Professional Documents
Culture Documents
NigerPostgradMedJ28122-5530363 152143
Uploaded by
YUSUF MUSAOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NigerPostgradMedJ28122-5530363 152143
Uploaded by
YUSUF MUSACopyright:
Available Formats
[Downloaded free from http://www.npmj.org on Thursday, February 25, 2021, IP: 105.112.74.
61]
Original Article
Clinical, Endoscopic and Histological Profile of Colorectal
Cancers Seen on Colonoscopy in Kano, North‑Western Nigeria
Yusuf Musa, Mansur Femi Mohammed1, Nurudeen Olalekan Muhammad2, Ibrahim Yusuf3, Abdulrashid Onimisi Abdulrahim4, Adamu Alhaji Samaila2,
Musa Muhammad Borodo2
Department of Internal Medicine, Federal Medical Centre, Katsina, Katsina State, 1Department of Internal Medicine, Ahmadu Bello University Teaching Hospital, Zaria,
Kaduna State, 2Department of Internal Medicine, Aminu Kano Teaching Hospital and Bayero University Kano, Kano State, 3Department of Histopathology Aminu Kano
Teaching Hospital and Bayero University, Kano, 4Department of Internal Medicine, Federal Medical Centre, Azare, Bauchi State, Nigeria
Abstract
Background: Colorectal cancer (CRC) is the most prevalent gastrointestinal (GI) cancer. With 5% risk of developing CRC in life, it became
the third leading cause of cancer death in developed nations. In Nigeria, it is the most common GI cancer. However, there are limited data on
CRC in the study area (North‑Western part of Nigeria). The aim of this study was to identify the clinical, endoscopic and histological profile of
CRC seen on colonoscopy. Methodology: This was a retrospective descriptive study where colonoscopic and histological records of suspected
CRC in the study centre between January 2008 to December 2017 were evaluated. Results: Records of 135 patients were reviewed, and males
constituted 63.7%. The mean age was 46.61 ± 16.80 years, with 30–39 years as a modal group. Common presentations were diarrhoea (86.7%)
and bleeding per rectum (68.9%). Areas affected were rectosigmoid colon (63%), ascending colon (14.1%), descending colon (8.9%),
transverse colon (7.4%) and anal canal (6.7%). Histologically, adenocarcinoma was reported in 57.8%, mucinous adenocarcinoma in 8.1%
and signet ring cell adenocarcinoma in 3.7%. Tubular and villous adenomas were 3% each. Others were carcinoid tumours (1.5%), metastatic
adenocarcinoma, squamous cell carcinoma, basal cell carcinoma, GI stromal tumour, inflammatory myofibroblastic tumour, angiosarcoma and
adenoid cyst carcinoma reported in 0.7% each. Conclusion: Majority of the patients with CRC were in their young age. The most common
presentations were diarrhoea, weight loss and anaemia. The most common site of affectation was in the left colon, while the most common
histological finding was adenocarcinoma.
Keywords: Adenocarcinoma, anal canal, ascending colon, colonoscopy, colorectal cancer, descending colon, mucinous adenocarcinoma,
rectosigmoid colon, signet ring adenocarcinoma, transverse colon, tubular adenoma, villous adenoma
Introduction CRC is the fourth most common malignancy amongst men
and women in Nigeria.[10] The actual Nigerian incidence
Colonic and rectal malignancies are very common cancers
and prevalence of CRC are lacking. However, the estimated
globally.[1] Colorectal cancer (CRC) is the third most common
prevalence is about 3.4 cases per 100,000 population,[11] while
cancer in both sexes and the second most common cause of
the incidence is 6.4–8.7 and ≤6.3 per 100,000 in males and
cancer‑related deaths.[2‑5] Incidence and prevalence are on
females, respectively.[2,3] Similarly, the combined incidence for
the rise globally, but early detection and modern treatment
both sexes was 5.5–6.5/100,000.[5] CRC is recently found to be
facilities in industrialised nations have made its morbidity and
the most common gastrointestinal (GI) tumour in Nigeria.[7,12‑15]
mortality to be more glaring in unindustrialised nations.[5‑8] This
in part is related to the establishment of screening programmes, Cancer of the colon was found to have an incidence of 3.3 and
with early cancer detection in such nations, unlike what is 3.0 for males and females in West Africa in 2018, while rectal
obtainable in developing countries like Nigeria.[9,10]
Address for correspondence: Dr. Yusuf Musa,
Department of Internal Medicine, Federal Medical Centre, Katsina, Nigeria.
E‑mail: yusuf.musa@npmcn.edu.ng
Received: 02‑09‑2020 Revised: 01-10-2020
Accepted: 28-11-2020 Published: 25‑02‑2021
This is an open access journal, and articles are distributed under the terms of the Creative
Commons Attribution‑NonCommercial‑ShareAlike 4.0 License, which allows others to remix,
Access this article online
tweak, and build upon the work non‑commercially, as long as appropriate credit is given and
Quick Response Code: the new creations are licensed under the identical terms.
Website:
www.npmj.org For reprints contact: reprints@medknow.com
How to cite this article: Musa Y, Mohammed MF, Muhammad NO, Yusuf I,
DOI: Abdulrahim AO, Samaila AA, et al. Clinical, endoscopic and histological
10.4103/npmj.npmj_288_20 profile of colorectal cancers seen on colonoscopy in Kano, North-Western
Nigeria. Niger Postgrad Med J 2021;28:22-6.
22 © 2021 Nigerian Postgraduate Medical Journal | Published by Wolters Kluwer - Medknow
[Downloaded free from http://www.npmj.org on Thursday, February 25, 2021, IP: 105.112.74.61]
Musa, et al.: Colorectal cancers seen on colonoscopy in Kano, Nigeria
cancer had 2.7 and 2.1 for the two sexes.[2,3] CRC has a global Aminu Kano Teaching Hospital is an institution in Kano city,
incidence of 19.7 for both sexes with 23.6 and 16.3 for males North‑Western Nigeria. It is equipped with an endoscopy
and females, respectively.[2,3,5] suite since 1992 and manned by gastroenterologists from the
Department of Internal Medicine. The unit receives requests
CRC, though previously reported mainly amongst the middle
from Jigawa, Katsina, Bauchi, Yobe, Borno and Zamfara states.
aged and elderly worldwide,[1,6,7,9,11,13,16‑21] is now increasingly
The unit has also a colonoscopy suite which is equipped with an
reported amongst younger individuals even before the age of
Olympus adjustable procedure couch, Pentax EPK‑1000 video
20.[22‑25] Similarly, CRC has been postulated to be seen one or
colonoscope, Olympus Optera CV‑170 video system with
two decades earlier in Africans compared to Caucasians.[26]
ADVAN AMM215WTD Monitor, TE‑NE Compact Trolley
CRC has a variety of modifiable and non‑modifiable risk factors. assembly and CF‑H170 colonoscope. The common agents used
The non‑modifiable factors are ethnicity, hereditary cancer for bowel preparation are oral and rectal Bisacodyl (Dulcolax)
syndromes, family history of CRC, male gender, advancing as well as castor oil and 20% diluted oral mannitol. Boston
age, long stature, history of adenomatous polyps, history of Bowel Preparation Score is the most common guide used for
inflammatory bowel disease, type 2 diabetes mellitus, previous assessing the adequacy of bowel preparation.
CRC, cystic fibrosis, abdominal radiation during childhood
The endoscopy register was reviewed, and all the patients
and cholecystectomy amongst others.[5,6,11,12,16,17,21,22,27] On the
with suspected CRC between January 2008 and December
other hand, modifiable risk factors include obesity, physical
2017 were isolated and their relevant data such as sex, age
inactivity, consumption of excessive red meat, fat and
and symptomatology or indication for the procedure as well
processed food, excessive calcium intake excessive alcohol
as endoscopic findings were noted accordingly. The biopsies
intake, low fibre intake, low Vitamin D, reduced fruits and
taken were followed up at the Histopathology Department of
vegetable intake, cigarette smoking, low socio‑economic
the same institution where previous histology registers were
status and some gut microbiota. However, high fibre diet,
checked for confirmation of histological diagnosis.
fruits, vegetables and non‑steroidal anti‑inflammatory agents
are said to be protective.[5,6,11,12,16,17,21,22,27] Variables were recorded on Microsoft Excel sheet version 2016
and transferred into computer‑based Statistical Program for
Early‑onset CRC is asymptomatic in >80% of cases, but
the Social Sciences (SPSS) software version 20.0 (SPSS Inc.,
non‑specific symptoms such as malaise, weight loss, lassitude,
Chicago IL, USA) for analysis. Qualitative variables were
abdominal pain, change in bowel habits and haematochezia
summarised using mean and standard deviations and their
are less common. Similarly, late‑onset CRC (LOCRC) may be
differences determined using the t‑test. Quantitative variables
asymptomatic or identified during routine screening exercise
were grouped into proportions, median, interquartile range
on colonoscopy. However, advanced LOCRC (Stage III or IV)
and percentages and their associations determined using the
may present with distant metastasis and/or complications,[22,25]
X2 test. A confidence interval of 95% was used, and P < 0.05
features of obstruction, perforation, bleeding, abdominal
was considered statistically significant.
pain, asthenia, anaemia, altered bowel habit feeling of mass
per abdominal, bowel perforation and other constitutional
features.[11,12,22,26] Results
After thorough evaluation of the register, 135 patients
CRC prevention involves screening and lifestyle and dietary
fulfilled the colonoscopic finding of CRC with male
changes, exercise, weight reduction and removal of polyps
preponderance (63.7%). The mean age of the participants was
during screening. Drugs such as aspirin, bisphosphonates,
46.61 ± 16.03 years, with a range of 15–80 years. The modal
statins and hormones have been shown to have some protective
age was 30 years while the modal age group is 30–39 years.
effect.
Overall young and middle‑aged participants seem to have
Screening methods include faecal occult blood testing, equal frequency of occurrence amongst the study participants.
faecal immune‑histochemical test and faecal DNA, flexible Similarly, the most common presenting symptom was loose
sigmoidoscopy, computed tomography colonography, stool, followed by weight loss, anaemia and rectal bleeding.
double‑contrast barium enema and colonoscopy.[5,12,16] The detail distribution of age and clinical presentations is
The aim of this study is to evaluate retrospectively the clinical shown in Table 1.
profile of patients found with colonic tumour on endoscopy, Rectosigmoid colon was the most common area of affectation,
various sites of affectation and histology of such lesions. followed by ascending colon. Conversely, anal canal was
the least affected. Anal canal, rectosigmoid and right colon
Methodology affectations were commonly seen amongst the young, middle
aged and elderly, respectively. Similarly, colonic polyps were
This is a retrospective descriptive study of CRCs diagnosed
found to be more associated with rectosigmoid tumours.
over 10 years during endoscopy from January 2008 to
December 2017 in the Endoscopy Unit and Histopathology The most common CRC seen on histology was adenocarcinoma,
Department, Aminu Kano Teaching Hospital, Kano, Nigeria. followed by mucinous adenocarcinoma. Mucinous, signet ring
Nigerian Postgraduate Medical Journal ¦ Volume 28 ¦ Issue 1 ¦ January-March 2021 23
[Downloaded free from http://www.npmj.org on Thursday, February 25, 2021, IP: 105.112.74.61]
Musa, et al.: Colorectal cancers seen on colonoscopy in Kano, Nigeria
adenocarcinoma and villous adenoma were more common studies.[7,20,28‑30] Presence of CRC was found to be commoner
amongst the young (45.5%, 80% and 75%, respectively), among younger individuals in our study, a finding somehow
while adenocarcinoma was more common in the middle different from commonly reported figures.[7,14,19,20,31] However,
aged (46.2%). Table 2 shows the various tumour sites and these figures are in keeping with recently reported ones.[1,28]
histological subtypes identified.
Other histological lesions identified were metastatic
adenocarcinoma, squamous cell carcinoma, basal cell
carcinoma, GI stromal tumour, inflammatory myofibroblastic
tumour, angiosarcoma and adenoid cyst carcinoma.
Figures 1‑4 show the original pictures of the colonoscopic and
histologic findings of some of the patients.
Discussion
In this 10‑year review, CRC was more prevalent amongst males
with a M: F ratio of 1.75:1, a finding similar to many previous
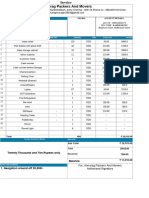
Table 1: Age distribution and clinical presentations of
patients on colonoscopy
Figure 1: Suspected tumour seen at rectosigmoid colon on
Category Variable Frequency (%) endoscopy
Age distribution of study <20 3 (2.22)
participants (years) 20-29 16 (11.85)
30-39 30 (22.22)
40-49 23 (17.04)
50-59 27 (20.00)
60-69 23 (17.04)
70-79 10 (7.41)
≥80 3 (2.22)
Presentations at Melena 6 (4.44)
colonoscopy Abdominal pain 103 (76.30)
Abdominal swelling 11 (8.15)
Rectal bleeding 94 (69.63)
Weight loss 106 (75.52)
Constipation 25 (18.52)
Anaemia 104 (77.04)
Diarrhoea 117 (86.67)
Figure 2: Photomicrography of adenocarcinoma
Table 2: Colonoscopic and histological characteristics of
suspected colorectal cancer
Attribute Name Frequency (%)
Tumour Anal canal 5 (4)
site on Rectosigmoid colon 85 (63)
colonoscopy Descending colon 12 (9)
Transverse colon 10 (7)
Ascending colon 19 (14)
Left colon 4 (3)
Histological Histology not available 24 (17.78)
diagnosis of Carcinoid tumour 2 (1.48)
suspected Adenocarcinoma 78 (57.78)
tumours
Mucinous adenocarcinoma 11 (8.15)
Signet ring cell adenocarcinoma 5 (3.70)
Tubular adenoma 4 (2.96)
Villous adenoma 4 (2.96)
Others 7 (5.19) Figure 3: Photomicrography of mucinous adenocarcinoma
24 Nigerian Postgraduate Medical Journal ¦ Volume 28 ¦ Issue 1 ¦ January-March 2021
[Downloaded free from http://www.npmj.org on Thursday, February 25, 2021, IP: 105.112.74.61]
Musa, et al.: Colorectal cancers seen on colonoscopy in Kano, Nigeria
imperative for the stakeholders concern to employ possible
means of detecting these tumours earlier through screening
programmes that could detect pre‑cancerous lesions. The
modal age group affected by this potentially preventable
disease was in their young age, and more importantly, they
were affected by histological type with worst outcome, hence
the youths may need to be considered for CRC screening
programmes.
Acknowledgement
Drs. Yussuf A Maisuna, Mohammed A Nahuche, Yusuf S Umar,
Muhammad Manko and other supporting staffs at the
Endoscopy and Histopathology Department.
Financial support and sponsorship
Nil.
Figure 4: Photomicrography of signet ring adenocarcinoma
Conflicts of interest
This is important to note in our day‑to‑day practice where There are no conflicts of interest.
we commonly consider CRC in elderly individuals and also
consider the possibility of lowering the age limit for screening References
colonoscopy in our setting. 1. Asombang AW, Madsen R, Simuyandi M, Phiri G, Bechtold M,
Ibdah JA, et al. Descriptive analysis of colorectal cancer in Zambia,
All the patients present with a myriad of symptoms ranging Southern Africa using the national cancer disease hospital database.
from diarrhoea to melena stool, with diarrhoea as the most PanAfr Med J 2018;30:1-8.
common. This shows how most of our patients present with 2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A.
advanced disease as obtained in most developing nations Global cancer statistics 2018: GLOBOCAN estimates of incidence and
mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin
from previous studies.[1,19] This calls for more enlightenment 2018;68:394-424.
amongst the public and health workers, especially doctors to 3. American Cancer Society, Inc., Surveillance Research. American Cancer
have a high index of suspicion in any patient presenting with Society. Global Cancer Facts & Figures 4th ed. Atlanta, GA 30303-1002:
some of the common features of CRC such as diarrhoea, weight American Cancer Society; 2018. Available from: http://www.cancer.org.
[Last accessed on 2020 Jan 01].
loss and anaemia regardless of their age at presentation. 4. IARC Global Cancer Observatory (Internet). International Agency for
Rectosigmoid colon is the most common site of affection Research on Cancer. Latest Global Cancer Data: Cancer Burden Rises
to 18.1 Million New Cases and 9.6 Million Cancer Deaths in; 2018.
amongst the participants consisting of almost two‑third of the Available from: http://gco.iarc.fr/. [Last accessed on 2020 Jan 01].
study findings, while anal tumour was the least frequent. This 5. Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer:
is similar to most of the reported cases in both developing and incidence, mortality, survival, and risk factors. Prz Gastroenterol
developed nations.[1,7,13,18‑20,28,30,31] 2019;14:89-103.
6. Gandomani HS, Yousefi SM, Aghajani M, Mohammadian-Hafshejani A,
Adenocarcinoma constitutes the most predominant histological Tarazoj AA, Pouyesh V, et al. Colorectal cancer in the world: Incidence,
type of CRC identified on pathological analysis, followed by mortality and risk factors. Biomed Res Ther 2017;4:1656-75.
7. Abdulkareem FB, Abudu EK, Awolola NA, Elesha SO, Rotimi O,
mucinous adenocarcinoma and signet ring adenocarcinoma. Akinde OR, et al. Colorectal carcinoma in Lagos and Sagamu,
However, about 5% of the participants have no traceable Southwest Nigeria: A histopathological review. World J Gastroenterol
histology reports, and this may likely be due to the patients 2008;14:6531-5.
taking their tissues outside the hospital for analysis. The 8. Aminu DM, Iliyasu Y, Yusuf I. Microsatellite instability profile of
colorectal cancers in Kano Northwestern Nigeria. Arch Int Surg
above histological findings go in tandem with various studies 2017;7:126.
reported previously where adenocarcinoma constitutes a modal 9. Irabor DO, Afuwape OO, Ayandipo O. The present status of the
histology pattern.[1,7,13,18,28] Mucinous adenocarcinoma and management of colon and rectal cancer in nigeria. J Cancer Res
signet ring adenocarcinoma were more common amongst the 2014;14:1-7.
10. Federal ministry of Health Nigeria (Internet). Nigeria National Cancer
young participants as reported in some studies from Nigeria
Control Plan 2018. Abuja, Nigeria: Federal ministry of Health Nigeria;
and beyond.[7,8,14,19,31] The two histological subtypes are known 2022. Available from: http://www.health.gov.ng. [Last accessed on 2019
to have poorer outcomes. This is a serious cause for concern, Dec 31].
especially considering the category participants involved. 11. Sack J, Rothman JM. Colorectal cancer: Natural history and
management. Hosp Phys 2000;36:64-73.
12. Society of Gastroenterology and Hepatology in Nigeria (SOGHIN)
Conclusion Clinical Practice Guidelines [Internet]. OAUTH Ile-Ife. Management of
colorectal cancer in Nigeria in 2016: Society of Gastroenterology and
It is obvious that CRC mainly present late in North‑Western Hepatology in Nigeria. Available from: www.soghin.org.ng. [Last cited
Nigeria in advanced stage with overwhelming symptomatology. on 2018 Aug 13].
Hence, the prognosis is usually guarded. It is, therefore, 13. Ibrahim KO, Anjorin AS, Afolayan AE, Badmos KB. Morphology of
Nigerian Postgraduate Medical Journal ¦ Volume 28 ¦ Issue 1 ¦ January-March 2021 25
[Downloaded free from http://www.npmj.org on Thursday, February 25, 2021, IP: 105.112.74.61]
Musa, et al.: Colorectal cancers seen on colonoscopy in Kano, Nigeria
colorectal carcinoma among Nigerians: A 30-year review. Niger J Clin 23. Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RG, Barzi A, et al.
Pract 2011;14:432-5. Colorectal cancer statistics, 2017. CA Cancer J Clin 2017;67:177-93.
14. Yusuf I, Atanda AT, Umar AB, Imam MI, Mohammed AZ, Ochicha O, 24. Vuik FE, Nieuwenburg SA, Bardou M, Lansdorp-Vogelaar I, Dinis-
et al. Cancer in Kano, Northwestern Nigeria : A 10 Year update of the Ribeiro M, Bento MJ, et al. Increasing incidence of colorectal cancer in
Kano cancer registry. Ann Trop Pathol 2018;8:87. young adults in Europe over the last 25 years. Gut 2019;68:1820-6.
15. Ebughe GA, Ugbem TI, Ushie DE. Cancer in cross river state. J Adv 25. Campos FG, Figueiredo MN, Monteiro M, Nahas SC, Cecconello I.
Med Med Res 2019;30:1-8. Incidence of colorectal cancer in young patients. Rev Col Bras Cir
16. Kolligs FT. Diagnostics and epidemiology of colorectal cancer. Visc 2017;44:208-15.
Med 2016;32:158-64. 26. Irabor D, Adedeji OA. Colorectal cancer in Nigeria: 40 years on.
17. Team ACS medical and Editorial Content. American Cancer Society. A review. Eur J Cancer Care (Engl) 2009;18:110-5.
Colorectal Cancer Causes, Risk Factors, and Prevention. Team ACS 27. Sierra MS, Forman D. International Agency for Research on Cancer.
medical and Editorial Content; 2018. p. 1-21. Available from: http:// Etiology of colorectal cancer (C18 – 20) in Central and South America.
www. cancer.org/cancer/colon-rectal-cancer. [Last accessed on 2020 Jan Lyon: International Agency for Research on Cancer; 2016. Available
05]. from: http://www-ep.iarc.fr/CSU_ resources. [Last accessed on 2020
18. Khiari H, Hsairi M. Colorectal cancer incidence and clinicopathological Feb 01].
features in Northern Tunisia 2007-2009. Color Cancer 2019;6:131-41. 28. Irabor DO, Arowolo A, Afolabi AA. Colon and rectal cancer in Ibadan,
19. Khougali HS, Albashir AA, Daffaalla HN, Salih M. Demographic and Nigeria: an update. Colorectal Dis 2010;12:e43-9.
clinicopathological patterns of colorectal cancer at the national cancer 29. Saber T, Bedran K, Ghandour F, El Khoury M, Bou Khalil R, Farhat S.
institute, Sudan. Saudi J Med Med Sci 2019;7:146-50. Results from a retrospective analysis of colonoscopies for Inflammatory
20. Golfam F, Golfam P, Neghabi Z. Frequency of all types of colorectal bowel disease and colorectal cancer in a Lebanese tertiary care centre.
tumors in the patients referred to selected hospitals in Tehran. Iran Red BMJ Open Gastroenterol 2017;4:e000167.
Crescent Med J 2013;15:473-6. 30. Graham A, Adeloye D, Grant L, Theodoratou E, Campbell H. Estimating
21. Wong MC, Ding H, Wang J, Chan PS, Huang J. Prevalence and risk the incidence of colorectal cancer in Sub-Saharan Africa: A systematic
factors of colorectal cancer in Asia. Intest Res 2019;17:317-29. analysis. J Glob Health [Internet]. 2012;2(2). [About 14 p.]. Available
22. Mikaeel RR, Price TJ, Smith E, Drew PA, Uylaki W, Horsnel M, et al. from: http:// www.jogh.org. [Last Citeded on 2019 Dec 23].
Colorectal cancer in Australian young adults. Mathews J Cancer Sci 31. Irabor DO. Ethnic differences in colon and rectal cancer incidence in
2019;4:1-18. Nigeria: A case of dietary determinants? Ann Niger Med 2012;6:71‑4.
26 Nigerian Postgraduate Medical Journal ¦ Volume 28 ¦ Issue 1 ¦ January-March 2021
You might also like
- A 10 Year Review of Colonoscopy at Aminu Kano Teaching Hospital, Kano NigeriaDocument5 pagesA 10 Year Review of Colonoscopy at Aminu Kano Teaching Hospital, Kano NigeriaYUSUF MUSANo ratings yet
- One Year Review of Pityriasis Rosea Among Outpatients in Kano, Northwestern NigeriaDocument4 pagesOne Year Review of Pityriasis Rosea Among Outpatients in Kano, Northwestern NigeriaEBNY MOBA & PUBG Mobile GamingNo ratings yet
- Cancer Science - 2022 - Liu - A Bayesian Network Predicting Survival of Cervical Cancer Patients Based On SurveillanceDocument11 pagesCancer Science - 2022 - Liu - A Bayesian Network Predicting Survival of Cervical Cancer Patients Based On SurveillanceRony TeguhNo ratings yet
- Development of Electrochemical Biosensor For Breast Cancer Detection Using Gold Nanoparticle Doped CA 15-3 Antibody and Antigen InteractionDocument7 pagesDevelopment of Electrochemical Biosensor For Breast Cancer Detection Using Gold Nanoparticle Doped CA 15-3 Antibody and Antigen InteractionwardaninurindahNo ratings yet
- Research Article: Gopinath P.G ., Anitha V.R ., Aruna Mastani SDocument5 pagesResearch Article: Gopinath P.G ., Anitha V.R ., Aruna Mastani SGautami SumanNo ratings yet
- An Overview of Breast Cancer Epidemiology, Risk Factors, Pathophysiology, and Cancer Risks ReductionDocument5 pagesAn Overview of Breast Cancer Epidemiology, Risk Factors, Pathophysiology, and Cancer Risks ReductionIde Yudis TiyoNo ratings yet
- Epidemiological Study On Breast Cancer Associated Risk Factors and Screening Practices Among Women in Mbaise Imo State, NigeriaDocument8 pagesEpidemiological Study On Breast Cancer Associated Risk Factors and Screening Practices Among Women in Mbaise Imo State, NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Jgo 27 E1Document10 pagesJgo 27 E1Angga Witra NandaNo ratings yet
- HPV Genotypes in High Grade Cervical Lesions and Invasive Cervical Carcinoma Detected in Gabonese WomenDocument8 pagesHPV Genotypes in High Grade Cervical Lesions and Invasive Cervical Carcinoma Detected in Gabonese WomenDian DamNo ratings yet
- Knowledge, Attitude and Practice Toward Cervical Cancer and Cervical Cancer Screening and Its Associated Factors Among Women in The City of Bamenda, CameroonDocument17 pagesKnowledge, Attitude and Practice Toward Cervical Cancer and Cervical Cancer Screening and Its Associated Factors Among Women in The City of Bamenda, CameroonEditor IJTSRDNo ratings yet
- 18 - Inian - Esophageal Cancer in India - Current Status and Future PerspectivesDocument6 pages18 - Inian - Esophageal Cancer in India - Current Status and Future PerspectivesNatalindah Jokiem Woecandra T. D.No ratings yet
- 1 s2.0 S2405844020304485 MainDocument5 pages1 s2.0 S2405844020304485 MainSome LaNo ratings yet
- Evaluation of The Algerian Pilot Program of Colorectal Cancer Screening by Immunological TestDocument9 pagesEvaluation of The Algerian Pilot Program of Colorectal Cancer Screening by Immunological TestPriyanka KilaniyaNo ratings yet
- Metaplastic Carcinoma of Breast A Series of Nine Cases From Regional Cancer Centre in North East IndiaDocument6 pagesMetaplastic Carcinoma of Breast A Series of Nine Cases From Regional Cancer Centre in North East IndiaDr SrigopalNo ratings yet
- JPCS 704 1 012011Document12 pagesJPCS 704 1 012011ferNo ratings yet
- Cancers 13 03840Document17 pagesCancers 13 03840Alaa OmarNo ratings yet
- Fnano 04 972421Document12 pagesFnano 04 972421Wildan AttariqNo ratings yet
- Exploring vismodegig A non-surgical breakthrough in the management of advanced periocular basal cell carcinomaDocument11 pagesExploring vismodegig A non-surgical breakthrough in the management of advanced periocular basal cell carcinomaGeorgios LavasidisNo ratings yet
- Ijms 25 02165Document24 pagesIjms 25 02165Adina GeambasuNo ratings yet
- WJCC 3 231Document15 pagesWJCC 3 231byk5s82mwnNo ratings yet
- ART20176809Document5 pagesART20176809dkhatri01No ratings yet
- Comparison Between The Effectiveness Fecal Immunochemical Test and Colonoscopy As A Tool For Colorectal Cancer Early DetectionDocument6 pagesComparison Between The Effectiveness Fecal Immunochemical Test and Colonoscopy As A Tool For Colorectal Cancer Early DetectioncecilliacynthiaNo ratings yet
- v07p0681 PDFDocument6 pagesv07p0681 PDFAzizaNo ratings yet
- PG Art 34580-10Document15 pagesPG Art 34580-10Horia MineaNo ratings yet
- 1541-Article Text-7468-3-10-20230531Document8 pages1541-Article Text-7468-3-10-20230531Putri WulandariNo ratings yet
- Colorectal Cancer - 2022 Review of Carcinogenesis, Global Epidemiology, Risk FactorsDocument25 pagesColorectal Cancer - 2022 Review of Carcinogenesis, Global Epidemiology, Risk FactorsRafael Salas MeléndezNo ratings yet
- Analysis of The Determinants of Low Cervical CanceDocument8 pagesAnalysis of The Determinants of Low Cervical CanceMWANGINo ratings yet
- 248413-Article Text-594567-1-10-20230527Document8 pages248413-Article Text-594567-1-10-20230527Dewi RizkiNo ratings yet
- Colorectal Cancer in The Young, Many Questions, Few AnswersDocument9 pagesColorectal Cancer in The Young, Many Questions, Few AnswersIsa AguilarNo ratings yet
- HealthcareDocument13 pagesHealthcareMaria Liliana Calderon MaciasNo ratings yet
- Ojog 2023071715010527Document9 pagesOjog 2023071715010527Julien BwamaNo ratings yet
- Go 21 00140Document10 pagesGo 21 00140Abdul HadiNo ratings yet
- NanoparticlesDocument16 pagesNanoparticlesAmi nathNo ratings yet
- Genomica Del CáncerDocument15 pagesGenomica Del CáncerDaniel PintoNo ratings yet
- Epidemiological Profile of Gynecologic Breast Cancer inDocument3 pagesEpidemiological Profile of Gynecologic Breast Cancer indomi kalondaNo ratings yet
- Impact of Knowledge and AttituDocument23 pagesImpact of Knowledge and AttituAnis SolikahNo ratings yet
- Epi of Oral CancerDocument294 pagesEpi of Oral CancerHansa KunduNo ratings yet
- Biochemical Markers of Colorectal Cancer Present and FutureDocument10 pagesBiochemical Markers of Colorectal Cancer Present and FutureMarcellia AngelinaNo ratings yet
- 2 - Cancer of The Vagina 2021 UpdateDocument9 pages2 - Cancer of The Vagina 2021 UpdateMarcell InfanteNo ratings yet
- Genotypes and Associated Risk Levels of Human Papilloma Virus Among Female Patients Attending Rabuor Sub County Hospital, KisumuDocument13 pagesGenotypes and Associated Risk Levels of Human Papilloma Virus Among Female Patients Attending Rabuor Sub County Hospital, KisumuMJBAS JournalNo ratings yet
- Adenocarcinoma Article 2021Document7 pagesAdenocarcinoma Article 2021Bapai MallikNo ratings yet
- Genetics of Cancer and Its Recent ProgressDocument8 pagesGenetics of Cancer and Its Recent ProgressAaron OsorioNo ratings yet
- 2 Erewrf 242Document5 pages2 Erewrf 242supaidi97No ratings yet
- AlbaBernal ChallengesAndDocument10 pagesAlbaBernal ChallengesAndKhairul ScNo ratings yet
- Acfs 2020 00024Document5 pagesAcfs 2020 00024Marcos OliveiraNo ratings yet
- Intl J Gynecology Obste - 2021 - Bhatla - Cancer of The Cervix Uteri 2021 UpdateDocument17 pagesIntl J Gynecology Obste - 2021 - Bhatla - Cancer of The Cervix Uteri 2021 UpdateDamian BarrancoNo ratings yet
- Nikbakht Et Al 2020 Survival Rate of Colorectal Cancer in Eastern Mediterranean Region Countries A Systematic ReviewDocument15 pagesNikbakht Et Al 2020 Survival Rate of Colorectal Cancer in Eastern Mediterranean Region Countries A Systematic ReviewAhmed HAMIMESNo ratings yet
- 1 s2.0 S092375341935241X MainDocument8 pages1 s2.0 S092375341935241X MainMaria PalNo ratings yet
- A Review On The Accuracy of Bladder Cancer Detection MethodsDocument7 pagesA Review On The Accuracy of Bladder Cancer Detection MethodsrekanihlaNo ratings yet
- Research Paper Colorectal CancerDocument4 pagesResearch Paper Colorectal Cancerxactrjwgf100% (1)
- Jibir Ibn Hayyan Medical University Colorectal Cancer ReportDocument6 pagesJibir Ibn Hayyan Medical University Colorectal Cancer Reportعلي حسين عودة العلياويNo ratings yet
- Delayed Management of Squamous Cell Carcinoma of Soft Palate: Case Report and Review of LiteratureDocument11 pagesDelayed Management of Squamous Cell Carcinoma of Soft Palate: Case Report and Review of LiteratureIJAR JOURNALNo ratings yet
- Analysis of Ovarian Tumor Pathology by Fourier Transform Infrared SpectrosDocument6 pagesAnalysis of Ovarian Tumor Pathology by Fourier Transform Infrared SpectrosDAVID ROSAS VARANo ratings yet
- Epidemiology and Factors Related To The Survival of Metastatic Kidney Cancers: Retrospective Study at The Mohamed VI Center For The Cancer Treatment in Casablanca, MoroccoDocument5 pagesEpidemiology and Factors Related To The Survival of Metastatic Kidney Cancers: Retrospective Study at The Mohamed VI Center For The Cancer Treatment in Casablanca, MoroccoInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Circulating Cell-Free DNA or Circulating Tumor DNA in The Management of Ovarian and Endometrial CancerDocument14 pagesCirculating Cell-Free DNA or Circulating Tumor DNA in The Management of Ovarian and Endometrial CancerSergio J Calleja FreixesNo ratings yet
- A Review of Computational Methods For Cervical CelDocument38 pagesA Review of Computational Methods For Cervical Celvyvie89No ratings yet
- Esophageal Cancer and Associated GenesDocument16 pagesEsophageal Cancer and Associated GenesEditor IJTSRDNo ratings yet
- A Review On Application of Biosensors For Cancer DetectionDocument5 pagesA Review On Application of Biosensors For Cancer DetectionJesifAhmedNo ratings yet
- Ecancermedicalscience 2023 Article 1610Document11 pagesEcancermedicalscience 2023 Article 1610Jose Richard Tenazoa VillalobosNo ratings yet
- Acute Kidney Injury in COVIDDocument16 pagesAcute Kidney Injury in COVIDYUSUF MUSANo ratings yet
- Abstract On Fibrosis Among HBVDocument1 pageAbstract On Fibrosis Among HBVYUSUF MUSANo ratings yet
- Jos Journal of Medicine Vol 13 No 2 2019Document93 pagesJos Journal of Medicine Vol 13 No 2 2019YUSUF MUSANo ratings yet
- Hemoperitoneum Complicating Venomous Snakebite: A Case ReportDocument4 pagesHemoperitoneum Complicating Venomous Snakebite: A Case ReportYUSUF MUSANo ratings yet
- Acute Kidney Injury in COVID-19: A Single-Center Experience in NigeriaDocument8 pagesAcute Kidney Injury in COVID-19: A Single-Center Experience in NigeriaYUSUF MUSANo ratings yet
- A 10-Year Review of Colonoscopy at Aminu Kano Teaching Hospital, Kano NigeriaDocument5 pagesA 10-Year Review of Colonoscopy at Aminu Kano Teaching Hospital, Kano NigeriaYUSUF MUSANo ratings yet
- Exam Unit 1 Out and About 1º BachilleratoDocument5 pagesExam Unit 1 Out and About 1º Bachilleratolisikratis1980No ratings yet
- TL 496 DatasheetDocument7 pagesTL 496 DatasheetAnonymous vKD3FG6RkNo ratings yet
- Guidelines For Selecting Materials For Downhole Completions Equipment (Jewellery)Document32 pagesGuidelines For Selecting Materials For Downhole Completions Equipment (Jewellery)Slim.BNo ratings yet
- Consumer Notebook Price List For September 2010Document4 pagesConsumer Notebook Price List For September 2010Anand AryaNo ratings yet
- S7 - Q2 - Answer KeyDocument11 pagesS7 - Q2 - Answer KeyRaniel LacuarinNo ratings yet
- 2020 Exam-Sample-Questions-Computer-ScienceDocument8 pages2020 Exam-Sample-Questions-Computer-ScienceNesrine LaradjiNo ratings yet
- Guidelines SLCM BWDocument60 pagesGuidelines SLCM BWpnaarayanNo ratings yet
- DANGEL 4as LESSON PLANNINGDocument2 pagesDANGEL 4as LESSON PLANNINGCarlz BrianNo ratings yet
- Cooler Ok El8sDocument11 pagesCooler Ok El8sIBRAHIM ALMANLANo ratings yet
- Powerful and Durable JCB JS200 Tracked ExcavatorDocument6 pagesPowerful and Durable JCB JS200 Tracked ExcavatorMB Viorel100% (1)
- Pcit Brochure TemplateDocument2 pagesPcit Brochure Templateapi-370829251No ratings yet
- 5.test Report - RFU-C-7Ghz IP10 Extract VersionDocument42 pages5.test Report - RFU-C-7Ghz IP10 Extract Versionminhdung.pham4713No ratings yet
- Critical Buckling Load of Pile in Liquefied SoilDocument8 pagesCritical Buckling Load of Pile in Liquefied SoilKefas JanuarNo ratings yet
- Chapter 11 RespirationDocument2 pagesChapter 11 Respirationlock_jaw30No ratings yet
- Accounting For Non Specialists Australian 7th Edition Atrill Test BankDocument26 pagesAccounting For Non Specialists Australian 7th Edition Atrill Test BankJessicaMitchelleokj100% (49)
- Titan InvoiceDocument1 pageTitan Invoiceiamdhanush017No ratings yet
- Bachelor of Arts (Psychology HR Management) Y3 V2Document1 pageBachelor of Arts (Psychology HR Management) Y3 V2Kenny sylvainNo ratings yet
- Neolithic Farming Villages Jericho and Catal HuyukDocument1 pageNeolithic Farming Villages Jericho and Catal HuyukPream BoleoNo ratings yet
- PDA Technical Documents on Sterilization ProcessesDocument3 pagesPDA Technical Documents on Sterilization ProcessesManas MishraNo ratings yet
- R4850G2 Rectifier Data Sheet 05Document2 pagesR4850G2 Rectifier Data Sheet 05PP CharlyNo ratings yet
- Computer Organization and Assembly Language: Lecture 1 - Basic ConceptsDocument13 pagesComputer Organization and Assembly Language: Lecture 1 - Basic ConceptsNosreffejDelRosarioNo ratings yet
- Families of Carbon Compounds: Functional Groups, Intermolecular Forces, & Infrared (IR) SpectrosDocument79 pagesFamilies of Carbon Compounds: Functional Groups, Intermolecular Forces, & Infrared (IR) SpectrosRuryKharismaMuzaqieNo ratings yet
- Mikes ResumeDocument2 pagesMikes Resumeapi-312645878No ratings yet
- Why War: Einstein and Freud's Little-Known Correspondence On Violence, Peace, and Human Nature by Maria PopovaDocument24 pagesWhy War: Einstein and Freud's Little-Known Correspondence On Violence, Peace, and Human Nature by Maria PopovaVagueBlurNo ratings yet
- Berkowitz Et Al (2010) - Skills For Psychological Recovery - Field Operations GuideDocument154 pagesBerkowitz Et Al (2010) - Skills For Psychological Recovery - Field Operations GuideRita CamiloNo ratings yet
- But Virgil Was Not There": The Lasting Impact of Dante's Homosocial HellDocument7 pagesBut Virgil Was Not There": The Lasting Impact of Dante's Homosocial HellЮлия ЧебанNo ratings yet
- Vici Line Card 2015Document14 pagesVici Line Card 2015Argel Linard Francisco MabagaNo ratings yet
- 6.1.2 The Solar SystemDocument4 pages6.1.2 The Solar System205 NursyazliyanaNo ratings yet
- University of Cambridge International Examinations General Certificate of Education Ordinary LevelDocument12 pagesUniversity of Cambridge International Examinations General Certificate of Education Ordinary Levelmstudy123456No ratings yet
- 2011 Mena Annual Reportv1Document73 pages2011 Mena Annual Reportv1Yasmeen LayallieNo ratings yet