Professional Documents
Culture Documents
2017 CBCT
Uploaded by
Syifa IKOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2017 CBCT
Uploaded by
Syifa IKCopyright:
Available Formats
[Downloaded free from http://www.amsjournal.com on Thursday, December 21, 2017, IP: 190.194.178.
64]
Case Report
Ameloblastic Fibro‑odontoma with a Predominant Radiopaque
Component
Saurabh Gajanan Kale, Akshay Shetty, Jintu Balakrishnan1, Praveen Purvey
Departments of Oral and Maxillofacial Surgery, and 1Oral and Maxillofacial Pathology, Sri Rajiv Gandhi College of Dental Sciences and Hospital, Bengaluru,
Karnataka, India
Abstract
Ameloblastic fibro‑odontoma (AFO) is a rare odontogenic tumor. Initially believed to be a lesion similar to ameloblastic fibroma (AF), it is now
considered as a separate entity in the WHO odontogenic tumor classification. Commonly associated with a painless swelling and an associated
absence of eruption of a tooth, AFO presents as a mixed radiopaque and radiolucent lesion in the younger population with a predilection for the
posterior region. Histologically, it shows the characteristics of an immature complex odontoma with irregularly arranged enamel, dentinoid,
cementoid‑like structures, and ectomesenchymal tissue. The following case report describes a case of AFO with a predominantly radiopaque
component and briefly discusses the available literature pertaining to this rare entity.
Keywords: Ameloblastic fibro‑odontoma, ameloblastic fibroma, radiopaque
Introduction Case Report
Odontogenic tumors are a pathology occasionally encountered A 19‑year‑old male patient presented to us with a chief
by the practicing clinician. Studies from North America seem complaint of a painless swelling in the lower right side of
to indicate that odontogenic tumors represent approximately the mouth since 6 months. Examination revealed a small
1% of all accessions in oral pathology laboratories.[1] While hard swelling in the right mandibular buccal and lingual
ameloblastomas and odontomas are encountered more sulcus and absence of the tooth 47. History revealed that
frequently, ameloblastic fibro‑odontoma (AFO) is rare, the patient had not undergone any extraction for the tooth
accounting for 1%–3% of all the odontogenic tumors.[2] AFO in the past and that the tooth had not erupted in the mouth.
was defined as a lesion similar to ameloblastic fibroma (AF), Opposite arch 37 was erupted and the 38 was found to be
but also showing inductive changes that lead to the formation impacted clinically. The overlying mucosa was normal, the
of both dentine and enamel.[3] However, AFO is presently nerve function was well preserved, and the tooth 46, adjacent
defined by the World Health Organization as a neoplasm to the swelling exhibited no pathologic mobility or pockets.
consisting of odontogenic ectomesenchyme resembling the There was no draining sinus or fistula formation. Aspiration
dental papilla, epithelial strands, and nest resembling dental was performed to rule out any vascular malformation
lamina and enamel organ in conjunction with the presence of and on aspirate being negative; an incisional biopsy was
dentine and enamel.[4] performed. An incisional biopsy report of odontomes was
received, and a cone‑beam computed tomography (CBCT)
The pathogenesis of AFO appears to be from an abnormal
proliferation of odontogenic epithelium from a permanent tooth
germ, which exerts an organizing effect on the mesodermal Address for correspondence: Dr. Saurabh Gajanan Kale,
element with the formation of calcified dental tissues.[5] Department of Oral and Maxillofacial Surgery, Sri Rajiv Gandhi
College of Dental Sciences and Hospital, Cholanagar, R T Nagar Post,
The following is a case report of a male patient with a large Bengaluru ‑ 560 032, Karnataka, India.
AFO lesion in the posterior mandible with a predominant E‑mail: saurabh.dent@gmail.com
radiopaque component.
This is an open access article distributed under the terms of the Creative Commons
Access this article online Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak,
Quick Response Code: and build upon the work non-commercially, as long as the author is credited and the new
Website: creations are licensed under the identical terms.
www.amsjournal.com
For reprints contact: reprints@medknow.com
DOI: How to cite this article: Kale SG, Shetty A, Balakrishnan J, Purvey P.
10.4103/ams.ams_84_17 Ameloblastic fibro-odontoma with a predominant radiopaque component.
Ann Maxillofac Surg 2017;7:304-7.
304 © 2017 Annals of Maxillofacial Surgery | Published by Wolters Kluwer - Medknow
[Downloaded free from http://www.amsjournal.com on Thursday, December 21, 2017, IP: 190.194.178.64]
Kale, et al.: AFO with a predominant radiopaque component
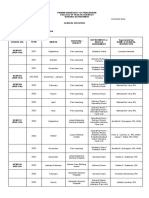
was advised. CBCT revealed the presence of a large hypothesized that AF, ameloblastic fibrodentinoma (AFD),
well‑defined radiolucency extending from the mesial root and AFO could represent a single entity in different stages of
of 46 to the inferior aspect of the ascending border of the development: AF or AFD would evolve to AFO as they mature
ramus. Measuring approximately 6 cm × 3 cm in the greatest and the latter could differentiate into odontoma. However,
dimension anteroposteriorly and superoinferiorly, it could be when clinical characteristics of these lesions are analyzed,
seen extending till the inferior border of the mandible. Teeth AFO is more frequent in a younger age group with a mean age
47 and 48 were involved within the radiolucency, and the of 9.6 years, than AF, which affects individuals with a mean
inferior alveolar canal was deflected inferiorly. Correlating age of 14.8 years, thereby in disagreement to the continuous
clinically, a mild buccolingual cortical expansion could be differentiation hypothesis.[2] Philipsen et al. suggested the
appreciated. The patient gave no neurological disturbances hypothesis of two lines of development for AF, AFD, and AFO.
secondary to inferior alveolar nerve compression. The bulk A hamartomatous line was represented by AFO as a primary
of the radiolucency was interspersed with well‑defined areas stage of odontoma whereas a neoplastic line comprised AF
of radiopacity [Figure 1a and b]. and AFD.[5]
A surgical excision of the lesion was planned owing to the The diagnostic difficulties for AFO can be due to its
well‑defined nature of the radiolucency and an incisional resemblance to calcifying epithelial odontogenic tumor,
biopsy report of an odontome. Informed consent was obtained adenomatoid odontogenic tumor, AFD, and AF. The
from the patient, and the surgical procedure was performed differential diagnosis between AFO and AF is made based
under general anesthesia with oral intubation. Due to the on the presence or absence of elements indicative of tooth
proximity of the lesion to the inferior border of the mandible germ differentiation (enamel or dentin). While AFO exhibits
and an associated risk of mandibular fracture, an extraoral evidence of tooth germ differentiation, AF does not. [6]
submandibular incision was given. Surgical exposure of the However, differentiating AFO from AFD can be difficult as
lesion revealed an expanded buccal cortex which was not both present as well‑circumscribed, expansile radiolucencies
breached [Figure 2a]. A bony window was created in the buccal on radiographs that generally contain a few solitary or multiple
cortex, and the lesion was excised in a piecemeal fashion small radiopaque foci with irregular sizes that form a calcified
owing to the large dimensions of the lesion [Figure 2b]. 46 product in the lesion and are often associated with impacted
was extracted intraoperatively based on the severe bone loss tooth/teeth. Consequently, a histopathological diagnosis is
in relation to its distal aspect. The resulting surgical defect typically required to distinguish AFD from AFO.[7]
was evaluated [Figure 2c]. Owing to the thin margin of the
inferior border of the mandible which was left behind, a risk These tumors are commonly seen in the younger population
for pathologic fracture was suspected. A 2.5 mm titanium with 98.8% cases occurring before the age of 20 years.
reconstruction plate was hence placed along the body and While certain authors claim no gender preference,[6] a recent
the ramus of the mandible to support it [Figure 2d]. The systematic review by Chrcanovic and Gomez[8] found that AFO
closure was done in layers, and the specimen was sent for was more prevalent in men than women (1.4:1). The lack of any
histopathologic examination. The postoperative recovery of clinical complaints such as pain, pus discharge, or significant
the patient was uneventful [Figure 3a‑c]. swelling could be a possible reason for their delay in diagnosis
or an incidental diagnosis during a routine dental check‑up.
Histologic examination
Radiographic appearance of AFO may be in the form of a
The specimen consisted of multiple hard tissue bits, the largest
well‑defined radiolucent area containing variable amounts
hard tissue bit measuring around 10 mm × 5 mm × 3 mm
of radiopaque materials of irregular size and form. About
and 8 mm × 5 mm × 3 mm. The H and E stained soft tissue
86% lesions are found to be associated with impacted teeth.
sections exhibited connective tissue consisting of round to
Root resorption of the adjacent teeth may also occur, the
ovoid‑shaped odontogenic islands which were peripherally
majority of the teeth being deciduous teeth.[8] The presence
lined by tall columnar cells arranged in a palisading pattern
of a predominant radiopacity within the radiolucency was
with reversal of polarity and subnuclear vacuolization. The
consistent with our case.
center of the odontogenic islands showed the presence of
stellate reticulum like cells. The islands were surrounded by Despite the considerable size the lesions of AFO may attain,
a clear zone which was previously occupied by the enamel pain and/or paresthesia are unusual symptoms, although tooth
matrix. Areas of hyalinization resembling dysplastic dentin displacement may occasionally occur.[2] Our patient presented
could also be seen [Figure 3d and e]. with no complaints of pain or parsesthesia despite evidence
of downward displacement of the inferior alveolar canal due
Discussion to the lesion. In addition, our patient also did not exhibit any
tooth displacement in relation to 46.
First described by Hooker in 1967,[5] AFO has since been
extensively studied in literature. However, due to its rare Araki et al.[9] studied the diverse calcification patterns seen
occurrence, the available literature has remained restricted in radiographs of patients with AFO. He categorized the
to mainly single case reports. Some investigators have calcification patterns based on their appearance and their
Annals of Maxillofacial Surgery ¦ Volume 7 ¦ Issue 2 ¦ July-December 2017 305
[Downloaded free from http://www.amsjournal.com on Thursday, December 21, 2017, IP: 190.194.178.64]
Kale, et al.: AFO with a predominant radiopaque component
a b
a b
Figure 1: (a) Three‑dimensional reconstruction showing the extent of the
tumor. (b) Sagittal computed tomography section exhibiting impacted 47,
48 within the mixed lesion
c d
Figure 2: (a) Surgical exposure of the lesion. (b) Tumor excision.
(c) Defect post excision. (d) Reconstruction plate fixation
been attributed to the inadequate surgical removal at the time of
initial treatment. The use of carnoy’s solution and cryosurgery
has also been reported to reduce the chances for recurrence.[2]
a b Large lesions pose a risk for pathologic fracture during surgical
removal because of thinning of the bone. The lesion should
hence be removed in small pieces by sectioning the mineralized
tissue to preserve the bone and minimize the amount of bone
lost. Due to the large size of the lesion in this case, a large
surgical defect was produced with a resultant increased risk
of pathologic fracture. To support the mandibular bone in this
region, a 2.5 mm reconstruction plate was adapted and plated
c along the mandible extending from the ramus to the body.
Another clinical decision pertaining to enucleation of AFO
lies in the fate of the teeth around the lesion. Zouhary et al.[10]
advocated that if the teeth do not interfere with the enucleation
of the tumor, there is no reason to remove them, with the
possibility of a spontaneous eruption occurring later. In case of
our patient, the impacted 47 and 48 were completely embedded
within the lesion and were hence removed along with the tumor.
d e A recent systematic review by Chrcanovic and Gomez revealed
Figure 3: (a and b) 6 month postoperative frontal and profile
th that unilocular lesions appeared to recur more frequently
photographs. (c) 2nd month post‑operative orthopantomogram with the compared to multilocular varieties of AFO. Furthermore,
residual defect and the reconstruction plate in place. (d and e) Histological multilocular lesions were found to be a more common feature
features at ×10 and ×40 magnification of AFD compared to AFO.[8]
AFO is a rare group of odontogenic tumors with a good
location within the radiolucency. While the appearances were
prognosis. The involved teeth can be left behind to allow
categorized into lucent, sand, cluster, blended and tooth‑like,
spontaneous eruption into the oral cavity as long as it does
the location was categorized as peripheral, central, or full. The not interfere or compromise with the complete excision of the
radiographic features of our patient could be hence categorized lesion. The well‑defined nature of this lesion and meticulous
as cluster appearance located centrally within the lesion. surgery makes excision easy and minimizes chances for
However, the fill of the lesion was found to be extensive with recurrences further.
a minimal radiolucent rim.
Declaration of patient consent
A conservative surgical approach in the form of excision The authors certify that they have obtained all appropriate
or enucleation has been found to be satisfactory for these patient consent forms. In the form the patient(s) has/have
well‑encapsulated lesions. Sporadic recurrences of AFO have given his/her/their consent for his/her/their images and other
306 Annals of Maxillofacial Surgery ¦ Volume 7 ¦ Issue 2 ¦ July-December 2017
[Downloaded free from http://www.amsjournal.com on Thursday, December 21, 2017, IP: 190.194.178.64]
Kale, et al.: AFO with a predominant radiopaque component
clinical information to be reported in the journal. The patients 4. Barnes L, Eveson JW, Reichart P, Sidransky D. World Health
understand that their names and initials will not be published Organization Classification of Tumours. Pathology and Genetics. Head
and Neck Tumors. Lyon: IARC Press; 2005.
and due efforts will be made to conceal their identity, but 5. Philipsen HP, Reichart PA, Praetorius F. Mixed odontogenic tumours
anonymity cannot be guaranteed. and odontomas. Considerations on interrelationship. Review of the
literature and presentation of 134 new cases of odontomas. Oral Oncol
Financial support and sponsorship 1997;33:86‑99.
Nil. 6. Soares RC, Godoy GP, Neto JC, Souza LB, Pinto LP. Ameloblastic
fibro‑odontoma: Report of a case presenting an unusual clinical course.
Conflicts of interest Int J Pediatr Otorhinolaryngol Extra 2006;1:200‑3.
There are no conflicts of interest. 7. Tsuji K, Yoshida H, Watanabe S, Yamamoto E, Yamada K, Tominaga K,
et al. A case of ameloblastic fibro‑odontoma accompanied with a number
of impacted teeth. J Oral Maxillofac Surg Med Pathol 2015;27:366‑8.
References 8. Chrcanovic BR, Gomez RS. Ameloblastic fibrodentinoma and
1. Carlson ER. Odontogenic cysts and tumors. In: Miloro M, Ghali GE, ameloblastic fibro‑odontoma: An updated systematic review of
Larsen PE, Waite PD, editors. Petersons Principles of Maxillofacial cases reported in the literature. J Oral Maxillofac Surg 2017.
Surgery. 2nd ed. London: BC Decker Inc.; 2004. p. 583. pii: S0278‑239131326‑X.
2. Lopes ML, Severo ML, Medeiros MR, Clemente TE, Neto AC, Silveira EJ. 9. Araki M, Namaki S, Amemiya T, Matsumoto K, Honda K, Yonehara Y,
Ameloblastic fibro‑odontoma: Case report and immunohistochemical et al. Diverse calcification patterns of ameloblastic fibro‑odontoma on
profile. J Oral Maxillofac Surg Med Pathol 2017;29:77‑82. radiographic examination. J Oral Sci 2016;58:533‑7.
3. Kramer IR, Pindborg JJ, Shear M. Histological typing of odontogenic 10. Zouhary KJ, Said‑Al‑Naief N, Waite PD. Ameloblastic fibro‑odontoma:
tumours. In: World Health Organisation, editor. International Histologic Expansile mixed radiolucent lesion in the posterior maxilla: A case report.
Classification of Tumours. 2nd ed. Berlin: Springer; 1992. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106:e15‑21.
Annals of Maxillofacial Surgery ¦ Volume 7 ¦ Issue 2 ¦ July-December 2017 307
You might also like
- An Unusual Case of 177 Pieces of Mandibular Compound Odontoma: 10-Year Follow-UpDocument4 pagesAn Unusual Case of 177 Pieces of Mandibular Compound Odontoma: 10-Year Follow-UpTrianita DivaNo ratings yet
- 2 51 1647598330 5ijmpsjun202205Document10 pages2 51 1647598330 5ijmpsjun202205TJPRC PublicationsNo ratings yet
- Cemento-Osseous Dysplasia Masquerading as CystDocument5 pagesCemento-Osseous Dysplasia Masquerading as CystQintari FauziaNo ratings yet
- Case Report: Peripheral Cemento-Ossifying Fibroma: Case Series Literature ReviewDocument6 pagesCase Report: Peripheral Cemento-Ossifying Fibroma: Case Series Literature ReviewMariela Judith UCNo ratings yet
- Cabt 12 I 3 P 330Document4 pagesCabt 12 I 3 P 330abeer alrofaeyNo ratings yet
- 2017 - Ameloblastic Fibroodontoma Uncommon Case Presentation in A 6 Year Old ChildDocument4 pages2017 - Ameloblastic Fibroodontoma Uncommon Case Presentation in A 6 Year Old ChildSyifa IKNo ratings yet
- Article-PDF-Vajendra Joshi Kalwa Pavan Kumar Shalini Joshi Sujatha Gopal-177Document3 pagesArticle-PDF-Vajendra Joshi Kalwa Pavan Kumar Shalini Joshi Sujatha Gopal-177sagarjangam123No ratings yet
- Case ReportDocument4 pagesCase ReportAjeng Narita CaustinaNo ratings yet
- Lapsus Journal OriginalDocument5 pagesLapsus Journal Originalrozi piresNo ratings yet
- Odontogenic Keratocyst - A Deceptive EntityDocument4 pagesOdontogenic Keratocyst - A Deceptive EntityIJAR JOURNALNo ratings yet
- Adenomatoid Odontogenic Tumor, An Uncommon TumorDocument3 pagesAdenomatoid Odontogenic Tumor, An Uncommon TumorHarshavardhan ReddyNo ratings yet
- AF Tumor PDFDocument2 pagesAF Tumor PDFRaden Bryan S.RNo ratings yet
- Pulpitis JurnalDocument2 pagesPulpitis JurnalIsmail YusufNo ratings yet
- 826-Abstract, Key Words, Introduction and Article Text and References-6236-1!10!20230324Document4 pages826-Abstract, Key Words, Introduction and Article Text and References-6236-1!10!20230324Ketut SariasihNo ratings yet
- Adenomatoid Odontogenic Tumour of Maxilla A Case ReportDocument6 pagesAdenomatoid Odontogenic Tumour of Maxilla A Case ReportAthenaeum Scientific PublishersNo ratings yet
- Rare Mandibular Tumor CaseDocument3 pagesRare Mandibular Tumor CaseBrutusRexNo ratings yet
- Article-Ossifying Fibroma in The Maxilla and MandibleDocument12 pagesArticle-Ossifying Fibroma in The Maxilla and MandibleMaged NabilNo ratings yet
- Jurnal Gilut 3Document3 pagesJurnal Gilut 3adintaNo ratings yet
- Otorhinolaryngology: Ameloblastic Fibrodentinosarcoma: A Rare Malignant Odontogenic TumorDocument4 pagesOtorhinolaryngology: Ameloblastic Fibrodentinosarcoma: A Rare Malignant Odontogenic TumorTERCERO 2019No ratings yet
- JIndianSocPeriodontol18185-5364653 145406Document3 pagesJIndianSocPeriodontol18185-5364653 145406marethadwiNo ratings yet
- Peripheral Ameloblastoma With Neoplastic Osseous Invasion Versus Peripheral Intraosseous AmeloblastomaDocument5 pagesPeripheral Ameloblastoma With Neoplastic Osseous Invasion Versus Peripheral Intraosseous AmeloblastomaDeb SNo ratings yet
- Peripheral Ameloblastoma of The GingivaDocument5 pagesPeripheral Ameloblastoma of The GingivaLourena MarinhoNo ratings yet
- JDS 17 370Document15 pagesJDS 17 370Ferry HendrawanNo ratings yet
- A Parulis-Like Soft Tissue Tumor in Relation With A Dental Implant: Case ReportDocument3 pagesA Parulis-Like Soft Tissue Tumor in Relation With A Dental Implant: Case ReportDr. AtheerNo ratings yet
- Cementoblastoma Jinak Sebuah Laporan Kasus Yang Jarang Terjadi Dengan Kajian LiteraturDocument4 pagesCementoblastoma Jinak Sebuah Laporan Kasus Yang Jarang Terjadi Dengan Kajian LiteraturRayAdityaParipurnaNo ratings yet
- Peripheral Ossifying Fibroma: A Case ReportDocument3 pagesPeripheral Ossifying Fibroma: A Case ReportIJAR JOURNALNo ratings yet
- Amhsr 3 285Document3 pagesAmhsr 3 285Dwi Dayanti AgustinaNo ratings yet
- Case MTDocument4 pagesCase MTĐạt Bùi TấnNo ratings yet
- 7 OsteosarcomaDocument4 pages7 OsteosarcomaDodNo ratings yet
- Compound Odontome A Case ReportDocument4 pagesCompound Odontome A Case ReportMariane SantosNo ratings yet
- Solitary central osteoma of mandible in a geriatric patientDocument4 pagesSolitary central osteoma of mandible in a geriatric patientNurul SalsabilaNo ratings yet
- Follicular and Plexiform Ameloblastoma Case ReportDocument6 pagesFollicular and Plexiform Ameloblastoma Case Reportluckytung07No ratings yet
- Treatment Evaluation of Odontogenic Keratocyst by Using CBCTDocument6 pagesTreatment Evaluation of Odontogenic Keratocyst by Using CBCTShinta PurnamasariNo ratings yet
- 2017 OmrDocument4 pages2017 Omrcalmua1234No ratings yet
- Rare Mandibular AOT CaseDocument3 pagesRare Mandibular AOT CaseSuman ChaturvediNo ratings yet
- Min 2018Document7 pagesMin 2018CindyNo ratings yet
- Compound Odontoma Associated With Impacted Maxillary Anterior Teeth A Case ReportDocument4 pagesCompound Odontoma Associated With Impacted Maxillary Anterior Teeth A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Dafpus 1Document8 pagesDafpus 1Winda WidhyastutiNo ratings yet
- Odontogenic FibromaDocument5 pagesOdontogenic FibromaGowthamChandraSrungavarapuNo ratings yet
- Peripheral Ameloblastic FibromaDocument3 pagesPeripheral Ameloblastic FibromadoktergigikoeNo ratings yet
- tmpB15C TMPDocument5 pagestmpB15C TMPFrontiersNo ratings yet
- Cancellous Osteoma of Maxilla A Rare Case ReportDocument4 pagesCancellous Osteoma of Maxilla A Rare Case Reportanindya permatasyafiraNo ratings yet
- BCR 2013 200316Document4 pagesBCR 2013 200316ay lmaoNo ratings yet
- Content ServerDocument4 pagesContent ServerAndrea Carolina Rojas MendezNo ratings yet
- Peripheral Ossifying Fi Broma: ASE EportDocument4 pagesPeripheral Ossifying Fi Broma: ASE Eporterr3sNo ratings yet
- Ejd - Ejd 261 16Document5 pagesEjd - Ejd 261 16Neggy YudibrataNo ratings yet
- Calcifying Odontogenic Cyst With Atypical FeaturesDocument5 pagesCalcifying Odontogenic Cyst With Atypical FeaturesHerminaElenaNo ratings yet
- Partial Odontectomy 2007Document7 pagesPartial Odontectomy 2007Yoga ChrisnugrohoNo ratings yet
- 30121-Article Text-56500-1-10-20200810Document7 pages30121-Article Text-56500-1-10-20200810IfadahNo ratings yet
- Ameloblastic Fibroma: Report of A Case: Su-Gwan Kim, DDS, PHD, and Hyun-Seon Jang, DDS, PHDDocument3 pagesAmeloblastic Fibroma: Report of A Case: Su-Gwan Kim, DDS, PHD, and Hyun-Seon Jang, DDS, PHDdoktergigikoeNo ratings yet
- Histopathological Insight of An Adenomatoid Odontogenic Lesion - A Cyst, Tumor or Hamartoma?Document6 pagesHistopathological Insight of An Adenomatoid Odontogenic Lesion - A Cyst, Tumor or Hamartoma?gunawan121982No ratings yet
- Juvenile Ossifying Fibroma: ASE EportDocument3 pagesJuvenile Ossifying Fibroma: ASE Eportsagarjangam123No ratings yet
- 1 s2.0 S2210261223007496 MainDocument6 pages1 s2.0 S2210261223007496 MainReyes Ivan García CuevasNo ratings yet
- Compoun MolarDocument4 pagesCompoun MolarGhea AlmadeaNo ratings yet
- Pof CR1Document4 pagesPof CR1Swab IndonesiaNo ratings yet
- 13 - 2018 - Ooc - JOralMaxillofacPathol22420-3155112 - 084551Document4 pages13 - 2018 - Ooc - JOralMaxillofacPathol22420-3155112 - 084551Uma DatarNo ratings yet
- Peripheral Cemento-Ossifying Fibroma - A Case Report With A Glimpse On The Differential DiagnosisDocument5 pagesPeripheral Cemento-Ossifying Fibroma - A Case Report With A Glimpse On The Differential DiagnosisnjmdrNo ratings yet
- MainDocument7 pagesMainPaula Francisca Moraga HidalgoNo ratings yet
- Ameloblastic Fibroma or Fibrosarcoma: A Dilemma of Oral SurgeonDocument3 pagesAmeloblastic Fibroma or Fibrosarcoma: A Dilemma of Oral SurgeonJeyachandran MariappanNo ratings yet
- 2016 - A Case of Periimplantitis and OsteoradionecrosisDocument5 pages2016 - A Case of Periimplantitis and OsteoradionecrosisSyifa IKNo ratings yet
- 2016 - Diagnostic Features and Management Strategy of A Refractory Case of Radionecrosis of The MandibleDocument12 pages2016 - Diagnostic Features and Management Strategy of A Refractory Case of Radionecrosis of The MandibleSyifa IKNo ratings yet
- Case Report: 3D Reconstruction and Prediction of Sialolith SurgeryDocument5 pagesCase Report: 3D Reconstruction and Prediction of Sialolith SurgerySyifa IKNo ratings yet
- 2016 - Fibular Flap For Mandible Reconstruction in Osteoradionecrosis of The JawDocument7 pages2016 - Fibular Flap For Mandible Reconstruction in Osteoradionecrosis of The JawSyifa IKNo ratings yet
- 2018 - Banyak Foto - Osteoradionecrosis of Jaw An Institutional ExperienceDocument8 pages2018 - Banyak Foto - Osteoradionecrosis of Jaw An Institutional ExperienceSyifa IKNo ratings yet
- 2019 - Banyak Foto - Osteoradionecrosis of The Jaws Triggered by Dental Implants PlacementDocument6 pages2019 - Banyak Foto - Osteoradionecrosis of The Jaws Triggered by Dental Implants PlacementSyifa IKNo ratings yet
- 2018 - Banyak Foto - Oral Rehabilitation of The Cancer PatientDocument18 pages2018 - Banyak Foto - Oral Rehabilitation of The Cancer PatientSyifa IKNo ratings yet
- 2018 - Banyak Foto - Oral Rehabilitation of The Cancer PatientDocument18 pages2018 - Banyak Foto - Oral Rehabilitation of The Cancer PatientSyifa IKNo ratings yet
- 2019 - Use of Platelet Rich Fibrin and Surgical Approach For Combined Treatment of RadionecrosisDocument6 pages2019 - Use of Platelet Rich Fibrin and Surgical Approach For Combined Treatment of RadionecrosisSyifa IKNo ratings yet
- 2018 - Fofo Gjls - Potential Role of Post Treatment Follow Up FDG PET CTDocument7 pages2018 - Fofo Gjls - Potential Role of Post Treatment Follow Up FDG PET CTSyifa IKNo ratings yet
- 2018 - Fofo Gjls - Potential Role of Post Treatment Follow Up FDG PET CTDocument7 pages2018 - Fofo Gjls - Potential Role of Post Treatment Follow Up FDG PET CTSyifa IKNo ratings yet
- 2019 - Use of Platelet Rich Fibrin and Surgical Approach For Combined Treatment of RadionecrosisDocument6 pages2019 - Use of Platelet Rich Fibrin and Surgical Approach For Combined Treatment of RadionecrosisSyifa IKNo ratings yet
- 2016 - A Case of Periimplantitis and OsteoradionecrosisDocument5 pages2016 - A Case of Periimplantitis and OsteoradionecrosisSyifa IKNo ratings yet
- PDFDocument6 pagesPDFFed Espiritu Santo GNo ratings yet
- Ameloblastic Fibro-Odontoma Associated With Paresthesia of The Chin and Lower Lip in A 12-Year-Old GirlDocument4 pagesAmeloblastic Fibro-Odontoma Associated With Paresthesia of The Chin and Lower Lip in A 12-Year-Old GirlIrinaNo ratings yet
- Ameloblastic Fibro-Odontoma Associated With Paresthesia of The Chin and Lower Lip in A 12-Year-Old GirlDocument4 pagesAmeloblastic Fibro-Odontoma Associated With Paresthesia of The Chin and Lower Lip in A 12-Year-Old GirlIrinaNo ratings yet
- 2016 - Byk FotoDocument7 pages2016 - Byk FotoSyifa IKNo ratings yet
- Case ReportDocument4 pagesCase ReportAjeng Narita CaustinaNo ratings yet
- 2017 - Ameloblastic Fibroodontoma Uncommon Case Presentation in A 6 Year Old ChildDocument4 pages2017 - Ameloblastic Fibroodontoma Uncommon Case Presentation in A 6 Year Old ChildSyifa IKNo ratings yet
- 2016 - Large Ameloblastic Fibro Odontoma in A 7 Year Old GirlDocument8 pages2016 - Large Ameloblastic Fibro Odontoma in A 7 Year Old GirlSyifa IKNo ratings yet
- Donning and Removing Sterile Gloves (Open Method) Preparation RationaleDocument2 pagesDonning and Removing Sterile Gloves (Open Method) Preparation RationalecharmainchavezNo ratings yet
- Bilirubin Metabolism: Hd. - Msc. (Biochemistry)Document18 pagesBilirubin Metabolism: Hd. - Msc. (Biochemistry)MuhamadMarufNo ratings yet
- Blood ReportDocument2 pagesBlood ReportDeepak VasudevNo ratings yet
- Nursing Care Plan PPROM 1Document1 pageNursing Care Plan PPROM 1Nickaela Calalang100% (1)
- D20rha25 2013-1Document2 pagesD20rha25 2013-1Icmi KadarsihNo ratings yet
- Final Presentation Journal OtitisDocument34 pagesFinal Presentation Journal OtitisKevin HartonoNo ratings yet
- Lecture 2 - Urine ExaminationDocument62 pagesLecture 2 - Urine ExaminationmihalachemirelaNo ratings yet
- Anemia of Diminished ErythropoiesisDocument43 pagesAnemia of Diminished ErythropoiesisJared Khoo Er HauNo ratings yet
- UntitledDocument10 pagesUntitledGuia Charish SalvadorNo ratings yet
- Teenage Pregnancy Brief DiscussionDocument3 pagesTeenage Pregnancy Brief DiscussionJoanna Peroz100% (1)
- Assessing Community Health ProblemsDocument5 pagesAssessing Community Health ProblemsMARC JOSHUA SARANILLONo ratings yet
- Kimia Farma Per 30 September ZRMM076Document271 pagesKimia Farma Per 30 September ZRMM076SriyatiNo ratings yet
- Merge-Davao (Multi - Educational Review Group Experts) : Physiological IntegrityDocument12 pagesMerge-Davao (Multi - Educational Review Group Experts) : Physiological IntegrityNom NomNo ratings yet
- Clinical RotationDocument2 pagesClinical RotationDarwin QuirimitNo ratings yet
- TM's Pathology Q BankDocument22 pagesTM's Pathology Q BankChanukya GvNo ratings yet
- CA 2 - CHN Review 50 Items PretestDocument10 pagesCA 2 - CHN Review 50 Items PretestAlibasher Macalnas100% (1)
- Krok 1 Stomatology 2015Document20 pagesKrok 1 Stomatology 2015MarinaNo ratings yet
- Development of the Gastrointestinal SystemDocument109 pagesDevelopment of the Gastrointestinal SystemRaju Mehta100% (1)
- Detecting Hemoperitoneum: Limitations of Repeat FAST ExamsDocument123 pagesDetecting Hemoperitoneum: Limitations of Repeat FAST ExamsSinisa Ristic50% (2)
- Macrocytic anemia causes and treatmentDocument2 pagesMacrocytic anemia causes and treatmentLefteris ChatzidoukasNo ratings yet
- Domestic Accident: Group 7 Muhammad Afil Rooban Sumitha SanchiaDocument22 pagesDomestic Accident: Group 7 Muhammad Afil Rooban Sumitha SanchiaMuhmd shiyas.HNo ratings yet
- Aubf MergeDocument164 pagesAubf MergeVia Gail CanlasNo ratings yet
- Drug Abuse Essay - AlcoholismDocument5 pagesDrug Abuse Essay - Alcoholismapi-509288017No ratings yet
- Guidelines For Deploying Student NursesDocument2 pagesGuidelines For Deploying Student NursesDivya ToppoNo ratings yet
- What Effects Do Smoking and DrinkingDocument8 pagesWhat Effects Do Smoking and DrinkingDulce M. LupaseNo ratings yet
- Ethical Issues in Mandatory Smallpox VaccinationDocument2 pagesEthical Issues in Mandatory Smallpox VaccinationFaizaNadeemNo ratings yet
- Pharmaceutical MicrobiologyDocument8 pagesPharmaceutical MicrobiologyDipali KatareNo ratings yet
- Post Stroke WritingDocument9 pagesPost Stroke WritingAdi ParamarthaNo ratings yet
- Clinical Case NobelReplace Conical Connection Alessandro PozziDocument8 pagesClinical Case NobelReplace Conical Connection Alessandro PozziShyam BhatNo ratings yet
- PG List 2016 17Document4 pagesPG List 2016 17Sundeep ArcheliesNo ratings yet