Professional Documents
Culture Documents
Muerte Por Zinc
Muerte Por Zinc
Uploaded by
Francico XavierOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Muerte Por Zinc
Muerte Por Zinc
Uploaded by
Francico XavierCopyright:
Available Formats
MEDICATION ERRORS
A Fatal Zinc Overdose in a Neonate
Confusion of Micrograms With Milligrams
Matthew Grissinger, RPh, FASCP
Mr. Grissinger is Director Around 3 a.m., a nurse hung the bag of into the automated compounder. The
of Error Reporting TPN. Around 6 a.m., the technician who pharmacy computer order entry system
Programs at the Institute prepared the TPN discussed the previous and the automated compounder used to
for Safe Medication evening’s work with the oncoming lead mix the TPN did not alert the pharmacist
Practices in Horsham, Pa. technician, noting the unusual prepara- that a 1,000-fold overdose had been en-
(www.ismp.org). tion of the TPN that required numerous tered into the systems for the zinc addi-
replenishments of the zinc syringe. The tive.
PROBLEM: An infant received a lethal latter technician checked the order, dis- 3. The TPN order was processed in
dose of zinc stemming from an error that covered the error, and alerted a pharma- the evening, when staffing was lim-
occurred during the order-entry process cist, who immediately called the unit to ited despite the hospital’s policy that
and compounding of a total parenteral stop the infusion. The pharmacist quickly TPN orders must be received and
nutrition (TPN) solution. Although the called Poison Control and searched the In- TPN solutions must be prepared be-
Institute for Safe Medication Practices ternet for treatment guidelines. fore 5 p.m. On the day of the error, the
(ISMP) was not privy to a full root-cause The infant received edetate calcium physician prescribed TPN at 4:30 p.m.,
analysis, details about this unfortunate disodium (calcium disodium versenate, or but the order was not scanned and trans-
event are presented in hopes that the les- calcium EDTA), which had been com- mitted to the pharmacy until after 5 p.m.
sons learned can be applied in hospitals pounded by an external pharmacy. The The pharmacist entered the order after
across the nation to prevent similar chelation therapy was unsuccessful, and 7 p.m., and the TPN solution was com-
mishaps. 1–3 the infant died. The coroner listed cardiac pounded later in the evening, when fewer
failure caused by zinc intoxication as the pharmacy staff members were available
TPN therapy was prescribed for a cause of death. to process complex orders. Staffing was
preterm infant born at 26 weeks of gesta- further reduced that evening because of
tion. On the day of the birth, the physician’s Several mistakes resulted in the fatal- the absence of a technician who usually
TPN order included directions to add zinc ity: compounded products.
in a concentration of 330 mcg/ 100 mL. Be- 4. Limited education and experi-
cause the automated compounder used 1. The method used to prescribe ence, along with ineffective compe-
for TPN required entry of zinc in a mcg/kg the zinc additive differed from the tency validation in compounding
dose, the pharmacist conver ted the method required to enter the order products, particularly for infants,
mcg/mL dose to a mcg/kg dose. She per- into the automated compounder soft- contributed to the technician’s failure
formed this calculation correctly but acci- ware program. This factor contributed to notice the TPN order entr y error.
dentally entered the zinc dose in the phar- to an order-entry error. The automated The technician who prepared the TPN
macy computer in mg , not mcg . This compounder required entry of the zinc did not have sufficient experience to
resulted in a final concentration of 330 additive in mcg/kg. A preprinted order appreciate the significance of the large
mg/100 mL—a 1,000-fold overdose. form was used to prescribe neonatal volume of zinc required by the auto-
Another pharmacist checked the work TPN. The usual TPN ingredients listed mated compounder to prepare the TPN.
and product labels that were printed for on the order form prompted the physi- Her prior training had consisted of a
preparation of the TPN, but she did not no- cian to prescribe doses by patient weight week of shadowing another technician.
tice the error involving the erroneous (e.g., mEq/kg, mg/kg). However, zinc During that period, she compounded
change from mcg to mg. A pharmacy tech- was not listed on the form, and the physi- fewer than 20 products using the auto-
nician prepared the TPN using a 500-mL cian wrote a free-text order for zinc, 330 mated compounder. In that time, she had
bag. The technician had to replenish the mcg/100 mL. The pharmacist had to con- never replenished a syringe on the com-
compounder syringe that contained zinc vert the dose to mcg/kg, after which she pounder. She thought it was unusual to
11 times while preparing the solution, mistakenly chose mg instead of mcg from replenish the zinc syringe 11 times dur-
which required dozens of vials of zinc sul- a pull-down list when entering the dose ing the course of making the TPN but did
fate. Several TPN additives had to be of zinc (the units of measure were next not mention this to a pharmacist. She
added manually, which the technician pre- to each other on the pull-down list). also did not question the need to use a
pared and brought to a third pharmacist to 2. Dosing alerts did not occur when 500-mL bag to make the TPN (normally,
check before adding them to the solution. the TPN order was entered into the a 250-mL bag is used for neonatal TPN).
The final TPN bag was then dispensed to pharmacy computer or when direc- Although staff members had raised
the neonatal intensive care unit (NICU). tions for preparation were scanned concerns about the technician’s level of
Vol. 36 No. 7 • July 2011 • P&T® 393
MEDICATION ERRORS
training, on the day of the error, the tech- fact that the TPN bag was unusually • needing to use more than a few
nician was asked to compound some large. dosage containers (tablets, cap-
products because the usual compound- sules, vials, or ampules) to prepare
ing technician was not available. SAFE PRACTICE RECOMMENDATIONS: or administer a single dose of any
5. The inexperienced technician Some strategies to prevent errors follow: drug
reported replenishing the zinc sy- • unexpected differences in the
ringe 11 times while compounding 1. Prescribing methods should be appearance of a drug or solution
the TPN to the lead technician the standardized. The method of ordering • other unusual circumstances
next morning but had not mentioned TPN solutions should be standardized regarding a drug or solution
her concern to the on-duty pharma- for neonates, pediatric patients, and • unexpected patient response to a
cist the previous evening. She re- adults so that each prescribed ingredient medication
ported feeling intimidated talking to the matches the dosing templates used for
pharmacist about a condition she con- entering the orders into the computer Technicians who compound products
sidered unusual, uncer tain about system and automated compounder. should be required to stop the process if
whether it signaled an actual error. She Preprinted forms or standard order sets they find that they need to add an elec-
believed that the pharmacist who en- should be used to list typical ingredi- trolyte or mineral in large doses or in
tered the order was correct and that she ents and to prompt the correct dosing large volumes in order to complete a sin-
should not question the pharmacist. method. On the rare occasions when cal- gle preparation. A full review of the work
6. Ineffective or nonexistent sys- culations are necessary, two clinicians label and order by a pharmacist should
tems for independent double-checks should be available to check the dose be required before the technician pro-
allowed the error to bypass at least independently and to compare their an- ceeds. Nurses who work in pediatric
six staff members without notice. At swers for verification. units and NICUs should question prod-
several points during dispensing and 2. Prescribing and transmitting ucts that are dispensed in larger quanti-
administration, pharmacists or nurses TPN orders should take place during ties than typically supplied for children or
checked the TPN orders and labels but the day. Policies that require prescribers neonates. A culture that encourages all
did not recognize the error. The first to order TPN during the day shift should staff, despite their level of experience or
check failed, primarily as a result of be established and enforced to maximize education, to speak up about unusual
human error, when the pharmacist who safety. The pharmacy staff should know conditions should be fostered.
compared the work and product labels which patients are receiving TPN and 6. Effective redundancies should
with the original order did not notice that should check whether orders have been be performed. Independent double-
the zinc dose was expressed in mil- received by the established deadline. checks should be conducted during
ligrams, not micrograms. 3. Manual-only additions of low- TPN-related dispensing and administra-
The next faulty check involved verify- volume ingredients should be al- tion processes. At least three verification
ing only the additives that had been lowed. For TPN ingredients that typi- processes should occur in the pharmacy:
added manually to the TPN. Hospital pol- cally require very small volumes, the
icy required pharmacists only to check staff should prepare, check, and inject • after initial order entry of TPN
the vials and syringes of the additives those ingredients manually. A trace ele- • before additives are injected manu-
against the label; they were not required ment such as zinc should not be allowed ally into the TPN
to compare the TPN product label with to be loaded onto a compounder for auto- • after TPN is compounded
the original order. To verify the additives, mated preparation.
the pharmacist looked at the identifying 4. Automated warnings must be For each verification, a pharmacist
information on the top of the label, then built and heeded. Automated dose-limit should compare the actual prescriber’s
skipped down to the bottom of the label warnings should be installed, tested, and order with the printed labels and the
to identify the additives to be added man- maximized in the pharmacy computer printed labels should be compared with
ually. As a result, he failed to read the system and automated compounders, the additives and final product. For veri-
middle of the label, which noted that particularly for high-alert medications fying the manual additives, the vials and
481.8 mL of zinc had been added to a bag such as TPN and its ingredients. All syringes that contain the additives
that contained 560 mL. alerts encountered during order entry should be inspected.
In the NICU, one nurse read the “num- could be printed so that the person The final verification of the com-
bers” associated with the dose for each checking it can also view and respond to pounded TPN should include a compre-
ingredient from the TPN label but not the the alerts. The importance of reading hensive review of the TPN order, the
units of measure (e.g., mg/kg, mg/dL) and reacting to the alerts should be re- product label, and the work label. Qual-
to another nurse, who was reading the inforced with all staff. ity-control checks and verification of re-
original order. Although the numbers 5. Suspicion of an error should be placement solutions on the compounder,
(including 330 for the zinc additive) raised. The following “red flags” should either manually or via bar coding, should
matched, again the accidental entry of be continually emphasized to trigger a be conducted, and an independent dou-
mg instead of mcg was not noticed. Many full review of the patient’s medications ble-check of any calculations should be
clues that indicated an error were over- and treatment plan to ensure that an made. Before administering TPN, two
looked during verification, including the error has not occurred: nurses should also independently com-
continued on page 409
394 P&T® • July 2011 • Vol. 36 No. 7
MEDICATION
ERRORS
continued from page 394
pare the label on the solution with the
physician’s order.
7. Education should be of fered,
and competency should be validated.
A formal training process should be es-
tablished for pharmacy staff members
who enter TPN orders into the pharmacy
computer, compound the solutions, or
check the products after preparation.
Selected staff members should be des-
ignated and trained to act as preceptors
to provide one-on-one supervision until
trainees are comfortable providing the
service and have demonstrated the skills
and knowledge necessar y to function
independently. Training should focus on
dosage and dose concentration, not just
the volume of additives, during solution
preparation.
If compounding services are provided
for neonatal and pediatric patients, age-
specific training that emphasizes weight-
based dosing should be included and the
competency of all staff who serve these
groups should be validated. Learning
modules and competency-validation tools
should be developed to expose trainees
to a broad spectrum of responsibilities
that they might not encounter during
their on-the-job orientation.
Acknowledgment: The ISMP thanks
the Nevada State Board of Pharmacy for
providing details of its investigation.
REFERENCES
1. Wells A. Error that led to baby’s death
slipped through many hands. Las Vegas
Review J August 5, 2007. Available at:
www.lvrj.com/news/8921512.html.
Accessed June 2, 2011.
2. Wells A. Answers bring more tears. Las
Vegas Review J, July 26, 2007. Available
at: www.lvrj.com/news/8723912.html.
Accessed June 2, 2011.
3. Nevada State Board of Pharmacy Order
of August 9, 2007. Available at: http://
bop.nv.gov/Minutes/2007/2007-07-25-
Minutes-BOP.pdf. Accessed June 2, 1011.
The reports described in this column were
received through the ISMP Medication
Errors Reporting Program (MERP). Errors,
close calls, or hazardous conditions may be
reported on the ISMP Web site (www.ismp.
org) or communicated directly to ISMP by
calling 1-800-FAIL-SAFE or via e-mail at
ismpinfo@ismp.org. I
Vol. 36 No. 7 • July 2011 • P&T® 409
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Metabical Case Study SolutionDocument4 pagesMetabical Case Study Solutionparoengineer100% (7)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 023-SOP For Conducting Hold Time StudyDocument3 pages023-SOP For Conducting Hold Time StudyAshok Lenka100% (2)
- Drugs Acting On GitDocument119 pagesDrugs Acting On GitNathaniel Mbiu Tim100% (1)
- 2017-06 NewsletterDocument5 pages2017-06 Newsletterapi-235801784No ratings yet
- Anti Scabies DrugsDocument4 pagesAnti Scabies DrugsNavjot Brar100% (2)
- NCP PneumoniaDocument47 pagesNCP Pneumoniabhevpat251100% (1)
- Nama Antibiotik Regimen Dosis Dosis Per-Hari Rute No Kode PasienDocument10 pagesNama Antibiotik Regimen Dosis Dosis Per-Hari Rute No Kode PasienAri AnggaraNo ratings yet
- Clinical PharmacyDocument38 pagesClinical PharmacyJurusan Farmasi Poltekkes MedanNo ratings yet
- At Home Steroid Testing GuideDocument11 pagesAt Home Steroid Testing GuideMyHomeTestingNo ratings yet
- USFDA Guidelines For PharmaceuticalsDocument5 pagesUSFDA Guidelines For PharmaceuticalsemranNo ratings yet
- Xenobiotic Metabolism PDFDocument50 pagesXenobiotic Metabolism PDFroxy8marie8chanNo ratings yet
- B Pharm 8 Sem Pharmalite - inDocument30 pagesB Pharm 8 Sem Pharmalite - inAnurag PatelNo ratings yet
- General PHARMAKOLOGY - Загальна фармакологія - Курс лекцій - изд.2005-215 сDocument219 pagesGeneral PHARMAKOLOGY - Загальна фармакологія - Курс лекцій - изд.2005-215 сSahil Saini100% (4)
- Olive Oil PEG-7 EstersDocument29 pagesOlive Oil PEG-7 EstersNurulNo ratings yet
- Syn 3 - Roche and Tamiflu-SG3Document29 pagesSyn 3 - Roche and Tamiflu-SG3Yani RahmaNo ratings yet
- Aripiprazole Lai Prescribing GuidelinesDocument8 pagesAripiprazole Lai Prescribing Guidelinestabic68932No ratings yet
- Common Drugs and Their Antidotes - PDF Version 1Document4 pagesCommon Drugs and Their Antidotes - PDF Version 1Maryam Khushbakhat50% (2)
- ChemDocument13 pagesChemKrislyn Joy FloresNo ratings yet
- 2 PirrolidonaDocument4 pages2 PirrolidonaAstrid Carolina Gutierrez ShimabukuroNo ratings yet
- Morocco Pharmaceuticals ReportDocument45 pagesMorocco Pharmaceuticals ReportGone Fishin100% (2)
- Drug and Alcohol Policy CAN enDocument43 pagesDrug and Alcohol Policy CAN enrv0014No ratings yet
- 1.2 Drug Devt and ProcessDocument14 pages1.2 Drug Devt and ProcessJohn King AmuraoNo ratings yet
- Research Paper About Herbal PlantsDocument8 pagesResearch Paper About Herbal Plantssvfziasif100% (1)
- Drug StudyDocument14 pagesDrug StudyNikki RodrigoNo ratings yet
- Stock Obat BPJS Desember 2017Document16 pagesStock Obat BPJS Desember 2017Vika FujiNo ratings yet
- Potassium Chloride - Uses, Dosage & Side EffectsDocument4 pagesPotassium Chloride - Uses, Dosage & Side EffectsKenneth Mark B. TevesNo ratings yet
- Chapter 11 Multiple Dosage RegimenDocument35 pagesChapter 11 Multiple Dosage RegimenYuli Irvaransiah DIatun NIkmah100% (2)
- Auto ClaveDocument4 pagesAuto ClaveSarah Swasti PNo ratings yet
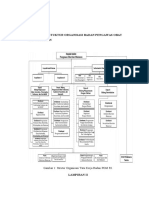
- Lampiran 1: Stuktur Organisasi Badan Pengawas Obat Dan MakananDocument13 pagesLampiran 1: Stuktur Organisasi Badan Pengawas Obat Dan MakananmeilaNo ratings yet
- Ketoconazole Cream Clinical ParticularsDocument2 pagesKetoconazole Cream Clinical ParticularsJai MurugeshNo ratings yet