Professional Documents
Culture Documents
Immunogenicity of Single Vaccination With BNT162b2
Uploaded by
Christian GaraffaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Immunogenicity of Single Vaccination With BNT162b2
Uploaded by
Christian GaraffaCopyright:
Available Formats
Articles
Immunogenicity of single vaccination with BNT162b2 or
ChAdOx1 nCoV-19 at 5–6 weeks post vaccine in participants
aged 80 years or older: an exploratory analysis
Helen Parry, Rachel Bruton, Gokhan Tut, Myah Ali, Christine Stephens, David Greenwood, Sian Faustini, Sam Hughes, Aarnoud Huissoon,
Rory Meade, Kevin Brown, Gayatri Amirthalingam, Ashley Otter, Bassam Hallis, Alex Richter, Jianmin Zuo, Paul Moss
Summary
Background In several countries, extended interval COVID-19 vaccination regimens are now used to accelerate Lancet Healthy Longev 2021;
population coverage, but the relative immunogenicity of different vaccines in older people remains uncertain. In this 2: e554–60
study we aimed to assess the antibody and cellular responses of older people after a single dose of either the BNT162b2 Published Online
August 11, 2021
vaccine (tozinameran; Pfizer–BioNTech) or ChAdOx1 nCoV-19 vaccine (Oxford University–AstraZeneca).
https://doi.org/10.1016/
S2666-7568(21)00169-0
Methods Participants aged 80 years or older, who did not live in a residential or care home or require assisted living, See Comment page e529
and had received a single dose of either the BNT162b2 vaccine or ChAdOx1 nCoV-19 vaccine were eligible to Institute of Immunology and
participate. Participants were recruited through local primary care networks in the West Midlands, UK. Blood samples Immunotherapy, University of
and dried blood spots were taken 5–6 weeks after vaccination to assess adaptive immune responses using Elecsys Birmingham, Birmingham, UK
(H Parry MBChB, R Bruton PhD,
electrochemiluminescence immunoassay and cellular responses by ELISpot. Primary endpoints were percentage
G Tut PhD, M Ali MSc,
response and quantification of adaptive immunity. C Stephens MSc,
D Greenwood MSc,
Findings Between Dec 29, 2020, and Feb 28, 2021, 165 participants were recruited and included in the analysis. S Faustini PhD,
Prof A Richter MBChB, J Zuo PhD,
76 participants had received BNT162b2 (median age 84 years, IQR 82–89; range 80–98) and 89 had received ChAdOx1
Prof P Moss BMBCh);
nCoV-19 (median age 84 years, 81–87; 80–99). Antibody responses against the spike protein were detectable in Department of Immunology,
69 (93%) of 74 BNT162b2 vaccine recipients and 77 (87%) of 89 ChAdOx1 nCoV-19 vaccine recipients. Median Birmingham Heartlands
antibody titres were of 19·3 U/mL (7·4–79·4) in the BNT162b2 vaccine recipients and 19·6 U/mL (6·1–60·0) in the Hospital, University Hospitals
Birmingham, Birmingham, UK
ChAdOx1 nCoV-19 vaccine recipients (p=0·41). Spike protein-specific T-cell responses were observed in nine (12%) of
(S Hughes MSc,
73 BNT162b2 vaccine recipients and 27 (31%) of 88 ChAdOx1 nCoV-19 vaccine recipients, and median responses were A Huissoon MBBCh); Harborne
three-times higher in ChAdOx1 nCoV-19 vaccine recipients (24 spots per 1 × 10⁶ peripheral blood mononuclear cells) Medical Practice, Harborne,
than BNT162b2 vaccine recipients (eight spots per 1 × 10⁶ peripheral blood mononuclear cells; p<0·0001). Humoral Birmingham, UK
(R Meade MBBS); National
and cellular immune responses against spike protein were correlated in both cohorts. Evidence of previous
Infection Service, Public Health
SARS-CoV-2 infection was seen in eight participants (n=5 BNT162b2 recipients and n=3 ChAdOx1 nCoV-19 recipients), England, Colindale, London, UK
and was associated with 691-times and four-times increase in humoral and cellular immune responses across the (K Brown MBBChir,
whole cohort. G Amirthalingam MBBS);
National Infection Service,
Public Health England, Porton
Interpretation Single doses of either BNT162b2 or ChAdOx1 nCoV-19 in older people induces humoral immunity in Down, Salisbury, UK
most participants, and is markedly enhanced by previous infection. Cellular responses were weaker, but showed (A Otter PhD, B Hallis PhD)
enhancement after the ChAdOx1 nCoV-19 vaccine at the 5–6 week timepoint. Correspondence to:
Prof Paul Moss, Institute of
Immunology and
Funding Medical Research Council, National Institute for Health Research, and National Core Studies.
Immunotherapy, University of
Birmingham,
Copyright © 2021 The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY-NC-ND Birmingham B15 2TT, UK
4.0 license. p.moss@bham.ac.uk
Introduction (Oxford University–AstraZeneca) is longer, with
Vaccines have shown high levels of effectiveness evidence that delayed boosting might increase efficacy.5
against COVID-19-related illness, hospitalisation, and To accelerate population coverage with COVID-19
death.1,2 A range of vaccine approaches have been vaccines, some countries have elected to delay the timing
developed for delivery of the spike immunogen, of the second dose by 10–12 weeks. Real-world evidence
including mRNA, adenovirus, and protein-adjuvant now indicates that this protocol is highly effective, with
platforms.3 Most vaccine regimens use a two-dose over 80% relative protection against hospitalisation and
protocol with some variation in the time interval death in people aged 70 years and older.2
between vaccines. The BNT162b2 mRNA vaccine The BNT162b2 and ChAdOx1 nCoV-19 vaccines both
(tozinameran; Pfizer–BioNTech) is authorised for display high clinical efficacy, but little attention has been
administration at a 3-week interval,4 whereas the given to assessment of their relative immunogenicity after
interval for the ChAdOx1 nCoV-19 adenovirus vaccine single-dose administration. Information on single-dose
www.thelancet.com/healthy-longevity Vol 2 September 2021 e554
Articles
Research in context
Evidence before this study are equivalent in their ability to induce antibody responses at
Extended interval COVID-19 vaccine regimens are now used 5–6 weeks after vaccination. However, the proportion of people
widely in many countries. Real-world evidence suggests clinical who generate a spike-specific cellular response, and the
efficacy, but little is known regarding the relative induction of magnitude of this response, are both higher after the ChAdOx1
immune responses from different vaccines. This knowledge is nCoV-19 vaccine.
of particular importance in older people in whom
Implications of all the available evidence
immunosenescence might limit immune responses.
Cellular immune responses at 5–6 weeks after a single COVID-19
Added value of this study vaccine are stronger in older people who receive the ChAdOx1
Here we compare and contrast the immune response against nCoV-19 vaccine. The potential significance of this in relation to
spike protein after one dose of either the BNT162b2 vaccine or clinical protection prior to the second vaccine is currently
ChAdOx1 nCoV-19 vaccine in older people (aged 80–96 years) uncertain.
living in community settings. We show that the two vaccines
immunogenicity is particularly needed in relation to Immunological Analysis Urgent Public Health research
their use in older people, where the influence of study, according to the Declaration of Helsinki and good
immunosenescence might limit immune responses.6 clinical practice.
Furthermore, older people are under-represented in the Procedures All participants had received a single
vaccine registration studies, and for the majority of people vaccination of either BNT162b2 or ChAdOx1 nCoV-19 as
aged 80 years or older who live independently, data on part of the UK-wide national COVID-19 vaccination
immunological responses to the COVID-19 vaccines are programme. A 50 mL blood sample and dried blood spot
lacking. were taken at the same time, 5–6 weeks after the first
The BNT162b2 and ChAdOx1 nCoV-19 vaccines both vaccine, for antibody testing for SARS-CoV-2 responses
deliver full spike protein, with BNT162b2 including and IFN-γ ELISPot for cellular studies. This timepoint
a di-proline inclusion to stabilise the pre-fusion spike was selected as an approximate midpoint between first
protein.7 However, the different delivery systems are and second vaccines with an extended interval vaccination
likely to mediate markedly different forms of antigen schedule. Samples were used for antibody and cellular
presentation, which might be reflected in a different studies in this exploratory study.
profile or magnitude of humoral or adaptive immune
response. Outcomes
We compared adaptive immune responses in a IgG, IgA, and IgM antibodies specific to SARS-CoV-2 were
population of older people who had received a single detected using electrochemiluminescence assays on the
dose of either the BNT162b2 or ChAdOx1 nCoV-19 automated Cobas e801 analysers (Roche Diagnostics,
vaccines. Mannheim, Germany). Calibration and quality control
were done as recommended by the manufacturer. Anti-
Methods nucleocapsid protein antibodies were detected using the
Study design and participants qualitative Elecsys Anti-SARS-CoV-2 ECLIA (Roche
Participants aged 80 years or older, who had received Diagnostics, Indianapolis, IN, USA; COV2, product code
either the BNT162b2 vaccine or ChAdOx1 nCoV-19 09203079190), while anti-spike antibodies were detected
vaccine and who did not live in a residential or care using the quantitative Elecsys Anti-SARS-CoV-2 S ECLIA
home, or did not require assisted living and who were (Roche Diagnostics, Indianapolis, IN, USA; COV2 S,
living independently, were eligible for inclusion in the product code 09289275190). Anti-nucleocapsid results are
study. Comorbidities were permitted. Participants were expressed as cutoff index values, with a value of 1·0 or
recruited through local primary care networks in the more considered positive for anti-nucleocapsid antibodies.
West Midlands, UK. Participants were sent invitation Anti-spike protein values of 0·8 U/mL or more were
letters, and were asked to contact the research team if considered positive for anti-spike antibodies, within the
they wanted to participate. After initial contact with the fully quantitative range of the assay (0·4–2500 U/mL).
study team, participants were given the participant Samples of more than 2500 U/mL were diluted further
information sheet and consented verbally over the phone. (1:10, 1:100, and 1:1000) to within the quantitative range.
This was substantiated with written consent obtained at IgG antibodies specific for SARS-CoV-2 were detected
the first phlebotomy timepoint. Ethical approval was using chemiluminescent microparticle immunoassays
obtained from The North West Preston Research Ethics run on the Alinity i-series platform (Abbott, North
Committee with favourable outcome (number REC Chicago, IL, USA). Calibration and quality control were
20\NW\0240). The study was done under the Coronavirus done as recommended by the manufacturer. Antibodies
e555 www.thelancet.com/healthy-longevity Vol 2 September 2021
Articles
were detected using the Alinity SARS-CoV-2 IgG II
BNT162b2, ChAdOx1
Quant assay (Abbott; master lot number 25346FN00, n=76 nCoV-19,
kit insert number 06S61), with samples with a result of n=89
50 U/mL or more considered positive for anti-spike Sex
antibodies within the fully quantitative range of the Female 45 (59%) 53 (60%)
assay (21–40 000 U/mL). The Alinity platform was set Male 31 (41%) 36 (40%)
up to report results between 0·00 U/mL and Age at first vaccination, years 84 (82–89) 84 (81–87)
40 000 U/mL. Time between first vaccination and 40 39
Quantitative IgG antibody titres were measured sample, days
against spike protein, nucleocapsid protein, and other Data are n (%), median IQR, or mean.
antigens using the V-PLEX COVID-19 Respiratory
Panel 2 (96-well, ten spot plate was coated with three Table: Participant demographics
SARS-CoV-2 antigens [spike, spike receptor-binding
domain, spike N-terminal domain, and nucleocapsid];
category number K15372U, lot number Z0056764; Meso Statistical analysis
Scale Discovery [MSD], Rockville, MD, USA). Antigens Data were tested for normality using Kolmogorov-
were spotted at 200−400 μg/mL. Multiplex MSD Assays Smirnov analysis. For comparative analysis of antibody
were done as per the manufacturer’s instructions. To titres and cellular responses between the BNT162b2 or
measure IgG antibodies, 96-well plates were blocked ChAdOx1 nCoV-19 vaccine cohorts, a Mann-Whitney
with MSD Blocker A for 30 min. After washing with U test was done. Spearman rank correlation was used for
buffer, the samples were diluted 1:500 in diluent. comparing assay platforms for titres and correlating
Reference standards and positive controls and diluted T-cell responses. Antibody titres are also presented as the
samples were added to the wells. After a 2 h incubation, geometric mean with SEM for each method of antibody
plates were washed three times with wash buffer and assessment (appendix). The index of multiple deprivation See Online for appendix
detection antibody (SULFO-TAG Anti-Human IgG decile scores were derived from residential postcodes
Antibody, 1/200; Meso Scale Diagnostics, Rockville, using guidance on the national statistics website for For residential postcode data
MD, USA) diluted in diluent 100 was added. After 1 h of England. All analysis was done using Graphpad prism, see https://imd-by-postcode.
opendatacommunities.org
incubation at room temperature, the plates were washed version 9.1.0.
three times with wash buffer. MSD GOLD Read Buffer B
was added and plates were read immediately using a Role of the funding source
MESO QuickPlex SQ 120 (Meso Scale Diagnostics, The funder had no role in the study design, collection,
Rockville, MD, USA). Text files were then generated analysis, interpretation of the data, or writing of the
from the Methodical Mind software and then Article.
transferred to the DISCOVERY WORKBENCH
software, version 4.0. Data were then converted to Results
AU/mL, exported as csv files, and then adjusted for any Between Dec 29, 2020, and Feb 28, 2021, 165 participants
sample dilution. were recruited and included in the analysis. 76 participants
had received BNT162b2 (median age 84 years, IQR 82–89;
Cellular assays range 80–98) and 89 had received ChAdOx1 nCoV-19
Peripheral blood mononuclear cells (PBMCs) were isolated (median age 84 years, 81–87; 80–99; table). Participant
from whole blood samples using T-Cell Xtend (Oxford demographics showed no differences in age or gender.
Immunotec, Oxford, UK) and Ficoll. After quantification The multiple deprivation score indices were marginally
and dilution of recovered cells, 250 000 PBMCs different in participants who received ChAdOx1 nCoV-19
were plated into each well of a T-SPOT Discovery (7, IQR 3–9) compared with participants who received
SARS-CoV-2 kit (Oxford Immunotec). This test measures BNT162b2 (4, IQR 4–6). Spike protein-specific antibody
responses to overlapping peptides pools, covering protein responses were assessed using quantitative Roche spike
sequences of four different SARS-CoV-2 antigens, without protein-specific ELISA and positive responses were seen
HLA restriction, and includes negative control and in 69 (93%) of 74 participants after the BNT162b2 vaccine,
phytohaemagglutinin-stimulated cells as a positive control. and 77 (87%) of 89 participants after the ChAdOx1
Peptide sequences that showed high homology to endemic nCoV-19 vaccine (p=0·32). Corresponding median
coronaviruses were removed from the sequences, but antibody measurements were 19·3 U/mL after the
sequences that might have homology to SARS-CoV-1 were BNT162b2 vaccine and 19·6 U/mL after the ChAdOx1
retained. Cells were incubated and IFN-γ-secreting T cells nCoV-19 vaccine (p=0·41). Responses were also assessed
were counted. A cutoff of 24 or more spots per million cells using the quantitative Abbott spike-specific ELISA; no
on the S1 pool was defined as a positive result, in line significant difference was observed, with 62 (84%) of 74
with the T-SPOT Discovery SARS-CoV-2 kit (Oxford participants responding to BNT162b2 and 69 (78%) of 89
Immunotec, Oxford, UK). participants responding after ChAdOx1 nCoV-19 (p=0·70;
www.thelancet.com/healthy-longevity Vol 2 September 2021 e556
Articles
BNT162b2 ChAdOx1 Previous SARS-CoV-2 infection
A *
100000 100000 100000
spike IgG, IgA, and IgM titre
MSD SARS-CoV-2 spike IgG
10000 10000 10000
Abbott SARS-CoV-2
Roche SARS-CoV-2
response (AU/mL)
1000
spike IgG titre
1000 1000
100
100 100
10
1 10 10
0·1 1 1
BNT162b2 ChAdOx1 BNT162b2 ChAdOx1 BNT162b2 ChAdOx1
COVID-19 vaccine received COVID-19 vaccine received COVID-19 vaccine received
B
100000 100000 100000
spike IgG, IgA, and IgM titre
MSD SARS-CoV-2 spike IgG
MSD SARS-CoV-2 spike IgG
10000 10000 10000
Roche SARS-CoV-2
response (AU/mL)
response (AU/mL)
1000
1000 1000
100
100 100
10
1 p<0·0001 10 p<0·0001 10 p<0·0001
R=0·93 R=0·86 R=0·90
0·1 1 1
1 10 100 1000 10000 100000 0·1 1 10 100 1000 10000 100000 1 10 100 1000 10000 100000
Abbott SARS-CoV-2 spike IgG titre Roche SARS-CoV-2 spike IgG, IgA, and IgM titre Abbott SARS-CoV-2 spike IgG titre
C † † †
100000 100000 100000
spike IgG, IgA, and IgM titre
MSD SARS-CoV-2 spike IgG
10000 10000 10000
Abbott SARS-CoV-2
Roche SARS-CoV-2
response (AU/mL)
1000
spike IgG titre
1000 1000
100
100 100
10
1 10 10
0·1 1 1
Previous infection No previous infection Previous infection No previous infection Previous infection No previous infection
Previous SARS-CoV-2 infection status Previous SARS-CoV-2 infection status Previous SARS-CoV-2 infection status
D *
1000 10000 100000
spike IgG, IgA, and IgM titre
MSD SARS-CoV-2 spike IgG
10000
Abbott SARS-CoV-2
100 1000
Roche SARS-CoV-2
response (AU/mL)
spike IgG titre
1000
10 100
100
1 10
10
0·1 1 1
BNT162b2 ChAdOx1 BNT162b2 ChAdOx1 BNT162b2 ChAdOx1
COVID-19 vaccine received COVID-19 vaccine received COVID-19 vaccine received
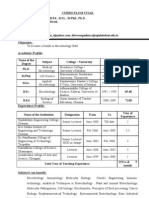
Figure 1: Spike protein-specific antibody responses after single vaccination with BNT162b2 or ChAdOx1 nCoV-19 in older people
Spike protein-specific antibody responses (A) and correlation between spike protein-specific antibody responses (B) measured using Roche, Abbott, and MSD tests in participants after a single
vaccination with BNT162b2 or ChAdOx1 nCoV-19 in the total cohort. Correlation was determined using Spearman’s correlation test. (C) Comparison of spike-protein specific antibody responses in
participants with previous SARS-CoV-2 infection or no previous infection after a single vaccination with BNT162b2 or ChAdOx1 nCoV-19. (D) Spike protein-specific antibody responses in participants
without previous SARS-CoV-2 infection after single BNT162b2 or ChAdOx1 nCoV-19 vaccination. MSD=Meso Scale Discovery. *p<0·05. †p<0·0001.
figure 1; median 216 U/mL [IQR 75–680] in the BNT162b2 domain-specific responses. Using this platform,
group vs 200 U/mL [60–478] in the ChAdOx1 nCoV-19 antibody responses were higher in participants who had
group; p=0·33). received the ChAdOx1 nCoV-19 vaccine on both assays
Analyses were also done on the MSD platform to (p=0·04; figure 1). These data reveal some potential
measure whole spike protein-specific or receptor-binding difference in the nature of the humoral response
e557 www.thelancet.com/healthy-longevity Vol 2 September 2021
Articles
BNT162b2 ChAdOx1 Previous SARS-CoV-2 infection
A B C
* †
10000 10000 10000
IFN-γ spike-specific cellular
IFN-γ spike-specific cellular
response (SFU/10⁶ PBMCs)
response (SFU/10⁶ PBMCs)
1000 1000
phytohaemagglutinin
(SFU/10⁶ PBMCs)
IFN-γ spot with
1000
100 100
10 10
100
1 1
0·1 0·1 10
BNT162b2 ChAdOx1 Previous No previous BNT162b2 ChAdOx1
infection infection
COVID-19 vaccine received Previous SARS-CoV-2 infection status COVID-19 vaccine received
D
10000 p=0·01 10000 p=0·02 10000 p=0·0004
R=0·20 R=0·19 R=0·27
IFN-γ spike-specific cellular
IFN-γ spike-specific cellular
IFN-γ spike-specific cellular
response (SFU/10⁶ PBMCs)
response (SFU/10⁶ PBMCs)
response (SFU/10⁶ PBMCs)
1000 1000 1000
100 100 100
10 10 10
1 1 1
0·1 1 10 100 1000 10000 100000 0·1 1 10 100 1000 10000 100000 0·1 1 10 100 1000 10000 100000
Roche SARS-CoV-2 spike IgG, IgA, and Abbott SARS-CoV-2 spike IgG titre (AU/mL) MSD SARS-CoV-2 spike IgG response (AU/mL)
IgM titre (AU/mL)
Figure 2: Spike protein-specific cellular responses after single vaccination with BNT162b2 or ChAdOx1 nCoV-19 in older people
(A) SARS-CoV-2 spike protein-specific cellular responses after single vaccination with BNT162b2 or ChAdOx1 nCoV-19. Assessment was by IFN-γ ELISpot. (B) Comparison of cellular responses in those
with previous SARS-CoV-2 infection or no previous infection. (C) Positive control of IFN-γ ELISpot with phytohaemagglutinin stimulation. (D) Correlation between spike protein-specific cellular and
humoral immune responses after single vaccination with BNT162b2 or ChAdOx1 nCoV-19, measured using Roche, Abbott, and MSD tests. PBMC=peripheral blood mononuclear cells. *p<0·0001.
†p<0·05.
induced by the two vaccines, with associated variation (BNT162b2 p=0·01 vs ChAdOx1 nCoV-19 p=0·0004;
on different assay systems, but strong correlations were figure 1).
observed between assays, and responses are overall We next assessed the induction of spike protein-
similar after each vaccine (figure 1). specific T-cell responses after vaccination using IFN-γ
Eight participants showed evidence of previous ELISpot, which detects CD4-positive and CD8-positive
SARS-CoV-2 infection on the basis of positive T-cell responses. Cellular responses were detectable at
nucleocapsid protein-specific serology. Of these 5 weeks after a single dose of BNT162b2 in nine (12·3%)
participants, five had received BNT162b2 and three had of 73 participants and in 27 (30·7%) of 88 participants
received ChAdOx1 nCoV-19. Spike protein-specific after a single dose of ChAdOx1 nCoV-19. Furthermore,
antibody titres by Roche ELISA were 691-times higher the magnitude of cellular responses was three-times
in these eight participants compared with participants greater within the ChAdOx1 nCoV-19 subgroup at
without previous infection (n=11 750 previous infection 24 spots per 1 × 10⁶ PBMCs compared with eight spots
vs n=17 no previous infection; p<0·0001) and were per 1 × 106 PBMCs after BNT162b2 (p<0·0001), and this
also significantly higher in all other assay systems difference remained after exclusion of participants
(figure 1). with previous SARS-CoV-2 infection (24 spots per
To understand the efficacy of vaccination within 1 × 106 PBMCs vs eight spots per 1 × 10⁶ PBMCs;
infection-naive participants, we compared immune p<0·0001). Participants with serological evidence of
responses after exclusion of participants with previous previous SARS-CoV-2 infection showed a four-times
SARS-CoV-2 infection. No difference was observed increase in cellular responses compared with
in spike protein-specific antibody titres by Roche participants with no previous infection (previous
(BNT162b2 n=17 vs ChAdOx1 nCoV-19 n=18; p=0·63) or infection median 48 vs no previous infection median 12;
Abbott platform (BNT162b2 n=178 vs ChAdOx1 nCoV-19 p=0·002; figure 2).
n=194; p=0·52), but a difference was observed using the We next assessed the relationship between spike
MSD platform for spike protein-specific and receptor- protein-specific cellular and humoral responses and
binding domain-specific responses, with higher found cellular responses to be correlated positively with
titres observed after the ChAdOx1 nCoV-19 vaccine antibody titres from all four assay systems (figure 2).
www.thelancet.com/healthy-longevity Vol 2 September 2021 e558
Articles
Discussion to an adjuvant effect from the adenovirus vector. The
Extended dose COVID-19 vaccine protocols have been Johnson & Johnson vaccine, which is also based on an
initiated in several countries, and have shown high levels adenoviral delivery system, is now licensed for
of clinical protection after the first dose.2 Here we assessed single-dose administration, and has been shown to
the immune responses after single COVID-19 vaccinations induce effective immune responses and strong clinical
in a population of people aged 80–96 years, in whom protection.15 It is important to highlight that this
vaccine responses against infections such as influenza are comparison reflects only a single timepoint, and
often suboptimal.6,8 We recruited 165 participants of the differences in the kinetics of humoral and cellular
appropriate age within the logistical timeframe offered by responses after the two vaccine platforms might differ.
the vaccination programme and while under lockdown In the present study, across the whole cohort, cellular
restrictions . Our results show reassuring levels of humoral responses were lower than has been reported for younger
immunity after one dose of BNT162b2 or ChAdOx1 participants after single-dose vaccination, which might
nCoV-19, which is likely to correlate with protection against reflect the effect of immunosenescence within our
primary infection; however, the ChAdOx1 nCoV-19 cohort.10 As such, any potential negative effect of ageing
adenovirus-based platform was associated with induction might be more noticeable in relation to cellular response
of a stronger cellular immune response than vaccination than humoral immunity. At this stage, the importance of
with the mRNA-based BNT162b2 vaccination. cellular immunity in relation to protection from infection
Measurable spike protein-specific antibody responses is unclear for SARS-CoV-2. Influenza-specific cellular
were observed in more than 87% across all vaccine responses have been shown to limit the severity of
recipients. The median titre of spike protein-specific infection, and this effect might also be the case for
antibody was 19·3 U/mL, which was lower than that SARS-CoV-2 infection.16 However, there is currently no
reported in younger individuals.9–11 Antibody responses evidence of differential control of severe clinical outcomes
after one dose of either vaccine were similar, as measured after a single vaccination with either BNT162b2 or
using the Roche and Abbott assays; however, results were ChAdOx1 nCoV-19. Cellular-specific immune responses
significantly higher after vaccination with ChAdOx1 might also be of value in supporting and maintaining
nCoV-19 when measured using the MSD platform. The humoral immunity over the long term, and as such it will
reasons for these results are unclear, but do not appear to be of interest to study this cohort over time.
be related to factors such as isotype assay. In our cohort of older people, T-cell responses were
We observed a 691-times increase in median antibody measured on the standard assessment of IFN-γ secretion,
titre after vaccination in participants who had previous but this does not preclude the presence of spike protein-
SARS-CoV-2 infection. A similar result was observed specific T cells that make other inflammatory cytokines,
previously in people with a median age of 40 years who and this possibility will be assessed going forward. The
were given the BNT162b2 or elasomeran (CX-024414; possible presence of other spike protein-specific T cells
Moderna) vaccines, but the relative increase was only will be particularly important in this cohort, in
45 times.12 In health-care workers, a more modest whom the balance of inflammatory and anti-inflammatory
6·5-times increase was observed after one vaccination cytokines associated with inflammaging can modulate
with BNT162b2 in participants with previous SARS- responsiveness to vaccination and might be influenced
CoV-2 infection.10 This result indicates a 15-times further by the type of vaccine platform and adjuvant used.
increase in infection-priming in older people,12 and is a Our study is limited by the fact that it was exploratory,
similar relative enhancement to that we observed in and therefore not randomised. An assessment was
patients with immune suppression (unpublished data). therefore made to consider potential selection bias. We
It appears probable that natural infection markedly are not aware of any known confounding demographic
enhances the breadth and quality of spike protein- association between vaccine type and immune response.
specific immune responses, and to overcome some of Potential confounding differences between the BNT162b2
the negative influences of age on the vaccine-induced and ChAdOx1 nCoV-19 cohorts include differences in
immune response. The mechanisms behind this finding comorbidities, lifestyle, and medication, but this
will be necessary to investigate further, and could provide information was not available for analysis. Participant
insight into the optimal nature and timing of booster demographics showed no differences in age or gender.
vaccinations. Participants who received BNT162b2 were living in
We noted a marked difference in the induction of spike slightly more socioeconomically deprived areas. To the
protein-specific cellular responses, whereby the ChAdOx1 best of our knowledge, there has not been any study
nCoV-19 vaccine resulted in a three-times higher median of COVID-19 vaccine-induced immune responses in
virus-specific T-cell response than BNT162b2. This relation to social deprivation index. It is possible that
vaccine platform has been shown previously to induce social deprivation index might affect vaccine-induced
strong cellular immunity, which might be reflected in immune responses, but clinical protection after
our observations.13,14 The mechanisms that led to vaccination appears equally strong across the whole
improved celluar response are not clear, but might relate population.
e559 www.thelancet.com/healthy-longevity Vol 2 September 2021
Articles
The approved regimen for BNT162b2 vaccination is the 4 Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the
delivery of two doses at 3 weeks apart, and the second BNT162b2 mRNA COVID-19 vaccine. N Engl J Med 2020; 383: 2603–15.
5 Voysey M, Clemens SAC, Madhi SA, et al. Safety and efficacy of the
vaccine strongly enhances humoral and cellular ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2:
immunity.10,17 As such, our findings relate only to an interim analysis of four randomised controlled trials in Brazil,
assessment of vaccine efficacy in relation to an extended- South Africa, and the UK. Lancet 2021; 397: 99–111.
6 Ciabattini A, Nardini C, Santoro F, Garagnani P, Franceschi C,
interval second dose, where both vaccines have shown Medaglini D. Vaccination in the elderly: the challenge of immune
strong clinical efficacy. The immune correlates identified changes with aging. Semin Immunol 2018; 40: 83–94.
in our study should be studied futher in long-term 7 Klasse PJ, Nixon DF, Moore JP. Immunogenicity of clinically
relevant SARS-CoV-2 vaccines in nonhuman primates and humans.
assessment of clinical responses in this older age group. Sci Adv 2021; 7: eabe8065.
Contributors 8 Siegrist C-A, Aspinall R. B-cell responses to vaccination at the
HP, RB, and PM designed the study. PM, HP, and JZ wrote the Article. extremes of age. Nat Rev Immunol 2009; 9: 185–94.
HP, RB, and RM recruited participants. SH, JZ, CS, SF, GT, AR, and HP 9 Müller L, Andrée M, Moskorz W, et al. Age-dependent immune
did the experiments. HP, JZ, PM, and DG verified and analysed the data. response to the Biontech/Pfizer BNT162b2 COVID-19 vaccination.
MA, AO, BH, and AH did the experiments. GA and KB designed the medRxiv 2021; published online March 5. https://www.medrxiv.org/
study. All authors had full access to the data and approved submission of content/10.1101/2021.03.03.21251066v1 (preprint).
this Article. PM had the final responsibility to submit for publication. 10 Angyal A, Longet S, Moore S, et al. T-cell and antibody responses to
first BNT162b2 vaccine dose in previously SARS-CoV-2-infected and
Declaration of interests infection-naive UK healthcare workers: a multicentre, prospective,
We declare no competing interests. observational cohort study. SSRN 2021; published March 25. http://
dx.doi.org/10.2139/ssrn.3812375 (preprint).
Data sharing
The de-identified data used in this study can be shared after approval by 11 Manisty C, Otter A, Treibel T, et al Antibody response to first
BNT162b2 dose in previously SARS-CoV-2-infected individuals.
the ethics authority and on request to the corresponding author.
Lancet 2021; 397: 1057–58.
Acknowledgments 12 Krammer F, Srivastava K, Alshammary H, et al. Antibody responses
This work was partially supported by National Core Studies Immunity in seropositive persons after a single dose of SARS-CoV-2 mRNA
and the UK Coronavirus Immunology Consortium funded by vaccine. N Engl J Med 2021; 384: 1372–74.
National Institute for Health Research/UK Research and Innovation. 13 Anywaine Z, Whitworth H, Kaleebu P, et al. Safety and
We thank Rory Meade, Rosie Laugharne, Tom Groves, Parjit Dhillon, immunogenicity of a 2-dose heterologous vaccination regimen with
Eleanor Brodie, and the patients and staff at Harborne Medical Practice, Ad26.ZEBOV and MVA-BN-Filo Ebola vaccines: 12-month data
Northumberland House Surgery, New Road Surgery, Lapal Medical from a phase 1 randomized clinical trial in Uganda and Tanzania.
Practice and Wychbury Medical Group. We also thank Millie Manning, J Infect Dis 2019; 220: 46–56.
Danielle Sutherland, Tamsin Drury, and Alex Bray for their help in 14 Williams K, Bastian AR, Feldman RA, et al. Phase 1 safety and
recruitment. We are grateful for support from Rajinder Jeet and immunogenicity study of a respiratory syncytial virus vaccine with
an adenovirus 26 vector encoding prefusion F (Ad26.RSV.preF) in
Shahada Rahman Joli with phlebotomy services.
adults aged ≥60 years. J Infect Dis 2020; 222: 979–88.
References 15 Sadoff J, Le Gars M, Shukarev G, et al. Interim results of a
1 Dagan N, Barda N, Kepten E, et al. BNT162b2 mRNA COVID-19 phase 1-2a trial of Ad26.COV2.S COVID-19 vaccine. N Engl J Med
vaccine in a nationwide mass vaccination setting. N Engl J Med 2021; 384: 1824–35.
2021; 384: 1412–23. 16 Sant AJ, DiPiazza AT, Nayak JL, Rattan A, Richards KA. CD4 T cells
2 Bernal JL, Andrews N, Gower C, et al. Effectiveness of the Pfizer- in protection from influenza virus: Viral antigen specificity and
BioNTech and Oxford-AstraZeneca vaccines on covid-19 related functional potential. Immunol Rev 2018; 284: 91–105.
symptoms, hospital admissions, and mortality in older adults in 17 Parry HM, Tut G, Faustini S, et al. BNT162b2 vaccination in people
England: test negative case-control study. BMJ 2021; 373: n1088. over 80 years of age induces strong humoral immune responses
3 WHO. Draft landscape and tracker of COVID-19 candidate vaccines. with cross neutralisation of P.1 Brazilian variant. SSRN 2021;
https://www.who.int/publications/m/item/draft-landscape-of-covid- published online March 31. http://dx.doi.org/10.2139/ssrn.3816840
19-candidate-vaccines (accessed July 24, 2021). (preprint).
www.thelancet.com/healthy-longevity Vol 2 September 2021 e560
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- LAS 4 - Recognize The Major Categories of Biomolecules Such As Carbohydrates, Lipids, Proteins, and Nucleic AcidsDocument3 pagesLAS 4 - Recognize The Major Categories of Biomolecules Such As Carbohydrates, Lipids, Proteins, and Nucleic AcidsSalve Serrano0% (1)
- Systems Vaccinology of The BNT162b2 MRNA Vaccine in HumansDocument38 pagesSystems Vaccinology of The BNT162b2 MRNA Vaccine in HumansChristian GaraffaNo ratings yet
- Articles: BackgroundDocument10 pagesArticles: BackgroundChristian GaraffaNo ratings yet
- Safety and Efficacy of The BNT162b2 MRNA Covid-19 Vaccine Through 6 MonthsDocument13 pagesSafety and Efficacy of The BNT162b2 MRNA Covid-19 Vaccine Through 6 MonthsChristian GaraffaNo ratings yet
- Comparative Immunogenicity of BNT162b2 MRNA Vaccine With Natural SARS-CoV-2 InfectionDocument13 pagesComparative Immunogenicity of BNT162b2 MRNA Vaccine With Natural SARS-CoV-2 InfectionChristian GaraffaNo ratings yet
- Decreased Infectivity Following BNT162b2 VaccinatiDocument9 pagesDecreased Infectivity Following BNT162b2 VaccinatiChristian GaraffaNo ratings yet
- Dynamics of Antibody Response To BNT162b2 Vaccine After Six MonthsDocument9 pagesDynamics of Antibody Response To BNT162b2 Vaccine After Six MonthsChristian GaraffaNo ratings yet
- Antibody Response After Second BNT162b2 Dose in Allogeneic HSCT RecipientsDocument2 pagesAntibody Response After Second BNT162b2 Dose in Allogeneic HSCT RecipientsChristian GaraffaNo ratings yet
- Association Between Exposure Characteristics and The Risk For COVID-19 Infection Among Health Care Workers With and Without BNT162b2 VaccinationDocument4 pagesAssociation Between Exposure Characteristics and The Risk For COVID-19 Infection Among Health Care Workers With and Without BNT162b2 VaccinationChristian GaraffaNo ratings yet
- 10 PlasmidsDocument17 pages10 Plasmidsparduman kumarNo ratings yet
- TraducidoDocument23 pagesTraducidoLuis Fabricio PlazaNo ratings yet
- DR S ThiruvengadamDocument5 pagesDR S ThiruvengadamThiruvengadam SubramaniyanNo ratings yet
- New IF-2022-JCR完整Document1,477 pagesNew IF-2022-JCR完整Alia JavedNo ratings yet
- Dot Blot ProtocolDocument2 pagesDot Blot ProtocolSuki BlytheNo ratings yet
- Lecture 8 PhotosynthesisDocument35 pagesLecture 8 PhotosynthesisAllison AllaucaNo ratings yet
- Nicotine ProductionDocument10 pagesNicotine Productionkyungsoo's death glareNo ratings yet
- Biosimilar Approval ProcessDocument2 pagesBiosimilar Approval ProcessMoustapha El-AmineNo ratings yet
- EXER10Document4 pagesEXER10Wency Joy ObreroNo ratings yet
- AgeLOC Power Point by Dr. Joe Chang (Aug 15, 2009)Document33 pagesAgeLOC Power Point by Dr. Joe Chang (Aug 15, 2009)trasuccess100% (1)
- Relative Quantitation of Gene ExpressionDocument60 pagesRelative Quantitation of Gene ExpressionmarianariasNo ratings yet
- MSP 3Document15 pagesMSP 3Arunaditya Deshmukh (Adi)No ratings yet
- Biochemistry JSS Medical College: DR - Prashant VishwanathDocument68 pagesBiochemistry JSS Medical College: DR - Prashant VishwanathAravind VPNo ratings yet
- Unit 4: Modern Biotechnological Processes: Guidelines For Choosing Host-Vector SystemsDocument3 pagesUnit 4: Modern Biotechnological Processes: Guidelines For Choosing Host-Vector SystemsSudarsan CrazyNo ratings yet
- เอกสารการบรรยาย - หัวข้อ 1 IntroductionDocument77 pagesเอกสารการบรรยาย - หัวข้อ 1 Introduction许伟思No ratings yet
- Alu LabDocument32 pagesAlu LabSusan HuynhNo ratings yet
- Tutorial 3-Necleic AcidDocument4 pagesTutorial 3-Necleic AcidEngNo ratings yet
- T4 DNA Ligation Kit TAKARADocument12 pagesT4 DNA Ligation Kit TAKARAxprakashNo ratings yet
- Protein Engineering and Its Applications in Food Industry 2017Document10 pagesProtein Engineering and Its Applications in Food Industry 2017SerkanNo ratings yet
- Azithromycin Brands in PakistanDocument4 pagesAzithromycin Brands in PakistanibNo ratings yet
- SasdsadsaDocument11 pagesSasdsadsaJorge MariaNo ratings yet
- History of GeneticsDocument4 pagesHistory of GeneticsJanine FandaganiNo ratings yet
- Unit 2Document15 pagesUnit 2Anadi ChauhanNo ratings yet
- Cellular Respiration: How Is Energy Transferred and Transformed in Living Systems?Document10 pagesCellular Respiration: How Is Energy Transferred and Transformed in Living Systems?Fitore RociNo ratings yet
- Biology Midterm Review 2023Document8 pagesBiology Midterm Review 2023beegirl954No ratings yet
- Construction of Phylogenetic TreeDocument12 pagesConstruction of Phylogenetic TreeKris ManuelNo ratings yet
- Nonribosomal Peptide Synthetase Biosynthetic Clusters of ESKAPE PathogensDocument29 pagesNonribosomal Peptide Synthetase Biosynthetic Clusters of ESKAPE PathogensMarina DomencoNo ratings yet
- Ncert Line by Line 28updated29-286-299Document14 pagesNcert Line by Line 28updated29-286-299123No ratings yet
- EMA - Question From Croatian Fact-Checking Website Regarding L1 ElementsDocument5 pagesEMA - Question From Croatian Fact-Checking Website Regarding L1 ElementsAna BenacicNo ratings yet