Professional Documents
Culture Documents
Corticosteroids For Pediatric Septic Shock Patiens
Uploaded by
Reka Vikaria AnggreliaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Corticosteroids For Pediatric Septic Shock Patiens
Uploaded by
Reka Vikaria AnggreliaCopyright:
Available Formats
Paediatrica Indonesiana
p-ISSN 0030-9311; e-ISSN 2338-476X; Vol.59, No.2(2019). p. 67-71; doi: http://dx.doi.org/10.14238/pi59.2.2019.67-71
Original Article
Corticosteroids for pediatric septic shock patients
Irene Yuniar, Vembricha Nindya Manusita, Sonya Leonardy Low
S
Abstract epsis is defined as a life-threatening condition
Background Septic shock remains a major cause of mortality of organ dysfunction caused by a dysregulated
and admission to the pediatric intensive care unit (PICU) in host response to infection.1 Sepsis is still
children. Management includes adequate fluid resuscitation,
followed by catecholamine infusion, if needed. Corticoster- one of the major causes of morbidity, and
oid therapy is advised for catecholamine-refractory shock, the leading cause of pediatric intensive care unit
although this practice is controversial, as it was not beneficial (PICU) admissions.2 The World Health Organization
in other studies. (WHO) reported 80% mortality of children below
Objective To assess corticosteroid use in pediatric septic
shock patients in Cipto Mangunkusumo Hospital. 4 years of age with sepsis.3 Based on medical record
Methods This cross-sectional study included all patients aged data in Cipto Mangunkusumo Hospital in 2009, the
1 month-18 years with a diagnosis of septic shock during the incidence of sepsis in children admitted to the PICU
study period of January 2014 to July 2018 admitted in PICU was 19.3% and the mortality rate was 10%. Also,
Dr. Cipto Mangunkuskumo Hospital, Jakarta. Data obtained
from medical records were, age, sex, immunology status, port 5-30% of pediatric sepsis cases can progress to septic
d’entrée of sepsis, inotropic and vasopressor usage, mechani- shock.4 Rusmawatiningtyas et al.5 reported an 88.2%
cal ventilation, corticosteroid type, hospital length of stay mortality rate in children with septic shock admitted
(LoS), and mortality outcome. to the PICU.
Results Of 217 children with septic shock, 12 patients
(5.5%) received corticosteroid therapy. The most common The American College of Critical Care Medicine
corticosteroid given was hydrocortisone (80%), with a 2 mg/ (ACCM) developed an algorithm to target an initial
kg BW loading dose, followed by a continuous infusion dose resuscitation fluid of 20 mL/kg BW of crystalloid or
of 2-50 mg/kg BW/day. Almost all patients (11/12) received colloid which can be repeated to 60 mL/kg BW, until
corticosteroid therapy until they died. Median duration of
corticosteroid use was 2 (range 1-7) days, median number perfusion improves or unless rales or hepatomegaly
of inotropes and vasopressors used was 3 (range 2-4) agents,
median LoS was 3 (range 1-9) days, and mortality rate was
100%.
Conclusion A small proportion of pediatric septic shock
patients received corticosteroid therapy. Their mortality rate From the Department of Child Health, Universitas Indonesia Medical
was 100%. Further clinical study is needed to evaluate the School/Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia.
benefit of corticosteroid therapy in pediatric septic shock
patients. [Paediatr Indones. 2019;59:67-71; doi: http://dx.doi. Corresponding author: Irene Yuniar, Ph.D. Department of Child Health,
org/10.14238/pi59.2.2019.67-71 ]. Universitas Indonesia Medical School/Dr. Cipto Mangunkusumo Hospital.
Jl. Pangeran Diponegoro No. 71, Jakarta, Indonesia. Phone +62-21-
3907742; Fax. +62-21-3907743; Email: irene.tambunan@yahoo.co.id.
Keywords: corticosteroid; mortality; pediatric
septic shock; septic shock Submitted December 11, 2018. Accepted February 21, 2019.
Paediatr Indones, Vol. 59, No. 2, March 2019 • 67
Irene Yuniar et al.: Corticosteroids for pediatric septic shock patients
develop. For fluid refractory shock, vasopressors and were immunocompromised, of whom 2 patients had
inotropes must be given. If the shock does not resolve, systemic lupus erythematosus (SLE), 2 patients had
it may progress to catecholamine-resistant shock. poor nutritional status, 1 patient had lymphoma
This condition is related to adrenal insufficiency, and poor nutritional status, and 1 patient received
which requires corticosteroid administration such as post-liver transplantation immunosuppressant drugs.
hydrocortisone. The sources of sepsis were respiratory tract (6/12),
Several studies on intravenous hydrocortisone abdominal organs (5/12), and urogenital tract (1/12).
administration for catecholamine-resistant shock Patients’ characteristics are described in Table 1.
yielded varying results. Wong et al.8 suggested that
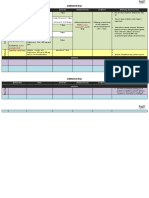
corticosteroid administration for catecholamine- Table 1. Characteristics of pediatric septic shock patients
resistant shock be reconsidered, due to side effects receiving corticosteroid therapy
including gastrointestinal bleeding, delayed wound Variables (N=12)
healing, hyperglycemia, and immunosuppression. In Median age (range), months 165 (11-533)
addition, Atkinson et al.9 reported that corticosteroid Sex, n
administration in children with refractory septic shock Male 8
Female 4
had no benefits.
In Cipto Mangunkusumo Hospital, corticosteroid Immunity status, n
Immunocompromised 6
administration for pediatric septic shock has not been Not immunocompromised 6
well studied. As such, we aimed to assess corticosteroid Port d’ entrée sepsis, n
therapy for pediatric septic shock to see the prognosis Respiratory tract 6
or outcomes as a treatment consideration for future Abdominal organ 5
Urogenital tract 1
pediatric shock patients.
The most common type of corticosteroid given
Methods was hydrocortisone (83%). One patient received
dexamethasone as a hydrocortisone replacement.
This cross-sectional study was done with patients’ One remaining patient received hydrocortisone,
medical records in Cipto Mangunkusumo Hospital. followed by methylprednisolone as a hydrocortisone
Subjects were children aged 1 month to 18 years replacement. The hydrocortisone loading dose was
diagnosed with septic shock in the emergency room/ 2 mg/kg (equal to 50 mg/m2), followed by a continuous
PICU from January 2014 to July 2018. Patients with infusion dose of 2-50 mg/kg/day (equal to 50-1,250 mg/
incomplete medical records were excluded from the m2/day). In our study, the maximum hydrocortisone
study. Data obtained from medical records were, age, dose recorded was 48 mg/kg/day (equal to 1,125 mg/
sex, immunology status, port d’entrée of sepsis, inotropic m2/day). The dexamethasone dose used was 1.8 mg/
and vasopressor usage, and mechanical ventilation. m2/24 hours. One patient received hydrocortisone at
The type, dose, and duration of corticosteroid therapy a dose of 2 mg/kg/day (equal to 50 mg/m2/day) that
were collected for all subjects. Outcomes data were was increased gradually to 4 mg/kg/day (100 mg/m2/
hospital LoS and mortality. day) in one day, before getting methylprednisolone at
a dose of 0.4 mg/kg/day (equal to 10 mg/m2/24 hours)
that was increased gradually to 0.8 mg/kg/day (equal
Results to 20 mg/m2/day).
Corticosteroid doses were adjusted during
From January 2014 to July 2018, 217 children were administration. Most patients (58.3%) experienced that
diagnosed with septic shock at Cipto Mangunkusumo the corticosteroid dose was gradually increased until
Hospital, of whom 132 (60.8%) were male. Twelve they died. However, one patient (8.3%) experienced
patients received corticosteroid therapy for septic tapering down to cessation of hydrocortisone during
shock, 8 (67%) of whom were male. Subjects’ median 7 days of administration. Almost all patients (92%)
age was 165 (range 11-553) months. Six patients were still receiving corticosteroid therapy when
68 • Paediatr Indones, Vol. 59, No. 2, March 2019
Irene Yuniar et al.: Corticosteroids for pediatric septic shock patients
they died. Table 2 shows that the median duration et al.12 reported lower numbers of vasopressor and
of corticosteroid use was 2 (1-7) days. The median inotropes used, [median 2 (range 1-2)]. In their study,
number of inotropes and vasopressors used was 3 corticosteroids were given to patients with continuous
(2-4). The median LoS of patients with septic shock need for catecholamine infusion for 6 or more hours
receiving corticosteroid therapy was 3 (1-9) days and following initial fluid resuscitation of ≥ 60 mL/kg
the mortality rate was 100%. of crystalloid and/or colloid solutions. The cut-off
for starting the corticosteroid therapy was not the
Table 2. Outcomes of pediatric septic shock patients receiving amount of catecholamine used, but the duration of
corticosteroid therapy catecholamine infusion. Nichols et al.12 also showed
Outcomes (N=12) the catecholamine included dopamine > 5 μg/kg/min,
Median duration of corticosteroid use (range), 2 (1-7) vasopressin, and any dose of dobutamine, epinephrine,
days
norepinephrine, phenylephrine, or milrinone.
Median number of inotropic and vasopressor agents 3 (2-4) We noted that corticosteroid therapy was given
used (range)
without cortisol level examinations, in accordance
Median LoS (range), days 3 (1-9)
with the Surviving Sepsis Campaign guidelines
Mechanical ventilation, n 12
which state that in catecholamine-resistant shock,
Mortality, n 12
hydrocortisone administration should be given
immediately without cortisol level examination.
Discussion Nichols et al.12 also showed the same statement and in
contrast, Casartelli et al.14 concluded that the cortisol
The proportion of pediatric septic shock patients given assay should be used in deciding whether or not to
corticosteroids was only 12 of 217 patients (5.5%) in give corticosteroids in septic shock.
the 4-year period at Cipto Mangunkusumo Hospital. The most commonly used corticosteroid in
Corticosteroid therapy was given when shock had our study was hydrocortisone (10/12). Similarly, a
not resolved after administering a minimum two previous study reported that 78% of subjects were
types of vasopressors and inotropes. In contrast, prescribed hydrocortisone, 16% methylprednisolone,
Chrysostomos et al.10 noted a larger proportion and 6% dexamethasone. 9 However, another
of septic shock patients receiving corticosteroids previous study reported that 53% of subjects were
because the corticosteroid administration did not prescribed hydrocortisone, 29% dexamethasone, 14%
depend on the number, but on the duration, of methylprednisolone, and 4% prednisolone.15
inotropes and vasopressors used. They found that Gibbison et al.16 also mostly used hydrocortisone
early initiation of corticosteroid administration, after as corticosteroid of choice to treat catecholamine-
9 hours vasopressor and inotrope administration, resistant septic shock, since the advantages of
resulted in better prognoses compared to late initiation hydrocortisone are increased capillary permeability and
of corticosteroid administration in patients with cardiovascular activity. Furthermore, hydrocortisone
catecholamine-resistant septic shock.10 has the lowest risk of side effects such as hyperglycemia,
We found high usage of inotropic and vasopressor severe infection, and gastrointestinal bleeding
agents prior to corticosteroid therapy in our subjects, compared to other corticosteroids. Hydrocortisone
with median of 3 (range 2-4) drugs. Although administration may affect cortisol assay results
corticosteroid therapy was usually given to patients in catecholamine-resistant septic shock, while
after a combination of a minimum of two inotropic dexamethasone administration does not.13
and vasopressor agents with maximum dose did not We noted hydrocortisone loading doses of 2mg/
overcome shock, there was no standard protocol kg, followed by 2-50 mg/kg/d infusion dose. The initial
among physicians for starting corticosteroid therapy loading dose was similar to that reported by Menon
in such cases. In comparison, Menon et al.11 reported et al.,11 who used a hydrocortisone dose of 2 mg/kg.
that corticosteroid therapy was given to patients who Their hydrocortisone infusion dose of 1 mg/kg was
had a minimum of two vasoactive infusions and had given every 6 hours and weaned to every 8 hours
received 50 mL/kg of resuscitation fluids. Nichols until all vasoactive infusions had been discontinued
Paediatr Indones, Vol. 59, No. 2, March 2019 • 69
Irene Yuniar et al.: Corticosteroids for pediatric septic shock patients
for 12 hours. Nichols et al.12 reported an initial groups. Furthermore, Nichols et al.12 stated that
hydrocortisone dose of ≥ 50 mg/m2 (or ≥ 1mg/kg) stress dose hydrocortisone therapy in children with
followed by a dose ≥ 50mg/m2/d (or ≥ 1mg/kg/d). catecholamine-dependent septic shock was associated
The median duration of corticosteroid usage with worst outcomes. In addition, 2 previous studies
in our subjects was 2 (range 1-7) days, with 11/12 reported that adjunctive corticosteroid therapy
patients still receiving corticosteroids when they died. in severe pediatric sepsis showed no definitive
The maximum duration was similar to the Menon et improvement.9,15 Also, a pediatric meta- analysis by
al. study,11 in which corticosteroids were given for a Menon et al.17 showed no benefit of corticosteroids
maximum of 7 days to prevent adrenal suppression. for treating shock.
However, Nichols et al.12 reported a median of 4 Despite the lack of convincing evidence, a
(range 2-4) days corticosteroid therapy in the group Canadian survey revealed that almost all pediatric
with random cortisol level (rSTC) < 18 μg/dL and 4 intensivists (91.4%) would administer corticosteroids
(range 2-5) days in the group with rSTC ≥ 18 μg/dL. to patients in persistent shock who had received
Atkinson et al.9 also showed a higher median duration 60 mL/kg of fluid and were on two or more vasoactive
of corticosteroid use of 5 (range 3-7) days. medications. 18 Possible rationales for the use of
In our study, the mortality rate was high (100%), corticosteroids in sepsis are beneficial pharmacologic
with a median LOS of 3 (range 1-9) days. The high effect on the cardiovascular system and anti-
mortality rate may have been caused by the extreme inflammatory properties. Nonetheless, high dose
severity of illness among subjects, as indicated by the corticosteroid administration in septic shock has
high use of vasopressor and inotropic agents [median been associated with higher infection rates, such
3 (range 2-4) types] and the high use of mechanical as disseminated candidiasis and hospital- acquired
ventilation in 100% of subjects. Menon et al.11 noted pneumonia.19 Other potential side effects include
a 2% mortality in patients receiving corticosteroid hyperglycemia, bleeding, critical illness associated
therapy, with PICU median LoS of 8.3 (range 3.7-15.0) neuropathy/myopathy, and hypernatremia. 15,19
days. The median PELOD score of their corticosteroid Corticosteroid use was also associated with suppression
group was 6 (range 4-9), with 65.2% mechanical of genes corresponding to adaptive immunity.8
ventilation use. According to Dewi Metta et al.20, In conclusion, we find that a small proportion of
PELOD scores at 20 increasing mortality to 50%. pediatric septic shock patients received corticosteroid
Nichols et al.12 showed a 24% mortality rate among therapy, mostly hydrocortisone. The mortality rate
septic shock patients in the stress dose hydrocortisone of patients who received corticosteroids is 100% and
therapy group, with median LoS of 10 (range their LoS is short. Corticosteroids do not seem to have
5-20) days. The median Pediatric Risk of Mortality beneficial results in our sepsis patient population.
(PRISM) III score at 12 hours was 16 (range 10-12)
and 88% of subjects were mechanically ventilated.
Vineet Popli et al.21 showed Pediatric Risk of Mortality Conflict of Interest
(PRISM) III had a biphasic effect on the length
of stay (LOS). Their study showed length of stay None declared .
increased with increasing PRISM III score up to the
score of 14; while score of 19, length of stay decreased
gradually because an increasing severity of illness as Funding Acknowledgement
the mortality reaches almost 100%. The author received no specific grant from any funding agency
Some guidelines recommend the use of in the public, commercial, or not-for-profit sectors.
corticosteroids in catecholamine-resistant shock,
however, we noted no benefit to such therapy, as 100%
of the patients who received corticosteroids died. References
Menon et al.11 stated that there were no statistically
significant differences in outcomes or adverse 1. Latief A, Chairulfatah A, Alam A, Pudjiadi A, Malisie RF,
events between the hydrocortisone and placebo Hadinegoro SR. Pedoman nasional pelayanan kedokteran
70 • Paediatr Indones, Vol. 59, No. 2, March 2019
Irene Yuniar et al.: Corticosteroids for pediatric septic shock patients
Ikatan Dokter Anak Indonesia: diagnosis dan tatalaksana 12. Nichols B, Kubis S, Hewlett J, Yehya N, Srinivisan V.
sepsis pada anak. Jakarta: Badan penerbit Ikatan Dokter Hydrocortisone therapy in catecholamine-resistant
Anak Indonesia; 2016. p.1-47. pediatric septic shock: a pragmatic analysis of clinician
2. Jaramillo-Bustamante JC, Marín-Agudelo A, Fernández- practice and association with outcomes. Pediatr Crit
Laverde M, Bareño-Silva J. Epidemiology of sepsis in Care Med. 2017;18:406-14. https://doi.org/10.1097/
pediatric intensive care units: first Colombian multicenter pcc.0000000000001237.
study. Pediatr Crit Care Med. 2012;13:501-8. https://doi. 13. Dellinger PR, Carlet JM, Masur H, Gerlach H, Calandra
org/10.1097/pcc.0b013e31823c980f. T, Cohen J, et al. Surviving Sepsis Campaign guidelines
3. Bryce J, Boschi-Pinto C, Shibuya K, Black RE, WHO Child for management of severe sepsis and septic shock. Crit
Health Epidemiology Reference Group. WHO estimates of Care Med. 2004;32:859-73. https://doi.org/10.1097/01.
the cause of death in children. Lancet. 2005;365:1147-52. ccm.0000117317.18092.e4.
https://doi.org/10.1016/s0140-6736(05)71877-8. 14. Casartelli CH, Garcia PC, Piva JP, Branco RG. Adrenal
4. Saraswati DD, Pudjiadi AH, Djer MM, Supriyatno B, Syarif insufficiency in children with septic shock. J Pediatr (Rio J).
DR, Kurniati N. Faktor risiko yang berperan pada mortalitas 2003;79:169-76. https://doi.org/10.2223/jped.1093.
sepsis. Sari Pediatri. 2014;15:281-8. https://doi.org/10.14238/ 15. Zimmerman JJ, Williams MD. Adjunctive corticosteroid
sp15.5.2014.281-8. therapy in pediatric severe sepsis: observations from the
5. Rusmawatiningtyas D, Nurnaningsih. Mortality rates in RESOLVE study. Pediatr Crit Care Med. 2011;12:2-8.
pediatric septic shock. Paediatrica Indonesiana. 2016;56: https://doi.org/10.1097/pcc.0b013e3181d903f6.
304-10. https://doi.org/10.14238/pi56.5.2016.304-10. 16. Gibbison B, Lopez-Lopez JA, Higgins JP, Miller T, Angelini
6. de Oliveira CF. Early goal-directed therapy in treatment of GD, Lightman SL, et al. Corticosteroids in septic shock: a
pediatric septic shock. Shock. 2010;34:44-7. https://doi. systematic review and network meta-analysis. Crit Care.
org/10.1097/shk.0b013e3181e7e6d5. 2017;21:78. https://doi.org/10.1186/s13054-017-1659-4.
7. Pizarro CF, Troster EJ, Damiani D, Carcillo JA. Absoolute and 17. Menon K, McNally D, Choong K, Sampson M. A systematic
relative adrenal insufficiency in children with septic shock. review and meta-analysis on the effect of steroids in pediatric
Crit Care Med. 2005;33:855-9. https://doi.org/10.1097/01. shock. Pediatr Crit Care Med. 2013;14:474-80.
https://doi.
ccm.0000159854.23324.84. org/10.1097/pcc.0b013e31828a8125.
8. Wong HR, Cvijanovich NZ, Allen GL, Thomas NJ, Freishtat 18. Menon K, McNally JD, Choong K, Ward RE, Lawson ML,
RJ, Anas N, et al. Corticosteroids are associated with Ramsay T, et al. A survey of stated physician practices
repression of adaptive immunity gene programs in pediatric and beliefs on the use of steroids in pediatric fluid
septic shock. Am J Respir Crit Care Med. 2014;189:940-6. and/or vasoactive infusion-dependent shock. Pediatr
https://doi.org/10.1164/rccm.201401-0171oc. Crit Care Med. 2013;14:462-6. https://doi.org/10.1097/
9. Atkinson SJ, Cvijanovich NZ, Thomas NJ, Allen GL, pcc.0b013e31828a7287.
Anas N, Bigham MT, et al. Corticosteroids and pediatric 19. Davis AL, Carcillo JA, Aneja RK, Deymann AJ, Lin JC,
septic shock outcomes: a risk stratified analysis. PLoS Nguyen TC, et al. American College of Critical Care
ONE. 2014;9:112702. https://doi.org/10.1371/journal. Medicine clinical practice parameters for hemodynamic
pone.0112702. support of pediatric and neonatal septic shock. Crit
10. Katsenos CS, Antonopoulou AN, Apostolidou EN, Care Med. 2017;45:1061-93. https://doi.org/10.1097/
Ioakeimidou A, Kalpakou GT, Papanikolaou MN, et al. ccm.0000000000002573.
Early administration of hydrocortisone replacement after 20. Metta D, Soebardja D, Hudaya D. The Use of Pediatric
the advent of septic shock: impact on survival and immune Logistic Organ Dysfunction (PELOD) scoring system to
response. Crit Care Med. 2014;42:1651-7. https://doi. determine the prognosis of patients in pediatric intensive
org/10.1097/ccm.0000000000000318. care units. Peadiatrica Indonesiana. 2006; 46: 1-6. https://
11. Menon K, McNally DM, O’Hearn K, Acharya A, Wong doi.org/10.14238/pi46.1.2006.1-6.
HR, Lawson M, et al. A randomized controlled trial of 21. Popli V, Kumar A. Validation of PRISM III ( Pediatric Risk of
corticosteroids in pediatric septic shock: a pilot feasibility Mortality) scoring system in predicting risk of mortality in a
study. Pediatr Cric Care Med. 2017;18:505-12. https://doi. pediatric intensive care unit. IOSR Journal. 2018;17: 81-7.
org/10.1097/pcc.0000000000001121.
Paediatr Indones, Vol. 59, No. 2, March 2019 • 71
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Update On Congenital Hypothyroidism: ReviewDocument7 pagesUpdate On Congenital Hypothyroidism: ReviewReka Vikaria AnggreliaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Current Antibiotic Use in The Treatment of EntericDocument26 pagesCurrent Antibiotic Use in The Treatment of EntericReka Vikaria AnggreliaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- 2015 Myopia A Growing Global Problem WithDocument1 page2015 Myopia A Growing Global Problem WithReka Vikaria AnggreliaNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Commissioned Article Computer Vision Syndrome: A Review: Jatinder Bali, Naveen Neeraj, Renu Thakur BaliDocument8 pagesCommissioned Article Computer Vision Syndrome: A Review: Jatinder Bali, Naveen Neeraj, Renu Thakur BaliReka Vikaria AnggreliaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Computer Vision Syndrome (CVS)Document9 pagesComputer Vision Syndrome (CVS)Reka Vikaria AnggreliaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Tumbling e ChartDocument21 pagesTumbling e ChartReka Vikaria AnggreliaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Energy Pen: MeridianDocument11 pagesEnergy Pen: Meridianjose luis lamadrid armasNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Program-SUFU 2020 Winter Meeting-2252020Document39 pagesProgram-SUFU 2020 Winter Meeting-2252020Christopher KinsellaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Ascorbic Acid-Vitamin C Brochure PDFDocument8 pagesAscorbic Acid-Vitamin C Brochure PDFl10n_ass50% (2)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Use of "Zingiber Officinale Roscoe L" Root in Various DiseasesDocument8 pagesUse of "Zingiber Officinale Roscoe L" Root in Various DiseasesCentral Asian StudiesNo ratings yet
- GastritisDocument3 pagesGastritisaliceNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Draw-Over Anaesthesia - DobsonDocument7 pagesDraw-Over Anaesthesia - DobsonHuynh Quoc SangNo ratings yet
- Handout and Questions of HysterosalpingDocument12 pagesHandout and Questions of Hysterosalpingahmad shaltout100% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Medical Students Career Choice GuidelineDocument16 pagesMedical Students Career Choice Guidelineአማረ ተመስገንNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- GFD Ambulance Service Business PlanDocument36 pagesGFD Ambulance Service Business Planmyfoxmemphis100% (8)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Stress and Adaptation: Jyoti 1 YearDocument29 pagesStress and Adaptation: Jyoti 1 YearNancy SinghNo ratings yet
- Documenting Pharmaceutical Care Patient Medical Records PDFDocument3 pagesDocumenting Pharmaceutical Care Patient Medical Records PDFPuspa NurrochmawatiNo ratings yet
- Central Bank Vs CSCDocument6 pagesCentral Bank Vs CSCRonn PagcoNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- National Accreditation Board For Hospitals and Healthcare ProvidersDocument104 pagesNational Accreditation Board For Hospitals and Healthcare ProviderssridhartrichyNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- HarveyDocument6 pagesHarveyapi-276953527No ratings yet
- Gambaran Pelaksanaan Kegiatan Program Pengelolaan Penyakit Kronis (Prolanis) Bpjs Kesehatan Di Puskesmas Siak Hulu IIIDocument10 pagesGambaran Pelaksanaan Kegiatan Program Pengelolaan Penyakit Kronis (Prolanis) Bpjs Kesehatan Di Puskesmas Siak Hulu IIIDiky WahyuNo ratings yet
- Fractures in ChildrenDocument26 pagesFractures in ChildrenRafli SoehadakNo ratings yet
- SLIDE DECK - Capacity Building For NGAs.Document40 pagesSLIDE DECK - Capacity Building For NGAs.hanniemaelimonNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Theory, Research and Practice (SPRING, 1970 ISSUE) Hypnotherapy: A Reappraisal Alfred A BarriosDocument9 pagesTheory, Research and Practice (SPRING, 1970 ISSUE) Hypnotherapy: A Reappraisal Alfred A BarriosMNo ratings yet
- Red AlertDocument4 pagesRed AlertrositajarauNo ratings yet
- Disabilities Act 1995Document4 pagesDisabilities Act 1995directdeoNo ratings yet
- Rajiv Gandhi University of Health Sciences, Karnataka, BangaloreDocument27 pagesRajiv Gandhi University of Health Sciences, Karnataka, BangaloreJyotiNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- DVT and PeDocument25 pagesDVT and PeOmar AbdillahiNo ratings yet
- Hipertensi KrisisDocument30 pagesHipertensi KrisisLuthfan HakimNo ratings yet
- Indications Dose Duration Administration Stability Warning & PrecautionsDocument2 pagesIndications Dose Duration Administration Stability Warning & PrecautionsFatma HasanNo ratings yet
- Peace Corps Report of Physical Examination - Guide - Att 19 Report of Physical ExaminationDocument6 pagesPeace Corps Report of Physical Examination - Guide - Att 19 Report of Physical ExaminationAccessible Journal Media: Peace Corps DocumentsNo ratings yet
- Chapter 006 Practice TestDocument14 pagesChapter 006 Practice TestnursingstudentdNo ratings yet
- Continuing Education Activity: HypospadiasDocument6 pagesContinuing Education Activity: HypospadiasMaulani Nurlatifah100% (1)
- Our Lady of Fatima University College of Medicine Clinical Clerkship Summary of Learning ExperiencesDocument3 pagesOur Lady of Fatima University College of Medicine Clinical Clerkship Summary of Learning ExperiencesrenzNo ratings yet
- Anatomy & Physiology - Chapter 19: BLOOD Book Questions and AnswersDocument6 pagesAnatomy & Physiology - Chapter 19: BLOOD Book Questions and AnswersVanessa CarmodyNo ratings yet
- Xavier BrochureDocument20 pagesXavier BrochureJohn PareraNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)