Professional Documents
Culture Documents
Association of Histamine 2 Blockers And.7
Uploaded by
Diana AngelesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Association of Histamine 2 Blockers And.7
Uploaded by
Diana AngelesCopyright:
Available Formats
OBSERVATIONAL STUDY
Association of Histamine-2 Blockers and
Proton-Pump Inhibitors With Delirium
Development in Critically Ill Adults:
A Retrospective Cohort Study
Ami Shiddapur, BS1
OBJECTIVES: Histamine-2 receptor antagonists are commonly administered for Christine E. Kistler, MD, MASc2,3
stress ulcer prophylaxis in critically ill adults and may be associated with delirium
Jan Busby-Whitehead, MD2
development. We aimed to determine differential associations of histamine-2 re-
ceptor antagonist or proton-pump inhibitor administration with delirium develop- C. Adrian Austin, MD, MSCR2,4
ment in patients admitted to a medical ICU.
Downloaded from http://journals.lww.com/ccejournal by BhDMf5ePHKbH4TTImqenVA+lpWIIBvonhQl60EtgtdlLYrLzSPu+hQedJnbNaXBf on 08/13/2021
DESIGN: Retrospective observational study using a deidentified database
sourced from the University of North Carolina Health Care system. Participants
were identified as having delirium utilizing an International Classification of
Diseases-based algorithm. Associations among histamine-2 receptor antagonist,
proton-pump inhibitor, or no medication administration and delirium were identi-
fied using relative risk. Multiple logistic regression was used to control for poten-
tial confounders including mechanical ventilation and age.
SETTING: Academic tertiary care medical ICU in the United States.
PATIENTS: Adults admitted to the University of North Carolina medical ICU from
January 2015 to December 2019, excluding those on concurrent histamine-2 re-
ceptor antagonists and proton-pump inhibitors in the same encounter.
INTERVENTIONS: None.
MEASUREMENTS AND MAIN RESULTS: We identified 6,645 critically ill
patients, of whom 29% (n = 1,899) received mechanical ventilation, 45% (n = 3,022)
were 65 or older, and 22% (n = 1,487) died during their medical ICU encounter. Of
the 6,645 patients, 31% (n = 2,057) received an histamine-2 receptor antagonist
and no proton-pump inhibitors, 40% (n = 2,648) received a proton-pump inhibitor
and no histamine-2 receptor antagonists, and 46% (n = 3,076) had delirium. The
histamine-2 receptor antagonist group had a greater association with delirium than
the proton-pump inhibitor group compared with controls receiving neither medica-
tion, after controlling for mechanical ventilation and age (risk ratio, 1.36; 1.25–1.47;
p < 0.001) and (risk ratio, 1.15; 1.07–1.24; p < 0.001, respectively). Copyright © 2021 The Authors.
CONCLUSIONS: Histamine-2 receptor antagonists are more strongly associ- Published by Wolters Kluwer Health,
Inc. on behalf of the Society of Critical
ated with increased delirium than proton-pump inhibitors. Prospective studies are
Care Medicine. This is an open-access
necessary to further elucidate this association and to determine if replacement of
article distributed under the terms of
histamine-2 receptor antagonists with proton-pump inhibitors in ICUs decreases
the Creative Commons Attribution-
the burden of delirium in critically ill patients. Non Commercial-No Derivatives
KEY WORDS: critical care; delirium; histamine H2 antagonists; mechanically License 4.0 (CCBY-NC-ND), where it
ventilated; older adults; proton-pump inhibitors is permissible to download and share
the work provided it is properly cited.
D
The work cannot be changed in any
elirium is an acute decline in cognitive function associated with way or used commercially without
multiple adverse outcomes such as an increased fall risk, prolonged permission from the journal.
hospital stay, and a two- to three-fold increased risk of death (1–3). DOI: 10.1097/CCE.0000000000000507
Critical Care Explorations www.ccejournal.org 1
Shiddapur et al
Delirium is frequently encountered in the ICU set- Care System. Researchers can apply criteria for patient
ting, with older ICU patients facing the highest disease demographics, encounter information, International
burden, for whom delirium rates are as high as 80% Classification of Diseases, 9th Revision (ICD-9) and
(1). Medications are a common inciting factor for de- International Classification of Diseases, 10th Revision
lirium development and are responsible for 12–39% of diagnoses, ICD-9 procedure codes, vitals, laboratory
cases (4). As delirium is often resolved upon cessation results, and medications. In response to a query, i2b2
of the inciting medication, it is critical to identify po- returns the number of patients matching the search
tentially risky medications, especially those that are criteria. No patient identifiers or clinical data are re-
commonly prescribed. vealed in the result set.
An estimated 70% of patients admitted to ICUs re- The Institutional Review Board (IRB) at the UNC at
ceive proton-pump inhibitors (PPIs) and histamine-2 Chapel Hill (UNC-CH) waived approval and informed
receptor antagonists (H2RAs) for stress ulcer prophy- consent due to the aggregated level of the data (IRB
laxis (5). H2 receptor antagonism in the brain can No. 20-1073).
dampen neural cholinergic stimulation and adversely
affect arousal, wakefulness, and attention to cause de- Study Population and Cohort Definition
lirium (6, 7). Anti-histaminergic effects of H2RAs
should be localized to the gastric mucosa; however, Deidentified patient data from the UNC-CH i2b2 da-
H2 receptors are also widely distributed in the brain, tabase was queried to include all critically ill patients
creating the potential for delirium precipitation in eld- admitted to the UNC-CH Memorial Hospital Medical
erly patients with compromised blood-brain barriers ICU (UNCMH MICU) during the study period.
(6, 8–10). In studies of long-term hospitalized patients, UNCMH is a large tertiary care center with an active
H2RAs have been associated with variable rates of CNS 30-bed MICU. This ICU is well-versed in delirium
symptoms such as psychosis, agitation, hallucinations, assessment and management. The UNC-CH MICU
mental status changes, and disorientation, with rates was one of the study centers for the Modifying the
ranging from 1.6% to 80% (6, 11–14). Impact of ICU-Associated Neurological Dysfunction
Prior retrospective studies have demonstrated study and The Society of Critical Care Medicine's ICU
greater prevalence of delirium in critically ill patients Liberation Bundle Project. The Confusion Assessment
taking H2RAs rather than PPIs and have reported Method for the ICU is the standard delirium assess-
reduced delirium severity after patients taking H2RAs ment method in the UNCMH MICU, and it is per-
were switched to PPIs (15–19). These studies are limited formed at least once per nursing shift (every 12 hr).
in number and have low generalizability due to strict Participants were excluded if they had dual use of
inclusion criteria and small sample size. We sought to both H2RAs and PPIs during their hospitalization,
better characterize the association between delirium as this reflects a unique population and was unlikely
and medications commonly used for stress ulcer pro- to represent those receiving routine care. Eligibility
phylaxis in a large, heterogeneous ICU sample. was not limited to any specific medical indications
for either H2RA or PPI use. Participants were 18
MATERIALS AND METHODS and older. Mechanical ventilation was screened for
using CPT codes 5A1935Z, 5A1945Z, and 5A1955Z.
Setting and Design
Death during hospitalization was identified using
We conducted a retrospective, observational study discharge dispositions of “expired” or “expired in
using the Informatics for Integrating Biology and the medical facility.” We also collected data on routine
Bedside (i2b2) to gather patient data from January patient demographics such as age, race, ethnicity,
2015 to December 2019. i2b2 is a self-service way for and sex.
researchers to examine patient cohorts by querying The H2RA group was defined as having no PPI use
the Carolina Data Warehouse for Health (CDW-H). and having one or more instances of administration of
The CDW-H is a central data repository containing the following medications: famotidine, cimetidine, ra-
clinical, research, and administrative data sourced nitidine, and nizatidine. The PPI group was defined as
from the University of North Carolina (UNC) Health having no H2RA use and having one or more instances
2 www.ccejournal.org August 2021 • Volume 3 • Number 8
Observational Study
of administration of the following medications: dex- Statistical Analysis
lansoprazole, esomeprazole, esomeprazole/naproxen,
Statistical analysis was conducted using Stata statistical
pantoprazole, rabeprazole, lansoprazole, omeprazole,
software (Release 16; StataCorp LLC, College Station,
magnesium hydroxide/omeprazole/sodium bicarbo-
TX). Descriptive statistics were used to report basic
nate, omeprazole/sodium bicarbonate. The control co-
demographic characteristics of the entire cohort. We
hort was comprises patients with no instances of either
collapsed age into a dichotomous variable with those
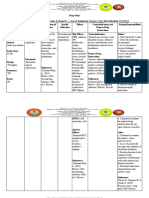
PPI or H2RA administration (Fig. 1).
less than 65 years old versus those 65 years and older.
We conducted a univariate binomial regression to ob-
Outcomes
tain the relative risk of delirium development among
We defined delirium development based on the al- patients on H2RAs compared with controls. We also
gorithm delineated by Kim et al (20), in which conducted within-group univariate regressions to ex-
a set of specific ICD codes was found to best cap- amine the associations of age and mechanical ven-
ture delirium diagnosis in a retrospective analysis tilation with delirium. This was repeated for the PPI
of electronic medical records. Presence of one or group. We then conducted univariate analyses to ex-
more instances of any of these codes was used as a amine whether any individual PPI might be more
marker for delirium (Table S1, Supplemental Digital associated with delirium than another. We also com-
Content, http://links.lww.com/CCX/A750). i2b2 pared delirium development among those on H2RAs
queries were structured such that administration of compared with those on PPIs, excluding control
the medication of interest had to occur in the same patients not on medications, in a univariate binomial
encounter (MICU stay) as delirium development. regression. Lastly, we conducted multivariate modi-
Cohort grouping methods are outlined in Figure 1. fied Poisson regressions to examine the associations of
H2RA and PPI groups were further stratified by in- H2RAs or PPIs with delirium, controlled for patient
dividual medication to assess for differences in de- characteristics found to be significantly associated
lirium associations between single agents. with delirium in the previous univariate regressions.
Figure 1. Flow diagram of patient cohort selection in Informatics for Integrating Biology and the Bedside. H2RA = histamine-2 receptor
antagonist, MICU = medical ICU, PPI = proton-pump inhibitor, UNCMH = University of North Carolina at Chapel Hill Memorial Hospital.
Critical Care Explorations www.ccejournal.org 3
Shiddapur et al
We also conducted a stratified analysis by any patient Group Characteristics: Age, Mechanical
characteristic that changed the risk ratio (RR) of either Ventilation, and Mortality Among the H2RA and
an H2RA or PPI with delirium by more than 10% upon PPI Groups
addition to the multivariate model. p values less than
Patients on H2RAs were less likely to be 65 or older
0.01 were considered statistically significant.
compared with those on PPIs or those on neither
medication (41% [95% CI, 39–43%] vs 50% [48–52%]
RESULTS and 44% [42–46%], respectively) (Table 1). However,
Cohort Characteristics patients on H2RAs had higher inhospital mechanical
ventilation rates (54% [52–56%] vs 24% [22–26%] or
Between January 2015 and December 2019, 8,075 8% [7–9%], respectively) and higher inhospital mor-
adults were admitted to the UNC-CH MICU. Of these tality rates than patients on PPIs or control patients on
patients, 6,645 were included in the cohort after re- neither drug (27% [25–29%] vs 23% [21–24%] or 16%
moval of the 1,430 patients prescribed both H2RAs [14–18%], respectively).
and PPIs in the same hospital encounter. In the re-
maining cohort, 45% (n = 3,022) were 65 or older, 29%
(n = 1,899) received mechanical ventilation, and 22% Association of Group Characteristics and
H2RA and PPI Use With Delirium in Unadjusted
(n = 1,487) died during their MICU encounter. Of the
Analysis
6,645 patients, 31% (n = 2,057) received an H2RA and
no PPIs, 40% (n = 2,648) received a PPI and no H2RAs, Patients 65 or older had a small but statistically sig-
and 46% (n = 3,076) had a delirium diagnosis (Table 1). nificantly higher relative risk of delirium than younger
Over 99% of patients (n = 2,048) who received H2RAs patients (RR, 1.07; 1.02–1.13; p = 0.008). Mechanical
were prescribed famotidine. Of those who received a ventilation was significantly associated with increased
PPI, 70% (n = 1,839) were prescribed pantoprazole delirium compared with nonmechanically ventilated
and 20% (n = 517) were prescribed omeprazole. The patients (RR, 1.69; 1.61–1.78; p < 0.001). The risk of
remainder were prescribed esomeprazole (1%, n = 14) delirium was significantly higher in the H2RA group
and other PPIs. and the PPI group than controls (RR, 1.61; 1.50–1.73;
TABLE 1.
Cohort Characteristics
Entire Control Histamine-2 Receptor Proton-Pump
Cohort, Group, Antagonist Group, Inhibitor Group,
Cohort Characteristics n = 6,645, n (%) n = 1,937, n (%) n = 2,057, n (%) n = 2,648, n (%)
Female 3,224 (49) 1,051 (50 1,016 (49) 1,220 (46)
Race
White or Caucasian 3,956 (60) 1,096 (57) 1,187 (58) 1,671 (63)
Black or African American 1,925 (29) 579 (30) 640 (31) 706 (27)
Other/unknown 621 (9) 211 (11) 186 (9) 221 (8)
Age
18–44 1,257 (19) 478 (25) 466 (23) 315 (12)
45–64 2,363 (36) 601 (31) 748 (36) 1,014 (38)
65 and above 3,022 (45) 857 (44) 843 (41) 1,319 (50)
Mechanical ventilation 1,899 (29) 157 (8) 1,109 (54) 633 (24)
Deceased during hospitalization 1,487 (22) 309 (16) 559 (27) 596 (23)
Delirium 3,076 (46) 685 (35) 1,169 (57) 1,188 (45)
4 www.ccejournal.org August 2021 • Volume 3 • Number 8
Observational Study
p < 0.001) and (RR, 1.27; 1.18–1.37; p < 0.001, respec- respectively). In both of the multivariate analyses, after
tively). Risk of delirium was significantly higher in adjusting for older age, the risk of delirium in patients
the H2RA group than that in the PPI group (RR, 1.27; on either H2RAs or PPIs did not change significantly,
1.20–1.34; p < 0.001). or by more than 10% of their unadjusted value. Thus,
age was not a significant confounder of the association
Association of Group Characteristics and H2RA between H2RA or PPI use and delirium. However, the
and PPI Use With Delirium in Adjusted Analysis risk of delirium in patients on either H2RAs or PPIs
changed significantly after adjusting for mechanical
We built two multivariate models to assess the asso-
ventilation, suggesting the presence of confounding.
ciation of medication administration (either H2RA or
PPI), age, and ventilation status with delirium. Within
Stratification by Ventilation Status
the H2RA model in the adjusted analysis, H2RA use,
older age, and mechanical ventilation were significantly When patient groups were stratified by ventilation
associated with delirium development (RR, 1.35; 1.25– status to account for confounding, mechanically ven-
1.47; p < 0.001), (RR, 1.19; 1.11–1.26; p < 0.001), and tilated patients on H2RAs or on PPIs had significantly
(RR, 1.44; 1.33–1.55; p < 0.001, respectively) (Table 2). greater associations with delirium compared with ven-
In the adjusted PPI models, PPI use, older age, and tilated controls on neither medication (RR, 1.41; 1.19–
mechanical ventilation were significantly associated 1.67; p < 0.001) and (RR, 1.40; 1.17–1.67; p < 0.001,
with delirium development (RR, 1.15; 1.07–1.24; respectively) (Fig. 2). However, no significant differ-
p < 0.001), (RR, 1.11; 1.03–1.19; p = 0.003), and (RR, ence in ventilated patients was present between H2RA
1.65; 1.54–1.78; p < 0.001, respectively) (Table 3). and PPI associations with delirium when compared to
Risk of delirium was significantly higher in the H2RA each other (RR, 1.01; 0.94–1.08; p = 0.81).
group than that in the PPI group (RR, 1.10; 1.04–1.17; In the nonmechanically ventilated patient set,
p = 0.001). patients on H2RAs had significant associations with
When stratifying by individual PPIs given and delirium compared with nonventilated controls (RR,
controlling for mechanical ventilation and age, pan- 1.33; 1.21–1.46; p < 0.001). Patients on PPIs did not
toprazole was significantly associated with delirium have a significant association with delirium (RR, 1.12;
development, whereas omeprazole was not (RR, 1.15; 1.02–1.21; p = 0.012). In nonventilated patients, H2RAs
1.06–1.24; p = 0.001) and (RR, 1.00; 0.89–1.14; p = 0.93, had significantly greater associations with delirium
TABLE 2.
Relative Risk of Delirium Development by Cohort Characteristics on Histamine Blockers
(n = 2,057)
No Absolute
Delirium, Delirium, Unadjusted Difference, Adjusted
Cohort Characteristics n (%) n (%) RR (95% CI) p % RR (95% CI)a p
H2RAb (n =2,057) 1,169 (57) 888 (43) 1.61 (1.50–1.73) < 0.001 22 1.35 (1.25–1.47) < 0.001
Proton-pump inhibitor/H2RA 685 (35) 1,252 (65)
control (n = 1,937)
≥ 65 yr old (n = 843) 504 (60) 339 (40) 1.17 (1.10–1.25) < 0.001 5 1.18 (1.11–1.26) < 0.001
< 65 yr old (n = 1,214) 665 (55) 549 (45)
Mechanically ventilated (n = 1,109) 737 (66) 372 (34) 1.68 (1.57–1.78) < 0.001 20 1.44 (1.33–1.55) < 0.001
Not ventilated (n = 948) 432 (46) 516 (54)
H2RA = histamine-2 receptor antagonist, RR = risk ratio.
a
Adjusted for mechanical ventilation and age.
b
Compared with control group.
Critical Care Explorations www.ccejournal.org 5
Shiddapur et al
TABLE 3.
Relative Risk of Delirium Development by Cohort Characteristics on Proton-Pump Inhibitors
(n = 2,648)
No Absolute
Delirium, Delirium, Unadjusted Difference, Adjusted
Cohort Characteristics n (%) n (%) RR (95% CI) p % RR (95% CI)a p
PPIb (n = 2,648) 1,188 (45) 1,460 (55) 1.26 (1.18–1.37) < 0.001 10 1.15 (1.07–1.24) < 0.001
PPI/histamine-2 receptor 685 (35) 1,252 (65)
antagonist control (n = 1,937)
≥ 65 yr old (n = 1,319) 574 (44) 745 (56) 1.10 (1.02–1.17) 0.010 2 1.11 (1.03–1.86) 0.003
< 65 yr old (n = 1,329) 614 (46) 715 (54)
Mechanically ventilated (n = 633) 417 (66) 216 (34) 1.71 (1.59–1.83) < 0.001 28 1.65 (1.54–1.78) < 0.001
Not ventilated (n = 2,015) 771 (38) 1,244 (62)
PPI = proton-pump inhibitor, RR = risk ratio.
a
Adjusted for mechanical ventilation and age.
b
Compared with control group.
than PPIs, contrasting with the previous finding in renal or liver failure, septic shock, extracorporeal
ventilated patients (RR, 1.19; 1.09–1.30; p < 0.001). membrane oxygenation, or major operative proce-
dures including transplants (23, 24). UNC treatment
DISCUSSION guidelines indicate the use of H2RAs as the first-line
drugs for stress ulcer prophylaxis. PPIs are second-line
In this retrospective observational cohort study of
drugs and are administered to higher risk patients.
MICU patients, we found that H2RAs were more
Concern for potential confounding by indication was
strongly associated with increased risk of delirium
lessened by the fact that H2 blockers were prescribed
than PPIs. Overall, 46% of our MICU cohort devel-
to lower risk patients but were still more significantly
oped delirium, in agreement with previous studies,
where the rate of delirium in ICUs has been reported associated with delirium than PPIs.
to range from 20% to 80% (1, 2, 21). Mechanical ven- Our main finding mirrored the overall conclusion
tilation and increased age also demonstrated a signif- of other smaller studies found in the literature search
icant association with delirium, in accordance with that characterized H2RA use, PPI use, and delirium.
prior literature (22). The association between H2RAs In a prospective study of 21 Japanese hepatectomized
and delirium was most significant for those not me- recipients, patients were randomized to treatment
chanically ventilated. with either famotidine or omeprazole for postoper-
In nonventilated patients, those on H2RAs had a ative ulcer management. The incidence rates and se-
statistically significant 12% absolute increase in de- verity of delirium were significantly higher in the
lirium development compared with those receiving no famotidine group (90%) than the omeprazole group
medications. Those on PPIs had a nonsignificant 4% (27.3.%) (odds ratio, 3.82; 1.15–12.71; p < 0.01) (18).
increase in the frequency of delirium. Given the lack The second study retrospectively studied rates of de-
of treatments for delirium, the ability to reduce the in- lirium in 60 postsurgical esophageal cancer patients
cidence of delirium by over 10% might represent an treated with either H2RAs or PPIs for ulcer prevention.
important opportunity for reducing the morbidity and The incidence of delirium was significantly higher in
mortality seen in ICUs. the H2RA group (43.3%) than the PPI group (16.7%)
In the UNCMH MICU, indications for stress ulcer (p = 0.047). Additionally, in the 11 patients from the
prophylaxis include mechanical ventilation greater H2RA group who developed delirium, switch from an
than 48 hours, coagulopathy, severe trauma or burn, H2RA to a PPI reduced delirium severity (19).
6 www.ccejournal.org August 2021 • Volume 3 • Number 8
Observational Study
Figure 2. Percent of patients developing delirium in relation to type of medication administered, stratified by ventilation status. H2RA =
histamine-2 receptor antagonist, PPI = proton-pump inhibitor.
Compared with these studies, our analysis had a In the United States overall, PPIs are prescribed more
much larger sample size, fewer exclusion criteria, and widely than H2RAs for hospitalized patients (27–29).
controlled for potential confounders such as mechan- Prior literature concerning the differential efficacy of
ical ventilation. These differences could account for the the agents for upper gastrointestinal bleed prophylaxis
discrepancy in absolute percentages of delirium; in our is conflicting, and studies suggest that PPIs are associ-
cohort, 57% of patients on H2RAs developed delirium, ated with higher rates of pneumonia and Clostridium
compared with 45% of patients on PPIs. Unlike the difficile infection, as well as increased healthcare costs
aforementioned studies, ours also used nonmedicated (28, 30). Compared with PPIs, H2RAs demonstrate
control groups to generate RRs. Future clinical trials greater rates of tachyphylaxis (31).
may be needed to determine the benefits of switching This study’s strengths include a large sample size and
from an H2RA to a PPI in critically ill patients for de- limited exclusion criteria. This study also has important
lirium prevention. limitations. This was a retrospective, observational sin-
In our mechanically ventilated patient group, both gle-site study, meaning that causation could not be es-
H2RAs and PPIs were associated with an increased tablished, and generalizability is limited. Furthermore,
risk of delirium development, and there was no statisti- we were unable to assess the temporal relationships
cally significant difference in the delirium risk between between events using i2b2. We could not establish
H2RAs and PPIs. This suggests an underlying mech- the order of medication administration, ventilation,
anism of delirium related to ventilation or medications and delirium development within a hospitalization.
taken during ventilation. Studies have postulated that Additionally, association strength may have increased
mechanical ventilation can increase the permeability as a patient requiring H2RAs or PPIs may have had
of the blood-brain barrier (25). Furthermore, me- other risk factors that predisposed them to delirium,
chanically ventilated patients usually have a higher independent of the medications themselves. These po-
medication burden than nonventilated patients (26). tential confounders include use of deliriogenic medi-
Potential deliriogenic effects of H2RAs or PPIs could cations, comorbidities such as prior gastrointestinal
be outweighed by these factors relating to mechanical pathology, and prior delirium diagnoses. To minimize
ventilation; this finding points to a need for further bias, we adjusted for age and ventilation status, two of
research. the most contributory risk factors to delirium devel-
Further work will need to examine the risk-benefit opment. Finally, though we used the currently most
ratio of H2RAs versus PPIs, including delirium risk. thoroughly vetted set of ICD and antipsychotic codes
Critical Care Explorations www.ccejournal.org 7
Shiddapur et al
to abstract a delirium diagnosis, this algorithm was For information regarding this article, E-mail: as4304@mynsu.
shown to identify delirium with a sensitivity of 30%, nova.edu
a specificity of 97%, and a positive predictive value of The content is solely the responsibility of the authors and does
not necessarily represent the official views of the National
83% (20). Furthermore, this algorithm showed higher Institutes of Health.
sensitivity for hyperactive or mixed delirium (64%) This work was performed at University of North Carolina at
and severe delirium (73%). Due to this, our study may Chapel Hill.
have under-abstracted delirium diagnoses, especially
milder or hypoactive delirium cases.
REFERENCES
CONCLUSIONS 1. Ely EW, Margolin R, Francis J, et al: Evaluation of delirium in
critically ill patients: Validation of the Confusion Assessment
In a large, retrospective study of 6,645 critically ill Method for the Intensive Care Unit (CAM-ICU). Crit Care Med
adults, H2RA exposure was more strongly associ- 2001; 29:1370–1379
ated with delirium than PPI exposure. This associ- 2. Pandharipande PP, Ely EW, Arora RC, et al: The intensive care
delirium research agenda: A multinational, interprofessional
ation could be limited by underlying confounders
perspective. Intensive Care Med 2017; 43:1329–1339
outside the scope of the study design, as the database 3. Pandharipande PP, Girard TD, Jackson JC, et al; BRAIN-ICU
used could not abstract delirium subtypes or relevant Study Investigators: Long-term cognitive impairment after crit-
comorbidities, nor establish a temporal association. ical illness. N Engl J Med 2013; 369:1306–1316
Prospective studies are necessary to further elucidate 4. Clegg A, Young JB: Which medications to avoid in people
at risk of delirium: A systematic review. Age Ageing 2011;
this association, eliminate confounders, and determine
40:23–29
if replacement of H2RAs with PPIs in ICUs decreases 5. Young PJ, Bagshaw SM, Forbes AB, et al: Effect of stress
the burden of delirium in high-risk patients. ulcer prophylaxis with proton pump inhibitors vs histamine-2
receptor blockers on in-hospital mortality among ICU patients
receiving invasive mechanical ventilation: The PEPTIC ran-
ACKNOWLEDGMENTS domized clinical trial. JAMA 2020; 323:616–626
6. Chazot PL, Johnston L, Mcauley E, et al: Histamine and de-
We acknowledge the editorial assistance of biostatis- lirium: Current opinion. Front Pharmacol 2019; 10:299
ticians at the NC Translational and Clinical Sciences 7. Maldonado JR: Delirium pathophysiology: An updated hy-
Institute. pothesis of the etiology of acute brain failure. Int J Geriatr
Psychiatry 2018; 33:1428–1457
8. Naja M, Zmudka J, Hannat S, et al: In geriatric patients, de-
1 Dr. Kiran C. Patel College of Allopathic Medicine, Nova lirium symptoms are related to the anticholinergic burden.
Southeastern University, Fort Lauderdale, FL. Geriatr Gerontol Int 2016; 16:424–431
2 Divison of Geriatric Medicine, Department of Medicine, 9. Farrall AJ, Wardlaw JM: Blood-brain barrier: Ageing and mi-
University of North Carolina, Chapel Hill, NC. crovascular disease–systematic review and meta-analysis.
3 Department of Family Medicine, University of North Carolina, Neurobiol Aging 2009; 30:337–352
Chapel Hill, NC. 10. Inotsume N, Nishimura M, Fujiyama S, et al: Pharmacokinetics
4 Division of Pulmonary and Critical Care Medicine, of famotidine in elderly patients with and without renal insuf-
Department of Medicine, University of North Carolina, ficiency and in healthy young volunteers. Eur J Clin Pharmacol
Chapel Hill, NC. 1989; 36:517–520
Supplemental digital content is available for this article. Direct 11. Kim KY, McCartney JR, Kaye W, et al: The effect of ci-
URL citations appear in the printed text and are provided in the metidine and ranitidine on cognitive function in postoper-
HTML and PDF versions of this article on the journal’s website ative cardiac surgical patients. Int J Psychiatry Med 1996;
(http://journals.lww.com/ccejournal). 26:295–307
Supported, in part, by the University of North Carolina (UNC) 12. Castro REV, Sousa CDC, de Magalhães-Barbosa MC, et al:
Chapel Hill Medical Student Training in Aging Research Program Ranitidine-induced delirium in a 7-year-old girl: A case report.
through Grant Award Number National Institutes of Health (NIH) Pediatrics 2019; 143:e20182428
2-T35-AG038047-09. The Informatics for Integrating Biology and 13. Catalano G, Catalano MC, Alberts VA: Famotidine-associated
the Bedside instance at the UNC is supported by the National delirium. A series of six cases. Psychosomatics 1996;
Center for Advancing Translational Sciences, NIH, through Grant 37:349–355
Award Number UL1TR002489. 14. Yuan RY, Kao CR, Sheu JJ, et al: Delirium following a switch
The authors have disclosed that they do not have any potential from cimetidine to famotidine. Ann Pharmacother 2001;
conflicts of interest. 35:1045–1048
8 www.ccejournal.org August 2021 • Volume 3 • Number 8
Observational Study
15. Lochhead P, Hagan K, Joshi AD, et al: Association between 4. UNC Medical Center Guideline: Stress Ulcer Prophylaxis. 2021
2
proton pump inhibitor use and cognitive function in women. 25. Sasannejad C, Ely EW, Lahiri S: Long-term cognitive impair-
Gastroenterology 2017; 153:971–979.e4 ment after acute respiratory distress syndrome: A review of
16. Bebarta VS, King JA, McDonough M: Proton pump inhibitor- clinical impact and pathophysiological mechanisms. Crit Care
induced rhabdomyolysis and hyponatremic delirium. Am J 2019; 23:352
Emerg Med 2008; 26:519.e1–e2 26. Wedemeyer RS, Blume H: Pharmacokinetic drug interaction
17. van Gool WA, van de Beek D, Eikelenboom P: Systemic infec- profiles of proton pump inhibitors: An update. Drug Saf 2014;
tion and delirium: When cytokines and acetylcholine collide. 37:201–211
Lancet 2010; 375:773–775
27. Barkun AN, Adam V, Martel M, et al: Cost-effectiveness anal-
18. Yamasaki M, Fukuda Y, Tanimoto A, et al: Reduction in the ysis: Stress ulcer bleeding prophylaxis with proton pump
rate of postoperative delirium by switching from famotidine to inhibitors, H2 receptor antagonists. Value Health 2013;
omeprazole in Japanese hepatectomized recipients. J Pharm 16:14–22
Heal Care Sci 2019; 1:1–8
28. MacLaren R, Reynolds PM, Allen RR: Histamine-2 receptor
19. Fujii S, Tanimukai H, Kashiwagi Y: Comparison and analysis
antagonists vs proton pump inhibitors on gastrointestinal tract
of delirium induced by histamine h(2) receptor antagonists
hemorrhage and infectious complications in the intensive care
and proton pump inhibitors in cancer patients. Case Rep Oncol
unit. JAMA Intern Med 2014; 174:564–574
2012; 5:409–412
20. Kim DH, Leeb J, Kim CA, et al: Evaluation of algorithms to 29. Durand C, Willett KC, Desilets AR: Proton pump inhibitor use
identify delirium in administrative claims and drug utilization in hospitalized patients: Is overutilization becoming a problem?
database. Pharmacoepidemiol Drug Saf 2018; 26:945–953 Clin Med Insights Gastroenterol 2012; 5:65–76
21. Cavallazzi R, Saad M, Marik PE: Delirium in the ICU: An over- 30. Alhazzani W, Alenezi F, Jaeschke RZ, et al: Proton pump inhibi-
view. Ann Intensive Care 2012; 2:49 tors versus histamine 2 receptor antagonists for stress ulcer
22. Ely EW, Shintani A, Truman B, et al: Delirium as a predictor of prophylaxis in critically ill patients: A systematic review and
mortality in mechanically ventilated patients in the intensive meta-analysis. Crit Care Med 2013; 41:693–705
care unit. JAMA 2004; 291:1753–1762 31. McRorie JW, Kirby JA, Miner PB: Histamine2-receptor antag-
23. UNC Medical Center Guideline: Proton Pump Inhibitors for onists: Rapid development of tachyphylaxis with repeat dosing.
Adults. 2021 World J Gastrointest Pharmacol Ther 2014; 5:57–62
Critical Care Explorations www.ccejournal.org 9
You might also like
- Kdoqi PDFDocument164 pagesKdoqi PDFcindyrelyNo ratings yet
- 1 Hurth 2020Document13 pages1 Hurth 2020ironmaidenmaciasNo ratings yet
- PharmacologicalDocument7 pagesPharmacologicaldharahasitha03No ratings yet
- Drug StudyDocument4 pagesDrug Studystrawberrykate26No ratings yet
- Can Pyridoxine Successfully Reduce Behavioral Side.15Document4 pagesCan Pyridoxine Successfully Reduce Behavioral Side.15ilonaskorinNo ratings yet
- Ds CiticolineDocument3 pagesDs Citicolinepearl japsonNo ratings yet
- Beta Block 2Document24 pagesBeta Block 2Evelyn GrandaNo ratings yet
- MagnascoDocument8 pagesMagnascoMeliana SulistioNo ratings yet
- Phase I Study of Lovastatin, An Inhibitor of The Mevalonate Pathway, in Patients With CancerDocument10 pagesPhase I Study of Lovastatin, An Inhibitor of The Mevalonate Pathway, in Patients With CancerdianNo ratings yet
- Risperidone in The Treatment of Acute Mania - Double-Blind, Placebo-Controlled StudyDocument8 pagesRisperidone in The Treatment of Acute Mania - Double-Blind, Placebo-Controlled StudyKKN 11 UMY 2017No ratings yet
- NCP 2Document5 pagesNCP 2Ezequiel RosalesNo ratings yet
- Side-Effects Associated With Ketamine Use in DepressionDocument14 pagesSide-Effects Associated With Ketamine Use in Depression賀立安No ratings yet
- Quetiapine Doe Primary Insomnia Consider The RiskDocument9 pagesQuetiapine Doe Primary Insomnia Consider The RiskFlorence Matthew T BesaresNo ratings yet
- Drug-Induced Serotonin Syndrome - A ReviewDocument10 pagesDrug-Induced Serotonin Syndrome - A ReviewAshrafNo ratings yet
- 2022 Society of Critical Care Medicine Clinical.15Document37 pages2022 Society of Critical Care Medicine Clinical.15diegorojasNo ratings yet
- Oral Ketamine in Treatment-Resistant Depression: Rief EportDocument4 pagesOral Ketamine in Treatment-Resistant Depression: Rief EportDeepaNo ratings yet
- 0905 (1) When Cardiovascular Medications Become ToxinsDocument20 pages0905 (1) When Cardiovascular Medications Become ToxinsIsaura MendezNo ratings yet
- Efecto de La Vit B2, Vit C, Vit D, Vit E y A. Fólico en HipertensiónDocument10 pagesEfecto de La Vit B2, Vit C, Vit D, Vit E y A. Fólico en Hipertensiónhugoemr7277487No ratings yet
- Nebivolol Drug StudyDocument4 pagesNebivolol Drug Studyalteahmichaella.mintuNo ratings yet
- Panduan Nutrisi COVID 19Document4 pagesPanduan Nutrisi COVID 19Yosefin RatnaningtyasNo ratings yet
- Jurnal 2Document11 pagesJurnal 2citra kurnia pratiwiNo ratings yet
- Breast Cancer Immunology and Immunotherapy: Targeting The Programmed Cell Death Protein-1/programmed Cell Death Protein Ligand-1Document10 pagesBreast Cancer Immunology and Immunotherapy: Targeting The Programmed Cell Death Protein-1/programmed Cell Death Protein Ligand-1Inés Olivares IturraNo ratings yet
- Alzheimer Dementia Starting Stopping Drug Therapycleveland Clinic Journal of MedicineDocument6 pagesAlzheimer Dementia Starting Stopping Drug Therapycleveland Clinic Journal of MedicineLoida CamargoNo ratings yet
- Avent Et Al-2011-Internal Medicine JournalDocument9 pagesAvent Et Al-2011-Internal Medicine JournalAgil Wahyu WicaksonoNo ratings yet
- Improving Decannulation Rates in Trauma Patients: Critical Care Medicine January 2019Document5 pagesImproving Decannulation Rates in Trauma Patients: Critical Care Medicine January 2019Luis De jesus SolanoNo ratings yet
- Gastroenterología y Hepatología: Scientific LettersDocument2 pagesGastroenterología y Hepatología: Scientific LettersXimenaNo ratings yet
- Table of Contents - 2022 - Acta Pharmaceutica Sinica BDocument11 pagesTable of Contents - 2022 - Acta Pharmaceutica Sinica BMohammed Shuaib AhmedNo ratings yet
- Jur Nal LLLLLDocument9 pagesJur Nal LLLLLsabrina nurNo ratings yet
- SSM Winter 2007 Biomed DiabetesDocument2 pagesSSM Winter 2007 Biomed DiabetesstanscimagNo ratings yet
- Engoren 2020Document7 pagesEngoren 2020DEYVI JOHE ANGULO FLORIANNo ratings yet
- Hypertensive NCPDocument3 pagesHypertensive NCPjgaitera23223No ratings yet
- New Frontiers in Obesity Treatment - GLP-1 and Nascent Nutrient-Stimulated Hormone-Based TherapeuticsDocument18 pagesNew Frontiers in Obesity Treatment - GLP-1 and Nascent Nutrient-Stimulated Hormone-Based TherapeuticssacarrilNo ratings yet
- PediaDocument8 pagesPediaChloe CabingatanNo ratings yet
- Effectiveness and Adverse Drug Reactions of Levetiracetam and Midazolam in Refractory Neonatal Seizure: A Cross Sectional Comparative StudyDocument6 pagesEffectiveness and Adverse Drug Reactions of Levetiracetam and Midazolam in Refractory Neonatal Seizure: A Cross Sectional Comparative StudySultan Rahmat SeptianNo ratings yet
- Can We Improve Physical Health Monitoring For Patients Taking Antipsychotics On A Mental Health Inpatient Unit ?Document7 pagesCan We Improve Physical Health Monitoring For Patients Taking Antipsychotics On A Mental Health Inpatient Unit ?risang akrima fikriNo ratings yet
- Fphar 12 735841Document23 pagesFphar 12 735841ReywersonNo ratings yet
- Everett 1995Document7 pagesEverett 1995yayan kurniawanNo ratings yet
- Green 2018Document6 pagesGreen 2018reza arlasNo ratings yet
- Drug Study of Case Presentation 2Document6 pagesDrug Study of Case Presentation 2banana cueNo ratings yet
- Reducing PlainDocument9 pagesReducing PlainAtikah AbayNo ratings yet
- Alzheimer Dementia: Starting, Stopping Drug Therapy: ReviewDocument6 pagesAlzheimer Dementia: Starting, Stopping Drug Therapy: ReviewAnonymous ZUaUz1wwNo ratings yet
- Novilyn C. Pataray BSN - Ii Aids: St. Paul College of Ilocos SurDocument1 pageNovilyn C. Pataray BSN - Ii Aids: St. Paul College of Ilocos SurCharina AubreyNo ratings yet
- Manchia Et Al. - 2020 - Challenges and Future Prospects of Precision MedicDocument14 pagesManchia Et Al. - 2020 - Challenges and Future Prospects of Precision MedicRodrigo SosaNo ratings yet
- Natural Medicines For Psychotic DisordersDocument21 pagesNatural Medicines For Psychotic DisordersNath miaounNo ratings yet
- Effectiveness of Albumin in Wound HealingDocument5 pagesEffectiveness of Albumin in Wound HealingArum IndrianiNo ratings yet
- Jim 2020 001747Document6 pagesJim 2020 001747foaad foaadNo ratings yet
- Kheirabadi - Comparison of Rapid Antidepressant and Antisuicidal Effects of Im Ketamine, Oral Ketamine, EctDocument6 pagesKheirabadi - Comparison of Rapid Antidepressant and Antisuicidal Effects of Im Ketamine, Oral Ketamine, EctjasonNo ratings yet
- Assignment 1 - PHARMACOLOGYDocument4 pagesAssignment 1 - PHARMACOLOGYJewel SebastianNo ratings yet
- Hyperferritinemia in Severe Dengue Infection .13Document8 pagesHyperferritinemia in Severe Dengue Infection .13rsthsn6z8xNo ratings yet
- PSH-WARD Drugstudy MigallenDocument14 pagesPSH-WARD Drugstudy MigallenIvan A. EleginoNo ratings yet
- Case Report and Literature Review of Auto-Brewery Syndrome: Probably An Underdiagnosed Medical ConditionDocument5 pagesCase Report and Literature Review of Auto-Brewery Syndrome: Probably An Underdiagnosed Medical ConditionElmer Hernández CáceresNo ratings yet
- Beta-Carotene, Carotenoids, and Disease Prevention in HumansDocument12 pagesBeta-Carotene, Carotenoids, and Disease Prevention in HumansLoredana Veronica ZalischiNo ratings yet
- Promise 2Document14 pagesPromise 2JUAN MANUEL CERON ALVARADONo ratings yet
- Engebretsen2011, INSULINA EN B BLOQDocument7 pagesEngebretsen2011, INSULINA EN B BLOQFabiola Delia Rosas AlarcónNo ratings yet
- Simvastatin and Vitamin D For Migraine Prevention: A Randomized, Controlled TrialDocument12 pagesSimvastatin and Vitamin D For Migraine Prevention: A Randomized, Controlled TrialshehabNo ratings yet
- GROUP1 Drug Therapeutic RecordDocument6 pagesGROUP1 Drug Therapeutic RecordYori Nicole Martine CuyosNo ratings yet
- Severe Acute Kidney Injury Is Associated With Increased Risk of Death and New Morbidity After Pediatric Septic ShockDocument10 pagesSevere Acute Kidney Injury Is Associated With Increased Risk of Death and New Morbidity After Pediatric Septic ShockdoctoramanphalswalNo ratings yet
- Drug Therapeutic Record TemplateDocument1 pageDrug Therapeutic Record TemplateAubrey Justine GaleonNo ratings yet
- Infographic EndonutritionDocument1 pageInfographic EndonutritionLuis Felipe TorresNo ratings yet
- Efectos 2rios EstatinasDocument2 pagesEfectos 2rios EstatinasFranklin Flórez VidesNo ratings yet
- Biotin and Other Interferences in Immunoassays: A Concise GuideFrom EverandBiotin and Other Interferences in Immunoassays: A Concise GuideNo ratings yet
- 2021 - TorresDocument28 pages2021 - TorresCarlosNo ratings yet
- Seminar: Nuala J Meyer, Luciano Gattinoni, Carolyn S CalfeeDocument16 pagesSeminar: Nuala J Meyer, Luciano Gattinoni, Carolyn S CalfeeDiana AngelesNo ratings yet
- Cir 0000000000000628Document101 pagesCir 0000000000000628Diana AngelesNo ratings yet
- E-Cigarette or Vaping Product Use - Associated Lung Injury (EVALI) Masquerading As COVID-19Document4 pagesE-Cigarette or Vaping Product Use - Associated Lung Injury (EVALI) Masquerading As COVID-19Diana AngelesNo ratings yet
- Primer: Acute Kidney InjuryDocument17 pagesPrimer: Acute Kidney InjuryDiana AngelesNo ratings yet
- Hypertensionin PregnancyDocument100 pagesHypertensionin Pregnancyricky hutagalungNo ratings yet
- Activacion Inmune SepsisDocument7 pagesActivacion Inmune SepsisDiana AngelesNo ratings yet
- GINA Asthma 2006Document109 pagesGINA Asthma 2006api-3847280No ratings yet
- The Nomenclature, Definition and Distinction of Types of ShockDocument14 pagesThe Nomenclature, Definition and Distinction of Types of ShockDiana AngelesNo ratings yet
- 2579-Article Text-8486-1-10-20180302Document4 pages2579-Article Text-8486-1-10-20180302Diana AngelesNo ratings yet
- Activacion Inmune SepsisDocument7 pagesActivacion Inmune SepsisDiana AngelesNo ratings yet
- Immune Activation in Sepsis 2018 Critical Care ClinicsDocument14 pagesImmune Activation in Sepsis 2018 Critical Care ClinicsgiseladlrNo ratings yet
- Peanut AllergyDocument4 pagesPeanut AllergyLNICCOLAIONo ratings yet
- PM 50 Service ManualDocument60 pagesPM 50 Service ManualLeoni AnjosNo ratings yet
- Porter's 5-Force Analysis of ToyotaDocument9 pagesPorter's 5-Force Analysis of ToyotaBiju MathewsNo ratings yet
- 5045.CHUYÊN ĐỀDocument8 pages5045.CHUYÊN ĐỀThanh HuyềnNo ratings yet
- Nat Steel BREGENEPD000379Document16 pagesNat Steel BREGENEPD000379Batu GajahNo ratings yet
- Stratum CorneumDocument4 pagesStratum CorneumMuh Firdaus Ar-RappanyNo ratings yet
- How To Change Front Suspension Strut On Citroen Xsara Coupe n0 Replacement GuideDocument25 pagesHow To Change Front Suspension Strut On Citroen Xsara Coupe n0 Replacement Guidematej89No ratings yet
- Pyromet Examples Self StudyDocument2 pagesPyromet Examples Self StudyTessa BeeNo ratings yet
- Chemical & Ionic Equilibrium Question PaperDocument7 pagesChemical & Ionic Equilibrium Question PapermisostudyNo ratings yet
- Vest3000mkii TurntableDocument16 pagesVest3000mkii TurntableElkin BabiloniaNo ratings yet
- Visi RuleDocument6 pagesVisi RuleBruce HerreraNo ratings yet
- SPFL Monitoring ToolDocument3 pagesSPFL Monitoring ToolAnalyn EnriquezNo ratings yet
- FluteDocument13 pagesFlutefisher3910% (1)
- Managing Errors and ExceptionDocument12 pagesManaging Errors and ExceptionShanmuka Sreenivas100% (1)
- OBOE GougerDocument2 pagesOBOE GougerCarlos GaldámezNo ratings yet
- Localization On ECG: Myocardial Ischemia / Injury / InfarctionDocument56 pagesLocalization On ECG: Myocardial Ischemia / Injury / InfarctionduratulfahliaNo ratings yet
- SY22-23+Annual+Report FinalDocument47 pagesSY22-23+Annual+Report FinalNorus LizaNo ratings yet
- NCP - Impaired Urinary EliminationDocument3 pagesNCP - Impaired Urinary EliminationFretzgine Lou ManuelNo ratings yet
- Tax Havens IMF PDFDocument59 pagesTax Havens IMF PDFClassic PhyXNo ratings yet
- Our Story Needs No Filter by Nagarkar SudeepDocument153 pagesOur Story Needs No Filter by Nagarkar SudeepKavya SunderNo ratings yet
- The One With The ThumbDocument4 pagesThe One With The Thumbnoelia20_09No ratings yet
- Capgemini - 2012-06-13 - 2012 Analyst Day - 3 - Michelin - A Better Way ForwardDocument12 pagesCapgemini - 2012-06-13 - 2012 Analyst Day - 3 - Michelin - A Better Way ForwardAvanish VermaNo ratings yet
- PCM Cables: What Is PCM Cable? Why PCM Cables? Application?Document14 pagesPCM Cables: What Is PCM Cable? Why PCM Cables? Application?sidd_mgrNo ratings yet
- Collecting, Analyzing, & Feeding Back DiagnosticDocument12 pagesCollecting, Analyzing, & Feeding Back DiagnosticCaroline Mariae TuquibNo ratings yet
- Journal of Molecular LiquidsDocument11 pagesJournal of Molecular LiquidsDennys MacasNo ratings yet
- Population Second TermDocument2 pagesPopulation Second Termlubna imranNo ratings yet
- HKUST 4Y Curriculum Diagram CIVLDocument4 pagesHKUST 4Y Curriculum Diagram CIVLfrevNo ratings yet
- Institutions and StrategyDocument28 pagesInstitutions and StrategyFatin Fatin Atiqah100% (1)
- Ubicomp PracticalDocument27 pagesUbicomp Practicalvikrant sharmaNo ratings yet
- BAMDocument111 pagesBAMnageswara_mutyalaNo ratings yet