Professional Documents
Culture Documents
Oral Medicine - Update For The Dental Practitioner: Red and Pigmented Lesions
Oral Medicine - Update For The Dental Practitioner: Red and Pigmented Lesions
Uploaded by
shawn mary abrahamOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oral Medicine - Update For The Dental Practitioner: Red and Pigmented Lesions
Oral Medicine - Update For The Dental Practitioner: Red and Pigmented Lesions
Uploaded by
shawn mary abrahamCopyright:
Available Formats
6
IN BRIEF
• Most red or hyperpigmented lesions in the mouth are inconsequential.
• However, cancer and some systemic diseases may present in this way.
• Most red lesions are inflammatory or atrophic but erthythroplasia is potentially malignant.
• Most hyperpigmented lesions are racial or due to embedded material (eg amalgam tattoo)
but malignant and systemic disease can present in this way.
• Biopsy may be indicated.
Oral Medicine — Update for the dental practitioner
Red and pigmented lesions
C. Scully1 and D. H. Felix2
This series provides an overview of current thinking in the more relevant areas of oral medicine for primary care practitioners,
written by the authors while they were holding the Presidencies of the European Association for Oral Medicine and the British
Society for Oral Medicine, respectively. A book containing additional material will be published. The series gives the detail
necessary to assist the primary dental clinical team caring for patients with oral complaints that may be seen in general dental
practice. Space precludes inclusion of illustrations of uncommon or rare disorders, or discussion of disorders affecting the hard
tissues. Approaching the subject mainly by the symptomatic approach — as it largely relates to the presenting complaint — was
considered to be a more helpful approach for GDPs rather than taking a diagnostic category approach. The clinical aspects of the
relevant disorders are discussed, including a brief overview of the aetiology, detail on the clinical features and how the diagnosis
is made. Guidance on management and when to refer is also provided, along with relevant websites which offer further detail.
ORAL MEDICINE RED AND PIGMENTED LESIONS
1. Aphthous and other This article covers red lesions followed by hyper-
common ulcers pigmentation.
2. Mouth ulcers of more
serious connotation RED ORAL LESIONS
3. Dry mouth and disorders Red oral lesions are commonplace and usually
of salivation associated with inflammation in, for example,
4. Oral malodour mucosal infections. However, red lesions can also
be sinister by signifying severe dysplasia in ery-
5. Oral white patches
throplasia, or malignant neoplasms (Table 1).
6. Oral red and
hyperpigmented patches Geographic tongue (erythema migrans)
7. Orofacial sensation and Geographic tongue (Fig. 1) is a very common con- Fig. 1 Geographic
movement tongue
dition and cause of sore tongue, affecting at least
8. Orofacial swellings and 1-2% of patients. There is a genetic background,
lumps and often a family history. Many patients with a
9. Oral cancer fissured tongue (scrotal tongue) also have geo-
10. Orofacial pain graphic tongue. Erythema migrans is associated
with psoriasis in 4% and the histological appear-
ances of both conditions are similar. Some patients
1*Professor, Consultant, Dean, Eastman
have atopic allergies such as hay fever and a few
Dental Institute for Oral Health Care
Sciences, 256 Gray’s Inn Road, UCL,
relate the symptoms to various foods. A few have
University of London, London WC1X 8LD; diabetes mellitus.
2Consultant, Senior Lecturer, Glasgow
Dental Hospital and School, 378 Clinical features
Sauchiehall Street, Glasgow G2 3JZ /
Associate Dean for Postgraduate Dental Geographic tongue typically involves the
Education, NHS Education for Scotland, dorsum of the tongue, sometimes the ventrum. It Figs 2 and 3 Geographic tongue
2nd Floor, Hanover Buildings, 66 Rose is often asymptomatic but a small minority of
Street, Edinburgh EH2 2NN
*Correspondence to: Professor Crispian
patients complain of soreness; these patients are size, and spread or move to other areas sometimes
Scully CBE virtually invariably middle-aged. If sore, this may within hours (Figs 2 and 3).
Email: c.scully@eastman.ucl.ac.uk be noted especially with acidic foods (for example The red areas are often surrounded by dis-
tomatoes or citrus fruits) or cheese. tinct yellowish slightly raised margins. There is
Refereed Paper
© British Dental Journal 2005; 199: There are irregular, pink or red depapillated increased thickness of the intervening filiform
639–645 maplike areas, which change in shape, increase in papillae.
BRITISH DENTAL JOURNAL VOLUME 199 NO. 10 NOV 26 2005 639
PRACTICE
Keypoints for patients: Table 1 Most common causes of red lesions
Denture sore mouth
(denture-related stomatitis) Localised
• Denture sore mouth is common, Inflammatory lesions
but rarely sore Geographic tongue
• It is caused mainly by a yeast Candidosis
(Candida) that usually lives
Lichen planus
harmlessly in the mouth and
elsewhere Drugs
• It is not transmitted to others Reactive lesions
• It may be precipitated by Pyogenic granulomas
prolonged wearing of a dental Peripheral giant cell granulomas
appliance, especially at night, Fig. 4 Candida-associated denture stomatitis
Atrophic lesions
which allows the yeast to grow
Geographic tongue
• It predisposes to sores at the
corners of the mouth (angular Lichen planus
cheilitis) Lupus erythematosus
• It has no serious long-term Erythroplasia
consequences Avitaminosis B12
• Blood tests, microbiological studies Purpura
or biopsy may be required
Trauma
• It is best controlled by:
Thrombocytopenia
leaving out the appliance,
allowing the mouth to heal Vascular
cleaning the appliance (as below) Telangiectases (Hereditary haemorrhagic telangiectasia
or scleroderma or post-irradiation ngiomas) Fig. 5
disinfecting the appliance (as per Median rhomboid glossitis
additional instructions) Neoplasms
using antifungal creams or gels Squamous carcinoma
regularly for up to four weeks Kaposi’s sarcoma
• The appliance may require Giant cell tumour
adjustment or changing Wegener’s granulomatosis
• Keep the appliance as clean as
Generalised
natural teeth. Clean both surfaces
(inside and outside) after meals Inflammatory lesions
and at night. Use washing-up Most red lesions are inflammatory, usually geographic
liquid and a toothbrush and tongue (erythema migrans) (Figs 1 to 3)
lukewarm water and hold it over a Viral infections (eg herpes simplex stomatitis)
basin containing water, in case you
drop it, which could cause it to Fungal infections
break. Never use hot water, as it Candidosis
may alter the colour. A disclosing Fig. 6 Erythematous candidosis
denture-related stomatitis, discussed below, is
agent, for example Rayners Blue or usually a form of mild chronic erythematous
Red food colouring (available at candidosis consisting of inflammation beneath essary to exclude diabetes, or anaemia if there
most supermarkets) can be applied a denture,orthodontic or other appliance (Fig. 4) is confusion with a depapillated tongue of
with cotton buds, to help see
whether you are cleaning the
median rhomboid glossitis; a persistent red, glossitis.
rhomboidal depapillated area in the midline
appliance thoroughly enough. If
dorsum of tongue (Fig. 5)
stains or calculus deposits are Management
difficult to remove, try an acute oral candidosis; may cause widespread Reassurance remains the best that can be given.
overnight immersion (eg Dentural, erythema and soreness sometimes with thrush,
often a complication of corticosteroid or Zinc sulphate 200mg three times daily for three
Milton or Steradent), or an
application of Denclen antibiotic therapy. Red lesions of candidosis months or a topical rinse with 7% salicylic acid in
• Dentures should be left out
may also be seen in HIV disease, typically in the 70% alcohol are advocated by some and may
palate (Fig. 6) occasionally help.
overnight, so that your mouth has a
rest. It is not natural for your palate Bacterial infections:
to be covered all the time and the Cancer treatment-related mucositis; common Patient information and websites
chances of getting an infection are after irradiation of tumours of the head and http://www.usc.edu/hsc/dental/opath/Cards/Ge
increased if the dentures are worn neck, or chemotherapy eg for leukaemia
24 hours a day. Ensure you leave the ographicTongue.html
Immunological reactions such as lichen planus, http://www.worlddent.com/2001/05/series/ncut-
dentures out for at least some time
plasma cell gingivostomatitis, granulomatous
and keep them in Dentural or
disorders (sarcoidosis, Crohn’s disease, orofacial
tic1_2.xml
Steradent, as they may distort if
granulomatosis), amyloidosis, and graft versus
allowed to dry out
host disease DENTURE-RELATED STOMATITIS (DENTURE-
• Special precautions for dentures INDUCED STOMATITIS; DENTURE SORE
A vitaminosis B or iron deficiency or folate
with metal parts: Denclen,
Dentural and Milton may discolour
deficiency MOUTH; CHRONIC ERYTHEMATOUS
metal, so use with care. Brush CANDIDOSIS)
briefly to remove stains and Denture-related stomatitis consists of mild
deposits, rinse well with lukewarm Diagnosis inflammation of the mucosa beneath a
water and do not soak overnight The diagnosis of geographic tongue is clinical denture — usually a complete upper denture.
• Before re-use, wash in water and mainly from the history of a migrating pat- This is a common condition, mainly of the
brush the appliance to remove
loosened deposits
tern and the characteristic clinical appear- middle-aged or elderly, more prevalent in
ance. Blood examination may rarely be nec- women than men.
640 BRITISH DENTAL JOURNAL VOLUME 199 NO. 10 NOV 26 2005
PRACTICE
Aetiopathogenesis
Table 2 Management of denture-related stomatitis Keypoints for dentists:
Dental appliances (mainly dentures) especially Denture-related stomatitis
when worn throughout the night, or a dry • Denture hygiene measures
• Denture related stomatitis is
mouth, favour development of this infection. It • Antifungal therapy (eg topical or systemic) caused mainly by a yeast (Candida)
is not caused by allergy to the dental material (if • If unresponsive to above, investigate for underlying but bacteria may also be involved
it were, it would affect mucosae other than just predisposing factors • It may be precipitated by
that beneath the appliance). prolonged wearing of a dental
However, it is still not clear why only some dentures should be left out of the mouth at night, appliance, especially at night
denture wearers develop denture-related stomati- and stored in an appropriate antiseptic which • It predisposes to angular cheilitis
tis, since most patients appear otherwise healthy. has activity against yeasts (Table 2). • It is best controlled by:
Dentures can produce a number of ecological Cleansers containing alkaline hypochlorites, leaving out the appliance,
changes; the oral flora may be altered and disinfectants, or yeast lytic enzymes are most allowing the mouth to heal
plaque collects between the mucosal surface of effective against candida. Denture soak solution disinfecting the appliance
using antifungal creams or gels
the denture and the palate. containing benzoic acid is taken up into the
(eg miconazole),
The accumulation of microbial plaque (bacte- acrylic resin and can completely eradicate pastilles/lozenges (eg nystatin,
ria and/or yeasts) on and attached to the fitting C.albicans from the denture surface. Chlorhexi- amphotericin) or capsules
surface of the denture and the underlying mucosa dine gluconate can also eliminate C.albicans on (fluconazole) regularly for up to
produces an inflammatory reaction. When candi- the denture surface and a mouthwash can reduce four weeks
da is involved, the more common terms ‘candida- the palatal inflammation. • The appliance may require
adjustment or changing
associated denture stomatitis’, ‘denture-induced The mucosal infection is eradicated by
candidosis’ or ‘chronic erythematous candidosis’ brushing the palate with chlorhexidine mouth- • Blood tests, microbiological studies
or biopsy may be required if the
are used. wash or gel, and using miconazole gel, nys- lesion is unresponsive
In addition, the saliva that is present between tatin pastilles, amphotericin lozenges or flu-
the maxillary denture and the mucosa may have a conazole, administered concurrently with an
lower pH than usual. Denture-related stomatitis is oral antiseptic such as chlorhexidine which
sometimes associated also with various bacteria has antifungal activity.
but is not exclusively associated with infection,
and occasionally mechanical irritation is at play. Patient information and website
http://www.emedicine.com/derm/topic642.htm
Clinical features
The characteristic presenting features of den- Neoplastic lesions; red neoplasms include:
ture-related stomatitis are chronic erythema and • Peripheral giant cell tumours
oedema of the mucosa that contacts the fitting • Angiosarcomas such as Kaposi’s sarcoma—a
surface of the denture (Fig. 2). Uncommon com- common neoplasm in HIV/AIDS, appears in
plications include: the mouth as red or purplish areas or nodules
• Angular stomatitis especially seen in the palate
• Papillary hyperplasia in the vault of the palate. • Squamous cell carcinomas
• Wegener’s granulomatosis.
Classification
Denture-related stomatitis has been classified into Vascular anomalies (angiomas and
three clinical types (Newton’s types), increasing in telangiectasia) include:
severity: • Dilated lingual veins (varices) may be
• A localised simple inflammation or a pinpoint conspicuous in normal elderly persons
hyperaemia (Type I) • Haemangiomas are usually small isolated Keypoints for patients:
• An erythematous or generalised simple type pre- developmental anomalies, or hamartomas Geographic tongue
senting as more diffuse erythema involving part (Figs 7-9) • This is a common condition
of or the entire, denture-covered mucosa (Type II) • Telangiectasias — dilated capillaries — may • The cause is unknown
• A granular type (inflammatory papillary be seen after irradiation and in disorders • It may be inherited from parents
hyperplasia) commonly involving the central such as hereditary haemorrhagic telangiec- • There may be an allergic
part of the hard palate and the alveolar ridge tasia and systemic sclerosis (Fig. 10) component
(Type III). • Angiomas are benign and usually congenital • It is not thought to be infectious
(Figs 7-10). In general most do not require any • It is associated, rarely, with
Diagnosis active treatment unless symptoms develop, in psoriasis
Denture-related stomatitis is a clinical diagnosis which case they can be treated by injection of • It has no long-term consequences
although it may be confirmed by microbiological sclerosing agents, cryosurgery, laser excision
investigations. In addition haematological and or surgical excision. Keypoints for dentists:
biochemical investigations may be appropriate to Geographic tongue
identify any underlying predisposing factors such Vesiculobullous disorders • The cause is unknown but it may be
as nutritional deficiencies, anaemia and diabetes Erythema multiforme, pemphigoid and pem- inherited
mellitus in patients unresponsive to conventional phigus may present as red lesions (see article • It resembles, and is associated
management. two), especially localised oral purpura, which rarely with, psoriasis
presents with blood blisters (Fig. 11). Specialist • It has no long-term consequences
Management referral is usually indicated. • There is no cure and treatment and
The denture plaque and fitting surface is infested is therefore aimed at controlling
with micro-organisms, most commonly Candida Reactive lesions symptoms and reassuring the
patient
albicans and therefore, to prevent recurrence, Reactive lesions that can be red are usually per-
BRITISH DENTAL JOURNAL VOLUME 199 NO. 10 NOV 26 2005 641
PRACTICE
Keypoints for dentists:
Single hyperpigmented lesions
• If the lesion could be an amalgam
tattoo, take a radiograph
• If the lesion is radio-opaque, it is
probably a tattoo and should be
left alone
• If the lesion is not radio-opaque, or
if it was not initially considered
likely to be an amalgam tattoo,
biopsy it
Fig. 7 Vascular hamartoma (haemangioma) tongue Fig. 12 Pyogenic granuloma, lower lip
Fig. 8 Vascular hamartoma (haemangioma, palate) Fig. 13 Pyogenic epulis
sistent soft lumps (Figs 12 and 13) which include:
• Pyogenic granulomas
• Peripheral giant cell granulomas
Specialist referral is usually indicated.
Atrophic lesions
The most important red lesion is erythroplasia,
since it is often dysplastic (see below). Geographic
tongue also causes red lesions (see above),
desquamative gingivitis is a frequent cause of red
Fig. 9 Haemangioma in floor of mouth gingivae, almost invariably caused by lichen
planus or pemphigoid, and iron or vitamin defi-
ciency states may cause glossitis (Fig. 14) or other
red lesions.
ERYTHROPLAKIA (ERYTHROPLASIA)
Erythroplasia is a rare condition defined as ‘any
lesion of the oral mucosa that presents as bright
red velvety plaques which cannot be charac-
terised clinically or pathologically as any other
recognisable condition’.
Mainly seen in elderly males, it is far less com-
mon than leukoplakia, but far more likely to be
dysplastic or undergo malignant transformation.
Fig. 10 Telangiectasia, lips and tongue
Clinical features
Erythroplakia is seen most commonly on the soft
palate, floor or mouth or buccal mucosa. Some
erythroplakias are associated with white patches,
and are then termed speckled leukoplakia (Fig. 15).
Diagnosis
Biopsy to assess the degree of epithelial dysplasia
and exclude a diagnosis of carcinoma.
Prognosis
Erythroplasia has areas of dysplasia, carcinoma
Fig. 11 Angina bullosa haemorrhagica in situ, or invasive carcinoma in most cases.
642 BRITISH DENTAL JOURNAL VOLUME 199 NO. 10 NOV 26 2005
PRACTICE
deficiencies. Other investigations needed may
include other haematological tests and/or biop-
sy or imaging.
Management
Treatment is usually of the underlying cause, or
surgery.
HYPERPIGMENTATION
Oral mucosal discolouration may be superficial
(extrinsic) or due to deep (intrinsic — in or
Fig. 14 beneath mucosa) causes and ranges from brown
Atrophic glossitis
to black.
Extrinsic discolouration is rarely of conse-
quence and is usually caused by:
• Habits such as tobacco or betel use
• Coloured foods or drinks, (such as liquorice,
beetroot, red wine, coffee, tea)
• Drugs (such as chlorhexidine, iron salts, crack
cocaine, minocycline, bismuth subsalicylate,
and lansoprazole).
Fig. 15 Erythroplasia in soft palate complex
Carcinomas are seen 17 times more often in
erythroplakia than in leukoplakia and these are
therefore the most potentially malignant of all
oral mucosal lesions.
Management
Erythroplastic lesions are usually (at least 85%) Fig. 16 Black hairy tongue
severely dysplastic or frankly malignant. Any
causal factor such as tobacco use should be Black hairy tongue
stopped, and lesions removed. There is no hard This is one extrinsic type of discolouration seen
evidence as to the ideal frequency of follow-up, especially in patients on a soft diet, smokers, and
but it has been suggested that patients with those with dry mouth or poor oral hygiene (Fig.
mucosal potentially malignant lesions be re- 16).
examined within one month, at three months, at The best that can usually be done is to avoid
six months, at 12 months and annually thereafter. the cause where known, and to advise the patient
to brush the tongue or use a tongue-scraper.
PURPURA
This presents as bleeding into the skin and Intrinsic discolouration
mucosa and is usually caused by trauma. Occa- This may have much more significance (Table 3).
sional small petechiae are seen at the occlusal Localised areas of pigmentation may be caused
line in perfectly healthy people. mainly by:
Thrombocytopenia can result in red or • Amalgam tattoo (embedded amalgam). Typi-
brown pinpoint lesions (petechiae) or diffuse cally this is a single blue-black macule in the
bruising (ecchymoses) at sites of trauma, such
as the palate. Suction (eg fellatio) may produce Table 3 Main causes of intrinsic mucosal
hyperpigmentation
bruising in the soft palate). Localised oral pur-
pura or angina bullosa haemorrhagica is an Localised
idiopathic, fairly common cause of blood blis- • Amalgam or other tattoo
ters, often in the soft palate, in older persons • Naevus
(Fig. 11). Sometimes the use of a corticosteroid • Melanotic macule
inhaler precipitates this. • Neoplasms (eg malignant melanoma or Kaposi’s sarcoma)
• Pigmentary incontinence
• Peutz-Jegher’s syndrome
Diagnosis of red lesions
Diagnosis of red lesions is mainly clinical but Generalised
lesions should also be sought elsewhere, espe- • Racial pigmentation
• Localised irritation, eg tobacco or betel
cially on the skin or other mucosae.
• Drugs, eg antimalarials
It may be necessary to take a blood picture
• Pregnancy/oral contraceptive pill
(including blood and platelet count), and assess
• Addison’s disease (hypoadrenocorticism)
haemostatic function or exclude haematinic
BRITISH DENTAL JOURNAL VOLUME 199 NO. 10 NOV 26 2005 643
PRACTICE
is not radio-opaque, it is best biopsied to
exclude naevi or melanoma. Similar lesions
can be caused by other foreign bodies (eg
graphite tattoo), local irritation or inflamma-
tion.
• Naevi are blue-black often papular lesions
formed from increased melanin-containing
cells (naevus cells) seen particularly on the
palate. They are best removed to exclude
Fig. 17 Amalgam tattoo melanoma.
• Pigmentary incontinence may be seen in some
inflammatory lesions such as lichen planus,
especially in smokers (Fig. 20).
• Melanotic macules are usually flat single
brown, collections of melanin-containing
cells, seen particularly on the vermilion bor-
der of the lip and on the palate (Fig.
19). They are best removed to exclude
Fig. 18 Amalgam tattoo melanoma.
• Malignant melanoma is rare, seen usually in
the palate or maxillary gingivae. Features
suggestive of malignancy include a rapid
increase in size, change in colour, ulcera-
tion, pain, the occurrence of satellite pig-
mented spots or regional lymph node
enlargement. Incisional biopsy to confirm
the diagnosis followed by radical excision is
indicated.
Fig. 19 Melanotic macule, lower
labial mucosa • Kaposi’s sarcoma is usually a purple lesion seen
mainly in the palate or gingival of HIV-infected
and other immunocompromised persons.
Generalised pigmentation, often mainly
affecting the gingivae, is common in persons
of colour, and is racial and due to melanin.
Seen mainly in black and ethnic minority
groups it can also be noted in some fairly
light-skinned people (Fig. 21). Such pigmenta-
tion may be first noted by the patient in adult
Fig. 20 Smoking-induced melanosis,
buccal mucosa
life and then incorrectly assumed to be
acquired.
In all other patients with widespread intrinsic
pigmentation, systemic causes should be exclud-
ed. These may include:
• Tobacco, which can also cause intrinsic hyper-
pigmentation (smoker’s melanosis)
• Antimalarials, oral contraceptive pill, anticon-
vulsants, minocycline, phenothiazines, gold,
busulphan and other drugs
• Heavy metals (such as mercury, lead and bis-
muth) not used therapeutically now, rarely
Fig. 21 Racial pigmentation cause industrial exposure etc
• Pregnancy
mandibular gingiva close to the scar of an • Hypoadrenalism (Addison’s disease). Hyper-
apicectomy (Figs 17 and 18) or where amal- pigmentation in this is generalised but most
gam has accidentally been introduced into a obvious in normally pigmented areas (eg
wound, is painless, and does not change in the nipples, genitalia), skin flexures, and
size or colour. A lesion suspected to be an sites of trauma. The mouth may show
amalgam tattoo is best radiographed first to patchy hyperpigmentation. Patients also
see if there is radio-opaque material present, typically have weakness, weight loss, and
though not all are radio-opaque. If the lesion hypotension.
644 BRITISH DENTAL JOURNAL VOLUME 199 NO. 10 NOV 26 2005
PRACTICE
Diagnosis melanomas is to be achieved, all pigmented
Patients to refer
The nature of oral hyperpigmentation can oral cavity lesions should be viewed with
Erythroplasia/erythroplakia — in
sometimes only be established after further suspicion. The consensus of opinion is that
view of high risk of malignant
investigation. a lesion with clinical features as above transformation
In patients with localised hyperpigmenta- seriously suggestive of malignant melanoma, Squamous carcinoma
tion, in order to exclude melanoma, are best biopsied at the time of definitive
Isolated brown or black lesions of
radiographs may be helpful (they can some- operation. suspect aetiology
times show a foreign body) and biopsy may be In patients with generalised or multiple Generalised or multiple
indicated, particularly where there is a hyperpigmentation, specialist referral is hyperpigmentation
solitary raised lesion, a rapid increase in size, indicated. Kaposi’s sarcoma
change in colour, ulceration, pain, evidence of Wegener’s granulomatosis in view
satellite pigmented spots or regional lymph Management of associated systemic disease
node enlargement. If early detection of oral Management is of the underlying condition.
BRITISH DENTAL JOURNAL VOLUME 199 NO. 10 NOV 26 2005 645
You might also like
- Fungal Diseases of The Oral MucosaDocument5 pagesFungal Diseases of The Oral MucosaManar AlsoltanNo ratings yet
- HEAD AND NECK 1.robbins & Cotran Pathologic Basis of Disease ReviewerDocument14 pagesHEAD AND NECK 1.robbins & Cotran Pathologic Basis of Disease ReviewerSeff Causapin100% (1)
- ++OSCE Mock Exam With Answers Final PDFDocument129 pages++OSCE Mock Exam With Answers Final PDFPayal Jain80% (5)
- Tongue Lession PrintDocument9 pagesTongue Lession Printdlami_ahNo ratings yet
- Gi Pathology - Block 3 ReviewDocument34 pagesGi Pathology - Block 3 ReviewMatt McGlothlin100% (1)
- Anatomy of Oral Cavity and Common DisordersDocument24 pagesAnatomy of Oral Cavity and Common DisordersMuhammad SalmanNo ratings yet
- LeukoplakiaDocument60 pagesLeukoplakiadimasahadiantoNo ratings yet
- A Guide To Clinical Differential Diagnosis of Oral Mucosal LesionDocument46 pagesA Guide To Clinical Differential Diagnosis of Oral Mucosal LesionFasmiya ShariffNo ratings yet
- Epidemiology, Etiology & Prevention of Oral CancerDocument52 pagesEpidemiology, Etiology & Prevention of Oral CancerValsala Uday100% (1)
- Oral MedicineDocument136 pagesOral Medicineganang19No ratings yet
- Oral Medicine & Pathology from A-ZFrom EverandOral Medicine & Pathology from A-ZRating: 5 out of 5 stars5/5 (9)
- Oral Maxillofacial Pathology NotesDocument18 pagesOral Maxillofacial Pathology NotesJose TeeNo ratings yet
- A Simple Guide to Bad Breath and Mouth DiseasesFrom EverandA Simple Guide to Bad Breath and Mouth DiseasesRating: 5 out of 5 stars5/5 (3)
- Lesions of Oral CavityDocument43 pagesLesions of Oral CavityDawood NasserNo ratings yet
- Variasi Normal Rongga MulutDocument18 pagesVariasi Normal Rongga MulutRafi Kusuma Ramdhan SukonoNo ratings yet
- Oral and Maxillofacial Medicine The Basi PDFDocument436 pagesOral and Maxillofacial Medicine The Basi PDFNimas Putri100% (2)
- Oral Candidiasis - ReviewDocument9 pagesOral Candidiasis - ReviewAdhelia Galuh PrmtsrNo ratings yet
- Dermatology Mini-OSCEDocument322 pagesDermatology Mini-OSCEMarrkNo ratings yet
- Premalignant Lesions and Conditions: Submitted by-BALJEET KAUR B.D.S.-3 Year Roll No.15Document60 pagesPremalignant Lesions and Conditions: Submitted by-BALJEET KAUR B.D.S.-3 Year Roll No.15Rajat NangiaNo ratings yet
- Premalignant Lesions & ConditionsDocument76 pagesPremalignant Lesions & ConditionsAman KankariaNo ratings yet
- Tobacco-Associated Oral LesionsDocument48 pagesTobacco-Associated Oral LesionsSamridhi Srivastava100% (1)
- Oral Medicine - Update For The Dental PractitionerDocument8 pagesOral Medicine - Update For The Dental PractitionernavyaNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument63 pagesOral Medicine - Update For The Dental PractitionerPhuong MaiphuongNo ratings yet
- Oral Ulcers 1Document6 pagesOral Ulcers 1Khushbu MehtaNo ratings yet
- Red Lesions of Oral Cavity A ReviewDocument6 pagesRed Lesions of Oral Cavity A ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 734common Oral Diseases Final - 4Document22 pages734common Oral Diseases Final - 4Mahmoud HassanNo ratings yet
- Mouth Ulcers and Diseases of The Oral Cavity: Key PointsDocument7 pagesMouth Ulcers and Diseases of The Oral Cavity: Key PointsAimen ZahidNo ratings yet
- Steroid Inhaler Therapy and Oral Manifestation Similar To Median Rhomboid GlossitisDocument3 pagesSteroid Inhaler Therapy and Oral Manifestation Similar To Median Rhomboid GlossitisRochmahAiNurNo ratings yet
- Oral UlcerationDocument10 pagesOral Ulcerationمحمد حسنNo ratings yet
- Oral UlcerationDocument29 pagesOral UlcerationMINI DHABANo ratings yet
- Oral Medicine: (I. Penyakit Mulut)Document178 pagesOral Medicine: (I. Penyakit Mulut)claudiaciwiNo ratings yet
- 16-9+oropharyngeal CandidiasisDocument45 pages16-9+oropharyngeal CandidiasisشيماءNo ratings yet
- Clinical Oral Medicine Lecture NotesDocument3 pagesClinical Oral Medicine Lecture NotesDrMurali G ManoharanNo ratings yet
- Manchas Blancas y RojasDocument16 pagesManchas Blancas y RojasJosué Zuriel OrtizNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument3 pagesOral Medicine - Update For The Dental PractitionerGowriNo ratings yet
- 3 Benign Inflammatory LesionsDocument8 pages3 Benign Inflammatory LesionsalbaablyNo ratings yet
- Stomatitis. Aetiology and A Review. Part 2. Oral Diseases Caused Candida SpeciesDocument7 pagesStomatitis. Aetiology and A Review. Part 2. Oral Diseases Caused Candida SpeciesIzzahalnabilah_26No ratings yet
- Oral Medicine: (I. Penyakit Mulut)Document165 pagesOral Medicine: (I. Penyakit Mulut)Susanna Arie KNo ratings yet
- File - Penyakit Mukosa Pediatric 2022 - 732dceb5Document45 pagesFile - Penyakit Mukosa Pediatric 2022 - 732dceb5AZZAHRA KARYA BULAN IRIANDANo ratings yet
- Johnston - Good STM Summary - 2012Document5 pagesJohnston - Good STM Summary - 2012RONALDO CANDRA WIJAYANo ratings yet
- Oral Patho Lecture Shlav BDocument65 pagesOral Patho Lecture Shlav Bشبيبةالروم الملكيين الكاثوليكNo ratings yet
- 39 Ahmed EtalDocument6 pages39 Ahmed EtaleditorijmrhsNo ratings yet
- A Clinical Approach White LesionDocument5 pagesA Clinical Approach White LesionTirta KusumaNo ratings yet
- Benign Migratory Glossitis A Rare Presentation of A Common DisorderDocument3 pagesBenign Migratory Glossitis A Rare Presentation of A Common DisorderOjanNo ratings yet
- Diseases of The Lips & TongueDocument25 pagesDiseases of The Lips & Tongueshahlaraib001No ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument3 pagesOral Medicine - Update For The Dental PractitionerMugiNo ratings yet
- Developmental Disturbances - Dr. Nermine El BaheyDocument11 pagesDevelopmental Disturbances - Dr. Nermine El BaheyMOHAMED AMINNo ratings yet
- Oral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of SalivationDocument5 pagesOral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of SalivationGowriNo ratings yet
- Desquamative GingivitisDocument6 pagesDesquamative Gingivitissidra malikNo ratings yet
- Approach To Oral LesionsDocument53 pagesApproach To Oral LesionsUmut YücelNo ratings yet
- Oral DiseasesDocument4 pagesOral DiseasesAlphonse ElricNo ratings yet
- S Tomato LogyDocument3 pagesS Tomato LogyAjay The RockerNo ratings yet
- COLGATE Oral - Lesions - BookDocument89 pagesCOLGATE Oral - Lesions - BookVijetha RaiNo ratings yet
- Tongue Diseases NDocument46 pagesTongue Diseases NhazeemmegahedNo ratings yet
- Oral Frictional HyperkeratosisDocument15 pagesOral Frictional HyperkeratosisFajarRahmantiyoNo ratings yet
- Management of Patients With Oral and Esophageal DisordersDocument81 pagesManagement of Patients With Oral and Esophageal DisordersEdmond ChanNo ratings yet
- Tongue DisordersDocument2 pagesTongue Disordersluke swanepoelNo ratings yet
- Oral Findings in Secondary Syphilis: Zela Puteri Nurbani 1506668694Document15 pagesOral Findings in Secondary Syphilis: Zela Puteri Nurbani 1506668694adnanfananiNo ratings yet
- Dental Medicine 5Document4 pagesDental Medicine 5Vincent Luigil AlceraNo ratings yet
- 2 Diseases of Tongue Lips PDFDocument17 pages2 Diseases of Tongue Lips PDFmarianaffernandes10No ratings yet
- Tonguedisorders 150616104030 Lva1 App6892Document34 pagesTonguedisorders 150616104030 Lva1 App6892Mohan VeerabomalaNo ratings yet
- DD of TeethDocument53 pagesDD of TeethRanjit DanielNo ratings yet
- Oral Diagnosis and Treatment Planning IIDocument19 pagesOral Diagnosis and Treatment Planning IIAIME WILFRIED BEASSO FOZOCKNo ratings yet
- Review Article: Oral Ulceration - Aetiopathogenesis, Clinical Diagnosis and Management in The Gastrointestinal ClinicDocument14 pagesReview Article: Oral Ulceration - Aetiopathogenesis, Clinical Diagnosis and Management in The Gastrointestinal ClinicAmira KaddouNo ratings yet
- Oral Erythroplakia - A Case Report: Mahendra Patait, Urvashi Nikate, Kedar Saraf, Priyanka Singh and Vishal JadhavDocument4 pagesOral Erythroplakia - A Case Report: Mahendra Patait, Urvashi Nikate, Kedar Saraf, Priyanka Singh and Vishal JadhavhelmysiswantoNo ratings yet
- Oral Manifestations of Systemic Disease: Autoimmune DiseasesDocument7 pagesOral Manifestations of Systemic Disease: Autoimmune DiseaseshussainNo ratings yet
- Applied Sciences: The Pseudolesions of The Oral Mucosa: Di Diagnosis and Related Systemic ConditionsDocument8 pagesApplied Sciences: The Pseudolesions of The Oral Mucosa: Di Diagnosis and Related Systemic Conditionssiti baiq gadishaNo ratings yet
- Fissured Tongue: A Case Report and Review of Literature: KeywordsDocument5 pagesFissured Tongue: A Case Report and Review of Literature: Keywordssiti baiq gadishaNo ratings yet
- Acute Gingival LesionsDocument70 pagesAcute Gingival LesionsIesha Crawford100% (1)
- Gingival and Periodontal Problems in ChildrenDocument19 pagesGingival and Periodontal Problems in Childrenallakami777yousefNo ratings yet
- Verrucous Carcinoma Ackerman'sDocument3 pagesVerrucous Carcinoma Ackerman'sdarsunaddictedNo ratings yet
- Oral CancerDocument29 pagesOral CancerBijen LangpoklakpamNo ratings yet
- LeukoplakiaDocument12 pagesLeukoplakiaPrashant PuranikNo ratings yet
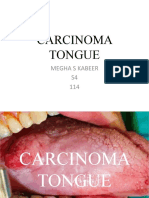
- 33) Carcinoma TongueDocument50 pages33) Carcinoma TongueMariam AntonyNo ratings yet
- Orallesions ClassificationDocument18 pagesOrallesions ClassificationRaj ChauhanNo ratings yet
- Exam 2017 Questions and AnswersDocument10 pagesExam 2017 Questions and AnswersKen LeeNo ratings yet
- Laryngeal DysplasiaDocument7 pagesLaryngeal DysplasiakarimahihdaNo ratings yet
- Lip CancerDocument4 pagesLip CancerSaman SadeghiNo ratings yet
- Peraturan Bpjs Poli GigiDocument11 pagesPeraturan Bpjs Poli GigitarikusumaNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument8 pagesOral Medicine - Update For The Dental PractitionerMugiNo ratings yet
- Mu CosaDocument222 pagesMu CosaAliImadAlKhasakiNo ratings yet
- Leukoplakia 170519204224Document27 pagesLeukoplakia 170519204224Mihai SemeniucNo ratings yet
- Jurnal OpmdDocument24 pagesJurnal OpmdQinthara NurichsanNo ratings yet
- Oral Manifestations of Systemic DiseasesDocument14 pagesOral Manifestations of Systemic Diseasesshygal1981No ratings yet
- 3 RfajDocument81 pages3 RfajSheikhaNo ratings yet
- Betel Nut Chewing and Its Deleterious Effects On Oral CavityDocument7 pagesBetel Nut Chewing and Its Deleterious Effects On Oral Cavitydwi fitrahNo ratings yet
- Target - Online Exam - Oral Pathology Medicine RadiologyDocument58 pagesTarget - Online Exam - Oral Pathology Medicine RadiologyplsssssNo ratings yet
- Alimentary Tract Pathology LGL 1 Oral and Salivary (WPS)Document68 pagesAlimentary Tract Pathology LGL 1 Oral and Salivary (WPS)jwan ahmedNo ratings yet