Professional Documents
Culture Documents
Outcome of Gastrointestinal Surgery During COVID-19 Lockdown in A Tertiary Care Hospital, Nepal
Outcome of Gastrointestinal Surgery During COVID-19 Lockdown in A Tertiary Care Hospital, Nepal
Uploaded by
Shiwali SinghOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Outcome of Gastrointestinal Surgery During COVID-19 Lockdown in A Tertiary Care Hospital, Nepal
Outcome of Gastrointestinal Surgery During COVID-19 Lockdown in A Tertiary Care Hospital, Nepal
Uploaded by
Shiwali SinghCopyright:
Available Formats
General Section: COVID-19 Original Article
Outcome of gastrointestinal surgery during
COVID-19 lockdown in a tertiary care
hospital, Nepal
Surendra Shah1 , Sanjay Paudyal2 , Shantabir Maharjan3 , Samir
Shrestha3 , Shailendra Shah4 , Niraj Giri4 , Upendra Bhandari4 , Samyukta
KC4 , Saroj Babu Pradhan4 , Suyog Bhandari4 , Erena Pradhan4 , Jay
Narayan Shah2
1Asst.Prof., 2Prof., 3Assoc. Prof., 4Lecturer, Dept. of Surgery, Patan Hospital,
Patan Academy of Health Sciences, Lalitpur, Kathmandu, Nepal
ISSN: 2091-2749 (Print)
2091-2757 (Online)
Abstract
Correspondence
2091-2757 (Online) Introduction: Perioperative strategies have been changing due to the
Dr. Surendra Shah COVID-19 pandemic to prevent the risk of postoperative complications
Dept. of Surgery and transmission of infection. This study was aimed to assess the
Patan Hospital, Patan Academy
outcome of gastrointestinal surgery and the risk of transmission by
of Health Sciences, Lalitpur,
Kathmandu, Nepal
implementing COVID-19 testing criteria and surgical strategy.
Email:
drsurendrashah@gmail.com Method: This was a retrospective descriptive study conducted at the
department of surgery at Patan Hospital, Nepal, during COVID-19 lock-
down from 24 march to 15 June 2020. All patients who underwent
Peer Reviewers
Prof. Dr. Ganesh Dangal gastrointestinal (GI) surgery were included. High-risk patients (as defined
Kathmandu Model Hospital by the Hospital Incident Command System, HICS) were tested for COVID-
19 preoperatively. Surgery was performed in COVID operating room with
Prof. Dr. Nabees MS Pradhan full protective gear. Low-risk patients were not tested for COVID-19
School of Medicine, Patan preoperatively and performed surgery in non-COVID OR. Data from
Academy of Health Sciences patient’s case-sheets were analyzed descriptively for age, gender,
comorbidities, hospital stay, RT-PCR results, surgeries, and postoperative
Submitted complications.
9 Sep 2020
Result: There were total 44 GI surgeries performed; 31(70.5%) were
Accepted emergency, 5(11.3%) semi-emergency and 8(18.2%) oncology. There
20 Oct 2020 were 11(25%) patients tested for COVID-19 preoperatively and were
negative. Nine HCWs tested for COVID-19 randomly were negative.
Severe postoperative complications developed in 3 patients, with one
How to cite this article
Surendra Shah, Sanjay Paudyal,
mortality.
Shantabir Maharjan, Samir
Shrestha, Shailendra Shah, Conclusion: Among GI surgeries, there was no increase in postoperative
Niraj Giri, et al. Outcome of complications and transmission of COVID-19 to the patients or HCWs
gastrointestinal surgery during following the implementation of standard testing criteria and surgical
COVID-19 lockdown in a strategy.
tertiary care hospital, Nepal.
Journal of Patan Academy of Keywords: COVID-19, gastrointestinal surgery outcome, lockdown
Health Sciences.
2020Dec;7(3):6-12.
DOI:
https://doi.org/10.3126/jpahs.
v7i3.33819
6 Journal of Patan Academy of Health Sciences. 2020Dec;7(3):6-12.
Surendra Shah: Surgical outcome during COVID-19 lockdown
Introduction time reverse transcriptase-polymerase chain
reaction (RT-PCR) status of suspected patients
Global health including surgical care has been and health care workers (HCW), name of the
disrupted due to the COVID-19 pandemic. surgery and postoperative complications were
Therefore, guidelines for the management of recorded from the patient’s case-sheets.
surgical patients have been developed from Patients with missing data in the case-sheets
societies of several countries.1-3 International were excluded from the study. Approval for
study group including neighboring country the study was obtained from the Institutional
China showed an increased risk of pulmonary Review Committee of PAHS.
complications and mortality after surgery in
COVID-19 patients.4,5 The objective of the study was to evaluate the
outcome of gastrointestinal surgery during
Routine preoperative screening with RT-PCR the COVID-19 lockdown in Nepal. Outcome
on the day before surgery for COVID-19 is variables included intraoperative, early
suggested to minimize the increased risk of postoperative complications, mortality during
morbidity and mortality.6 However, the true the hospital stay, PCR positive COVID-19
benefit of preoperative screening depends on patients, and HCWs after implementing
the local prevalence of COVID-19.1 COVID-19 testing criteria and surgical
Government of Nepal declared lockdown on strategies in the hospital. Descriptive analysis
23 March 2020 when there was the detection was performed using Microsoft Excel.
of the second case of COVID-19 who had
traveled from France.7 We followed the testing criteria of RT-PCR for
COVID-19 as per HICS.8
The testing criteria for COVID-19 and surgical
strategies have been developed by the For patients-
Hospital Incident Command System (HICS) of i. Patients with fever and belongs to the
Patan Hospital, Patan Academy of Health area where community outbreak is
Sciences (PAHS).8 There is a lack of studies documented or no localizing symptoms
from Nepal (PubMed, Google Scholar, and
that explain the alternative diagnosis,
NepJOL) on postoperative outcomes after
surgery in COVID-19 patients. This study ii. All patients coming from areas where
aimed to assess the outcome of community outbreak is documented or
gastrointestinal (GI) surgery patients by coming from out of the valley,
implementing testing criteria for COVID-19 iii. Respiratory symptoms AND does not
and surgical strategy at Patan Hospital during have travel history outside the valley
the lockdown. within the last 28 days AND are not in
contact with any person who has travelled
Method outside Kathmandu Valley.
This was a retrospective descriptive study For health care workers (HCWs)-
conducted in the department of surgery, i. Those involved in surgery of patients (who
Patan Hospital, PAHS, Nepal, from 24 March have not suspected or confirmed COVID-
2020 to 15 June 2020. All the patients who 19) without personal protective
underwent gastrointestinal surgery during the equipment (PPE) and patients detected as
study period were included in the study. Case- a COVID-19 post-operatively,
sheets were retrieved from the medical
ii. The HCWs involved in surgery of
record section using the hospital number. All
data (age, gender, diagnosis, comorbidities suspected or confirmed COVID-19
(hypertension, diabetes, chronic obstructive patients who have breached protective
pulmonary disease (COPD), hospital stay, real- measures or developed respiratory
7 Journal of Patan Academy of Health Sciences. 2020Dec;7(3):6-12.
Surendra Shah: Surgical outcome during COVID-19 lockdown
symptoms. Irrespective of the above The strategy that was followed by all the
criteria, random RT-PCR testing of HCWs surgical departments at Patan Hospital, PAHS,
were done in all departments. Figure 1.
iii. The HCWs who met the above criteria
were quarantined and tested with RT-
PCR on the 7th day of exposure.
Figure 1. Surgical strategy at Patan Hospital, PAHS during COVID-19 lockdown period
Note: OR = Operating Room, RT-PCR = Reverse Transcriptase Polymerase Chain Reaction, PPE = Personal Protective
Equipment, ICU = Intensive Care Unit.
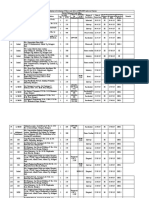
Result (25%) were emergency surgery cases. They
were admitted to the isolation ward through
There were 44 gastrointestinal surgeries the COVID-19 emergency. Their RT-PCR was
performed during COVID-19 lockdown which done preoperatively. These high-risk patients
included 22 males and 22 females. The mean were operated on in the COVID operation
age was 37 y, range from 8 to 76. There were room (OR) with full PPE without waiting for
31(70.5%) emergency, 5(11.3%) semi- RT-PCR reports. None of the high-risk patients
emergency and 8(18.2%) GI Oncologic surgery (11 i.e., 25%) tested positive for RT-PCR. The
cases performed, Table 1. Duration of surgery remaining patients (33 i.e., 75%) were
(mean) was 123 min (range from 40 to 600 operated on without RT-PCR in non-COVID
min) and mean hospital stay was 8 d (range 1 OR, Figure 2.
to 31).
The RT-PCR testing for COVID-19 was
Diabetes mellitus was present in 2-patients performed in 9 HCWs out of 19 involved in
and hypertension in 3-patients which were surgeries during the study period (based on a
controlled with medications. There were random selection by HICS for testing RT-PCR)
11(25%) patients who fit in testing criteria for and tests were negative for all. There was no
COVID-19 according to the definition of HICS intraoperative complication with high-risk or
and 33(75%) patients did not fit in testing low-risk cases. Severe postoperative
criteria. Those who fit into testing criteria complications (Clavien Dindo 3) developed in
8 Journal of Patan Academy of Health Sciences. 2020Dec;7(3):6-12.
Surendra Shah: Surgical outcome during COVID-19 lockdown
3-cases, including 1(2.3%) mortality. dehiscence (burst abdomen) developed in one
Mortality occurred in a case of gallbladder and had re-surgery under general anesthesia
perforation peritonitis with septic shock and for retention suture of the abdominal wound.
multiple organ dysfunction (acute renal One had an anastomotic leak after right
failure, coagulopathy with increased hemicolectomy following ileo-ileocolic
prothrombin time, and pneumonia). This intussusception. This patient required re-
patient was resuscitated in COVID ICU and laparotomy for peritoneal lavage and
performed open cholecystectomy and ileostomy, Table 2.
peritoneal lavage after resuscitation. Wound
Table 1. Gastrointestinal surgeries performed at Patan Hospital, PAHS during COVID-19 lockdown, N= 44
Diagnosis Name of Surgery N(%)
Emergency/semi-emergency 31(70.5%)
Acute appendicitis Open appendectomy 19(43.2%)
Duodenal perforation peritonitis Grahm’s patch repair 2(4.5%)
Giant duodenal perforation peritonitis Grahm’s patch + pyloric exclusion + GJ 1(2.3%)
Ileal perforation peritonitis Primary repair 2(4.5%)
Small bowel obstruction (postoperative) Exploratory laparotomy + band release 2(4.5%)
Appendicular perforation peritonitis Exploratory laparotomy + appendectomy 2(4.5%)
Meckel’s diverticular perforation peritonitis Exploratory laparotomy + wedge resection 1(2.3%)
Gallbladder perforation peritonitis Exploratory laparotomy + cholecystectomy 1(2.3%)
Ileo-ileo-colic intussusception Right hemicolectomy with ileal resection 1(2.3%)
Semi-emergency surgery 5(11.3%)
Status ileostomy Ileostomy closer (take-down) 2(4.5%)
Acute biliary pancreatitis Laparoscopic cholecystectomy 1(2.3%)
Acute calculus cholecystitis Open cholecystectomy (OC) 1(2.3%)
Gallstone with CBD (failed ERCP) OC with choledocholithotomy 1(2.3%)
GI oncologic surgery 8(18.2%)
Distal gastric cancer D2 subtotal gastrectomy 2(4.5%)
Locally advanced gastric cancer with GOO Gastro-jejunostomy 1(2.3%)
Periampullary cancer Pancreatico-duodenectomy 2(4.5%)
Gallbladder cancer Extended Cholecystectomy 2(4.5%)
Cystic neoplasm of the pancreas Extended pancreatico-duodenectomy 1(2.3%)
GJ = Gastrojejunostomy, CBD = Common bile duct, ERCP = endoscopic retrograde cholangio-pancreatography, GOO =
Gastric outlet obstruction
50
40
30 33
20
20
10 11 13 11
0
Emergency Surgery Elective Surgery Total
COVID OR Non-COVID OR
Figure 2. Type of surgery performed in COVID and non-COVID operation room (OR) at Patan Hospital, PAHS
during COVID-19 lockdown, N=44
9 Journal of Patan Academy of Health Sciences. 2020Dec;7(3):6-12.
Surendra Shah: Surgical outcome during COVID-19 lockdown
Table 2. Intra- and post-operative complications of GI surgery at Patan Hospital, PAHS during COVID-19
lockdown
Post-operative complications Clavien-Dindo N(%)
Wound dehiscence 3 1(2.3%)
Anastomotic leak 3 1(2.3%)
Multiorgan dysfunction 5 1(2.3%)
Duodenal stump leak 2 1(2.3%)
Mild intraluminal PPH 2 1(2.3%)
Pneumonia 2 2(4.6%)
Superficial surgical SSI 2 2(4.6%)
ISGPS Grade-B POPF 2 1(2.3%)
GI= gastrointestinal, PPH = post-pancreaticoduodenectomy hemorrhage, SSI = surgical site infection, ISGPS = International
Study Group for Pancreatic Surgery, POPF = postoperative pancreatic fistula
Discussion them developed COVID-19 during the hospital
stay.
There were 2(4.54%) pulmonary
complications (pneumonia) and 1(1.27%) Similarly, none of the HCWs involved in
mortality among 44 patients during the surgeries were infected during our study. This
postoperative period. None of them were could be because of a low level of the
positive for COVID-19. An international, outbreak and community transmission of
multicenter observational cohort study from COVID-19 in Nepal during the study period
235 hospitals in 24 countries among patients compared to other countries.9,10 The COVID-
with COVID-19 showed 51.2% pulmonary 19 outbreak was not at its peak in Nepal
complications and 7-days mortality of 5.2% during this study period. COVID-19 was first
and 30-days overall mortality of 23.7%.10 diagnosed on 23rd January 2020 in Nepal in a
student who returned from Wuhan, China on
Tracheal intubation and surgical procedures 5 January 2020.13 Second case of COVID-19
are prone to generate aerosol. Close contact was diagnosed on 23 March 2020 in a woman
for a prolonged period in OR further exposes who had returned from France on 17 March
HCWs to the transmission of COVID-19. Close 2020. After this, the Government of Nepal
contact increases the risk of transmission of declared lockdown in the country and started
COVID-19 to other patients in the ward.10,11 different measures to contain COVID-19.7
Surgery in COVID-19 patients is associated Quarantine, lockdown and isolation have
with an increased risk of postoperative been used in pandemics and shown to be
complications, particularly pulmonary useful a measure with coordinated and
complications, which may increase morbidity comprehensive approach to controlling the
and mortality. Therefore, preoperative testing transmission.14,15 However, cases of COVID-19
for COVID-19 in surgical patients is increased gradually in 57 districts out of 77 by
recommended.11,12 the end of May 2020, and 1572/69587 cases
(prevalence rate of 2.25%) were diagnosed as
Routine preoperative testing for COVID-19 COVID-19. Most districts had sporadic cases in
was not performed in our institute during the persons who had a travel history from abroad
study period. We followed a protocol and districts bordering India in the southern
developed by HICS at Patan Hospital, PAHS. plains of Nepal.16 Nepal and India have an
According to hospital protocol, only 11(25%) open border.
patients in the isolation ward required
preoperative testing and none of them were The role of selective preoperative testing for
diagnosed as COVID-19. The remaining COVID-19 needs to be re-evaluated when the
33(75%) patients did not qualify for RT-PCR outbreak is at its peak. Because the majority
testing criteria for COVID-19 and none of of COVID patients are asymptomatic and
asymptomatic patients cannot be detected
10 Journal of Patan Academy of Health Sciences. 2020Dec;7(3):6-12.
Surendra Shah: Surgical outcome during COVID-19 lockdown
without testing for COVID-19.16-18 So, there Author Contribution
was a possibility of not detecting patients and Concept, design, planning, accountability of
HCWs with asymptomatic COVID-19 infection the work - SS, SP, SM, SS, SS, NG, UB, SKC,
during our study period. SBP, SB, EP, JNS. Literature review, data
collection/ analysis - draft manuscript - SS.
Because of the COVID-19 pandemic, there has Revision and final manuscript - SS, JNS.
been a postponement and restriction for
elective surgery. However, prioritization has
been given for oncology and emergency Reference
surgeries.19 Surgeries have also been
postponed for inpatients with comorbidities 1. Søreide K, Hallet J, Matthews JB, Schnitzbauer
such as diabetes mellitus, hypertension, lung AA, Line PD, Lai PB, et al. Immediate and
diseases, obesity that could increase long‐term impact of the COVID‐19 pandemic
morbidity and mortality in COVID-19 on delivery of surgical services. Br J Surg.
infection.20 Our study also showed that most 2020;107(10):1250-61. | DOI | PubMed |
Google Scholar | Weblink |
of the surgeries performed were emergency
2. American College of Surgeons. Covid 19:
(70.5%), semi-emergency (11.3%), or GI elective case triage guidelines for surgical care.
malignancies (18.2%). | Weblink |
3. Moletta L, Pierobon ES, Capovilla G, Costantini
In our study, diabetes mellitus and M, Salvador R, Merigliano S, Valmasoni M.
hypertension were present in only two and International guidelines and recommendations
three patients respectively which were for surgery during COVID-19 pandemic: a
controlled with medication. systematic review. Int J Surg. 2020;79:180-8.
| DOI | PubMed | Google Scholar | Weblink |
The limitation of the study was that selective 4. Myles PS, Maswime S. Mitigating the risks of
surgery during the COVID-19 pandemic. Lancet.
testing for COVID-19 and random testing of
2020;396(10243);2-3. | DOI | PubMed | Google
HCWs might have missed asymptomatic Scholar | Weblink |
COVID cases. 5. Lei S, Jiang F, Su W, Chen C, Chen J, Mei W.
Clinical characteristics and outcomes of
patients undergoing surgeries during the
Conclusion incubation period of COVID-19 infection.
EClinicalMedicine. 2020;21:100331. | DOI |
There were no increased intraoperative and PubMed | Google Scholar | Full Text |
postoperative complications due to COVID-19. Weblink|
We did not find the transmission to HCW or 6. Nahshon C, Bitterman A, Haddad R, Hazzan D,
patients after implementing selective Lavie O. Hazardous postoperative outcomes of
unexpected COVID-19 infected patients: a call
preoperative testing criteria and surgical
for global consideration of sampling all
strategy implemented by the hospital asymptomatic patients before surgical
incidence command system. Further study treatment. World J Surg. 2020;44(8):2477-81.
would be needed to assess the role of | DOI | PubMed | Google Scholar | Weblink |
preoperative testing for COVID-19 if 7. Shrestha R, Shrestha S, Khanal P, KC B. Nepal’s
community transmission peaks in Nepal. first case of COVID-19 and public health
response. J Travel Med. 2020;27(3):taaa024.
| DOI | PubMed | Google Scholar | Full Text |
Conflict of Interest Weblink |
None 8. Adhikari S, Rijal S, Acharya PK, Sharma BP,
Ansari I, Rajbhandari P, Thapa P. Hospital
Funding incident command system, the pillar of COVID-
19 outbreak response: an experience from
None
Patan Hospital, Nepal. J Patan Acad Health Sci.
2020;7(1):80-4. | DOI | Google Scholar | Full
Text | Weblink |
11 Journal of Patan Academy of Health Sciences. 2020Dec;7(3):6-12.
Surendra Shah: Surgical outcome during COVID-19 lockdown
9. Reliefweb. COVID-19: Nepal response situation 15. Piryani RM, Piryani S, Shah JN. Nepal’s
report no XI, As of 15 June, 2020. ReliefWeb. response to contain COVID-19 infection. J
2020 Jun 15. | Weblink | Nepal Health Res Counc. 2020;18(1):128-34.
10. COVIDSurg Collaborative. Mortality and | DOI| | PubMed | Google Scholar| Full Text |
pulmonary complications in patients 16. Dhakal S, Karki S. Early epidemiological features
undergoing surgery with perioperative SARS- of COVID-19 in Nepal and public health
CoV-2 infection: an international cohort study. response. Front Med. 2020;7:524. | DOI |
Lancet. 2020;396:(10243):27-38. | DOI | PubMed | Google Scholar |
PubMed | Google Scholar | Weblink | 17. Day M. Covid-19: four fifths of cases are
11. Blouhos K, Boulas KA, Paraskeva A, asymptomatic, China figures indicate. BMJ.
Triantafyllidis A, Nathanailidou M, 2020;369:m1375. | DOI | PubMed | Google
Hatzipourganis K, Hatzigeorgiadis A. Scholar | Full Text | Weblink |
Understanding surgical risk during COVID-19 18. Nishiura H, Kobayashi T, Miyama T, Suzuki A,
pandemic: the rationale behind the decisions. Jung SM, Hayashi K, et al. Estimation of the
Front Surg. 2020;7:33. | DOI | PubMed | asymptomatic ratio of novel coronavirus
Google Scholar | Weblink | infections (COVID-19). Int J Infect Dis.
12. Kraft M, Pellino G, Jofra M, Sorribas M, Solís- 2020;94:154-5. | DOI | PubMed | Google
Peña A, Biondo S, Espín-Basany E. Incidence, Scholar |
features, outcome and impact on health 19. Mariani NM, Ceretti AP, Fedele V, Barabino M,
system of de-novo abdominal surgical diseases Nicastro V, Giovenzana M, Scifo G, De Nicola E,
in patients admitted with COVID-19. Surgeon. Opocher E. Surgical strategy during the COVID-
2020;S1479:e1-6. | DOI | PubMed | Google 19 pandemic in a University Metropolitan
Scholar | Full Text | Hospital in Milan, Italy. World J Surg.
13. Poudel K, Subedi P. Impact of COVID-19 2020:44(8):2471-6. | DOI | PubMed | Google
pandemic on socioeconomic and mental health Scholar |
aspects in Nepal. Int J Soc Psychiatry. 20. Cárdenas-Camarena L, Bayter-Marin JE, Durán
2020;66(8):748-55. | DOI | PubMed | Google H, Hoyos A, López-Romero CO, Robles-
Scholar | Cervantes JA, Echeagaray-Guerrero EE. Elective
14. Shah JN, Shah J, Shah J. Quarantine, isolation surgery during SARS-Cov-2/COVID-19
and lockdown: in context of COVID-19. JPAHS. pandemic: safety protocols with literature
2020 May 8;7(1):48–57. | DOI | Google Scholar review. Plast Reconstr Surg Glob Open.
| Full Text | 2020;8(6):e2973. | DOI | PubMed | Google
Scholar | Weblink |
12 Journal of Patan Academy of Health Sciences. 2020Dec;7(3):6-12.
You might also like
- 10 Leopold's ManeuverDocument5 pages10 Leopold's ManeuverKrizia R. Pingke83% (6)
- Tracheostomy Care With ChecklistDocument5 pagesTracheostomy Care With ChecklistHollan GaliciaNo ratings yet
- US Doctor Database Sample 1Document8 pagesUS Doctor Database Sample 1Shiwali SinghNo ratings yet
- JurnalDocument5 pagesJurnalJamila JuwitaNo ratings yet
- Management of Appendicitis During COVID-19 Pandemic Short-Term OutcomesDocument5 pagesManagement of Appendicitis During COVID-19 Pandemic Short-Term OutcomesLidiaNo ratings yet
- ExperimentalDocument6 pagesExperimentalDiego TorresNo ratings yet
- MANUSCRIPT-COVID-19-RAPID-ANTIGEN-TESTING-A-SCREENING-TOOL-AND-EXPOSURE-PREVENTION-STRATEGY-AMONG-CANCER-PATIENTS-UNDERGOING-OUTPATIENT-TREATMENT-INFUSIONS-IN-A-SECONDARY-LEVEL-HOSPITAL-IN-ANTIQUE-TRA-1Document14 pagesMANUSCRIPT-COVID-19-RAPID-ANTIGEN-TESTING-A-SCREENING-TOOL-AND-EXPOSURE-PREVENTION-STRATEGY-AMONG-CANCER-PATIENTS-UNDERGOING-OUTPATIENT-TREATMENT-INFUSIONS-IN-A-SECONDARY-LEVEL-HOSPITAL-IN-ANTIQUE-TRA-1Harrold BacosaNo ratings yet
- Privateroom JournalDocument5 pagesPrivateroom JournalNathaniel PulidoNo ratings yet
- Ahead of Print: Establishment of Diagnostic Protocols For COVID-19 PatientsDocument6 pagesAhead of Print: Establishment of Diagnostic Protocols For COVID-19 PatientsSana AbbasNo ratings yet
- Abdomen Quirurgico AgudoDocument7 pagesAbdomen Quirurgico AgudoJorge Luis Plasencia CubaNo ratings yet
- Recommendations For Surgery During The Novel CoronavirusDocument5 pagesRecommendations For Surgery During The Novel CoronavirusHéctor Juárez GrandaNo ratings yet
- Delayed RT PCR For AdultDocument6 pagesDelayed RT PCR For AdultAizawanda ReNo ratings yet
- 1921 7826 3 PBDocument9 pages1921 7826 3 PBLeilybadryaNo ratings yet
- Incidence Rate, Clinical Course and Risk Factor For Recurrent PCR Positivity in Discharged COVID-19 Patients in Guangzhou, China - A Prospective Cohort StudyDocument14 pagesIncidence Rate, Clinical Course and Risk Factor For Recurrent PCR Positivity in Discharged COVID-19 Patients in Guangzhou, China - A Prospective Cohort StudyolfianyNo ratings yet
- Effectiveness of Ivermectin As Add-On Therapy in COVID-19 ManagementDocument12 pagesEffectiveness of Ivermectin As Add-On Therapy in COVID-19 Managementprashant kumarNo ratings yet
- A National UK Audit For Diagnostic Accuracy of PreDocument4 pagesA National UK Audit For Diagnostic Accuracy of PreRaudha Dani RahmalisaNo ratings yet
- Artemisin PiperaquineDocument8 pagesArtemisin PiperaquineIrma Rahayu LatarissaNo ratings yet
- Aerosol-Generating Procedures inDocument5 pagesAerosol-Generating Procedures inHaris WidodoNo ratings yet
- Journal Pre-Proof: Journal of Infection and Public HealthDocument25 pagesJournal Pre-Proof: Journal of Infection and Public HealthMohammed Shuaib AhmedNo ratings yet
- Chen2020 Article ADiagnosticModelForCoronavirusDocument10 pagesChen2020 Article ADiagnosticModelForCoronavirusPier Cedron LescanoNo ratings yet
- Jama 2020 17022Document13 pagesJama 2020 17022wiwiNo ratings yet
- Meta 8Document9 pagesMeta 8Jonathan AiresNo ratings yet
- The Correlation Between Oral Health Status With The Recovery Period, C-Reactive Protein Values and Severity of Covid-19 Recovered Patients of Raichur - A Cross-Sectional StudyDocument8 pagesThe Correlation Between Oral Health Status With The Recovery Period, C-Reactive Protein Values and Severity of Covid-19 Recovered Patients of Raichur - A Cross-Sectional StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Background: Information About Critically Ill Patients WithDocument19 pagesBackground: Information About Critically Ill Patients WithamochiteamoNo ratings yet
- The Study of Clinical Profile of Acute Kidney Injury in COVID-19 PatientsDocument6 pagesThe Study of Clinical Profile of Acute Kidney Injury in COVID-19 PatientsbijgimNo ratings yet
- Clinical Characteristics and Durations of Hospitalized Patients With COVID-19 in BeijingDocument18 pagesClinical Characteristics and Durations of Hospitalized Patients With COVID-19 in BeijingTOMMYNo ratings yet
- Characterization of Patients Who Return To Hospital Following Discharge From Hospitalization For COVID-19Document7 pagesCharacterization of Patients Who Return To Hospital Following Discharge From Hospitalization For COVID-19RelviGuzmanApazaNo ratings yet
- Covid y CoagulaciónDocument6 pagesCovid y CoagulaciónMaría JoséNo ratings yet
- Clinical Characteristics of Imported Cases of COVID-19 in Jiangsu Province A Multicenter Descriptive StudyDocument23 pagesClinical Characteristics of Imported Cases of COVID-19 in Jiangsu Province A Multicenter Descriptive StudyAna Maria Romero IbagonNo ratings yet
- Preprint corticoidesNeuminiaCOVIDDocument16 pagesPreprint corticoidesNeuminiaCOVIDJorgelina BernetNo ratings yet
- Jourding 1 Elsa Tania FixDocument19 pagesJourding 1 Elsa Tania Fixelsa taniaNo ratings yet
- A Clinical and Procedural Guideline For Gastrointestinal Endoscopy Units During COVID-19 Pandemic EraDocument5 pagesA Clinical and Procedural Guideline For Gastrointestinal Endoscopy Units During COVID-19 Pandemic EraMorris LBNo ratings yet
- Kí Ninh Cô VidDocument5 pagesKí Ninh Cô Vidhuyphuc052019No ratings yet
- Impact of The COVID 19 Pandemic On Gallstone Disease Experience at A High Volume CenterDocument11 pagesImpact of The COVID 19 Pandemic On Gallstone Disease Experience at A High Volume CenterAthenaeum Scientific PublishersNo ratings yet
- 10 1513@annalsats 202004-324ocDocument36 pages10 1513@annalsats 202004-324ocDany Daniel Rafael HuamanNo ratings yet
- Impact of Corticosteroid Therapy On Outcomes of Persons With Sars-Cov-2, Sars-Cov, or Mers-Cov Infection: A Systematic Review and Meta-AnalysisDocument9 pagesImpact of Corticosteroid Therapy On Outcomes of Persons With Sars-Cov-2, Sars-Cov, or Mers-Cov Infection: A Systematic Review and Meta-AnalysisMax CamargoNo ratings yet
- Jurnal MPIDocument4 pagesJurnal MPIMarini TaslimaNo ratings yet
- CPT-REM Study Final Report (30July-31OCT2020) FINAL VERSIONDocument56 pagesCPT-REM Study Final Report (30July-31OCT2020) FINAL VERSIONSaroj BhattaraiNo ratings yet
- Anticoagulant TreatmentDocument6 pagesAnticoagulant TreatmentMonica AngNo ratings yet
- Recommendations To Manage Patients For Bariatric Surgery in The COVID-19 Pandemic: Experience From ChinaDocument4 pagesRecommendations To Manage Patients For Bariatric Surgery in The COVID-19 Pandemic: Experience From ChinaRadu MiricaNo ratings yet
- 2021 Article 10141Document9 pages2021 Article 10141Oskr VeraNo ratings yet
- Usefulness of High-Resolution Computed Tomography in Early Diagnosis of Patients With Suspected COVID-19Document7 pagesUsefulness of High-Resolution Computed Tomography in Early Diagnosis of Patients With Suspected COVID-19Israel Parra-OrtegaNo ratings yet
- 2020 03 01 20029611v1 FullDocument24 pages2020 03 01 20029611v1 FullJulius HalimNo ratings yet
- Re-Positive Coronavirus Disease 2019 PCR Test: Could It Be A Reinfection?Document6 pagesRe-Positive Coronavirus Disease 2019 PCR Test: Could It Be A Reinfection?Diego Armando Bolivar SilvaNo ratings yet
- Hospital Admission Criteria For COVID-19 Patients: MODIFIED: MAY 8, 2020Document2 pagesHospital Admission Criteria For COVID-19 Patients: MODIFIED: MAY 8, 2020Baebee LouNo ratings yet
- Jamainternal Ortigoza 2021 Oi 210071 1643648313.72397Document12 pagesJamainternal Ortigoza 2021 Oi 210071 1643648313.72397Joaquin OlivaresNo ratings yet
- An Epidemiological Study of Laboratory Confirmed COVID-19 Cases Admitted in Dhaka Medical College HospitalDocument7 pagesAn Epidemiological Study of Laboratory Confirmed COVID-19 Cases Admitted in Dhaka Medical College HospitalPranto BaraiNo ratings yet
- Clinical Microbiology and Infection: Research NoteDocument4 pagesClinical Microbiology and Infection: Research NoteNoorNo ratings yet
- JMV 9999 NaDocument10 pagesJMV 9999 NaNurul AzizahNo ratings yet
- Jama Li 2020 Oi 200065Document11 pagesJama Li 2020 Oi 200065Jheny LopezNo ratings yet
- LC PDFDocument10 pagesLC PDFJorge Andres Balza GranadosNo ratings yet
- Jurnal 1Document5 pagesJurnal 1Jojo McalisterNo ratings yet
- Jia2 25489Document9 pagesJia2 25489Ahmed AllamNo ratings yet
- Emergency Tracheal Intubation in 202 Patients With COVID-19 in Wuhan, China: Lessons Learnt and International Expert RecommendationsDocument10 pagesEmergency Tracheal Intubation in 202 Patients With COVID-19 in Wuhan, China: Lessons Learnt and International Expert RecommendationsKOASS UMY PKU GampingNo ratings yet
- Use of Approved Therapies For Treatment of COVID19 DiseaseDocument22 pagesUse of Approved Therapies For Treatment of COVID19 DiseaseSacad SuleimanNo ratings yet
- Covid CT Chest Scan Score & SeverityDocument7 pagesCovid CT Chest Scan Score & SeverityMohan DesaiNo ratings yet
- Dong J - Prediction For Progression Risk in Patients With COVID - 19 Pneumonia The CALL ScoreDocument7 pagesDong J - Prediction For Progression Risk in Patients With COVID - 19 Pneumonia The CALL ScoreMercedes Ah CardenasNo ratings yet
- Nutrition Bio-Shield Superfood (NBS)Document6 pagesNutrition Bio-Shield Superfood (NBS)Irma Rahayu LatarissaNo ratings yet
- JMV 25961Document9 pagesJMV 25961damar soebandNo ratings yet
- Development and Validation of A Nomogram Using On Admission Routine Laboratory Parameters To Predict In-Hospital Survival of Patients With COVID-19Document23 pagesDevelopment and Validation of A Nomogram Using On Admission Routine Laboratory Parameters To Predict In-Hospital Survival of Patients With COVID-19dariusNo ratings yet
- Ivermectin Covid 29Document20 pagesIvermectin Covid 29Esteban DavidNo ratings yet
- 2020 04 24 20078949v1 FullDocument14 pages2020 04 24 20078949v1 FullAbay SisayNo ratings yet
- Living on the Frontline of COVID-19 in MCO And CMCO: Clinical Updates in COVID-19From EverandLiving on the Frontline of COVID-19 in MCO And CMCO: Clinical Updates in COVID-19No ratings yet
- List CTapprove GCTDocument235 pagesList CTapprove GCTShiwali SinghNo ratings yet
- Methodology of Seasonal Waves of Respiratory.2Document12 pagesMethodology of Seasonal Waves of Respiratory.2Shiwali SinghNo ratings yet
- PTADocument1 pagePTAShiwali SinghNo ratings yet
- Address List 26.11.15Document73 pagesAddress List 26.11.15Shiwali SinghNo ratings yet
- Private Hospitals Consolidated ListDocument535 pagesPrivate Hospitals Consolidated ListJagsonpal Medical Insights100% (1)
- Iadvl Directory 2009: (This Directory Is in Name First Format)Document165 pagesIadvl Directory 2009: (This Directory Is in Name First Format)Shiwali SinghNo ratings yet
- LT PP 3PH Above 20KW List 290618Document408 pagesLT PP 3PH Above 20KW List 290618Shiwali SinghNo ratings yet
- 2 TNPG 2020 - State R1 Allotment List (ALL) With AI R2 Allotment - Course WiseDocument62 pages2 TNPG 2020 - State R1 Allotment List (ALL) With AI R2 Allotment - Course WiseShiwali SinghNo ratings yet
- Paste 2cSgUaIDocument4 pagesPaste 2cSgUaIShiwali SinghNo ratings yet
- Announcement-5c25a4e0151645 78846474Document12 pagesAnnouncement-5c25a4e0151645 78846474Shiwali SinghNo ratings yet
- Admission Year, 2019-20 Post Graduate StudentsDocument6 pagesAdmission Year, 2019-20 Post Graduate StudentsShiwali SinghNo ratings yet
- RTI 4 (1) A 2020-21 BelagaviDocument214 pagesRTI 4 (1) A 2020-21 BelagaviShiwali SinghNo ratings yet
- PNDT List of July 2017 HospitalDocument128 pagesPNDT List of July 2017 HospitalShiwali SinghNo ratings yet
- Jemds Title Page: DR - Budhi Prakash Bhatia 2.Dr - Vinod Kumar 3.Dr - Jaiveer Singh Shekhawat 4.Dr - Vinay NaithaniDocument1 pageJemds Title Page: DR - Budhi Prakash Bhatia 2.Dr - Vinod Kumar 3.Dr - Jaiveer Singh Shekhawat 4.Dr - Vinay NaithaniShiwali SinghNo ratings yet
- IMA Agra Directory.Document152 pagesIMA Agra Directory.Shiwali Singh100% (3)
- Department of NephrologyDocument3 pagesDepartment of NephrologyShiwali SinghNo ratings yet
- The West Bengal University of Health Sciences: WebsiteDocument2 pagesThe West Bengal University of Health Sciences: WebsiteShiwali SinghNo ratings yet
- Isa Maharashtra VotersDocument118 pagesIsa Maharashtra VotersShiwali Singh100% (1)
- Dr. Mahesh Y. Borikar: Curriculum VitaeDocument4 pagesDr. Mahesh Y. Borikar: Curriculum VitaeShiwali SinghNo ratings yet
- Shyam Star Unp 4459 Iepf 1 1Document254 pagesShyam Star Unp 4459 Iepf 1 1Shiwali SinghNo ratings yet
- M-7 Dr. Vimala Menon: P-10 Dr. Phiroze PatelDocument58 pagesM-7 Dr. Vimala Menon: P-10 Dr. Phiroze PatelShiwali SinghNo ratings yet
- Millenium Gold Medal Award 2021Document1 pageMillenium Gold Medal Award 2021Shiwali SinghNo ratings yet
- Talash Member List AxcelDocument9 pagesTalash Member List AxcelShiwali SinghNo ratings yet
- Directorsofcompaniesstruckoff RocjaipurDocument6,596 pagesDirectorsofcompaniesstruckoff RocjaipurShiwali SinghNo ratings yet
- List of Faculty September 2021Document22 pagesList of Faculty September 2021Shiwali SinghNo ratings yet
- CAREvent ALS BLS Manual Rev K Sept 08Document8 pagesCAREvent ALS BLS Manual Rev K Sept 08KennethAdrianRosaNo ratings yet
- Pharmaceutical Care 5: Clinical Pharmacy Coronary Artery DiseaseDocument80 pagesPharmaceutical Care 5: Clinical Pharmacy Coronary Artery DiseaseJerson Aizpuro SuplementoNo ratings yet
- Thenar FlapDocument23 pagesThenar FlapDiyar Abdulwahid SalihNo ratings yet
- Adhesive BridgesDocument22 pagesAdhesive BridgesShekinah Andrea DumlaoNo ratings yet
- Clinical File-1 2Document180 pagesClinical File-1 2Arslan SiddiquiNo ratings yet
- 2011 Early Cannulation Grafts in Straight Axillo Axillary AngioaccessesDocument4 pages2011 Early Cannulation Grafts in Straight Axillo Axillary AngioaccessesKindylight KindylightNo ratings yet
- Gastroenterology by Elagouri MohammedDocument31 pagesGastroenterology by Elagouri MohammedStylesh GuRlyNo ratings yet
- Neglected Femoral Neck Fractures in AdultsDocument21 pagesNeglected Femoral Neck Fractures in AdultsJauharil Wafi MuhammadNo ratings yet
- Open Reduction and Internal Fixation SurgerybyDocument3 pagesOpen Reduction and Internal Fixation SurgerybyLindsay Ann Garcia MariacaNo ratings yet
- Cardiac - Anatomy of The HeartDocument9 pagesCardiac - Anatomy of The HeartRiya ThoratNo ratings yet
- Revision Sinus Surgery-Springer-Verlag Berlin Heidelberg (2008)Document349 pagesRevision Sinus Surgery-Springer-Verlag Berlin Heidelberg (2008)Javier Gutiérrez CastilloNo ratings yet
- Laser Ophthalmology MergedDocument22 pagesLaser Ophthalmology MergedJack Ortega PuruggananNo ratings yet
- Inguinal Hernia: Dr. Amar Rathod M.S. (Ayurved)Document18 pagesInguinal Hernia: Dr. Amar Rathod M.S. (Ayurved)GAURAV0% (1)
- Colon CancerDocument75 pagesColon Cancershefalika mandremNo ratings yet
- Solution Manual For Human Anatomy Laboratory Manual With Cat Dissections 7 e 7th EditionDocument11 pagesSolution Manual For Human Anatomy Laboratory Manual With Cat Dissections 7 e 7th EditionJamesThomasngec100% (44)
- Laporan Kasus Hipertensi Pulmonal-Ridha MardhatillahDocument3 pagesLaporan Kasus Hipertensi Pulmonal-Ridha MardhatillahAtunNo ratings yet
- Lumbar PunctureDocument6 pagesLumbar PunctureShesly Philomina100% (1)
- Catalog Wellland Surgical PositioningDocument1 pageCatalog Wellland Surgical Positioningtyan eronNo ratings yet
- KACH Formulary Category OCT09Document5 pagesKACH Formulary Category OCT09dareesNo ratings yet
- NICU DOH Compliance Monitoring Sheet 1Document2 pagesNICU DOH Compliance Monitoring Sheet 1Sherilyn RodriguezNo ratings yet
- English Recovery RoomDocument5 pagesEnglish Recovery RoomRahima PutriNo ratings yet
- Volkmann's Ischemic ContractureDocument41 pagesVolkmann's Ischemic ContractureKrishna Madhukar91% (11)
- Abnormal Uterine BleedingDocument34 pagesAbnormal Uterine BleedingMohmmadRjab SederNo ratings yet
- Hepatobiliary SystemDocument131 pagesHepatobiliary SystemCurt Leye RodriguezNo ratings yet
- Week 2 Med Term List Amp Practice HandoutDocument3 pagesWeek 2 Med Term List Amp Practice Handoutapi-308826929No ratings yet
- Developmental Dysplasia of HipDocument68 pagesDevelopmental Dysplasia of HipwildanmalikNo ratings yet
- Split Earlobe Repair Using A Double-Flap TechniqueDocument3 pagesSplit Earlobe Repair Using A Double-Flap Techniquedrgurpal74No ratings yet
- Neck Swellings Final .Document11 pagesNeck Swellings Final .little miss scare-allNo ratings yet