially since vision loss in the amblyogenic age range can be permanent.
Keywords: vernal keratoconjunctivitis, allergic conjunctivitis, inflammation
For personal use only.
Introduction
Vernal keratoconjunctivitis (VKC) is a unique disorder among a spectrum of allergic
eye diseases. It is a chronic, bilateral, inflammatory condition most commonly involving
the upper tarsal conjunctiva. It more commonly affects young, male patients, but it is
frequently observed in tropical regions where it may affect both sexes equally.1 VKC
has also often been associated with higher socioeconomic status. The incidence, as
well as the type, of VKC varies depending on geographic region: limbal VKC is the
predominate form in central and southern African countries,2 while the palpebral form
is most frequent in Europe and the Americas.3 Seasonal exacerbations may occur
based on the time of year, most often in Europe and Asia, but a significant number of
patients may develop chronic perennial disease.4 Although the disease is most often
self-limiting, and will often resolve after puberty, some patients can develop sight-
threatening complications. Immunosuppressive therapy is the mainstay of treatment, but
surgical intervention may be required to manage the disease and its complications.
Pathophysiology
VKC is characterized by infiltration of the conjunctiva by a variety of inflammatory
cell types, especially eosinophils. Although VKC has previously been thought of as an
IgE-mediated disease,5 several other immunologic pathways have also been implicated.
Patients with VKC have been shown to have an increased number of activated CD4+
T-lymphocytes, predominantly Th2, indicating that there is a hypersensitivity reac-
tion to an unknown pathogen.6 Increased levels of inflammatory cytokines IL-3, IL-4,
Correspondence: Bennie H Jeng and IL-5 have also been demonstrated.7 Conjunctival papillae formation is related to
Department of Ophthalmology and Visual fibroblast activation and production, whereas limbal conjunctival nodules are related
Sciences, University of Maryland School
of Medicine, 419 W. Redwood Street,
to infiltration of inflammatory cells.6
Suite 470, Baltimore, MD 21201, USA Studies using in vivo confocal microscopy have shown cellular irregularities in
Tel +1 667 214 1232
Fax +1 410 328 1178
patients with VKC. Patients have been shown to have not only injury to the superficial
Email bjeng@som.umaryland.edu corneal epithelial layer but also involvement of the basal epithelium and anterior stroma.
submit your manuscript | www.dovepress.com Clinical Ophthalmology 2018:12 119–123 119
Dovepress © 2018 Addis and Jeng. This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php
http://dx.doi.org/10.2147/OPTH.S129552
and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). By accessing the work you
hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission
for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms (https://www.dovepress.com/terms.php).
Powered by TCPDF (www.tcpdf.org)
Addis and Jeng Dovepress
Corneal nerves may be affected in VKC, and they have occasional allergic eye drop use; grade 2 being the presence
been shown to have decreased density as well as increased of symptoms including photophobia; grade 3 representing
concentration of adjacent inflammatory cells.8 daily anti-allergic treatment and occasional topical steroid
It is also thought that aberrations in the normal ocular use; and grade 4 being diffuse punctate keratitis or corneal
surface microbiome may play a role in VKC. In a recent ulcer, and use of pulsed high-dose topical steroid. This
study, Staphylococcus aureus was more frequently iso- grading system identifies those patients with more severe
lated from the conjunctival specimens from patients with disease and at higher risk of recurrence and complications
VKC, and may be a significant cause of exacerbations, associated with VKC, leading to worse visual outcomes.10
Clinical Ophthalmology downloaded from https://www.dovepress.com/ by 43.252.233.243 on 27-Aug-2021
while S. epidermidis was more frequently found in normal
control patients.9 Differential diagnoses
Differential diagnosis of VKC includes any of the chronic
Clinical findings allergic conjunctivitis’s including seasonal allergic conjuncti-
Patients with VKC often present with symptoms of intense vitis, perennial allergic conjunctivitis, atopic keratoconjunc-
itching, redness, and watering eyes.4 They also may com- tivitis, or giant papillary conjunctivitis, as well as chlamydial
plain of photophobia and foreign body sensation. Clinical infection, especially in the early stages on the disease.11 VKC
signs of VKC include a papillary reaction of the upper tarsal may be differentiated from the above disorders by hypertro-
conjunctiva, and throughout the limbus. VKC is classified phic papillae in the tarsal form of VKC or Horner Trantas
as tarsal, limbal, or mixed3 based on the location, and the dots in the limbal form, or a combination of the two, along
For personal use only.
papillae may range in size from 1 mm to giant cobblestone with no involvement of the eyelids.12
papillae. The eyelid margins are not involved, in contrast Currently there is limited utility in testing for the diag-
to other types of allergic keratoconjunctivitis. Other typical nosis of VKC. Skin tests and IgE levels are rarely useful
signs of VKC include bulbar conjunctival hyperemia, a thick and may be negative in 50% of patients with VKC. In cases
mucus discharge, and corneal involvement, including super- where the diagnosis is unclear, conjunctival scrapings show-
ficial punctate keratitis, epithelial erosions, shield ulcers, ing eosinophilic infiltration may be beneficial in aiding
or plaques (Figure 1). A classic sign of VKC is Tranta’s the diagnosis.5
dots which represent lymphocytic infiltration of the limbal
conjunctiva. Treatment
A clinical grading system based on clinical symptoms and There is currently no defined gold-standard treatment algo-
signs has been proposed to help guide treatment and identify rithm for VKC, but there are many options available, and
patients at high risk for recurrences, corneal complications, treatment should be tailored to the individual.
and vision loss. In a recent study, patients were stratified Whatever treatment regimen is prescribed, it should
by symptoms: grade 0 being no symptoms and no therapy; be initiated promptly and the patient should be monitored
grade 1 being presence of symptoms without photophobia and closely for the development of any corneal complications.
A Cochrane review by Mantelli et al included 27 ran-
domized controlled trials encompassing 2,184 eyes in an
effort to evaluate topical therapies for the treatment of
VKC. They found that all common antiallergic eye drops
are effective in reducing signs and symptoms of disease,
and that some patients even respond to placebo.13 A critical
initial component of all allergic disease involves avoidance
of inciting factors. Patients should be encouraged to wash
hands frequently and avoid touching or rubbing their eyes.
Cold compresses and artificial tears may help to alleviate
symptoms in mild cases or as adjunctive therapy to pharma-
cologic treatment. First-line pharmacologic therapy for VKC
is topical treatment, and there is considerable therapeutic
Figure 1 Ten-year-old boy with vernal keratoconjunctivitis demonstrating superior overlap with other forms of allergic conjunctivitis. Mast cell
palpebral conjunctiva with giant papillae within an intensely inflamed conjunctiva and
shield ulcer in the cornea with fluorescein staining. (Courtesy of Todd P. Margolis,
stabilizers are a mainstay for prophylaxis. In milder cases,
MD, PhD). antihistamines may be of benefit, but more severe cases may
120 submit your manuscript | www.dovepress.com Clinical Ophthalmology 2018:12
Dovepress
Powered by TCPDF (www.tcpdf.org)
Dovepress Vernal keratoconjunctivitis
require corticosteroid treatment. Long-term steroid use is be treated with more potent steroids such as prednisolone
associated with many complications, so other immunomodu- acetate or dexamethasone.20
latory treatments have been studied extensively.
Cyclosporine
Mast cell stabilizers Cyclosporine is a calcineurin inhibitor that acts by inhib-
Mast cell stabilizers are thought to prevent mast cell degran iting cytokine production by T-lymphocytes. It also has
ulation via inhibition of calcium channels, but their mecha- inhibitory effects on eosinophil and mast cell activation.21
nism is not completely understood. There is increasing Low-dose cyclosporine has emerged as an alternative to
Clinical Ophthalmology downloaded from https://www.dovepress.com/ by 43.252.233.243 on 27-Aug-2021
evidence that mast cell stabilizers act more broadly on corticosteroids in some cases of VKC. It has an excellent
inflammatory cell chemotaxis.14 Commonly used mast cell side effect profile, limited to only a burning sensation and
stabilizers include cromolyn sodium and lodoxamide, which few systemic effects at the doses being used.22 Commercially
are frequently used as first-line therapy. Lodoxamide has available topical 0.05% cyclosporine A has been shown to
been shown to be superior to cromolyn sodium in relieving improve clinical signs and symptoms of VKC, as well as
symptoms and clinical signs of VKC.15 The medications decreasing tear cytokine concentration when used 4–6 times
should be used 4–6 times daily and may take up to 2 weeks per day.23 Higher concentrations of 1%–2% have been studied
to show response in mild cases of VKC. and shown to be safe and effective for even severe VKC,
but the disadvantage is that they need to be extemporane-
Antihistamines
ously compounded.24,25 More recent studies have shown
Antihistamines are sometimes used in the treatment of VKC:
For personal use only.
even a dose of cyclosporine 0.05% 4 times per day may be
they are most often used in alleviating the symptoms of mild
effective in drug-resistant VKC in conjunction with topical
disease, but they have limited utility in severe cases.
corticosteroids.26
More recent medications that combine antihistamine
properties with mast cell stabilization include ketotifen and
olopatadine. Both have been shown to improve the signs and
Tacrolimus
Tacrolimus is another calcineurin inhibitor that acts to inhibit
symptoms of VKC, and there is evidence that ketotifen may
T-lymphocyte activation and it causes the release of inflam-
be more effective.16 Some antihistamines may have a drying
matory cytokines.27 In recent studies tacrolimus has proven
effect, which could exacerbate symptoms.
to be very effective in the treatment of VKC at various
Nonsteroidal anti-inflammatory drugs concentrations. Chatterjee et al studied response to 0.03%
(NSAIDs) tacrolimus ointment in steroid-refractory patients with VKC.
NSAIDs may also be a useful therapeutic option in VKC. Out of 23 patients, only 4 required additional corticosteroid
Topical diclofenac or ketorolac have been shown to be therapy after 4 weeks of tacrolimus treatment.28
effective in treating symptoms.17,18 NSAIDs may be used in Tacrolimus may also be effective in patients with
conjunction with other topical anti-inflammatory medications corneal involvement. Miyazaki et al treated patients with
to provide rapid relief of symptoms; however, they have epitheliopathy, shield ulcers, or corneal plaques with 0.1%
limited utility in those patients with corneal involvement.19 topical tacrolimus, and showed similar improvement in epi-
While NSAIDs are a frequently prescribed ocular medi- theliopathy scores when compared to those using adjuvant
cation, there have been reports of severe corneal toxicity, topical corticosteroids.29
with even ulceration and corneal perforation in otherwise A recent randomized control trial compared treatment of
healthy eyes. As such, their use should be limited to short- VKC with 0.005% tacrolimus eye drops versus IFN alpha-2b
term treatment.12 who had failed topical antihistamines and corticosteroids.
The main outcome measure was improvement of subjective
Topical corticosteroids symptoms, but objective improvement of exam findings was
Topical corticosteroids are a critical component of VKC also measured. All of the patients with tacrolimus showed
management, particularly in VKC exacerbations, but they improvement of subjective symptoms while one patient
have extensive side effect profiles including cataract develop- treated with interferon had persistent symptoms.30
ment and glaucoma. Initial treatment in an acute exacerbation
should begin with steroids with low intraocular penetration Other therapies
such as loteprednol or fluorometholone to avoid complica- The most resistant cases of VKC may require treatment with
tions associated with steroid use. More resistant cases should systemic medications, including oral corticosteroids or other
Clinical Ophthalmology 2018:12 submit your manuscript | www.dovepress.com
121
Dovepress
Powered by TCPDF (www.tcpdf.org)
Addis and Jeng Dovepress
immunomodulatory agents. Recent case reports have shown particularly resistant to topical therapy and may require
treatment of VKC with omalizumab: 4 patients who had failed surgical intervention.
topical therapy of both cyclosporine and tacrolimus showed Patients with long-standing vernal keratoconjunctivitis
improvement of ocular symptoms of itching and tearing, as may also develop limbal stem cell deficiency due to long-
well as ocular signs of hyperemia, and papillae.31 There may standing inflammation. The prevalence of limbal stem cell
also be a role for allergen-specific immunotherapy which deficiency in patients with VKC may be as high as 1.2% and
avoids the side effects often seen with topical therapies. occurs in older patients with VKC. Treatment may include
Patients with VKC often have hypersensitivity to pollens amniotic membrane transplantation or allo-limbal stem cell
Clinical Ophthalmology downloaded from https://www.dovepress.com/ by 43.252.233.243 on 27-Aug-2021
and house dust and have been shown to have improvement transplantation.37 Other commonly associated complications
in signs and symptoms with subcutaneous allergen-specific from vernal keratoconjunctivitis include keratoconus and
immunotherapy (SCIT).32 In this study, treatment by SCIT irregular astigmatism due to frequent eye rubbing in the
was more effective in improving the clinical symptoms atopic pediatric population38 and steroid-induced glaucoma
and reducing the serum IgE than topical treatment because from frequent use of topical corticosteroids.3,38
there was a greater reduction in symptoms in group 1 of
immunotherapy (72%) than in group 2 of medical treatment Prognosis
(59%) (P,0.05). Also, there was a significant reduction in The prognosis for VKC patients is generally good and the
total serum IgE (P,0.05) in group 1 (62%) compared to disease is generally self-limiting with appropriate treatment.
group 2 (42%).32 Despite an overall good prognosis, up to 6% of patients will
For personal use only.
develop vision loss due to complications associated with
Surgical intervention VKC. In patients studied, over half will continue to have
Persistent corneal complications such as non-healing shield symptoms after 5 years and the presence of giant papilla may
ulcers or corneal plaques may require surgical treatment. indicate a worse prognosis.3
These interventions may range from scraping to superficial
keratectomy. In rare cases of refractory giant papillae that Future research
do not respond to medical treatment, surgical interventions The incidence of allergic disease is continuing to climb39
such as cryoablation may be employed. Therapies in con- and personalized therapeutic approaches are currently being
junction with surgical excision to prevent recurrence include studied. Further developments in allergic sensitization may
mitomycin-C application, autologous conjunctival graft, or prove to be the next innovation of VKC treatment.
mucous membrane transplantation. Amniotic membrane
transplantation in cases of refractory giant papillae has been Conclusion
shown to aid healing of corneal complications associated with VKC is a bilateral inflammatory disease that can cause visual
giant papillae such as epitheliopathy and ulcers.33 loss. Although little has changed in the diagnosis of VKC,
which continues to be largely clinical, based on symptoms
Complications and clinical signs, newer therapies have been developed.
Severe vernal keratoconjunctivitis is most frequently a self- This armamentarium of therapies continues to expand
limiting disease; however, in some cases sight-threatening with increasing use of immunomodulators. Unfortunately,
complications may develop. The corneal epithelium acts as a severe, protracted cases of VKC remain a challenge to treat.
barrier to circulating pathogens, but may become damaged in As such, continued research is necessary to better understand
severe disease both due to trauma from upper tarsal papillae the complex nature of VKC and to develop more effec-
and a complex array of inflammatory molecules.34 This tive therapies.
combination of repeated trauma and inflammatory milieu
may then lead to shield ulcers and plaques. Shield ulcers Disclosure
usually form on the upper third of the cornea and can lead The authors report no conflicts of interest in this work.
to sight-threatening complications in up to 6% of patients.35
They begin as punctate epithelial erosions which coalesce
References
to form macroerosions which then develop into shield ulcers 1. Chenge B, Makumyamviri AM, Kaimbo WA, Kaimbo D. La limbo-
which can be self-limiting or develop further consequences conjunctivite endemique des tropiques a Lubumbashi, Republique
Democratique du Congo. [Tropical endemic limbo-conjunctivitis in
such as bacterial keratitis.36 Plaques form when inflammatory Lúbumbashi, Democratic Republic of the Congo]. Bull Soc Belge Oph-
debris accumulates at the base of a shield ulcer. They are talmol. 2003;(290) 9–16. French.
122 submit your manuscript | www.dovepress.com Clinical Ophthalmology 2018:12
Dovepress
Powered by TCPDF (www.tcpdf.org)
Dovepress Vernal keratoconjunctivitis
2. Dahan E, Appel R. Vernal keratoconjunctivitis in the black child and 20. Leonardi A. Management of vernal keratoconjunctivitis. Ophthalmol
its response to therapy. Br J Ophthalmol. 1983;67(10):688–692. Ther. 2013;2(2):73–88.
3. Bonini S, Bonini S, Lambiase A, et al. Vernal keratoconjunctivitis 21. Donnenfeld E, Pflugfelder SC. Topical ophthalmic cyclosporine: phar-
revisited: a case series of 195 patients with long-term followup. macology and clinical uses. Surv Ophthalmol. 2009;54(3):321–338.
Ophthalmology. 2000;107(6):1157–1163. 22. Pucci N, Caputo R, Mori F, et al. Long-term safety and efficacy of
4. Saboo US, Jain M, Reddy JC, Sangwan VS. Demographic and clinical topical cyclosporine in 156 children with vernal keratoconjunctivitis.
profile of vernal keratoconjunctivitis at a tertiary eye care center in Int J Immunopathol Pharmacol. 2010;23(3):865–871.
India. Indian J Ophthalmol. 2013;61(9):486–489. 23. Oray M, Toker E. Tear cytokine levels in vernal keratoconjunctivitis:
5. Bonini S, Coassin M, Aronni S, Lambiase A. Vernal keratoconjuncti- the effect of topical 0.05% cyclosporine a therapy. Cornea. 2013;
vitis. Eye. 2004;18(4):345–351. 32(8):1149–1154.
6. Leonardi A. Vernal keratoconjunctivitis: pathogenesis and treatment. 24. Tesse R, Spadavecchia L, Fanelli P, et al. Treatment of severe ver-
Clinical Ophthalmology downloaded from https://www.dovepress.com/ by 43.252.233.243 on 27-Aug-2021
Prog Retin Eye Res. 2002;21(3):319–339. nal keratoconjunctivitis with 1% topical cyclosporine in an Italian
7. Metz DP, Hingorani M, Calder VL, Buckley RJ, Lightman SL. T-cell cohort of 197 children. Pediatr Allergy Immunol. 2010;21(2 pt 1):
cytokines in chronic allergic eye disease. J Allergy Clin Immunol. 1997; 330–335.
100(6 Pt 1):817–824. 25. Kiliç A, Gürler B. Topical 2% cyclosporine A in preservative-free
8. Leonardi A, Lazzarini D, Bortolotti M, Piliego F, Midena E, Fregona I. artificial tears for the treatment of vernal keratoconjunctivitis. Can
Corneal confocal microscopy in patients with vernal keratoconjuncti- J Ophthalmol. 2006;41(6):693–698.
vitis. Ophthalmology. 2012;119(3):509–515. 26. Yücel OE, Ulus ND. Efficacy and safety of topical cyclosporine A 0.05%
9. Al-Hakami AM, Al-Amri A, Abdulrahim I, Hamid ME. Is there is in vernal keratoconjunctivitis. Singapore Med J. 2016;57(9):507–510.
an association between the presence of Staphylococcus species and 27. Zhai J, Gu J, Yuan J, Chen J. Tacrolimus in the treatment of ocular
occurrence of vernal keratoconjunctivitis? Saudi J Ophthalmol. 2015; diseases. BioDrugs. 2011;25:89–103.
29(4):255–258. 28. Chatterjee S, Agrawal D. Tacrolimus in corticosteroid-refractory vernal
10. Sacchetti M, Lambiase A, Mantelli F, Deligianni V, Leonardi A, Bonini S. keratoconjunctivitis. Cornea. 2016;35(1):1444–1448.
Tailored approach to the treatment of vernal keratoconjunctivitis. 29. Miyazaki D, Fukushima A, Ohashi Y, et al. Steroid-sparing effect of
Ophthalmology. 2010;117(7):1294–1299. 0.1% Tacrolimus eye drop for treatment of shield ulcer and corneal
For personal use only.
11. Mannis MJ, Holland EJ. Cornea. 2nd ed. Vol. 1. Edinburgh: Elsevier; epitheliopathy in refractory allergic ocular diseases. Ophthalmology.
2017. 2017;124(3):287–294.
12. Leonardi A, Bogacka E, Fauquert JL, et al. Ocular allergy: recognizing 30. Zanjani H, Aminifard MN, Ghafourian A, et al. Comparative evalua-
and diagnosing hypersensitivity disorders of the ocular surface. Allergy. tion of tacrolimus versus interferon alpha-2b eye drops in the treatment
2012;67(11):1327–1337. of vernal keratoconjunctivitis: a randomized, double-masked study.
13. Mantelli F, Santos MS, Petitti T, et al. Systematic review and meta- Cornea. 2017;36(6):675–678.
analysis of randomised clinical trials on topical treatments for vernal 31. Occasi F, Duse M, Nebbioso M, et al. Vernal keratoconjunctivitis
keratoconjunctivitis. Br J Ophthalmol. 2007;91(12):1656–1661. treated with omalizumab: a case series. Pediatr Allergy Immunol. 2017;
14. Bruijnzeel PL, Warringa RA, Kok PT, Kreukniet J. Inhibition of neu- 28(5):503–505.
trophil and eosinophil induced chemotaxis by nedocromil sodium and 32. Mahdy RAR, Nada WM, Marei AA. Subcutaneous allergen-specific
sodium cromoglycate. Br J Pharmacol. 1990;99(4):798–802. immunotherapy versus topical treatment in vernal keratoconjunctivitis.
15. Caldwell DR, Verin P, Hartwich-Young R, Meyer SM, Drake MM. Cornea. 2012;31(5):525–528.
Efficacy and safety of lodoxamide 0.1% vs cromolyn sodium 4% in 33. Guo P, Kheirkhah A, Zhou W-W, Qin L, Shen X-L. Surgical resection
patients with vernal keratoconjunctivitis. Am J Ophthalmol. 1992; and amniotic membrane transplantation for treatment of refractory
113(6):632–637. giant papillae in vernal keratoconjunctivitis. Cornea. 2013;32(6):
16. Hida WT, Nogueira DC, Schaefer A, Dantas PEC, Dantas MCN. 816–820.
Comparação entre o uso tópico do fumarato de cetotifeno 0,025% e 34. Fukuda K, Nishida T. Ocular allergic inflammation: interaction between
do cloridrato de olopatadina 0,1% no tratamento da ceratoconjuntivite the cornea and conjunctiva. Cornea. 2010;29:S62–S67.
primaveril. [Comparative study between 0.025% ketotifen fumarate 35. Neumann E, Gutmann MJ, Blumenkrantz N, Michaelson IC. A review
and 0.1% olopatadine hydrochloride in the treatment of vernal kerato- of four hundred cases of vernal conjunctivitis. Am J Ophthalmol. 1959;
conjunctivitis]. Arq Bras Oftalmol. 2006;69(6):851–856. Portuguese. 47(2):166–172.
17. D’Angelo G, Lambiase A, Cortes M, et al. Preservative-free diclofenac 36. Cameron JA. Shield ulcers and plaques of the cornea in vernal kerato-
sodium 0.1% for vernal keratoconjunctivitis. Graefes Arch Clin Exp conjunctivitis. Ophthalmology. 1995;102(6):985–993.
Ophthalmol. 2003;241:192–195. 37. Sangwan VS, Jain V, Vemuganti GK, Murthy SI. Vernal keratoconjunc-
18. Sharma A, Gupta R, Ram J, Gupta A. Topical ketorolac 0.5% solution tivitis with limbal stem cell deficiency. Cornea. 2011;30(5):491–496.
for the treatment of vernal keratoconjunctivitis. Indian J Ophthalmol. 38. Tabbara KF. Ocular complications of vernal keratoconjunctivitis.
1997;45(3):177–180. Can J Ophthalmol. 1999;34(2):88–92.
19. Kosrirukvongs P, Luengchaichawange C. Topical cyclosporine 0.5 per 39. Backman H, Räisänen P, Hedman L, et al. Increased prevalence of
cent and preservative-free ketorolac tromethamine 0.5 per cent in vernal allergic asthma from 1996 to 2006 and further to 2016 – results from
keratoconjunctivitis. J Med Assoc Thai. 2004;87(2):190–197. three population surveys. Clin Exp Allergy. 2017;47(11):1426–1435.
Clinical Ophthalmology Dovepress
Publish your work in this journal
Clinical Ophthalmology is an international, peer-reviewed journal PubMed Central and CAS, and is the official journal of The Society of
covering all subspecialties within ophthalmology. Key topics include: Clinical Ophthalmology (SCO). The manuscript management system
Optometry; Visual science; Pharmacology and drug therapy in eye is completely online and includes a very quick and fair peer-review
diseases; Basic Sciences; Primary and Secondary eye care; Patient system, which is all easy to use. Visit http://www.dovepress.com/
Safety and Quality of Care Improvements. This journal is indexed on testimonials.php to read real quotes from published authors.
Submit your manuscript here: http://www.dovepress.com/clinical-ophthalmology-journal
Clinical Ophthalmology 2018:12 submit your manuscript | www.dovepress.com
123
Dovepress
Powered by TCPDF (www.tcpdf.org)
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- NG163Document24 pagesNG163Tim BrownNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- New England Journal of Medicine Volume 383 Issue 19 2020 (Doi 10.1056 - NEJMra1915327) Ropper, Allan H. Ashina, Messoud - MigraineDocument11 pagesNew England Journal of Medicine Volume 383 Issue 19 2020 (Doi 10.1056 - NEJMra1915327) Ropper, Allan H. Ashina, Messoud - MigraineMarija Sekretarjova100% (1)
- Case Study: A Patient With Type 2 Diabetes Working With An Advanced Practice Pharmacist To Address Interacting ComorbiditiesDocument8 pagesCase Study: A Patient With Type 2 Diabetes Working With An Advanced Practice Pharmacist To Address Interacting ComorbiditiessamanNo ratings yet
- Serrapeptase - The Miracle Enzyme Which Can Save Your LifeDocument53 pagesSerrapeptase - The Miracle Enzyme Which Can Save Your LifeRoger-Peter Weizenegger100% (7)
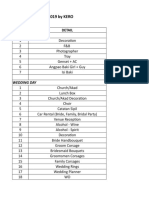
- Wedding Budget 2019 by Kero: NO DetailDocument9 pagesWedding Budget 2019 by Kero: NO DetailJaneLorensNo ratings yet
- Cardiovascular System Block BookDocument38 pagesCardiovascular System Block BookJaneLorensNo ratings yet
- Mechanical Bowel Obstruction and Related Risk Factors On Morbidity and MortalityDocument7 pagesMechanical Bowel Obstruction and Related Risk Factors On Morbidity and MortalityJaneLorensNo ratings yet
- Try Out MSK Senin, 8 September 2014Document3 pagesTry Out MSK Senin, 8 September 2014JaneLorensNo ratings yet
- Manual of Anatomy Lab MSK 300713Document4 pagesManual of Anatomy Lab MSK 300713JaneLorensNo ratings yet
- Health Promotion (Eng)Document25 pagesHealth Promotion (Eng)JaneLorens100% (1)
- Anti-Inflammatory Activity of Indonesian Nutmeg Seeds (Myristica Fragrans Houtt) : A Topical Gel FormulationDocument8 pagesAnti-Inflammatory Activity of Indonesian Nutmeg Seeds (Myristica Fragrans Houtt) : A Topical Gel FormulationIJPHSNo ratings yet
- Migraine Diagnosis and TreatmentDocument19 pagesMigraine Diagnosis and TreatmentMagdalila Pua RosalesNo ratings yet
- Drug StudyDocument8 pagesDrug StudyDhanNo ratings yet
- CNS DrugsDocument15 pagesCNS Drugsrechelle mae legaspi100% (1)
- AAOS Clinical Practice Guideline Summary .10Document9 pagesAAOS Clinical Practice Guideline Summary .10mukhlis akmalNo ratings yet
- Course: B.Pharm Class: 3 Year Subject: Medicinal Chemistry-I Chapter-1: Basic Principles of Medicinal ChemistryDocument9 pagesCourse: B.Pharm Class: 3 Year Subject: Medicinal Chemistry-I Chapter-1: Basic Principles of Medicinal ChemistryAnanda VijayasarathyNo ratings yet
- Comparison of A Preservative Free Nonsteroidal.Document7 pagesComparison of A Preservative Free Nonsteroidal.Danty IndriastutyNo ratings yet
- Blood Pressure - Blood Pressure SolutionDocument100 pagesBlood Pressure - Blood Pressure Solutionfarkad rawi100% (3)
- Drug Name Mechanism of Action Indication/ Contraindication Adverse Effect Nursing ResponsibilitiesDocument1 pageDrug Name Mechanism of Action Indication/ Contraindication Adverse Effect Nursing ResponsibilitiesJohnrick VenturaNo ratings yet
- Management of Mixed PainDocument19 pagesManagement of Mixed PainGita FitrianiNo ratings yet
- Pharmaceutical and Personal Care Products in DomesDocument10 pagesPharmaceutical and Personal Care Products in DomesSaraNo ratings yet
- 21 - Comparative Efficacy and Safety of Rimegepant Ubrogepane and Lasmiditan For Acute Treatment of Migraine A Network Meta-AnalysisDocument13 pages21 - Comparative Efficacy and Safety of Rimegepant Ubrogepane and Lasmiditan For Acute Treatment of Migraine A Network Meta-Analysiscuma cobaNo ratings yet
- Adverse Drug Reactions and InteractionsDocument6 pagesAdverse Drug Reactions and InteractionsAlvina HafidiatiNo ratings yet
- TercicaDocument1 pageTercicarehankhankhanNo ratings yet
- Summary of Product Characteristics: Apsifen-F Ibuprofen 600 MG Film-Coated TabletsDocument12 pagesSummary of Product Characteristics: Apsifen-F Ibuprofen 600 MG Film-Coated TabletsMeriam Gita Maulia SuhaidiNo ratings yet
- Master Drug ListDocument55 pagesMaster Drug Listnotgonnatell99No ratings yet
- Drug Study Drug Classification Mechanism of Action Adverse Effect/ Side Effects Nursing ResponsibilitiesDocument3 pagesDrug Study Drug Classification Mechanism of Action Adverse Effect/ Side Effects Nursing ResponsibilitiesMary Rose Bell AriasNo ratings yet
- All Mechanism of Action and Classification DrugsDocument28 pagesAll Mechanism of Action and Classification Drugselanthamizhmaran78% (9)
- Pharmacology & Therapeutics - Topical Past Papers-1Document42 pagesPharmacology & Therapeutics - Topical Past Papers-1Muhammad Mohsin MalikNo ratings yet
- Essential Drugs 2013Document378 pagesEssential Drugs 2013Chedeng KumaNo ratings yet
- Medicinal Plants in The Treatment of Arthritis: A. Subramoniam, V. Madhavachandran and A. GangaprasadDocument35 pagesMedicinal Plants in The Treatment of Arthritis: A. Subramoniam, V. Madhavachandran and A. GangaprasadVedhanayagiNo ratings yet
- Dental RoshetttaDocument29 pagesDental RoshetttaKORMAX LEAGUENo ratings yet
- MISOPROST Is Abortifacient Drug in Egypt-EnDocument2 pagesMISOPROST Is Abortifacient Drug in Egypt-Enpharmacia1.comNo ratings yet
- How Medicines Are Born The Imperfect Science of Drugs PDFDocument181 pagesHow Medicines Are Born The Imperfect Science of Drugs PDFAlinaNo ratings yet
- Pentasa Tablets and Sachets PIDocument14 pagesPentasa Tablets and Sachets PIGeo GeoNo ratings yet
- Top 100 Drugs - RxTechExamDocument6 pagesTop 100 Drugs - RxTechExamshaukijameelNo ratings yet