Professional Documents
Culture Documents
Posturologia 3
Uploaded by
Alberto Jesús CamposOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Posturologia 3
Uploaded by
Alberto Jesús CamposCopyright:
Available Formats
RESEARCH ARTICLE
Do different dental conditions influence the
static plantar pressure and stabilometry in
young adults?
Elena Amaricai1☯, Roxana Ramona Onofrei ID1*, Oana Suciu ID1☯, Corina Marcauteanu2☯,
Eniko Tunde Stoica2☯, Meda Lavinia Negruțiu3☯, Vlad Laurentiu David4, Cosmin Sinescu3
1 Department of Rehabilitation, Physical Medicine and Rheumatology, “Victor Babes” University of Medicine
and Pharmacy, Timisoara, Romania, 2 Department of Occlusiology, Faculty of Dentistry, “Victor Babes”
University of Medicine and Pharmacy, Timisoara, Romania, 3 Dental Materials and Dental Prosthesis
Department, Faculty of Dentistry, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania,
4 Department of Pediatric Surgery and Orthopedics, “Victor Babes” University of Medicine and Pharmacy,
a1111111111 Timisoara, Romania
a1111111111 ☯ These authors contributed equally to this work.
a1111111111 * onofrei.roxana@umft.ro
a1111111111
a1111111111
Abstract
OPEN ACCESS Background
Citation: Amaricai E, Onofrei RR, Suciu O, Posture is influenced by many factors and dental occlusion seems to have its role on pos-
Marcauteanu C, Stoica ET, Negruțiu ML, et al. tural stabilization. Our rationale to perform the study was to find out if there are differences
(2020) Do different dental conditions influence the
of static plantar pressure and stabilometric parameters depending on different dental
static plantar pressure and stabilometry in young
adults? PLoS ONE 15(2): e0228816. https://doi. conditions.
org/10.1371/journal.pone.0228816
Editor: Jean L. McCrory, West Virginia University, Methods
UNITED STATES The observational study consisted in plantar pressure assessment and stabilometric analy-
Received: August 23, 2019 sis of 95 right-handed healthy volunteer subjects (mean age 22.94 ± 2.52 years) by using
Accepted: January 23, 2020 the PoData system. Each subject followed four measurements with open eyes: mandibular
postural position, maximum intercuspation, biting on cotton rolls and maximum mouth open-
Published: February 11, 2020
ing. Plantar pressure was recorded on 1st and 5th metatarsal heads and heel, and was
Copyright: © 2020 Amaricai et al. This is an open
expressed as percentage of weight distribution on each foot. The recorded centre of pres-
access article distributed under the terms of the
Creative Commons Attribution License, which sure (CoP) parameters were: CoP path length, 90%confidence ellipse area and maximum
permits unrestricted use, distribution, and CoP speed. Statistical analysis used repeated-measures ANOVA with Bonferroni posthoc
reproduction in any medium, provided the original analysis and Friedman test.
author and source are credited.
Data Availability Statement: All relevant data used Results
in this study are held in Figshare (https://doi.org/
10.6084/m9.figshare.9724244.v1). Loading on the left 5th metatarsal head was significantly higher in maximum mouth opening
condition when compared to maximum intercuspation and to biting on cotton rolls. The left
Funding: The publishing fee has been funded by
the ”Victor Babes” University of Medicine and heel loading was significantly lower in the maximum mouth opening in comparison to maxi-
Pharmacy Timisoara, Romania. mum intercuspation. The CoP path length and maximum CoP speed were significantly
Competing interests: The authors have declared higher in maximum mouth opening compared to the other three conditions. Confidence
that no competing interests exist. ellipse area had significantly lower values in maximum intercuspation and in the biting on
PLOS ONE | https://doi.org/10.1371/journal.pone.0228816 February 11, 2020 1 / 10
Static plantar pressure and stabilometry
cotton rolls conditions compared to the mandibular postural position, and in maximum inter-
cuspation compared to maximum mouth opening.
Conclusion
In young adults with an optimum functional occlusion the static plantar pressure is influ-
enced by the maximum mouth opening. An improved postural stability was recorded in max-
imum intercuspation (a condition used during swallowing) in comparison to mandibular
postural position (a condition that allows relaxation of the masticatory muscles after func-
tional moments).
Introduction
The posture is influenced by many factors, while dental occlusion seems to have its role on
postural stabilization [1]. Many reviews have analysed the influence of dental occlusion on
body balance, focusing on the neuroanatomical interconnections between the trigeminal and
vestibular nuclei, and on the muscular interconnections implying influences between the mas-
ticatory and the postural muscles. Moon and Lee showed that dental occlusion influences
body-stabilizing activities such as body equilibrium and gravity fluctuation [2]. The review of
Cuccia and Caradonna also suggested that there are correlations between posture and the sto-
matognathic system [3]. Moreover, changes of different jaws relations also have effect on pos-
tural stability [4]. A more recent study (2013) demonstrated a weak correlation between
mandibular position and body posture in healthy subjects [5].
In contrast with the previous findings, the review of Manfredini D. et al. showed that there
is no evidence for the existence of a predictable relationship between occlusal and postural fea-
tures [6]. The review of Perinetti G. from 2013 analysed 11 studies regarding the effects of
mandibular position on body sway. The results were different, but the general conclusion was
that the mandibular position does not appear to be correlated to body sway at a clinically sig-
nificant level [7]. Another overview stated that it is not recommended to perform occlusal
treatment in order to treat or prevent postural imbalances or alteration of spine curvatures [8].
The study of Perinetti G. from 2006 showed no detectable correlation at the posturography
level between dental occlusion and body posture. However, the existence of a correlation
between these structures cannot be denied [9].
In spite of these contrasting results, a recent review of Julia-Sanchez S. et al. (2019) stated
that more studies are needed to elucidate the mechanisms by which dental occlusion may
influence balance control. The main conclusion of this review was that dental occlusion con-
tributes to balance control when there are external perturbations such as unstable support sur-
face or during performing unipedal or bipedal tasks [10].
The relationship between dental occlusion and posture was also studied in subjects with
temporo-mandibular disorders, as well as in physically well-trained or sporty subjects. The
study of Nota A. et al. demonstrated a significant difference in body postural stability between
subjects with myogenous temporo-mandibular disorders and healthy controls, with increased
sway area and sway velocity postural parameters in the first group [11]. Dental occlusion can
influence posture in air force and civilian pilots [12], while repercussion of dental occlusion
upon posture stabilization is suggested in the high level shooters [13].
Our rationale to perform the current study was to find out if there are differences of static
plantar pressure and stabilometric parameters depending on different dental conditions. To
PLOS ONE | https://doi.org/10.1371/journal.pone.0228816 February 11, 2020 2 / 10
Static plantar pressure and stabilometry
our knowledge there are no studies that compared the distribution of the plantar pressure on
the right and left foot, as well as the three weight distribution sites of each foot (1st and 5th
metatarsal heads, and calcaneus) in relation with dental occlusion.
The objective of our study was to analyse the distribution of static plantar pressure and sta-
bilometric parameters in relation to different dental conditions in healthy young adults.
Material and methods
Subjects
One hundred twenty-eight healthy volunteer subjects were asked to participate in the study.
They were recruited among the graduates of our university, their friends, relatives or acquain-
tances. The sample size was calculated using G� Power software version 3.1.9.2. For α = 0.05, β
= 0.2, a medium effect size (f = 0.25), with four measurements, a sample size of at least 94 sub-
jects would be required [14].
The subjects included in this study underwent a detailed anamnesis and a thorough extra-
oral and intraoral examination. The inclusion criteria were: age over 18 years; presence of at
least 28 teeth, with no large occlusal restorations (the composite and/or amalgam fillings satis-
fied the criteria of an optimum functional occlusion according to Okeson [15]); class I interin-
cisal relationships (with an overbite of 2–4 mm and an overjet of 1–2 mm); correct Angle’s key
on both sides. The exclusion criteria were: foot disorders; spinal deviations; myogenous or
arthrogenous temporo-mandibular disorders; trauma or surgery that can influence posture;
history of neurological diseases, vestibular or visual disturbances or any other pathology that
would influence posture; any type of crossbite, open bite or deep bite; extensive occlusal resto-
rations through either large fillings or fixed partial dentures. The TMD patients were excluded
from this study because of the significant difference in body posture between subjects with
TMD and healthy controls [11].
Participation in the study was voluntary. Written informed consent was obtained from all
the subjects. The study has been carried out in accordance with the Declaration of Helsinki
and was approved by Institutional Ethics Committee (no 23/2019).
Assessments
PoData system (Chinesport, Udine, Italy) was used for plantar pressure assessment and stabi-
lometric analysis. The PoData is a capacitive pressure distribution system with an integrated
podoscope and six load cells. The data are recorded at a sampling frequency of 100 Hz and
analysed by the provided GPS5 software. We followed the manufacturer’s instructions, per-
forming an initial no-load calibration of the platform. The six virtual sensors were set after the
subjects step up on the platform, corresponding to the 1st and 5th metatarsal heads and heel, in
both right and left foot [16]. The system provides information about weight distribution, bary-
centre and stabilometry [17].
The subjects were asked to stand on the platform, barefoot, in upright posture, lower limbs
extended and arms positioned naturally along their sides. The feet were positioned at an angle
of 30˚ to each other and 5 cm between the heels [18].
They were instructed to look ahead, fixing a target point on the wall, not to talk or move (S1
Fig). Measurements of plantar pressure and stabilometry were performed for each subject
under the following conditions, with open eyes: mandibular postural position (the position of
the mandible when an individual is resting comfortably in an upright position, with the con-
dyles in a neutral, unstrained position in the glenoid fossae and the associated muscles are in a
state of minimal contractual activity [19]), maximum intercuspation (optimum occlusal stabi-
lization), biting on three 8-mm cotton rolls placed between the opposing teeth at the level of
PLOS ONE | https://doi.org/10.1371/journal.pone.0228816 February 11, 2020 3 / 10
Static plantar pressure and stabilometry
the 1st molars and central incisors, and maximum mouth opening. The mandibular postural
position is characterized by a balance between the tonus of the mandibular elevator muscles
and the tonus of the mandibular depressor muscles; it is maintained by the intervention of the
myotactic reflex and is adopted by the mandible after swallowing saliva [15]. The postural posi-
tion of the mandible was confirmed by the following issues: the patient‘s lips were touching
lightly and effortlessly; the postural vertical dimension (measured between subnasale and
gnathion with the Willis bite gauge) was equal to the distance between the corner of the mouth
and the external angle of the eye; there was a space of 2–4 mm between the opposing dental
arches (freeway space). Each recording had duration of 20 seconds. The evaluations were per-
formed by the same experienced investigator. The testing was considered invalid and repeated
if at least one of the following errors were observed: the subject moved or lifted an arm or
both, lifting the forefoot or the heel, falling out of position, moving the head or talking.
Plantar pressure was recorded on three anatomical regions: 1st and 5th metatarsal heads and
heel, in both right and left foot [20]. Percentage of body weight distribution was calculated for
each area. An ideal load of an ideal subject has the following distribution: 1/6 (16.7%) of total
weight on 5th metatarsal head, 2/6 (33.33%) of total weight on 1st metatarsal head, and 3/6
(50%) of total weight on calcaneus, for the right and the left foot, respectively [17].
The measured body centre of pressure (CoP) was compared with the theoretical one
[21,22]. Body centre of pressure deviation from theoretical reference was measured on ante-
rior-posterior (CoPY) and latero-lateral (CoPX) axes [17,21,23]. Average distances from ideal
barycentre were provided by the software for both axes. A positive value represents an anterior
deviation on the anterior-posterior axis, and a right deviation on the latero-lateral axis. Based
on these deviations, the absolute mean CoP displacement from the ideal position was calcu-
lated [9]. Other CoP parameters analysed in this study were the CoP path length, the 90% con-
fidence ellipse area and the maximum CoP speed, as recommended by Nagymate and Kiss
[24]. The CoP path length is the length in millimetres of the subject’s centre of gravity shift
during the test. Confidence ellipse area is the area in mm2 of the ellipse that includes all the
centre of gravity points measured and transferred on a system of Cartesian axes with a confi-
dence level of 90%. Maximum CoP speed is the average centre of gravity shifting maximum
speed in millimetres per second.
Statistical analysis
Statistical analysis was performed using MedCalc version 8.11 (MedCalc Software bvba, Ost-
end, Belgium). Data were tested for normality with the Shapiro-Wilk test, and presented as
mean and standard deviation for normal distributed data, and as median and interquartile
range for non-normally distributed data. Differences in weight distribution and stabilometric
Table 1. Subjects’ demographic characteristics.
Variables
Age, years (mean ± SD) 22.94 ± 2.52
Gender
Male, n (%) 29 (30.5)
Female, n (%) 66 (69.5)
Weight, kg (mean ± SD) 64.17 ± 12.51
Height, cm (mean ± SD) 168.02 ± 8.23
BMI (mean ± SD) 22.61 ± 3.71
n: number of subjects; SD: standard deviation; BMI: body mass index.
https://doi.org/10.1371/journal.pone.0228816.t001
PLOS ONE | https://doi.org/10.1371/journal.pone.0228816 February 11, 2020 4 / 10
Static plantar pressure and stabilometry
parameters among the four conditions were assessed using the repeated-measures ANOVA
with a Bonferroni posthoc analysis and a Friedman test, respectively. Statistical significance
was set p<0.05 for all tests.
Results
Ninety-five subjects (66 females and 29 males, mean age 22.94 ± 2.52 years) met the inclusion
criteria and their data were analysed. The demographic characteristics are presented in
Table 1. All the subjects were right-handed.
The weight distributions in all the testing conditions are presented in Table 2. Significant
main effects of the conditions were found for the left 5th metatarsal head (F3,282 = 4.26,
p = 0.006) and left heel weight distribution (F3,282 = 3.72, p = 0.011). Posthoc analysis showed
that loading on the left 5th metatarsal head was significantly higher in the maximum mouth
opening condition when compared to maximum intercuspation (p = 0.003) and to biting on
cotton rolls (p = 0.04). The left heel loading was significantly lower in the maximum mouth
opening condition in comparison to maximum intercuspation (p = 0.003).
The stabilometric data are presented in Table 3 and Fig 1A–1D. Significant main effects of
the conditions were observed for CoP path length (F3,282 = 7.07, p = 0.0001), 90% confidence
ellipse area (F3,282 = 5.36, p = 0.001) and maximum CoP speed (F3,282 = 4.55, p = 0.003). The
CoP path length was significantly higher in maximum mouth opening compared to all the
other conditions (p<0.05). This parameter was significantly lower in maximum intercuspation
compared to the mandibular postural position (p<0.05). When recording the 90% confidence
ellipse area we noticed that it had significantly lower values in maximum intercuspation and in
the biting on cotton rolls conditions compared to the mandibular postural position (p<0.05),
and in maximum intercuspation compared to maximum mouth opening (p<0.05). The maxi-
mum CoP speed was significantly greater in maximum mouth opening compared to the other
three conditions (p<0.05). The CoP displacement did not differ significantly across
conditions.
Discussions
The current study aimed to investigate the static plantar pressure and stabilometry in relation
to different dental conditions. We assessed young adults with an optimum functional occlu-
sion according to Okeson [15].
The novelty of our study is represented by the fact that it assessed the static plantar pressure
distributed on the 1st and 5th metatarsal heads and calcaneus, of the right and the left foot, in
different dental conditions, namely mandibular postural position, maximum intercuspation,
biting on cotton rolls and maximum mouth opening. All the examinations were performed
with eyes open. We noticed that the left heel loading was reduced with an average of 1.9% in
maximum mouth opening condition when compared to maximum intercuspation. In con-
trast, the left 5th metatarsal loading increased with an average of 1.08% and 1.24%, respectively,
in maximum mouth opening condition when compared to biting on cotton rolls and maxi-
mum intercuspation, respectively. Our study also compared the stabilometric parameters
among the above mentioned dental conditions. Previous studies assessed the reliability of sta-
bilometric analysis using a force platform and showed good intra- and intersession reliability
[25,26]. Path length is considered to be a valid outcome measurement in numerous balance
conditions; the smaller the path length, the better is the postural stability [27]. When referring
to confidence area, a smaller surface means a better performance [28]. Velocity reflects the effi-
ciency of the postural control system (the smaller the velocity, the better the postural control)
[29]; it is considered the measurement with the greatest reliability among trials [30].
PLOS ONE | https://doi.org/10.1371/journal.pone.0228816 February 11, 2020 5 / 10
Static plantar pressure and stabilometry
Table 2. Static plantar pressure load distribution.
Variables Mandibular postural position Maximum intercuspation Bitingon cotton rolls Maximum mouth opening
Right foot (%) 49.85 ± 3.87 49.47 ± 4.61 49.43 ±4.83 49.71 ± 4.69
Right MT1 (%) 19.92 ± 8.08 19.69 ± 8.61 19.62 ± 8.93 19.63 ± 8.87
Right MT5 (%) 37 ± 8.29 36.72 ± 8.63 36.92 ± 8.11 37.24 ± 9.61
Right heel (%) 43.19 ± 10.85 43.68 ± 10.83 43.25 ± 10.46 43.23 ± 11.84
Left foot (%) 50.15 ± 3.87 50.49 ± 4.57 50.57 ± 4.83 50.29 ± 4.69
Left MT1 (%) 22.08 ± 6.62 21.51 ± 7.06 21.88 ± 6.68 22.36 ± 7.38
Left MT5 (%) 31.62 ± 9.13 30.81 ± 9.05 30.97 ± 9.47 32.05 ± 9.41
Left heel (%) 46.42 ± 11.08 47.63 ± 11.33 47.07 ± 11.85 45.73 ± 11.69
Data are presents as mean ± standard deviation; MT1: 1st metatarsal head; MT5: 5th metatarsal head.
https://doi.org/10.1371/journal.pone.0228816.t002
The study of Perinetti (2006) including 26 healthy subjects (mean age 26.8 ± 5.3 years)
showed that there were no differences of the posturographic parameters (absolute mean dis-
placement of the centre of pressure from the theoretical point, projected sway area and sway
length) between mandibular postural position and dental intercuspidation [9]. Sway area refers
to the swept area that connects the mean point of the trajectory to all subsequent points in the
trajectory, normalised to the duration of acquisition; it is expressed in mm2 per second. Sway
length (sway path) means the length of the trajectory followed by the CoP normalized to the
duration of acquisition; is coincides with the mean velocity or average speed [31].
Our study analysing 95 healthy young adults showed that the confidence ellipse area was
lower in maximum intercuspation in comparison to mandibular postural position. Perinetti
recommended future investigations that should focus on the effects of extreme mandibular
positions [9]. In our study we also recorded the stabilometric parameters in maximum mouth
opening. The stabilometric parameters, CoP path length and maximum CoP speed, were sig-
nificantly greater in maximum mouth opening condition in comparison to mandibular pos-
tural position, maximum intercuspation and biting on cotton rolls position. The confidence
ellipse area was also higher in maximum mouth opening when compared to maximum inter-
cuspation. These data suggest that the postural stability, expressed as CoP path length, maxi-
mum CoP speed and confidence ellipse area, is most decreased when the examination was
performed in maximum mouth opening condition.
Baldini et al. (2013) assessed 44 healthy volunteers in different conditions (mandibular pos-
tural position, mandibular position of centric occlusion and mandibular position with 8-mm
thick cotton rolls) and noticed that the position of the centre of the foot pressure was not influ-
enced by occlusal components [5]. The current study showed that there were no differences in
Table 3. Stabilometric data.
Mandibular postural position Maximum intercuspation Biting on cotton rolls Maximum mouth opening p
CoP X � 0.97 ± 7.91 1.29 ± 9.38 0.75 ± 9.83 1.38 ± 9.88 NS
CoP Y � 3.27 ± 14.17 1.42 ± 13.81 2.27 ± 12.81 2.94 ± 13.99 NS
CoP displacement (mm)�� 13.34 [7.36–20.45] 13 [8.56–19.98] 12.73 [8.5–17.66] 14.21 [9.89–21.39] NS
CoP path length (mm)�� 245 [215–275] 237 [206–260.25] 239 [215.25–261.25] 250 [221–286] 0.0001
90% confidence ellipse area (mm2)�� 51 [34.5–92.25] 36 [25–66] 46 [28–74.5] 47 [29–84.75] 0.001
��
Maximum CoP speed (mm/s) 49 [43–65.5] 50 [44–61] 51 [44–59.75] 55 [48–68.75] 0.003
�
Data are presented as mean ± standard deviation;
��
Data are presented as median [interquartile range]; COP: centre of pressure; NS: not significant.
https://doi.org/10.1371/journal.pone.0228816.t003
PLOS ONE | https://doi.org/10.1371/journal.pone.0228816 February 11, 2020 6 / 10
Static plantar pressure and stabilometry
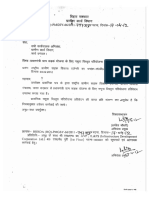
Fig 1. Stabilometric data comparison. Box plots (median, 95% confidence interval, interquartile range) describe the COP path length (A), 90% confidence area (B),
maximum COP speed (C) and COP displacement (D) according to the condition. (� —p<0.05).
https://doi.org/10.1371/journal.pone.0228816.g001
the CoP displacement measurement when comparing the mandibular postural position, maxi-
mum intercuspation, biting on cotton rolls and maximum mouth opening conditions.
The study of Oie E. et al. examining 15 adult males showed that occlusal contact is one of
the factors that affect gravity fluctuation; appropriate occlusion attained by maintaining even
occlusal contact in the posterior region is crucial for gravity fluctuation [32]. Julia-Sanchez S.
et al. (2016) showed that mandibular position has a significant influence in the balance control;
the body balance was better when dental occlusion was set in cotton rolls mandibular condi-
tion (with 8 mm thick cotton rolls placed between the two dental arches) in comparison with
intercuspal position (achieved by clenching the teeth) [33]. Scharnweber et al. (2016) after
assessing 87 healthy male subjects noticed that blocking occlusion leads to sway reduction
[34]. Our study recorded that in maximum intercuspation, the stabilometric parameters
showed a better postural stability than in mandibular postural position.
The lack of comparison between the subjects without any composite fillings and the sub-
jects with one or more composite fillings is a limitation of our study.
PLOS ONE | https://doi.org/10.1371/journal.pone.0228816 February 11, 2020 7 / 10
Static plantar pressure and stabilometry
Conclusions
In right-handed young adults the static plantar pressure is influenced by the maximum mouth
opening. This dental condition was characterized by a reduced loading on the left calcaneus in
comparison to maximum intercuspation and an increased loading on the left 5th metatarsal
head in comparison to maximum intercuspation and biting on cotton rolls. Regarding the sta-
bilometry, an improved postural stability was recorded in maximum intercuspation in com-
parison to mandibular postural position. The maximum intercuspation is used by the subject
during swallowing, while the mandibular postural position allows the relaxation of the masti-
catory muscles after functional moments. In contrast, a decreased postural stability was
recorded when the examination was performed with maximum mouth opening.
Supporting information
S1 Fig.
(TIF)
Author Contributions
Conceptualization: Elena Amaricai, Roxana Ramona Onofrei, Oana Suciu, Corina Marcau-
teanu, Eniko Tunde Stoica, Meda Lavinia Negruțiu, Cosmin Sinescu.
Data curation: Roxana Ramona Onofrei.
Formal analysis: Elena Amaricai, Oana Suciu, Corina Marcauteanu, Eniko Tunde Stoica,
Meda Lavinia Negruțiu.
Investigation: Elena Amaricai, Roxana Ramona Onofrei, Oana Suciu, Corina Marcauteanu,
Eniko Tunde Stoica, Meda Lavinia Negruțiu.
Methodology: Elena Amaricai, Roxana Ramona Onofrei, Oana Suciu, Corina Marcauteanu,
Eniko Tunde Stoica, Meda Lavinia Negruțiu, Vlad Laurentiu David.
Supervision: Cosmin Sinescu.
Visualization: Elena Amaricai, Oana Suciu, Corina Marcauteanu, Eniko Tunde Stoica, Meda
Lavinia Negruțiu.
Writing – original draft: Elena Amaricai, Roxana Ramona Onofrei, Oana Suciu, Corina Mar-
cauteanu, Eniko Tunde Stoica, Meda Lavinia Negruțiu, Vlad Laurentiu David, Cosmin
Sinescu.
Writing – review & editing: Elena Amaricai, Roxana Ramona Onofrei, Oana Suciu, Corina
Marcauteanu, Eniko Tunde Stoica, Meda Lavinia Negruțiu, Vlad Laurentiu David, Cosmin
Sinescu.
References
1. Milani RS, Deville De Perière D, Lapeyre L, Pourreyron L. Relationship between Dental Occlusion and
Posture. Cranio. 2000; 18: 127–134. https://doi.org/10.1080/08869634.2000.11746124 PMID:
11202823
2. Moon H-JJ, Lee Y-KK. The Relationship Between Dental Occlusion/Temporomandibular Joint Status
and General Body Health: Part 1. Dental Occlusion and TMJ Status Exert an Influence on General
Body Health. J Altern Complement Med. 2011; 17: 995–1000. https://doi.org/10.1089/acm.2010.0739
PMID: 22070442
3. Cuccia A, Caradonna C. The relationship between the stomatognathic system and body posture. Clin-
ics. 2009; 64: 61–66. https://doi.org/10.1590/S1807-59322009000100011 PMID: 19142553
PLOS ONE | https://doi.org/10.1371/journal.pone.0228816 February 11, 2020 8 / 10
Static plantar pressure and stabilometry
4. Bracco P, Deregibus A, Piscetta R. Effects of different jaw relations on postural stability in human sub-
jects. Neurosci Lett. 2004; 356: 228–230. https://doi.org/10.1016/j.neulet.2003.11.055 PMID:
15036636
5. Baldini A, Nota A, Tripodi D, Longoni S, Cozza P. Evaluation of the correlation between dental occlusion
and posture using a force platform. Clinics. 2013; 68: 45–49. https://doi.org/10.6061/clinics/2013(01)
OA07 PMID: 23420156
6. Manfredini D, Castroflorio T, Perinetti G, Guarda-Nardini L. Dental occlusion, body posture and tempo-
romandibular disorders: Where we are now and where we are heading for. Journal of Oral Rehabilita-
tion. 2012. pp. 463–471. https://doi.org/10.1111/j.1365-2842.2012.02291.x PMID: 22435603
7. Perinetti G, Primožič J, Manfredini D, Di Lenarda R, Contardo L. The diagnostic potential of static body-
sway recording in orthodontics: A systematic review. European Journal of Orthodontics. 2013. pp. 696–
705. https://doi.org/10.1093/ejo/cjs085 PMID: 23148113
8. Michelotti A, Buonocore G, Manzo P, Pellegrino G, Farella M. Dental occlusion and posture: An over-
view. Prog Orthod. 2011; 12: 53–58. https://doi.org/10.1016/j.pio.2010.09.010 PMID: 21515232
9. Perinetti G. Dental occlusion and body posture: No detectable correlation. Gait Posture. 2006; 24: 165–
168. https://doi.org/10.1016/j.gaitpost.2005.07.012 PMID: 16275097
10. Julià-Sánchez S, Álvarez-Herms J, Burtscher M. Dental occlusion and body balance: A question of
environmental constraints? Journal of Oral Rehabilitation. Blackwell Publishing Ltd; 2019. pp. 388–397.
https://doi.org/10.1111/joor.12767 PMID: 30664820
11. Nota A, Tecco S, Ehsani S, Padulo J, Baldini A. Postural stability in subjects with temporomandibular
disorders and healthy controls: A comparative assessment. J Electromyogr Kinesiol. 2017; 37: 21–24.
https://doi.org/10.1016/j.jelekin.2017.08.006 PMID: 28865312
12. Baldini A, Nota A, Cravino G, Cioffi C, Rinaldi A, Cozza P. Influence of vision and dental occlusion on
body posture in pilots. Aviat Sp Environ Med. 2013; 84: 823–827. https://doi.org/10.3357/ASEM.3541.
2013 PMID: 23926657
13. Gangloff P, Louis JP, Perrin PP. Dental occlusion modifies gaze and posture stabilization in human sub-
jects. Neurosci Lett. 2000; 293: 203–206. https://doi.org/10.1016/s0304-3940(00)01528-7 PMID:
11036196
14. Fasul F, Erfelder E, Buchner A, Lang A-G. G*Power Version 3.1.7 [Internet]. Available: http://www.
psycho.uni-duesseldorf.de/abteilungen/aap/gpower3
15. Okeson JP. Management of Temporomandibular disorders and Occlusion. Management of Temporo-
mandibular disorders and Occlusion. 8th ed. 2019. pp. 74–86.
16. Global Postural System. Manual GPS 5—version 1.0.42. 2014.
17. www.chinesport.com [Internet]. Available: http://www.chinesport.com/catalog/posture-analysis/
stabilometric-analysis/03001-podata-2-0
18. Scoppa F, Gallamini M, Belloni G, Messina G. Clinical stabilometry standardization: Feet position in the
static stabilometric assessment of postural stability. Acta Medica Mediterr. 2017; 33: 707–713. https://
doi.org/10.19193/0393-6384_2017_4_105
19. The Glossary of Prosthodontic Terms: Ninth Edition. J Prosthet Dent. 2017; 117: e1–e105. https://doi.
org/10.1016/j.prosdent.2016.12.001 PMID: 28418832
20. Gobbi G, Galli D, Carubbi C, Pelosi A, Lillia M, Gatti R, et al. Assessment of body plantar pressure in
elite athletes: An observational study. Sport Sci Health. 2013; 9: 13–18. https://doi.org/10.1007/s11332-
013-0139-8
21. Mancini M, Horak FB. The relevance of clinical balance assessment tools to differentiate balance defi-
cits. Eur J Phys Rehabil Med. 2010; 46: 239–248. PMID: 20485226
22. Degani AM, Leonard CT, Danna-dos-Santos A. The effects of early stages of aging on postural sway: A
multiple domain balance assessment using a force platform. J Biomech. 2017; 64: 8–15. https://doi.org/
10.1016/j.jbiomech.2017.08.029 PMID: 28893391
23. Jbabdi M, Boissy P, Hamel M. Assessing control of postural stability in community-living older adults
using performance-based limits of stability. BMC Geriatr. 2008; 31: 8. https://doi.org/10.1186/1471-
2318-8-8 PMID: 18377646
24. Nagymate G, Kiss RM. Replacing redundant stabilometry parameters with ratio and maximum deviation
parameters. Proceedings of the 12th IASTED International Conference on Biomedical Engineering,
BioMed 2016. Acta Press; 2016. pp. 140–144. doi:10.2316/P.2016.832-022
25. Baldini A, Nota A, Assi V, Ballanti F, Cozza P. Intersession reliability of a posturo-stabilometric test,
using a force platform. J Electromyogr Kinesiol. 2013; 23: 1474–1479. https://doi.org/10.1016/j.jelekin.
2013.08.003 PMID: 23992631
PLOS ONE | https://doi.org/10.1371/journal.pone.0228816 February 11, 2020 9 / 10
Static plantar pressure and stabilometry
26. Ruhe A, Fejer R, Walker B. The test-retest reliability of centre of pressure measures in bipedal static
task conditions—A systematic review of the literature. Gait and Posture. 2010. pp. 436–445. https://doi.
org/10.1016/j.gaitpost.2010.09.012 PMID: 20947353
27. Donath L, Roth R, Zahner L, Faude O. Testing single and double limb standing balance performance:
Comparison of COP path length evaluation between two devices. Gait Posture. 2012; 36: 439–443.
https://doi.org/10.1016/j.gaitpost.2012.04.001 PMID: 22565319
28. Asseman F, Caron O, Crémieux J. Is there a transfer of postural ability from specific to unspecific pos-
tures in elite gymnasts? Neurosci Lett. 2004; 358: 83–86. https://doi.org/10.1016/j.neulet.2003.12.102
PMID: 15026154
29. Paillard T, Noé F. Effect of expertise and visual contribution on postural control in soccer. Scand J Med
Sci Sport. 2006; 16: 345–348. https://doi.org/10.1111/j.1600-0838.2005.00502.x PMID: 16978254
30. Duarte M, S F Freitas SM. Revisão sobre posturografia baseada em plataforma de força para avaliação
do equilı́brio Revision of posturography based on force plate for balance evaluation. Rev Bras Fisioter.
2010; 14: 183–192. PMID: 20730361
31. Prieto TE, Myklebust JB, Hoffmann RG, Lovett EG, Myklebust BM. Measures of postural steadiness:
Differences between healthy young and elderly adults. IEEE Trans Biomed Eng. 1996; 43: 956–966.
https://doi.org/10.1109/10.532130 PMID: 9214811
32. Oiea E, Horiuchib M, Somac K. Effects of occlusal contact and its area on gravity fluctuation. Angle
Orthod. 2010; 80: 540–546. https://doi.org/10.2319/032309-173.1 PMID: 20050750
33. Julià-Sánchez S, Álvarez-Herms J, Gatterer H, Burtscher M, Pagès T, Viscor G. The influence of dental
occlusion on the body balance in unstable platform increases after high intensity exercise. Neurosci
Lett. 2016; 617: 116–121. https://doi.org/10.1016/j.neulet.2016.02.003 PMID: 26876449
34. Scharnweber B, Adjami F, Schuster G, Kopp S, Natrup J, Erbe C, et al. Influence of dental occlusion on
postural control and plantar pressure distribution. Cranio—J Craniomandib Pract. 2017; 35: 358–366.
https://doi.org/10.1080/08869634.2016.1244971 PMID: 27760494
PLOS ONE | https://doi.org/10.1371/journal.pone.0228816 February 11, 2020 10 / 10
You might also like
- Dari Dokter RudiDocument8 pagesDari Dokter RudiCuan JuiceNo ratings yet
- To Evaluate Whether There Is A Relationship Between Occlusion andDocument13 pagesTo Evaluate Whether There Is A Relationship Between Occlusion andSamNo ratings yet
- Examination of The Relationship Between Mandibular Position and Body PostureDocument14 pagesExamination of The Relationship Between Mandibular Position and Body PostureKiss KatalinNo ratings yet
- Artículo InglésDocument5 pagesArtículo InglésJose Manuel Flores GarciaNo ratings yet
- Postural StabilityDocument5 pagesPostural StabilityLaura LealNo ratings yet
- Tardieu 2009Document4 pagesTardieu 2009guille rivasNo ratings yet
- Revision Oclusion Dental y PosturaDocument6 pagesRevision Oclusion Dental y PosturaAlberto Jesús CamposNo ratings yet
- Occlusion, Orthodontics and Posture: Are There Evidences? The Example of ScoliosisDocument10 pagesOcclusion, Orthodontics and Posture: Are There Evidences? The Example of ScoliosisAndreaVanoyMartinNo ratings yet
- 2022 Article 16231Document7 pages2022 Article 16231Ana Carolina SouzaNo ratings yet
- Relação Entre A Postura Do Pé e Má Oclusão em Crianas de 6 A 9 AnosDocument9 pagesRelação Entre A Postura Do Pé e Má Oclusão em Crianas de 6 A 9 AnosWanniely KussNo ratings yet
- Occlusal Overload and Bone - Implant LossDocument14 pagesOcclusal Overload and Bone - Implant LossAngela ArrazolaNo ratings yet
- Occlusal Plane Dictated Skeletal and Dental Malocclusion With Concomitant Postural Diagnostic Findings A Pilot Study Using Functional Positioning OverlaysDocument17 pagesOcclusal Plane Dictated Skeletal and Dental Malocclusion With Concomitant Postural Diagnostic Findings A Pilot Study Using Functional Positioning OverlaysAthenaeum Scientific PublishersNo ratings yet
- Oclusion 1Document10 pagesOclusion 1Itzel MarquezNo ratings yet
- Sixty-Eight Years of Experimental Occlusal Interference Studies: What Have We Learned?Document10 pagesSixty-Eight Years of Experimental Occlusal Interference Studies: What Have We Learned?davidcosmin186832No ratings yet
- Variables Affecting Orthodontic Tooth Movement With Clear AlignersDocument10 pagesVariables Affecting Orthodontic Tooth Movement With Clear AlignersGoutamNo ratings yet
- Responses of Jawbone To Pressure : OriginalarticleDocument6 pagesResponses of Jawbone To Pressure : OriginalarticleZachary DuongNo ratings yet
- Pressure from lips and tongue in children with Class III malocclusionDocument6 pagesPressure from lips and tongue in children with Class III malocclusionFabian BarretoNo ratings yet
- Palaska 2014Document10 pagesPalaska 2014Marco TeixeiraNo ratings yet
- Dentición Normal (4646)Document6 pagesDentición Normal (4646)Fabian BarretoNo ratings yet
- Bite Force and Influential Factors On Bite Force Measurements A Literature Review-Duygu 2019Document10 pagesBite Force and Influential Factors On Bite Force Measurements A Literature Review-Duygu 2019Dan MPNo ratings yet
- Pocket Dentistry Clinical Dentistry Insight EngineDocument29 pagesPocket Dentistry Clinical Dentistry Insight EnginePadmini ReddyNo ratings yet
- Muscular Forces Exerted On The Normal Deciduous DentitionDocument6 pagesMuscular Forces Exerted On The Normal Deciduous DentitionEstaf EmkeyzNo ratings yet
- Body PostureDocument7 pagesBody Posturepopat78No ratings yet
- Dental Occlusion and Body PostureDocument9 pagesDental Occlusion and Body Posture190004No ratings yet
- Efeitos de Má Oclusão e MastigaçãoDocument17 pagesEfeitos de Má Oclusão e MastigaçãoTânia DiasNo ratings yet
- Jurnal PBL 1Document6 pagesJurnal PBL 1Sundae McdNo ratings yet
- OutDocument14 pagesOutlorena8804No ratings yet
- Dental Occlusion and Body Posture: A Surface EMG Study: Cranio®Document9 pagesDental Occlusion and Body Posture: A Surface EMG Study: Cranio®Kiss KatalinNo ratings yet
- Complete Denture Remounting: Acta Stomatol Croat, Vol. 35, Br. 3, 2001. 381Document7 pagesComplete Denture Remounting: Acta Stomatol Croat, Vol. 35, Br. 3, 2001. 381Dentist HereNo ratings yet
- 1 s2.0 S090150271501348X MainDocument7 pages1 s2.0 S090150271501348X MainHome BOXTVNo ratings yet
- Effect of Occlusal Vertical Dimension of CompleteDocument7 pagesEffect of Occlusal Vertical Dimension of CompletedrlenaaaNo ratings yet
- J Lebanese Dent Assoc 2017 52 2 53 58 EngDocument6 pagesJ Lebanese Dent Assoc 2017 52 2 53 58 EngMarcel PavoniNo ratings yet
- Effect of Occlusal SplintDocument6 pagesEffect of Occlusal SplintDr. Zardasht N. BradostyNo ratings yet
- ATT00183Document7 pagesATT00183Daniel VelezNo ratings yet
- 2014 Evaluation of Cranio-Cervical Posture in Children With Bruxism Before and After Bite Plate TherapyDocument4 pages2014 Evaluation of Cranio-Cervical Posture in Children With Bruxism Before and After Bite Plate TherapyRabia MekamchaNo ratings yet
- Model Art BiofluxDocument5 pagesModel Art BiofluxLaura IosifNo ratings yet
- 1 s2.0 S0901502713000374 MainDocument8 pages1 s2.0 S0901502713000374 MainVeerawit LukkanasomboonNo ratings yet
- Artículo 1Document7 pagesArtículo 1José Manuel Varela SánchezNo ratings yet
- Head and Cervical Spine Postures in Complete Denture WearersDocument7 pagesHead and Cervical Spine Postures in Complete Denture WearersPreeti Agarwal KatyayanNo ratings yet
- Occlusal Overload With Dental Implants: A ReviewDocument5 pagesOcclusal Overload With Dental Implants: A ReviewEmre TezulasNo ratings yet
- 7.principles of Dentofacial Orthopedics PDFDocument10 pages7.principles of Dentofacial Orthopedics PDFMafer VazquezNo ratings yet
- Articulo Reading Report 1Document12 pagesArticulo Reading Report 1Caro RodriguezNo ratings yet
- 10 1016@j Joms 2012 03 016Document12 pages10 1016@j Joms 2012 03 016Karam EidNo ratings yet
- PerilloDocument7 pagesPerilloRuxandra FitaNo ratings yet
- Pulling Er 2013Document23 pagesPulling Er 2013Diana Margarita EcheverriNo ratings yet
- 1985 Australian Orthodontic Journal, MelbourneDocument19 pages1985 Australian Orthodontic Journal, MelbourneMariyamNo ratings yet
- Scs 0b013e31826b8267Document5 pagesScs 0b013e31826b8267ANGELA ROMERONo ratings yet
- Age-Dependent Biologic Response To Orthodontic Forces: Original ArticleDocument13 pagesAge-Dependent Biologic Response To Orthodontic Forces: Original ArticleAnushriya DuttaNo ratings yet
- Journal Pone 0253968Document13 pagesJournal Pone 0253968Marcos LópezNo ratings yet
- Condylar Displacement Between Centric Relation and Maximum Intercuspation in Symptomatic and Asymptomatic IndividualsDocument8 pagesCondylar Displacement Between Centric Relation and Maximum Intercuspation in Symptomatic and Asymptomatic IndividualsCarlaNavarroJiménezNo ratings yet
- Artigo 1 - Do Infant Cleft Dimensions Have An Influence On Occlusal Relations? A Subgroup Analysis Within An RCT of Primary Surgery in Patients With Unilateral Cleft Lip and PalateDocument11 pagesArtigo 1 - Do Infant Cleft Dimensions Have An Influence On Occlusal Relations? A Subgroup Analysis Within An RCT of Primary Surgery in Patients With Unilateral Cleft Lip and PalateTalmo DiasNo ratings yet
- A Meta-Analysis of Breastfeeding and Osteoporotic Fracture Risk in The FemalesDocument5 pagesA Meta-Analysis of Breastfeeding and Osteoporotic Fracture Risk in The Femalesanisa rizkyNo ratings yet
- Stability of Tapered and Parallel-Walled Dental Implants: A Systematic Review and Meta-AnalysisDocument12 pagesStability of Tapered and Parallel-Walled Dental Implants: A Systematic Review and Meta-AnalysisBagis Emre GulNo ratings yet
- Jced 11 E947Document5 pagesJced 11 E947wafiqahNo ratings yet
- Tongue Support of Complete Dentures in The ElderlyDocument6 pagesTongue Support of Complete Dentures in The ElderlyMi Bazarcito PalmaritoNo ratings yet
- JDMT Volume 5 Issue 2 Pages 68-81Document14 pagesJDMT Volume 5 Issue 2 Pages 68-81do hong quangNo ratings yet
- A Practical Approach to Adolescent Bone Health: A Guide for the Primary Care ProviderFrom EverandA Practical Approach to Adolescent Bone Health: A Guide for the Primary Care ProviderSarah PittsNo ratings yet
- The Osteoporotic Syndrome: Detection, Prevention, and TreatmentFrom EverandThe Osteoporotic Syndrome: Detection, Prevention, and TreatmentNo ratings yet
- Secondary Fracture Prevention: An International PerspectiveFrom EverandSecondary Fracture Prevention: An International PerspectiveMarkus J. SeibelNo ratings yet
- Disorders of the Patellofemoral Joint: Diagnosis and ManagementFrom EverandDisorders of the Patellofemoral Joint: Diagnosis and ManagementNo ratings yet
- Porqué en Contra de DarwinDocument10 pagesPorqué en Contra de DarwinAlberto Jesús CamposNo ratings yet
- Maceira EDocument21 pagesMaceira EDewidewidewi Madridista Part II100% (1)
- Ablacion Por RadiofrecuenciaDocument4 pagesAblacion Por RadiofrecuenciaAlberto Jesús CamposNo ratings yet
- Articulo Trabajo Terapias 2Document23 pagesArticulo Trabajo Terapias 2Alberto Jesús CamposNo ratings yet
- Uso de La Teología en El Origen de Las Especies de DarwingDocument29 pagesUso de La Teología en El Origen de Las Especies de DarwingAlberto Jesús CamposNo ratings yet
- The Effect of Different Dephts of Medial Heel Skive On Plantar PressuresDocument10 pagesThe Effect of Different Dephts of Medial Heel Skive On Plantar PressuresAlberto Jesús CamposNo ratings yet
- Revision Oclusion Dental y PosturaDocument6 pagesRevision Oclusion Dental y PosturaAlberto Jesús CamposNo ratings yet
- Posturologia 1Document8 pagesPosturologia 1Alberto Jesús CamposNo ratings yet
- Las Deudas de Darwin Hacia El Mundo Estático en El Origen de Las EspeciesDocument14 pagesLas Deudas de Darwin Hacia El Mundo Estático en El Origen de Las EspeciesAlberto Jesús CamposNo ratings yet
- Giant Epidermal Cyst of The FootDocument3 pagesGiant Epidermal Cyst of The FootnurhanaNo ratings yet
- Posturologia 2Document10 pagesPosturologia 2Alberto Jesús CamposNo ratings yet
- Darwin's Explanation of Design: Natural Selection Completes Copernican RevolutionDocument4 pagesDarwin's Explanation of Design: Natural Selection Completes Copernican RevolutionAlberto Jesús CamposNo ratings yet
- Articulo Origina Test Resistencia SupinacionDocument34 pagesArticulo Origina Test Resistencia SupinacionAlberto Jesús CamposNo ratings yet
- Influencia de La Postura Del Pie en El Mecanismo de Windlass, Ensayo ClinicoDocument20 pagesInfluencia de La Postura Del Pie en El Mecanismo de Windlass, Ensayo ClinicoAlberto Jesús CamposNo ratings yet
- Eje Helicoidal Instantaneo Del Eje de Asa y Tpa Estudio en DinamicaDocument10 pagesEje Helicoidal Instantaneo Del Eje de Asa y Tpa Estudio en DinamicaAlberto Jesús CamposNo ratings yet
- Situacion Del Evolucionismo Hoy DiaDocument29 pagesSituacion Del Evolucionismo Hoy DiaAlberto Jesús CamposNo ratings yet
- Test in Vivo de Metodo Mejorado para La Localizacion Funacional Del Eje de ASA PDFDocument6 pagesTest in Vivo de Metodo Mejorado para La Localizacion Funacional Del Eje de ASA PDFAlberto Jesús CamposNo ratings yet
- Mecanica de La Articulación Subastragalina y Funcion Sobre La MarchaDocument18 pagesMecanica de La Articulación Subastragalina y Funcion Sobre La MarchaAlberto Jesús CamposNo ratings yet
- Variación Tridimensional en Miembro Inferior A Causa Del Mecanismo de Windlass PDFDocument13 pagesVariación Tridimensional en Miembro Inferior A Causa Del Mecanismo de Windlass PDFAlberto Jesús CamposNo ratings yet
- Determinacion Eje ASA 3D PDFDocument30 pagesDeterminacion Eje ASA 3D PDFAlberto Jesús CamposNo ratings yet
- By Counteracting Gravity, Triceps Surae Sets Both Kinematics and Kinetics of GaitDocument16 pagesBy Counteracting Gravity, Triceps Surae Sets Both Kinematics and Kinetics of GaitAlberto Jesús CamposNo ratings yet
- Determinacion Eje ASA 3D PDFDocument30 pagesDeterminacion Eje ASA 3D PDFAlberto Jesús CamposNo ratings yet
- Efecto de Neuro Tape en Fuerza MmiiDocument12 pagesEfecto de Neuro Tape en Fuerza MmiiAlberto Jesús CamposNo ratings yet
- By Counteracting Gravity, Triceps Surae Sets Both Kinematics and Kinetics of GaitDocument16 pagesBy Counteracting Gravity, Triceps Surae Sets Both Kinematics and Kinetics of GaitAlberto Jesús CamposNo ratings yet
- Variación Tridimensional en Miembro Inferior A Causa Del Mecanismo de Windlass PDFDocument13 pagesVariación Tridimensional en Miembro Inferior A Causa Del Mecanismo de Windlass PDFAlberto Jesús CamposNo ratings yet
- Sivision DigitalDocument12 pagesSivision Digitalbogdan_h2000No ratings yet
- Suzanne Saroff - Year 9 Exam AnnaDocument1 pageSuzanne Saroff - Year 9 Exam Annaapi-569107627No ratings yet
- 80nva StatcomDocument1 page80nva StatcomIdriShh HaiNo ratings yet
- Accounting Management SystemDocument64 pagesAccounting Management Systemnilesh50% (2)
- Why Astrology Is Science: Five Good Reasons: Tapan Das, PH.D., P.EngDocument56 pagesWhy Astrology Is Science: Five Good Reasons: Tapan Das, PH.D., P.EngNikhil TidkeNo ratings yet
- Sistema de Entrenamiento de La Serie LabvoltDocument60 pagesSistema de Entrenamiento de La Serie LabvoltJeferson Fernando Arirama GarciaNo ratings yet
- Why Single-Ended Tube AmplifiersDocument17 pagesWhy Single-Ended Tube Amplifiersjimmy67music100% (2)
- 2.25 ISO 6886 2016 Oxidative StabilityDocument22 pages2.25 ISO 6886 2016 Oxidative Stabilityreda yehia100% (1)
- British Royal Yachts Historical BackgroundDocument9 pagesBritish Royal Yachts Historical BackgroundFelipe Andrés Reinal AranedaNo ratings yet
- GEOMETRY CH 5 Law of SinesDocument2 pagesGEOMETRY CH 5 Law of SinesJackson LudtkeNo ratings yet
- Math Stars Grade 5Document40 pagesMath Stars Grade 5Rivka Share50% (2)
- Peugeot All Models Wiring Diagrams - GeneralDocument32 pagesPeugeot All Models Wiring Diagrams - GeneralFitra AhmadNo ratings yet
- DPR TemplateDocument74 pagesDPR TemplateAnupamPanja0% (1)
- RAMANUJAN Magic SquareDocument15 pagesRAMANUJAN Magic SquareDetective HomeNo ratings yet
- M.Sc. MATHEMATICS MODEL PAPERDocument22 pagesM.Sc. MATHEMATICS MODEL PAPERRatnesh RanjanNo ratings yet
- Itr Ew 07a - EngDocument1 pageItr Ew 07a - Engwassim nasriNo ratings yet
- Safety Solenoid Valve Nominal Width RP 1/2 - RP 2 SV SV-D Sv-DleDocument8 pagesSafety Solenoid Valve Nominal Width RP 1/2 - RP 2 SV SV-D Sv-DleAgustantoNo ratings yet
- Multi-Hole Orifice CalculationDocument10 pagesMulti-Hole Orifice Calculationadrianrrcc100% (1)
- C Language Basic Programs Which Used For BigginnersDocument112 pagesC Language Basic Programs Which Used For BigginnersRavikumar VendiNo ratings yet
- TMS470 Assembly Language Tools User' S GuideDocument336 pagesTMS470 Assembly Language Tools User' S GuideMadhu CkNo ratings yet
- Samsung CAC Duct S Brochure 20140729 0Document16 pagesSamsung CAC Duct S Brochure 20140729 0Callany AnycallNo ratings yet
- 1 Gravity IntroductionDocument13 pages1 Gravity IntroductionPerry SegereNo ratings yet
- Guia TeraSpanDocument73 pagesGuia TeraSpanTim Robles MartínezNo ratings yet
- Gen Math11 - Q1 - Mod1 - Functions - v2Document28 pagesGen Math11 - Q1 - Mod1 - Functions - v2Anonymous 6gthRen100% (1)
- Data Structures and Algorithms IntroductionDocument22 pagesData Structures and Algorithms IntroductionTadele Molla ታደለ ሞላNo ratings yet
- MS ExcelDocument37 pagesMS Excelravi100% (2)
- Mark VieDocument4 pagesMark VieWalid Bahi100% (1)
- EEE Course CurriculumDocument3 pagesEEE Course CurriculumAanshu MishraNo ratings yet
- Accounting exam covers receivables, payablesDocument3 pagesAccounting exam covers receivables, payableseXpadaNo ratings yet
- STSMDocument278 pagesSTSMMiguel Ruiz TatajeNo ratings yet