Professional Documents
Culture Documents
Diagnosing Parkinson Disease.6
Diagnosing Parkinson Disease.6
Uploaded by
Cristina GhizdavetOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diagnosing Parkinson Disease.6
Diagnosing Parkinson Disease.6
Uploaded by
Cristina GhizdavetCopyright:
Available Formats
Review Article
Diagnosing Parkinson
Address correspondence to
Dr Christopher W. Hess,
Downloaded from https://journals.lww.com/continuum by lMP1W6NunxvTg6oCl3C3psNNDJfXM0kl2u96ar15u968sH/vm1eTVPVoT/Cvn2ZUiWMccFvCMV0T+uQ/Dr1PVNJFBe50R4K8xCdYPGUQNyRbHyGQLZZFwWWCw2fResdy2d0/8o6DB0HTpARZWTQrKkH+Xs0LLZ3AVpYvw4KOz6fH27bJPum9ig== on 08/28/2020
University of Florida Health
Center for Movement
Disease Disorders and
Neurorestoration, 3450 Hull
Rd, Gainesville, FL 32607,
Christopher.Hess@neurology.
Christopher W. Hess, MD; Michael S. Okun, MD, FAAN ufl.edu.
Relationship Disclosure:
Dr Hess has received personal
ABSTRACT compensation as a speaker
for the Davis Phinney
Purpose of Review: While establishing the diagnosis of Parkinson disease (PD) can Foundation and the National
be straightforward, it can be challenging in some patients, even for the experienced Parkinson Foundation, has
neurologist. The misdiagnosis rate ranges from 10% to 20% or greater depending received grant support from
the University of Florida,
on clinician experience. and has participated in CME
Recent Findings: Despite promise in the search for a biomarker that can establish and educational activities
the presence of PD and act as a marker of its progression, the diagnosis of PD continues on movement disorders
sponsored by Allergan, Ipsen,
to be based on clinical examination. Core criteria, exclusion criteria, and suppor- Mertz Pharma, PeerView
tive criteria have been developed to aid the clinician in establishing the diagnosis. Press, and QuantiaMD.
Nonmotor symptoms of PD are usually present at the time of diagnosis, may precede Dr Okun serves as a consultant
for the National Parkinson
motor symptoms, and should be specifically sought during evaluation. Ancillary testing Foundation and has received
can be appropriate, but its indications and utility must be clearly understood. research grants from the
Summary: The diagnosis of PD requires the recognition of the core features of PD Bachmann-Strauss Dystonia &
Parkinson Foundation Inc,
and the differentiation of its clinical presentation from other entities with similar and the Michael J. Fox Foundation,
potentially overlapping symptoms. A careful history and examination guided by the National Institutes of
clinical diagnostic criteria will usually establish the diagnosis of PD or uncover red Health, the National Parkinson
Foundation, the Parkinson
flags for the possibilities of other diagnoses. Appropriate selection and interpretation Alliance, Smallwood Foundation,
of ancillary testing is critical to avoid misdiagnosis and unnecessary tests. the Tourette Association of
America, Tyler’s Hope, and the
University of Florida Foundation.
Continuum (Minneap Minn) 2016;22(4):1047–1063. Dr Okun has participated as a
site principal investigator and
coinvestigator for several trials
sponsored by the National
INTRODUCTION diagnostic pitfalls. This article focuses Institutes of Health and other
on establishing the clinical diagnosis of foundations and industries, but
Parkinson disease (PD) is the second has not received compensation.
most common neurodegenerative dis- PD and discusses the evolving defini- Dr Okun has received royalties
order after Alzheimer disease. Typically, tion of PD. The article also addresses from Amazon.com Inc,
Books4Patients LLC, Cambridge
PD develops in the fifth and sixth de- when PD occurs (premotor and motor), University Press, Demos,
cades. The disease affects 1% of persons the potential for biomarkers, genetic Manson Publishing Ltd,
Smashwords, and Taylor &
over the age of 60, and up to 60,000 testing, and the role of neuroimaging in Francis Group. Dr Okun serves
new cases are diagnosed each year in the diagnosis. as associate editor for the New
England Journal of Medicine
the United States.1,2 While establishing Journal Watch Neurology, and
the diagnosis of PD in many patients is MOTOR SYMPTOMS has lectured in CME activities for
Henry Stewart Conferences &
relatively straightforward, in some pa- Parkinsonism refers to the constellation Events, PeerView Press, Prime
tients it can be quite challenging, even of bradykinesia, rigidity, resting tremor, Education Inc, QuantiaMD,
for the experienced neurologist. The and postural and gait impairments. and Vanderbilt University.
Unlabeled Use of
rate of misdiagnosis of PD likely ranges While parkinsonism can have a variety Products/Investigational
from 10% to 20% or more, depending of etiologies (Table 1-1), the most com- Use Disclosure:
Drs Hess and Okun report
on the degree of specialization of the mon cause of parkinsonism is idio- no disclosures.
diagnosing physician.3,4 Being able to pathic PD. The motor symptoms are * 2016 American Academy
identify the core features of the disease secondary to the progressive loss of do- of Neurology.
as well as to evaluate the more nu- paminergic neurons in the pars compacta
anced characteristics that typify PD and of the substantia nigra.5 These neurons
its mimics can be helpful in avoiding project to the striatum (caudate and
Continuum (Minneap Minn) 2016;22(4):1047–1063 www.ContinuumJournal.com 1047
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Diagnosing Parkinson Disease
KEY POINTS
h Parkinsonism is a clinical TABLE 1-1 Classification of Parkinsonism
syndrome that can have a
variety of possible causes, b Idiopathic parkinsonism (Parkinson disease, including sporadic and
only one of which is genetic cases)
Parkinson disease.
b Atypical parkinsonian syndromes (eg, multiple system atrophy, progressive
h There are no clinically supranuclear palsy, corticobasal syndrome)
available biomarkers to
b Heredodegenerative parkinsonism (usually other additional neurologic
indicate the presence of
symptoms are present) (eg, PLA2G6-associated neurodegeneration,
Parkinson disease or track
aceruloplasminemia, X-linked dystonia-parkinsonism, spinocerebellar ataxias)
disease progression.
b Secondary parkinsonism (drug-induced, vascular, structural, infectious,
h The diagnosis of immunologic, toxic, traumatic, metabolic)
Parkinson disease
during the patient’s
lifetime is based on the
clinical examination. putamen) and modulate corticostriatal American Academy of Neurology (AAN),
h Core criteria, exclusion transmission. PD must be distin- the most common clinical criteria used
criteria, and supportive guished from many other forms of to establish the diagnosis of idiopathic
criteria have been parkinsonism.6 Additional or atypical PD is the UK Parkinson’s Disease Society
established that can neurologic symptoms as well as key Brain Bank (UKPDSBB) clinical diag-
assist in the diagnosis aspects of the reported history can nostic criteria (Table 1-2).8 These cri-
of Parkinson disease. help point to the correct diagnosis. teria provide essential clinical findings
Despite a concerted and continued as well as supportive and exclusion-
effort to develop a biomarker that can ary criteria for diagnosing PD.
accurately confirm or refute the pres-
ence of PD and monitor disease pro- Bradykinesia
gression, none has been found. Thus, The first and most important step in
the diagnosis of PD during the patient’s diagnosing PD is to establish the pres-
lifetime is based on a careful clinical ence of bradykinesia, or slowness of
examination. Practically speaking, this movement. While akinesia (the failure
is the most important criterion as few or delay in execution of a purposeful
patients diagnosed with PD undergo movement) and hypokinesia (a de-
postmortem neuropathologic evalua- crease in movement size) are distinct
tion.7 Recently, the use of clinical criteria entities from the motor control stand-
as the practical gold standard for the point, for the purposes of the clinical
diagnosis of PD has been questioned, examination they are often included
and the manner in which PD is best under the umbrella term of bradykinesia,
defined continues to be a current topic especially when describing the de-
of interest, as the clinical diagnosis of crease and slowing of movements as
PD does not always match the patho- well as the loss or decrease of automatic
logic diagnosis (especially in genetic movements that occur in PD.9 With
forms of PD, in which the presence of continued movement, true bradykinesia
pathologic gene mutations is compli- typically gets worse (movements be-
cated by incomplete penetrance).7 come progressively smaller or decre-
These detailed discussions and debates mental), a feature that is required for
are outside the scope of this review, the UKPDSBB criteria and more recent
and this article focuses on diagnosing European guidelines.8,10 Common early
PD for the practicing clinician. manifestations of bradykinesia in PD
Although no clinical diagnostic include decreased facial expression
criteria are formally endorsed by the (hypomimia), soft speech (hypophonia),
1048 www.ContinuumJournal.com August 2016
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
TABLE 1-2 UK Parkinson’s Disease Society Brain Bank Clinical
Diagnostic Criteriaa
b Step 1: Establish the presence of bradykinesia (slowness of initiation of
voluntary movement with reduced speed and amplitude of movements and/or
the loss or decrease of automatic movements) plus at least one of the following:
Rigidity
4Y6 Hz resting tremor
Postural instability (not otherwise explained by primary visual, vestibular,
cerebellar, or proprioceptive dysfunction)
b Step 2: Evaluate for exclusionary criteria for the diagnosis of Parkinson disease
The absence of a history of:
Repeated strokes with a stepwise progression of parkinsonism
Repeated head injury
Definite encephalitis
Neuroleptic treatment at onset of symptoms
More than one affected relative (although this exclusion criterion is
no longer commonly used)
Any period of sustained remission
Oculogyric crises
Early severe autonomic involvement
Early severe dementia with disturbances of memory, language, and praxis
1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) exposure
OR a finding of:
Strictly unilateral features after 3 years
Negative response to large doses of levodopa (if malabsorption is excluded)
Supranuclear gaze palsy
Cerebellar signs
Babinski sign
Cerebral tumor or communicating hydrocephalus on neuroimaging
b Step 3: Establish the presence of three or more of the supportive criteria
for the diagnosis of Parkinson disease
Unilateral onset
Resting tremor present
Progressive disorder
Persistent asymmetry with symptoms worse on the side of onset
Clear and definite response (70Y100% improvement on Unified
Parkinson’s Disease Rating Scale) to levodopa
Severe levodopa-induced chorea
Levodopa response for 5 years or more
Clinical course of 10 years or more
a
Modified with permission from Hughes AJ, et al, J Neurol Neurosurg Psychiatry.8 B 1992
British Medical Journal Publishing Group. jnnp.bmj.com/content/55/3/181.short.
Continuum (Minneap Minn) 2016;22(4):1047–1063 www.ContinuumJournal.com 1049
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Diagnosing Parkinson Disease
KEY POINTS
h Rigidity giving rise and small handwriting (micrographia). presenting symptoms of PD. Prominent
to decreased range of The latter can be tested by asking pa- axial rigidity early in the course of symp-
motion and shoulder tients to write the same sentence at toms is not typical and is commonly
pain (often misdiagnosed least three times sequentially, observing observed in progressive supranuclear
as orthopedic or the possibility of a progressive decrease palsy (PSP).
arthritic) and difficulty in sentence length and the size of the
turning over in bed at characters. Although bradykinesia is Resting Tremor
night are common required to make the diagnosis of PD, The classic parkinsonian resting tremor
presenting symptoms of it can sometimes be difficult to elicit in is present in approximately 70% of
Parkinson disease. strongly tremor-predominant patients patients with PD.13 It is typically 4 Hz
h Parkinson tremor can with PD, especially early in the PD course. to 6 Hz and starts unilaterally and distally
fluctuate significantly in In addition to bradykinesia, at least one and, over time, progresses more proxi-
amplitude with mental additional cardinal symptom of rigidity, mally and often to the contralateral side.
activity or voluntary resting tremor, or postural instability The resting tremor can variably involve
movements of other oscillations around the wrist and finger
must be present as a second step to
limbs, and, thus, it is
make the clinical diagnosis of PD.8 joints, although a pronation/supination
not unusual to be
axis at the wrist and a pill-rolling qual-
initially described as
Rigidity ity to finger tremor are classic in PD.14
intermittent. It often has
a reemergent quality Rigidity refers to the resistance of mus- Parkinson tremor can fluctuate signifi-
such that it can reappear cles to passive movement around a cantly in amplitude with mental activity
with postural sustention joint. While rigidity is a clinical sign or voluntary movements of other limbs,
after a variable delay, and detected by the examiner, it is experi- and, thus, it is not unusual to be initially
patients may report enced and often described by patients described as intermittent.14 It often has
noticing it for the first as stiffness.9 When absent or mild on a reemergent quality such that it can
time with sustained examination, rigidity can be augmented reappear with postural sustention after
postures, such as holding by asking the patient to perform volun- a variable delay, and patients may
a telephone or newspaper. tary movements of the contralateral report noticing it for the first time with
limb. In evaluating rigidity, it is impor- sustained postures, such as holding a
tant to distinguish true parkinsonian telephone or newspaper (Case 1-1).15
rigidity from both paratonia (involuntary This manifestation can sometimes lead
variable and proportional resistance in to confusion as it can be reported as an
response to passive movement [also action tremor. Some patients also re-
known as gegenhalten]) and the cog- port a sensation of ‘‘inner tremor’’ that
wheel phenomenon that can be ob- does not involve oscillations around a
served with essential and other types of joint.16 A jerky quality to tremor can
tremor without any underlying in- sometimes be observed in younger
creased tone (Froment sign, which is patients, but in older patients this can
the increase in resistance to passive signal the presence of multiple system
movement about a joint with voluntary atrophy (MSA). Although more charac-
action in another part of the body).11 teristic of essential tremor, kinetic
Similarly, reduced arm swing on one tremor (occurring during active move-
side can be misleading without the ment) is not unusual in PD, and
appropriate clinical context, as some amelioration of tremor with alcohol
degree of arm swing asymmetry can be (due to its relaxing effects) can also be
observed in healthy adults.12 Rigidity reported in PD, emphasizing the im-
giving rise to decreased range of motion portance of the clinical examination.17
and shoulder pain (often misdiagnosed Parkinsonian tremor does not uniformly
as orthopedic or arthritic) and difficulty respond to levodopa, so occasionally
turning over in bed at night are common patients, in whom the other cardinal
1050 www.ContinuumJournal.com August 2016
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
Case 1-1 h The lack of resting
tremor does not
A 68-year-old right-handed man was referred for a neurologic evaluation of
exclude the diagnosis
tremor. The patient had first noted tremor of the right hand when driving
of Parkinson disease.
and holding a newspaper approximately 2 years previously. Initially, tremor
seemed to be intermittent, but it gradually progressed to be present h The cardinal symptoms
continuously throughout the day. Two glasses of wine in the evening could of Parkinson disease are
reduce but not stop his tremor, and he had not noticed any tremor in his bradykinesia, rigidity,
nondominant hand. He also had chronic right shoulder pain of 6-months resting tremor, and
duration for which his primary care doctor ordered a shoulder x-ray, which was postural instability.
read as normal. Despite these symptoms, he did not feel that he was h Actual falls occurring
functionally impaired in any way. Upon further questioning, he reported mild early in the disease
difficulty getting up from the low sofa in his basement, and he had both course and especially
chronic constipation and erectile dysfunction for at least 5 years. He denied in the first year of
noticing any change in his sense of smell, but his wife stated that he often presenting symptoms
commented that her cooking was less flavorful. His wife had begun to sleep should elicit suspicion
in the guest room due to the patient hitting her in his sleep. of the possibility of
His neurologic examination was remarkable for a ‘‘poker face’’ and soft an atypical form
voice, a delay in right shoulder shrug, and mild cogwheel rigidity in the right of parkinsonism.
arm that was only noticeable with voluntary movement of the opposite
hand. He had a low-amplitude, low-frequency right hand resting tremor
that reappeared with sustained posture after a short pause. His finger
movements were slightly smaller and slower on the right side, and rapid
sequential movements became progressively smaller with repetition. His
posture was slightly stooped, and he walked with decreased right arm swing
and a more pronounced pronation/supination tremor in the right wrist. He
turned easily and had normal postural stability.
Comment. This patient’s presentation is typical for tremor-predominant
idiopathic Parkinson disease. It illustrates the occurrence of the cardinal
motor symptoms of parkinsonism with multiple supportive criteria that were
preceded by nonmotor symptoms commonly reported in Parkinson disease.
symptoms of the disease are mild first year of presenting symptoms
and not noticeable, can report a lack should elicit suspicion of the possi-
of benefit from levodopa despite an bility of an atypical form of parkin-
observable improvement with levo- sonism. Postural instability is also not
dopa administration. specific to parkinsonism and is com-
monly observed in the elderly, often
Postural Instability making it the least helpful criterion
Impairment in the ability to recover in the initial diagnosis of PD, but it is
one’s balance is often very subtle in helpful in suggesting to the clinician
patients first presenting with PD and the possibility of other diagnoses or
sometimes does not develop until well comorbid diagnoses.18
into the disease course. When present
in early PD, patients will often report Other Motor Abnormalities
tripping or requiring increased con- Outside of the diagnostic criteria, other
centration to avoid tripping on uneven motor features can be seen both at the
surfaces, yet will have a normal re- time of diagnosis and as the disease
sponse to pull testing in the clinic. progresses. Impaired finger dexterity,
Actual falls occurring early in the difficulty multitasking, and increased
disease course and especially in the concentration required for both motor
Continuum (Minneap Minn) 2016;22(4):1047–1063 www.ContinuumJournal.com 1051
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Diagnosing Parkinson Disease
KEY POINT
h Nonmotor symptoms and cognitive task completion are Since the initial publication of the
such as hyposmia, common early reported symptoms, while UKPDSBB criteria, the inclusion of a
erectile dysfunction, a progressively flexed posture, freezing strong family history (more than one
constipation, and rapid phenomenon, gait initiation difficul- affected relative) has been challenged
eye movement sleep ties, postural deformities, and swal- as an exclusionary criterion and is
behavior disorder can lowing difficulties tend to appear later often overlooked in the appropriate
precede the onset of in the disease. clinical context. Other features (such
motor symptoms of as hyposmia, rapid eye movement [REM]
Parkinson disease Exclusionary and Supportive sleep behavior disorder, and constipa-
by years. Criteria for Diagnosing tion) that are known to be strongly
Parkinson Disease associated with the diagnosis of PD
The exclusionary criteria for PD listed have been proposed as additional
in Table 1-2 need to be practically formal supportive criteria, especially as
considered on an individual basis, as they often precede the motor symp-
some criteria reflect confounders in toms of the disease.8,21Y23 Although
attributing symptoms to PD while early severe dementia is an exclusion
others suggest the presence of other criterion in the UKPDSBB criteria, more
diseases. For example, a history of than 15% of patients with PD can have
multiple concussions that preceded at least mild cognitive impairment at
the onset of parkinsonism is a poten- the time of diagnosis.24 However the
tial confounder in diagnosing PD, but presence of visual hallucinations at the
it does not exclude the diagnosis of time of presentation and especially in
PD or specifically suggest an alterna- untreated patients is suggestive of
tive diagnosis. However, cerebellar dementia with Lewy bodies, which
signs or a supranuclear gaze palsy de- some argue should be considered a
veloping simultaneously with progres- subtype of PD.7
sive parkinsonism would strongly
suggest an alternative diagnosis of an NONMOTOR SYMPTOMS
atypical parkinsonism such as MSA or The function of the basal ganglia was
PSP, respectively. traditionally thought to be limited to
Supportive criteria (of which three the modulation and processing of in-
or more are required) are all charac- formation related to motor control,
teristics that commonly are observed with projections solely to motor corti-
in PD. Patients with PD usually pres- ces.25 However, it is now accepted
ent with a clear asymmetry of symp- that the basal gangliaYthalamocortical
tom onset and respond well to trials of circuits consist of multiple subcircuit
levodopa when appropriate, but this loops projecting cortically to diverse
is not always the case. Resting tremor targets.26,27 These circuits are largely
is absent in 30% of patients with PD, parallel, somatotopically arranged, and
and patients without resting tremor functionally specific, and are organized
can experience a longer delay in into motor, oculomotor, associative,
diagnosis due to physician familiarity and limbic circuits. They are involved
with the association between resting in a variety of activities including emo-
tremor and PD.19 Patients with path- tion, reward behavior and habit forma-
ologically confirmed PD can go many tion, time estimation, attention, working
years from the onset of resting tremor memory, and learning.28 Thus, it would
before developing other symptoms and be expected that the basal ganglia
might never develop unequivocal dysfunction that occurs in PD would
bradykinesia.20 produce a more complicated clinical
1052 www.ContinuumJournal.com August 2016
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
picture than isolated motor dysfunc-
tion. Similarly, basal ganglia pathology TABLE 1-3 Continued
is now recognized to be only one aspect
of the neuropathologic changes that b Gastrointestinal Dysfunction
occur in PD, which include changes Constipation (39%)
to multiple neurotransmitter systems
Early satiety (23%)
throughout the brain, further suggesting
that the clinical course of PD should Loss of appetite
include nonmotor as well as motor b Sexual Dysfunction
symptoms.29,30 The most common non- Erectile dysfunction (28%)
motor symptoms that occur in PD are
listed in Table 1-3.31 Reduced libido (42%)
Approximately 90% of patients with b Sleep Disturbances
PD will develop at least one nonmotor Excessive daytime sleepiness
symptom, and nonmotor symptoms can (28%)
be the presenting feature in PD.23,32
Insomnia (36%)
Later in the disease, the disability from
Rapid eye movement (REM)
nonmotor symptoms often overshadows
sleep behavior disorder (28%)
that from motor symptoms, and uncon-
trolled nonmotor symptoms can be a Sleep fragmentation
deciding factor in the timing of place- Vivid dreams (24%)
ment in a long-term care facility.33,34 For b Somatosensory Dysfunction
Restless legs syndrome (17%)
TABLE 1-3 Common Nonmotor Unexplained pain (20%)
Symptoms of
b Special Sensory
Parkinson Disease at the
Time of Diagnosisa,b Impaired olfaction (46%)
Impaired taste (14%)
b Affective Disorders
b Urinary Dysfunction
Anhedonia (32%)
Frequency (28%)
Anxiety (30%)
Incontinence (10%)
Apathy (31%)
Urgency (34%)
Depression (43%)
Weak urinary stream (25%)
b Autonomic Dysfunction
b Visual Disturbances
Orthostatic hypotension (21%)
Impaired color discrimination
b Cognitive Dysfunction
Visuospatial abnormalities
Bradyphrenia
a
Modified with permission from Pont-
Inattention (28%) Sunyer C, et al, Mov Disord.31 B 2014
International Parkinson and Move-
Memory impairment (32%) ment Disorder Society. onlinelibrary.
wiley.com/doi/10.1002/mds.26077/
Word-finding difficulties abstract.
b
Reported prevalence of symptom
b Fatigue (36%) (%) within a year of diagnosis when
information is available.
Continuum (Minneap Minn) 2016;22(4):1047–1063 www.ContinuumJournal.com 1053
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Diagnosing Parkinson Disease
KEY POINTS
h Parkinson disease more information, refer to the article commonly referred to as early PD in
results in a variety of ‘‘Treatment of Advanced Parkinson Dis- clinical trials (in which motor symptoms
nonmotor symptoms ease and Related Disorders’’ by Janis M. are just beginning to manifest) is a point
that can sometimes be Miyasaki, MD, MEd, FRCPC, FAAN,35 in in time that is actually relatively later
more disabling than the this issue of Continuum. In the patient in the disease course. Therefore, it has
motor symptoms, and
presenting with PD, nonmotor symp- been recognized by many experts that a
studies suggest that the potential window for disease-modifying
toms often precede or present with
nonmotor symptoms and neuroprotective treatments exists,
have a greater effect motor symptoms but are not commonly
but that earlier diagnosis and a bio-
on quality of life. reported unless uncovered by the clini-
marker are necessary. Many current
h At least two subtypes cian during the encounter.36
neuroprotective and disease-modifying
(tremor-predominant strategies are being tested in patients
PARKINSON DISEASE SUBTYPES
Parkinson disease and where presumably a large proportion
postural instability and One of the most remarkable aspects of
PD is the degree of clinical heterogeneity of neurodegeneration has already
gait difficulty Parkinson
that exists across patients, to such a de- occurred.47 A variety of terms have
disease) have been
gree that some have questioned whether been proposed, including prephys-
identified, and both of
these entities manifest PD can be considered a unified disease.7 iologic, preclinical, prodromal, premotor,
different rates of It has long been recognized that and prediagnostic, to describe the
progression, disability, considerable variability exists between various stages that can be identified
nonmotor symptoms, patients with PD in the expression of prior to the diagnosis of PD.7,48 From
and complications clinical symptoms, the rate of disease the practical and clinical standpoint, it
of therapy. is most important to remember two
progression, and the response to
main points. First, the vast majority of
therapies.37 The approaches that have
patients with PD already manifest one
been used to try to organize this het-
or more nonmotor symptoms of the
erogeneity into distinct and useful clin-
disease at the time of diagnosis and
ical subtypes have largely been based
often years prior. 23 Evaluation of
on specific clinical or demographic
nonmotor symptoms in PD is a critical
features (empirical approach) or on
part of the history at the initial presen-
methods of statistical clustering (data-
tation and should be uncovered, if
driven approach) with a variety of
present, in all patients. Second, some
classifications proposed.38 The obser- patients may have nonmotor symp-
vation that a predominance of tremor toms and mild soft signs of parkinson-
in PD portends a slower disease pro- ism, but not enough clinical findings to
gression was one of the earliest indi- confer the diagnosis of PD. In these
cators of the existence of PD subtypes patients, monitoring symptom stability
and dates back more than 45 years.39 A and progression over time is impor-
tremor-predominant phenotype has tant, especially prior to labeling the
been associated with a slower disease patient as having PD.
progression and less cognitive impair-
ment, depression, and apathy when DIFFERENTIAL DIAGNOSIS
defined empirically in data-driven stud- A myriad of diseases and syndromes can
ies and retrospective clinicopathologic be mistaken for PD, including other
studies.40Y46 forms of parkinsonism (Table 1-1)
as well as nonparkinsonian mimics.
PREDIAGNOSTIC PARKINSON Table 1-4 lists the commonly consid-
DISEASE ered differential diagnoses in the ini-
In the field of PD research, it is be- tial presentation of PD. Atypical
coming increasingly clear that what is parkinsonism can sometimes initially
1054 www.ContinuumJournal.com August 2016
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
difficult to distinguish from PD; the h Atypical parkinsonism
TABLE 1-4 Common Differential most important factor in its consider-
Diagnoses of can sometimes initially
Parkinson Disease ation is a careful and complete medica- be mistaken for
tion history (Case 1-2). In cases of idiopathic Parkinson
b Atypical parkinsonian parkinsonism with a predominance of disease. Falls and
syndromes (multiple system lower body symptoms and urinary and significant autonomic
atrophy, progressive cognitive difficulties, structural neuro- dysfunction early within
supranuclear palsy, imaging can uncover the diagnosis of the disease course, a
corticobasal syndrome) poor response to
normal pressure hydrocephalus. For
b Dementia with Lewy bodies more information on normal pressure levodopa, symmetry
of symptoms at onset,
b Drug-induced parkinsonism hydrocephalus, refer to the article ‘‘Di-
and rapid symptom
agnosis and Treatment of Idiopathic
b Dystonic tremor progression are useful
Normal Pressure Hydrocephalus’’ by red flags indicating the
b Essential tremor Michael A. Williams, MD, FAAN, and possibility of atypical
b Frontotemporal dementias Jan Malm, MD, PhD,49 in the 2016 parkinsonism.
b Functional or psychogenic
Dementia issue of Continuum. Tradi-
h Drug-induced
parkinsonism tionally, vascular parkinsonism was parkinsonism can be
thought to produce a nontremulous very difficult to
b Normal pressure
hydrocephalus
lower body predominance of symptoms distinguish from Parkinson
with a poor levodopa response and a disease; the most
b Vascular parkinsonism stepwise progression; however, signifi- important factor in its
cant overlap exists in the clinical find- consideration is a
ings of vascular and other forms of careful and complete
be mistaken for idiopathic PD. Falls parkinsonism, and the entity remains medication history.
and significant autonomic dysfunction poorly defined. MRI can be helpful in
early within the disease course, a poor the diagnosis of vascular parkinsonism
response to levodopa, symmetry of depending on the location of white
symptoms at onset, and rapid symp- matter changes.50 Functional or psy-
tom progression are useful red flags chogenic parkinsonism can usually be
indicating the possibility of atypical diagnosed readily by the recognition of
parkinsonism. The presence of other unusual or inconsistent examination
signs and symptoms can be suggestive findings.
of other diagnoses. Visual hallucina-
tions within the first year of motor LEVODOPA CHALLENGE AND
symptoms are suggestive of dementia SMELL TESTING
with Lewy bodies. Essential tremor is In some cases, clinical response to an
usually 5 Hz or faster and is most adequate dose of levodopa can be help-
prominent with action, although es- ful in establishing the PD diagnosis
sential tremor that is long-standing (Case 1-3). However, a lack of re-
can sometimes occur at rest (usually sponse to a levodopa challenge (even
bilaterally), and its frequency can fall at doses greater than 200 mg per dose)
into the parkinsonian range.11 Pa- does not strictly rule out PD, and
tients with dystonia can have mild patients with atypical parkinsonism
parkinsonism, and patients with PD can have a partial levodopa response
can occasionally present with dystonia as discussed in the article ‘‘Diagnostic
(typically lower limb dystonia in young- Approach to Atypical Parkinsonian
onset patients), although dystonia is Syndromes’’ by Nikolaus R. McFarland,
not commonly observed early in PD. MD, PhD,51 in this issue of Continuum.
Drug-induced parkinsonism can be very A levodopa challenge can be useful
Continuum (Minneap Minn) 2016;22(4):1047–1063 www.ContinuumJournal.com 1055
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Diagnosing Parkinson Disease
KEY POINT
h Laboratory testing can Case 1-2
sometimes be useful in
A 56-year-old woman with a past medical history of hypertension,
ruling out metabolic
hyperlipidemia, and refractory major depressive disorder presented for
abnormalities that may
a neurologic evaluation because of a 4-month history of difficulty walking.
present as parkinsonism.
She reported problems with handwriting due to tremor and micrographia
and difficulty getting in and out of her car. She denied any sleep
disturbances, constipation, changes in her sense of smell, or urinary dysfunction.
A CT scan of her brain ordered by her primary care doctor 1 year previously
after an episode of acute dizziness was remarkable only for mild chronic
microvascular ischemic changes. She had been tried on multiple antidepressants
but denied ever taking a neuroleptic, and none was uncovered following
inspection of her current medication bottles. Her neurologic examination
was remarkable for decreased facial expression and blink rate, bilateral
rigidity, and low-frequency resting and action tremors. Perioral tremor was
noted as well. Since she had used the same pharmacy for the last 5 years, the
pharmacy was called and a list of all recently prescribed medications was
reviewed. The list included an atypical neuroleptic that had been prescribed
for depression 2 weeks prior to the onset of her neurologic symptoms. This
medication had been discontinued the month prior to her presentation, and
her symptoms gradually improved over the next few weeks and resolved
completely within 2 months.
Comment. Although features such as a subacute onset and relative
symmetry of symptoms can suggest a secondary cause of parkinsonism
such as drug-induced parkinsonism, it may not be possible to distinguish
these entities on a clinical basis alone. An accurate history of current and
recently prescribed medications is critical in establishing the accurate
diagnosis when a patient presents with parkinsonism.
in the diagnosis of PD; however, the from PSP or corticobasal degeneration
absence of a response to levodopa does as less olfactory impairment occurs in
not rule out PD and can result from these diseases compared to MSA.52
gastric emptying issues. Thus, in these
cases, clinicians will sometimes order a LABORATORY TESTING
gastric emptying study to uncover this There are currently no available labo-
potential issue. ratory tests that can establish the
Olfactory impairment can be a diagnosis of PD, despite a number of
useful screening test for PD, and recent potential serum-based biomarkers un-
European guidelines recommend its der evaluation.53 In patients with less
use in the differentiation of PD from than a classical presentation or an ap-
atypical and secondary parkinsonism.10 propriate history, exclusion of thyroid
A number of smell-identification tests and parathyroid dysfunction (which can
are commercially available, including result in parkinsonism) and basic labo-
the University of Pennsylvania Smell ratory testing (including liver function
Identification Test, Brief Smell Iden- tests) can be useful in ruling out sec-
tification Test, and Sniffin’ Sticks. A ondary causes of parkinsonism. In ad-
caveat of such tests is their low speci- dition, any patient who is less than
ficity, as decreased sense of smell can 50 years old and presenting with
be seen in normal aging and other parkinsonism should be screened for
neurodegenerative diseases. It may be Wilson disease with appropriate copper
more helpful in differentiating PD studies including serum ceruloplasmin
1056 www.ContinuumJournal.com August 2016
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINT
h Genetic testing in
Case 1-3 Parkinson disease
A 60-year-old right-handed woman presented for a second neurologic opinion is generally not
for the diagnosis of parkinsonism. She had developed masked face, stiffness, recommended except
and slowing in her activities of daily living 3 years earlier, and she had been for very specific
diagnosed with parkinsonism the following year. She had been started on patient populations.
carbidopa/levodopa 25 mg/100 mg 1 tablet 3 times a day, which she had
continued, but she had not noticed any benefit. Over the past year she had
developed freezing when going through doorways and when turning to get
into a chair. Over the past 6 months she had fallen backward multiple times,
and she reported a subjective difficulty with swallowing and bothersome
urinary urgency and frequency. She had been frustrated by her lack of
improvement and heard about ‘‘the brain scan that could diagnose Parkinson
disease’’ in her support group and requested it to be ordered. Neurologic
examination was remarkable for masked facies, hypophonia, moderately
asymmetric rigidity and bradykinesia, and diffusely increased reflexes without
tremor. She had a lack of postural response on pull testing, and mental
status examination was within normal limits.
Comment. This patient presented with a parkinsonian syndrome with the
most important differential diagnosis being Parkinson disease versus an
atypical parkinsonism such as multiple system atrophyYparkinsonism type.
Neuroimaging of the dopamine transporter will be abnormal in both diseases
and would not add any additional useful diagnostic or treatment information.
A further titration of her levodopa to at least 900 mg/d (up to 300 mg per dose
if she can tolerate it) to determine her responsiveness to an adequate dose of
carbidopa/levodopa would be far more helpful in clarifying her diagnosis.
levels, and 24-hour urine copper excre- the diagnosis of PD recommends con-
tion should be considered. For more sideration of specific gene testing in
information, refer to the article ‘‘Wilson patients without a family history of PD
Disease’’ by Ronald F. Pfeiffer, MD, but onset before the age of 40, patients
FAAN,54 in this issue of Continuum. with a strong family history of either a
recessive pattern of inheritance (espe-
GENETIC TESTING cially with onset before the age of 50)
Most patients (approximately 90%) or an autosomal dominant pattern of
diagnosed with PD do not have a family inheritance, and patients who belong
history of the disease and are, there- to ethnic groups associated with foun-
fore, considered to be sporadic cases.55 der mutations.10 These recommenda-
While monogenic forms of PD have tions are very similar to those put forth
been identified and may provide insight by the Consortium on Risk for Early-
into the pathophysiology and genetic Onset Parkinson Disease (CORE PD) in
heterogeneity of PD, they constitute a 2010.58 In such patients, genetic test-
very small portion of patients with PD.56 ing can be helpful in family and finan-
Recently, alleles that are more com- cial planning, aiding in prognosis, or in
mon in the general population and patients with a strong personal desire
that may increase the risk for PD have for testing.
been identified.57 No formal guidelines Clinicians also need to be aware that
exist regarding which patients with PD the first direct-to-consumer genetic
should be considered for genetic test- tests have been approved by the US
ing. A recent European guideline for Food and Drug Administration (FDA)
Continuum (Minneap Minn) 2016;22(4):1047–1063 www.ContinuumJournal.com 1057
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Diagnosing Parkinson Disease
KEY POINT
h While the research and may become available for PD.59 diseases, FDG-PET is currently lim-
utility of dopamine These tests can potentially mislead ited to the differentiation of Alzheimer
transporter single-photon asymptomatic patients into thinking disease and frontotemporal dementia.
emission computed they are sure to develop the disease if FDG-PET may be especially useful in
tomography is universally they are positive for an allele that the differentiation of atypical parkin-
agreed upon, its use increases the risk of PD, or that they sonism in the future as the research in
in the clinical setting are no longer at increased risk when this area evolves.64
for differential diagnosis a single gene or a limited number of In 2011, ioflupane I-123 single-
in the individual genes are tested. Any decision to pur- photon emission computed tomogra-
remains controversial. sue clinical genetic testing should be phy (SPECT) was approved in the
preceded by genetic counseling and United States as an adjunctive evalua-
family discussions to ensure patients tion tool for use in the diagnosis of
are aware of the implications for them- suspected parkinsonian syndromes.
selves and their families. This compound binds to the presyn-
aptic dopamine transporter (DAT) and
NEUROIMAGING acts as a marker for dopamine levels in
The clinical utility of structural neuro- the striatum. While the research utility
imaging in the evaluation of PD has of DAT-SPECT is universally agreed
traditionally been limited to ruling upon, its use in the clinical setting for
out secondary causes of parkinsonism, differential diagnosis in the individual
such as vascular parkinsonism or nor- remains controversial.65
mal pressure hydrocephalus, as MRI It is generally agreed on by experts
and CT are largely unremarkable in PD that DAT-SPECT does not currently
beyond generalized cortical atrophy. have a role in the differentiation of PD
Most experts make a bedside decision from other neurodegenerative forms
on the need for structural neuroimag- of parkinsonism as DAT binding will
ing on a case-by-case basis, and the most be reduced in all of these entities
recent AAN practice parameter on diag- (Case 1-3). Further, progression of
nosing PD did not render a recommen- PD cannot yet be followed by DAT-
dation regarding the need for structural SPECT as it has not been shown to
imaging prior to making the diagnosis define a clear and reliable relationship
of PD. However, structural imaging is between DAT binding and disease
often recommended to rule out sec- severity.66 Therefore, DAT-SPECT is
ondary causes of parkinsonism.60 Novel currently limited to the differentiation
techniques of diffusion, perfusion, and of a neurodegenerative parkinsonian
functional MRI (fMRI) continue to be syndrome from entities such as essential
developed and show promise as po- tremor, dystonia, or secondary causes
tential biomarkers of PD.61,62 of parkinsonism. Yet even in these
Metabolic imaging with fludeoxyglu- populations, findings are not always
cose positron emission tomography straightforward. DAT binding would be
(FDGYPET) measures regional differ- expected to be normal in essential
ences in glucose metabolism, and these tremor and thus useful for ruling out a
studies have uncovered patterns of dopamine deficiency in the long-
activity that are characteristic for the standing patient with essential tremor
motor and cognitive symptoms of PD, who has developed a superimposed
as well as patterns specific to atypical slowing of movement speed beyond
forms of parkinsonism such as MSA or that which can be seen in essential
PSP.17,63 Although approved in the tremor.11 It should also be normal in
United States for neurodegenerative dystonia, which is believed to account
1058 www.ContinuumJournal.com August 2016
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
for a significant proportion of patients
clinically diagnosed with PD who had TABLE 1-5 Relevant Drug Interactions With Dopamine
Transporter Single-Photon Emission Computed
DAT imaging scans without evidence Tomography (DAT-SPECT)a
of dopaminergic deficit (SWEDD).67
Yet even in such patients, false positives Effect on DAT-SPECT Time to Be Stopped Prior to
have been reported and some patients and Drug DAT-SPECT
with essential tremor may have mild Minor effectb
abnormalities with DAT imaging.68,69
Amantadine 6 days
Similarly, patients with parkinsonism
who have normal DAT-SPECT imaging Budipine 6 days
have been reported to both transition Citalopram 8 days
to abnormal scans on follow-up and Clomipramine 21 days
respond well to dopaminergic therapy.70
Duloxetine 3 days
Rarely, patients with vascular parkinson-
ism and drug-induced parkinsonism Ephedrine, epinephrine, 6Y10 hours
phenylephrine,
can also have abnormal DAT-SPECT
pseudoephedrine
imaging, and in these patient groups
its utility may be primarily focused on Escitalopram 8 days
those patients observed to have nor- Fluoxetine 45 days
mal DAT binding and a clinical presen- Fluvoxamine 5 days
tation of parkinsonism.66 However, DAT Imipramine 5 days
is usually negative in cases of drug-
Memantine 5 days
induced parkinsonism.
DAT-SPECT also has a number of Paroxetine 5 days
limitations that need to be considered, Sertraline 6 days
even when used judiciously. With the Venlafaxine 3 days
exception of a few studies that have Ziprasidone 2 days
included clinicopathologic correlation, c
Significant effect
most studies that have evaluated the ac-
curacy of DAT-SPECT in the diagnosis Amphetamine 7 days
of PD have used the clinical diagnosis Benztropine 5 days
of PD as the gold standard, which is Bupropion or 8 days
obviously problematic when one is amfebutamone
looking to the DAT-SPECT for support- Cocaine 2 days
ive data when the clinical diagnosis is
Dextroamphetamine 7 days
not clear.71 Additionally, interpretation
of the DAT-SPECT is currently qualita- Mazindol 3 days
tive, with a binary normal or abnormal Methylamphetamine 3 days
reading assigned based on visual in- Methylphenidate 2 days
spection. While objective quantitative
Modafinil 3 days
measures of DAT binding have been
developed, they are not currently clin- Phentermine 14 days
ically available.72 a
Modified with permission from Kägi G, et al. J Neurol Neurosurg Psychiatry.73
If DAT-SPECT imaging is pursued, it B 2010 BMJl Publishing Group Ltd. jnnp.bmj.com/content/81/1/5.abstract.
b
is important to note that a number of May have small effect on uptake (at most 15%). This is acceptable for routine
DAT-SPECT but not for research.
commonly prescribed medications can c
All of these drugs are likely to alter (usually decrease) radioligand uptake by at
interfere with DAT binding and pro- least 20% and often substantially more and, therefore, have to be stopped
prior to routine DAT-SPECT.
duce erroneous results (Table 1-5).73
Most of the drugs listed in this resource
Continuum (Minneap Minn) 2016;22(4):1047–1063 www.ContinuumJournal.com 1059
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Diagnosing Parkinson Disease
KEY POINT
h If dopamine transporter reduce DAT binding (potentially can emerge over time, it is important for
single-photon emission resulting in a false-positive interpreta- the clinician to continue to follow the
computed tomography tion). The duration of discontinuation patient long-term, monitor the exami-
imaging is pursued, it is recommended for some of these agents nation, and document the response to
important to note that a is significant (such as for some of the dopaminergic therapy. In many cases,
number of commonly selective serotonin reuptake inhibitors the diagnosis may be revised based on
prescribed medications [SSRIs]), and the decision to stop medi- the emergence of a pattern of symp-
can interfere with cations needs to be considered on an toms suggesting an atypical parkinso-
dopamine transporter individual basis. In contrast, dopami- nian syndrome or other diagnosis.
binding and produce nergic medications such as levodopa and
erroneous results.
dopamine agonists are generally not held REFERENCES
prior to scanning, as their influence on 1. de Lau LM, Breteler MM. Epidemiology of
DAT binding is not thought to be a Parkinson’s disease. Lancet Neurol 2006;5(6):
significant confounder.73 Recommenda- 525Y535. doi:10.1016/S1474-4422(06)70471-9.
tions on which medications to hold 2. Tanner CM, Goldman SM. Epidemiology of
Parkinson’s disease. Neurol Clin 1996;14(2):
prior to DAT scanning and for how long 317Y335. doi:10.1016/S0733-8619(05)70259-0.
have yet to be agreed upon by experts.
3. Jellinger KA. How valid is the clinical diagnosis
of Parkinson’s disease in the community?
CONCLUSION J Neurol Neurosurg Psychiatry 2003;74(7):
Making an accurate diagnosis of PD in 1005Y1006. doi:10.1136/jnnp.74.7.1005.
the early stages of the disease can be 4. Wermuth L, Lassen CF, Himmerslev L, et al.
Validation of hospital register-based
challenging. A careful history and
diagnosis of Parkinson’s disease.
examination guided by clinical diag- Dan Med J 2012;59(3):A4391.
nostic criteria will usually establish PD
5. Ehringer H, Hornykiewicz O. Verteilung von
or alternatively uncover red flags sug- Noradrenalin und Dopamin (3-hydroxytyramin)
gesting other diagnoses. The symptoms im Gehirn des Menschen und ihr Verhalten
bei Erkrankungen des extrapyramidalen
of PD can be variable, and subtypes
systems. Klin Wochenschr 1960;38:
exist that have differing clinical symp- 1236Y1239.
toms and rates of progression. Some 6. Fahn S, Jankovic J, Hallett M. Principles and
patients may not fulfill criteria for the practice of movement disorders. 2nd ed.
clinical diagnosis in the initial stages New York, NY: Elsevier/Saunders, 2011.
of their disease. The key is to closely 7. Berg D, Postuma RB, Bloem B, et al.
follow patients, as disease progression Time to redefine PD? Introductory
statement of the MDS Task Force on
usually gives the answer. Over time, the definition of Parkinson’s disease.
patients initially suspected of having PD Mov Disord 2014;29(4):454Y462.
will either have their diagnosis solidi- doi:10.1002/mds.25844.
fied by their clinical course and re- 8. Hughes AJ, Daniel SE, Kilford L, Lees AJ.
Accuracy of clinical diagnosis of idiopathic
sponse to medication or an alternative Parkinson’s disease: a clinico-pathological
diagnosis will emerge. Structural neu- study of 100 cases. J Neurol Neurosurg
roimaging and laboratory testing can be Psychiatry 1992;55(3):181Y184.
doi:10.1136/jnnp.55.3.181.
helpful in ruling out other diseases.
While imaging of the striatal DAT can 9. Mazzoni P, Shabbott B, Cortés JC.
Motor control abnormalities in
be useful in specific situations, clinical Parkinson’s disease. Cold Spring Harb
evaluation by a movement disorders Perspect Med 2012;2(6):a009282.
specialist or neurologist experienced in doi:10.1101/cshperspect.a009282.
movement disorders is usually ade- 10. Berardelli A, Wenning GK, Antonini A, et al.
EFNS/MDS-ES/ENS [corrected] recommendations
quate to the establish the diagnosis of for the diagnosis of Parkinson’s disease.
PD for most patients presenting with Eur J Neurol 2013;20(1):16Y34.
parkinsonism. Since other PD syndromes doi:10.1111/ene.12022.
1060 www.ContinuumJournal.com August 2016
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
11. Thenganatt MA, Louis ED. Distinguishing 24. Kang GA, Bronstein JM, Masterman DL,
essential tremor from Parkinson’s disease: et al. Clinical characteristics in early
bedside tests and laboratory evaluations. Parkinson’s disease in a central
Expert Rev Neurother 2012;12(6):687Y696. California population-based study. Mov
doi:10.1586/ern.12.49. Disord 2005;20(9):1133Y1142. doi:10.1002/
12. Plate A, Sedunko D, Pelykh O, et al. mds.20513.
Normative data for arm swing asymmetry: 25. Middleton FA, Strick PL. Basal ganglia and
how (a)symmetrical are we? Gait Posture cerebellar loops: motor and cognitive
2015;41(1):13Y18. doi:10.1016/ circuits. Brain Res Brain Res Rev 2000;
j.gaitpost.2014.07.011. 31(2Y3):236Y250. doi:10.1016/S0165-
13. Hughes AJ, Ben-Shlomo Y, Daniel SE, Lees AJ. 0173(99)00040-5.
What features improve the accuracy 26. Obeso JA, Rodrı́guez-Oroz MC,
of clinical diagnosis in Parkinson’s Benitez-Temino B, et al. Functional
disease: a clinicopathologic study. organization of the basal ganglia:
Neurology 1992;42(6):1142Y1146. therapeutic implications for Parkinson’s
doi:10.1212/WNL.42.6.1142. disease. Mov Disord 2008;23(suppl 3):
14. Hess CW, Pullman SL. Tremor: clinical S548YS559. doi:10.1002/mds.22062.
phenomenology and assessment techniques. 27. Alexander GE, DeLong MR, Strick PL. Parallel
Tremor Other Hyperkinet Mov (N Y) 2012;2. organization of functionally segregated
pii: tre-02-65-365-1. circuits linking basal ganglia and cortex.
Annu Rev Neurosci 1986;9:357Y381.
15. Jankovic J, Schwartz KS, Ondo W. Re-emergent
doi:10.1146/annurev.ne.09.030186.002041.
tremor of Parkinson’s disease. J Neurol
Neurosurg Psychiatry 1999;67(5):646Y650. 28. Obeso JA, Rodriguez-Oroz MC, Stamelou M,
doi:10.1136/jnnp.67.5.646. et al. The expanding universe of disorders
of the basal ganglia. Lancet 2014;384
16. Shulman LM, Singer C, Bean JA, Weiner WJ.
(9942):523Y531. doi:10.1016/S0140-6736
Internal tremor in patients with Parkinson’s
(13)62418-6.
disease. Mov Disord 1996;11(1):3Y7.
doi:10.1002/mds.870110103. 29. Braak H, Del Tredici K, Rüb U, et al.
17. Kraus PH, Lemke MR, Reichmann H. Staging of brain pathology related to
Kinetic tremor in Parkinson’s diseaseVan sporadic Parkinson’s disease. Neurobiol
underrated symptom. J Neural Transm Aging 2003;24(2):197Y211. doi:10.1016/S0197-
2006;113(7):845Y853. doi:10.1007/ 4580(02)00065-9.
s00702-005-0354-9. 30. Sung VW, Nicholas AP. Nonmotor symptoms
18. Weiner WJ, Nora LM, Glantz RH. Elderly in Parkinson’s disease: expanding the view
inpatients: postural reflex impairment. of Parkinson’s disease beyond a pure motor,
Neurology 1984;34(7):945Y947. pure dopaminergic problem. Neurol Clin
doi:10.1212/WNL.34.7.945. 2013;31(3 suppl):S1YS16. doi:10.1016/
j.ncl.2013.04.013.
19. Breen DP, Evans JR, Farrell K, et al.
Determinants of delayed diagnosis in 31. Pont-Sunyer C, Hotter A, Gaig C, et al.
Parkinson’s disease. J Neurol 2013; The onset of nonmotor symptoms in
260(8):1978Y1981. doi:10.1007/s00415- Parkinson’s disease (the ONSET PD study).
013-6905-3. Mov Disord 2015;30(2):229Y237. doi:10.1002/
mds.26077.
20. Selikhova M, Kempster PA, Revesz T,
et al. Neuropathological findings in 32. Park A, Stacy M. Non-motor symptoms
benign tremulous parkinsonism. in Parkinson’s disease. J Neurol 2009;
Mov Disord 2013;28(2):145Y152. 256(suppl 3):293Y298. doi:10.1007/
doi:10.1002/mds.25220. s00415-009-5240-1.
21. Lees AJ, Hardy J, Revesz T. Parkinson’s 33. Seppi K, Weintraub D, Coelho M, et al.
disease. Lancet 2009;373(9680):2055Y2066. The Movement Disorder Society
doi:10.1016/S0140-6736(09)60492-X. Evidence-Based Medicine Review Update:
treatments for the non-motor symptoms
22. Reichmann H. Clinical criteria for the of Parkinson’s disease. Mov Disord
diagnosis of Parkinson’s disease. 2011;26(suppl 3):S42YS80. doi:10.1002/
Neurodegener Dis 2010;7(5):284Y290. mds.23884.
doi:10.1159/000314478.
34. Hely MA, Morris JG, Reid WG, Trafficante R.
23. Shulman LM, Taback RL, Bean J, Weiner WJ. Sydney Multicenter Study of Parkinson’s
Comorbidity of the nonmotor symptoms disease: non-L-dopa-responsive problems
of Parkinson’s disease. Mov Disord 2001; dominate at 15 years. Mov Disord 2005;
16(3):507Y510. doi:10.1002/mds.1099. 20(2):190Y199. doi:10.1002/mds.20324.
Continuum (Minneap Minn) 2016;22(4):1047–1063 www.ContinuumJournal.com 1061
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Diagnosing Parkinson Disease
35. Miyasaki JM. Treatment of advanced therapy in Parkinson’s disease. Mov Disord
Parkinson disease and related disorders. 2013;28(1):86Y95. doi:10.1002/mds.24997.
Continuum (Minneap Minn) 2016; 48. Siderowf A, Lang AE. Premotor Parkinson’s
22(4 Movement Disorders):1104Y1116. disease: concepts and definitions. Mov
36. O’Sullivan SS, Williams DR, Gallagher DA, Disord 2012;27(5):608Y616. doi:10.1002/
et al. Nonmotor symptoms as presenting mds.24954.
complaints in Parkinson’s disease: a 49. Williams MA, Malm J. Diagnosis and
clinicopathological study. Mov Disord 2008;23(1): treatment of idiopathic normal pressure
101Y106. doi:10.1002/mds.21813. hydrocephalus. Continuum (Minneap Minn)
2016;22(2 Dementia):579Y599.
37. Zetusky WJ, Jankovic J, Pirozzolo FJ. The
heterogeneity of Parkinson’s disease: 50. Vizcarra JA, Lang AE, Sethi KD, Espay AJ.
clinical and prognostic implications. Vascular Parkinsonism: deconstructing a
Neurology 1985;35(4):522Y526. doi:/10.1212/ syndrome. Mov Disord 2015;30(7):886Y894.
doi:10.1002/mds.26263.
WNL.35.4.522.
38. Marras C, Lang A. Parkinson’s disease 51. McFarland NR. Diagnostic approach to
subtypes: lost in translation? J Neurol atypical parkinsonian syndromes. Continuum
Neurosurg Psychiatry 2013;84(4):409Y415. (Minneap Minn) 2016;22(4 Movement
doi:10.1136/jnnp-2012-303455. Disorders):1117Y1142.
52. Wenning GK, Shephard B, Hawkes C, et al.
39. Hoehn MM, Yahr MD. Parkinsonism: onset,
Olfactory function in atypical parkinsonian
progression and mortality. Neurology
syndromes. Acta Neurol Scand 1995;91(4):
1967;17(5):427Y442.
247Y250.
40. Rajput AH, Voll A, Rajput ML, et al. Course 53. Chahine LM, Stern MB, Chen-Plotkin A.
in Parkinson disease subtypes: a 39-year Blood-based biomarkers for Parkinson’s
clinicopathologic study. Neurology disease. Parkinsonism Relat Disord
2009;73(3):206Y212. doi:10.1212/ 2014;20(suppl 1):S99YS103. doi:10.1016/
WNL.0b013e3181ae7af1. S1353-8020(13)70025-7.
41. Oh JY, Kim YS, Choi BH, et al. Relationship 54. Pfeiffer RF. Wilson disease. Continuum
between clinical phenotypes and cognitive (Minneap Minn) 2016;22(4 Movement
impairment in Parkinson’s disease (PD). Arch Disorders):1246Y1261.
Gerontol Geriatr 2009;49(3):351Y354. 55. Thomas B, Beal MF. Parkinson’s disease.
doi:10.1016/j.archger.2008.11.013. Hum Mol Genet 2007;16(spec no. 2):
42. Burn DJ, Landau S, Hindle JV, et al. R183YR194. doi:10.1093/hmg/ddm159.
Parkinson’s disease motor subtypes and 56. Klein C, Westenberger A. Genetics of
mood. Mov Disord 2012;27(3):379Y386. Parkinson’s disease. Cold Spring Harb
doi:10.1002/mds.24041. Perspect Med 2012;2(1):a008888.
43. Reijnders JS, Ehrt U, Lousberg R, et al. The doi:10.1101/cshperspect.a008888.
association between motor subtypes and 57. Gasser T. Usefulness of genetic testing
psychopathology in Parkinson’s disease. in PD and PD trials: a balanced review.
Parkinsonism Relat Disord 2009;15(5):379Y382.
J Parkinsons Dis 2015;5(2):209Y215.
doi:10.1016/j.parkreldis.2008.09.003. doi:10.3233/JPD-140507.
44. Jankovic J, McDermott M, Carter J, et al. 58. Alcalay RN, Caccappolo E, Mejia-Santana H,
Variable expression of Parkinson’s disease:
et al. Frequency of known mutations in
a base-line analysis of the DATATOP cohort. The early-onset Parkinson disease: implication
Parkinson Study Group. Neurology 1990;40(10): for genetic counseling: the consortium on
1529Y1534. doi:10.1212/WNL.40.10.1529.
risk for early onset Parkinson disease study.
45. Lewis SJ, Foltynie T, Blackwell AD, et al. Arch Neurol 2010;67(9):1116Y1122.
Heterogeneity of Parkinson’s disease in the doi:10.1001/archneurol.2010.194.
early clinical stages using a data driven 59. US Food and Drug Administration.
approach. J Neurol Neurosurg Psychiatry
FDA permits marketing of first
2005;76(3):343Y348. doi:10.1136/ direct-to-consumer genetic carrier test for
jnnp.2003.033530. Bloom syndrome. www.fda.gov/NewsEvents/
46. Selikhova M, Williams DR, Kempster PA, Newsroom/PressAnnouncements/
et al. A clinico-pathological study of UCM435003. Updated February 23, 2015.
subtypes in Parkinson’s disease. Brain Accessed June 7, 2016.
2009;132(pt 11):2947Y2957. doi:10. 60. Pahwa R, Lyons KE. Early diagnosis of
1093/brain/awp234.
Parkinson’s disease: recommendations from
47. Lang AE, Melamed E, Poewe W, Rascol O. diagnostic clinical guidelines. Am J Manag
Trial designs used to study neuroprotective Care 2010;16(suppl implications):S94YS99.
1062 www.ContinuumJournal.com August 2016
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
61. Baglieri A, Marino MA, Morabito R, et al. 2016;87(3):319Y323. doi:10.1136/
Differences between conventional and jnnp-2004-310256.
nonconventional MRI techniques in
68. A multicenter assessment of dopamine
Parkinson’s disease. Funct Neurol
transporter imaging with DOPASCAN/SPECT
2013;28(2):73Y82. doi:10.11138/FNeur/
in parkinsonism. Parkinson Study Group.
2013.28.2.073.
Neurology 2000;55(10):1540Y1547.
62. Ofori E, Pasternak O, Planetta PJ, et al. doi:10.1212/WNL.55.10.1540.
Longitudinal changes in free-water
within the substantia nigra of Parkinson’s 69. Waln O, Wu Y, Perlman R, et al.
disease. Brain 2015;138(pt 8):2322Y2331. Dopamine transporter imaging in essential
doi:10.1093/brain/awv136. tremor with and without parkinsonian
features. J Neural Transm (Vienna)
63. Poston KL, Eidelberg D. FDG PET in the 2015;122(11):1515Y1521. doi:10.
evaluation of Parkinson’s disease. PET Clin 1007/s00702-015-1419-z.
2010;5(1):55Y64. doi:10.1016/j.cpet.
2009.12.004. 70. Menéndez-González M, Tavares F, Zeidan N,
et al. Diagnoses behind patients with
64. Stoessl AJ, Brooks DJ, Eidelberg D.
hard-to-classify tremor and normal
Milestones in neuroimaging. Mov Disord
DaT-SPECT: a clinical follow up study.
2011;26(6):868Y978. doi:10.1002/mds.23679.
Front Aging Neurosci 2014;6:56.
65. Perlmutter JS, Eidelberg D. To scan or not doi:10.3389/fnagi.2014.00056.
to scan: DaT is the question. Neurology
71. de la Fuente-Fernández R, Lövblad KO.
2012;78(10):688Y689. doi:10.1212/
DaTscan and Parkinson’s disease: DAT
WNL.0b013e3182494c72.
binding should not lead to binding decisions
66. Ba F, Martin WR. Dopamine transporter in clinical practice. Eur J Neurol 2014;21(11):
imaging as a diagnostic tool for parkinsonism 1351Y1352. doi:10.1111/ene.12458.
and related disorders in clinical practice. 72. Scherfler C, Nocker M. Dopamine transporter
Parkinsonism Relat Disord 2015;21(2):87Y94. SPECT: how to remove subjectivity?
doi:10.1016/j.parkreldis.2014.11.007. Mov Disord 2009;24(suppl 2):S721YS724.
67. Erro R, Schneider SA, Stamelou M, et al. doi:10.1002/mds.22590.
What do patients with scans without 73. Kägi G, Bhatia KP, Tolosa E. The role of
evidence of dopaminergic deficit (SWEDD) DAT-SPECT in movement disorders. J Neurol
have? New evidence and continuing Neurosurg Psychiatry 2010;81(1):5Y12.
controversies. J Neurol Neurosurg Psychiatry doi:10.1136/jnnp.2008.157370.
Continuum (Minneap Minn) 2016;22(4):1047–1063 www.ContinuumJournal.com 1063
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Coronary Artery Diseases Case StudyDocument20 pagesCoronary Artery Diseases Case StudyPyka Izzaty67% (3)
- Propanolol and Spironolactone Drug StudyDocument2 pagesPropanolol and Spironolactone Drug StudyLisette Castillo91% (11)
- Ethics Case StudyDocument9 pagesEthics Case Studyapi-305128971100% (1)
- Trastornos Del Ritmo CircardianoDocument38 pagesTrastornos Del Ritmo CircardianoHabib G. Moutran BarrosoNo ratings yet
- Tratamiento Farmacológico Trastornos Sueño REMDocument24 pagesTratamiento Farmacológico Trastornos Sueño REMHabib G. Moutran BarrosoNo ratings yet
- Trastornos Del Sueño en AMSDocument17 pagesTrastornos Del Sueño en AMSHabib G. Moutran BarrosoNo ratings yet
- Trastornos RBD en Atrofia de Múltiples SistemasDocument10 pagesTrastornos RBD en Atrofia de Múltiples SistemasHabib G. Moutran BarrosoNo ratings yet
- REM Sleep - ReviewDocument4 pagesREM Sleep - ReviewHabib G. Moutran BarrosoNo ratings yet
- REM - RBD ReviewDocument8 pagesREM - RBD ReviewHabib G. Moutran BarrosoNo ratings yet
- The Best Evidence For Progressive Myoclonic Epilepsy - A Pathway To Precision TherapyDocument11 pagesThe Best Evidence For Progressive Myoclonic Epilepsy - A Pathway To Precision TherapyHabib G. Moutran BarrosoNo ratings yet
- Rapid Eye Movement Sleep Behaviour Disorder - ReviewDocument10 pagesRapid Eye Movement Sleep Behaviour Disorder - ReviewHabib G. Moutran BarrosoNo ratings yet
- Neurologist Communicationg The Diagnosis of ELADocument9 pagesNeurologist Communicationg The Diagnosis of ELAHabib G. Moutran BarrosoNo ratings yet
- Brain Injury After Cardiac Arrest - From Prognostication of Comatose Patients To RehabilitationDocument12 pagesBrain Injury After Cardiac Arrest - From Prognostication of Comatose Patients To RehabilitationHabib G. Moutran BarrosoNo ratings yet
- Approach To Neurologic InfectionsDocument18 pagesApproach To Neurologic InfectionsHabib G. Moutran Barroso100% (1)
- POEMS Syndrome - A Report of 14 Cases and Review of The LiteratureDocument6 pagesPOEMS Syndrome - A Report of 14 Cases and Review of The LiteratureHabib G. Moutran BarrosoNo ratings yet
- CNS Diseases and UveitisDocument25 pagesCNS Diseases and UveitisHabib G. Moutran BarrosoNo ratings yet
- Afasia Primaria Progresiva y Apraxia Del Habla Continuum 2019Document27 pagesAfasia Primaria Progresiva y Apraxia Del Habla Continuum 2019Habib G. Moutran BarrosoNo ratings yet
- The Role of Diet in Multiple Sclerosis - A ReviewDocument16 pagesThe Role of Diet in Multiple Sclerosis - A ReviewHabib G. Moutran BarrosoNo ratings yet
- Dementia, Autonomy, and Unexpected HappinessDocument5 pagesDementia, Autonomy, and Unexpected HappinessHabib G. Moutran BarrosoNo ratings yet
- Check List Suturing Aseptik - Revisi 19-01-10Document4 pagesCheck List Suturing Aseptik - Revisi 19-01-10Arief Yunan PriyoutomoNo ratings yet
- Endometab Exam 2018Document8 pagesEndometab Exam 2018teabagmanNo ratings yet
- Sedation Policy LPCH 6 11Document24 pagesSedation Policy LPCH 6 11Tribowo WicaksonoNo ratings yet
- Kuliah 8. Anestesi - Syok Dan Tata LaksananyaDocument63 pagesKuliah 8. Anestesi - Syok Dan Tata LaksananyaDesi Suryani DewiNo ratings yet
- Leadership Skills For NursesDocument34 pagesLeadership Skills For NursesAdelaine Dalang-Ano100% (2)
- Open-Cap Acrylic SplintDocument3 pagesOpen-Cap Acrylic SplintFeras Al-ZbounNo ratings yet
- Midface-Lifting Evolution, Indications, and TechniqueDocument6 pagesMidface-Lifting Evolution, Indications, and Techniquedoctorban100% (1)
- Mazen Slim CV-UAEDocument4 pagesMazen Slim CV-UAEJoshua MorrowNo ratings yet
- Header LpuDocument3 pagesHeader LpuL.a.ZumárragaNo ratings yet
- 10th PICU NICU Final AnnouncementDocument29 pages10th PICU NICU Final AnnouncementdrtiwikNo ratings yet
- Hypoxic Ischaemic Encepalopathy - Nicole StevensDocument38 pagesHypoxic Ischaemic Encepalopathy - Nicole Stevenslena gutsanNo ratings yet
- Pain Management Clinical Guidelinesv2 PDFDocument15 pagesPain Management Clinical Guidelinesv2 PDFErwin Novia Rachmawati100% (1)
- Prochaska - Why Don't Continents Move Why Don't People ChangeDocument20 pagesProchaska - Why Don't Continents Move Why Don't People ChangeBraňo KrajčovičNo ratings yet
- Anterior CaptekDocument35 pagesAnterior CaptekcalitoswayNo ratings yet
- Hospital and Health Care FacilitiesDocument7 pagesHospital and Health Care FacilitiesToteng TanglaoNo ratings yet
- DementiaDocument1 pageDementiaidno1008No ratings yet
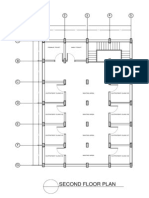
- 2nd Floor Plan PDFDocument1 page2nd Floor Plan PDFNeal Cristian PerlasNo ratings yet
- Amended Pma Code of EthicsDocument46 pagesAmended Pma Code of EthicsUlaysaNo ratings yet
- Principles of Cancer TreatmentDocument7 pagesPrinciples of Cancer TreatmentRenatoCosmeGalvanJuniorNo ratings yet
- Plotino On Bleaching JOE 2008Document14 pagesPlotino On Bleaching JOE 2008Mary DsbNo ratings yet
- Factors Affecting Sleep Nursing and Medical NewDocument13 pagesFactors Affecting Sleep Nursing and Medical NewMaryGraceVelascoFuentesNo ratings yet
- Organizing NSG ServiceDocument28 pagesOrganizing NSG ServiceAnusha VergheseNo ratings yet
- Pulmonary Leukostasis Mimicking Pulmonary Embolism: Case of The MonthDocument4 pagesPulmonary Leukostasis Mimicking Pulmonary Embolism: Case of The MonthkaremiaNo ratings yet
- Nursing Care Plan Cord CareDocument1 pageNursing Care Plan Cord CareMelanie Bagasol SisonNo ratings yet
- Foot Drop: Where, Why and What To Do?: ReviewDocument13 pagesFoot Drop: Where, Why and What To Do?: ReviewFrancisco Escobar MoralesNo ratings yet
- Interview Questions To PrepareDocument7 pagesInterview Questions To Prepareico_isNo ratings yet
- (Surg3b) Pediatric Surgery (Resurreccion) - PauzkiDocument13 pages(Surg3b) Pediatric Surgery (Resurreccion) - PauzkiAra CasalsNo ratings yet