Professional Documents
Culture Documents
Post Stroke Seizure
Post Stroke Seizure
Uploaded by
hadiatussalamah0 ratings0% found this document useful (0 votes)
12 views7 pagesCopyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
12 views7 pagesPost Stroke Seizure
Post Stroke Seizure
Uploaded by
hadiatussalamahCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 7
SECTION FDITOR: DAVID E PLEASURE. MD
Poststroke Seizures
Isaac E. Silverman, MD; Lucas Restrepo, MD; Gregory C. Mathews, MD, PhD
troke is the most common cause of seizures in the elderly, and seizures are among the most
common neurologic sequelae of stroke. About 10% of all stroke patients experience sei-
zures, from stroke onset until several years later. This review discusses current understand-
ing of the epidemiology, pathogenesis, classification, clinical manifestations, diagnostic stud-
ies, differential diagnosis, and management issues of seizures associated with various cerebrovascular
lesions, with a focus on anticonvulsant use in the elderly: Arch Neurol. 2002;59:195-202
EPIDEMIOLOGY
In population studies, stroke is the most
commonly identified cause of epilepsy in
adult populations older than 35 years." In
the elderly, stroke accounts for more than
half of the newly diagnosed cases of epi-
lepsy in which a cause is determined, ahead
of degenerative disorders, brain tumors, and
hhead trauma.’ From stroke registry data
shout 59% to 20% of ll individuals who have
stroke will have subsequent seizures but
epilepsy (recurrent seizures) will develop
{monly a small subset of this group. Given
that, in each year, more than 730000 people
im this country have a stroke, a conserva-
Uiveincidence of seizures alter stroke is about
36500 new cases per year
The largest and most rigorous meth-
odological attempt to examine poststroke
seizures was the prospective mullicenterre-
port from the Seizures After Stroke Study
Group. The study enrolled 1897 patients
and found an overall incidence of seizures
of 8.0%, Recurrent seizures consistent with
the development of epilepsy wet
curring in 25% ofthe patients, but the mean
follow-up was only 9 month
Seizures may bea more common ac-
companiment of hemorrhagie rather than
ischemic stroke.
bladin ct al found the incidence of sei
sures tobe 10,6%among 265 patients with
sntracerebral hemorehage vs 86% among
1632 with ischemic stroke. Ia another
prospective series,’ seizures occurred in
444% of 1000 patients, including 15.43% ith
lobar or extensive intracerebral hemor-
rhage, 8.5% with subarachnoid hemor
hage, 6.5% with cortical infarction, and
3.7% with hemispheric transient ischemic
altacks. 4 seizure was the presenting (
ture of intracranial hemorrhage in 30% of
1402 patients Among 95 patients with an-
curysmnal subarachnoid hemorrhage, the
fncidence rate of prchospital seizures was
higher (17.9%) than that occuring i the
hospital (4.19%)."
CLASSIFICATION AND.
PATHOGENESIS
Seizures after stroke are classified as early
or late onset, according to their timing af
ter brain ischemia, ina paradigm compa-
rable to post-traumatic epilepsy.*7 An
arbitrary cut point of 2 weeks after the pre-
senting stroke has been recognized to dis-
nguish between early- and late-onset
poststroke seizures.”"® Different charac-
{eristics and mechanisms of poststroke se
ures, according to their proximity to the
onset of brain ischemia, have heen pro-
posed, but no clear pathophysiologtcal
basis exists for the 2-week cut point
Most early-onset seizures occur dur-
ing the first 1 to 2days after ischemia. Al-
From The Stroke Center at Hartford Hospital, Hartford, Conn (Dr Silverman); the
{Cerebrovascular Program (Dr Restrepo) and The Johns Hopkins Epilepsy Center
(Dr Mathews), Department of Neurology, The Jos Hopkins University School of
‘Medicine, Balimore, Bd: and the Synaptic Physiology Unit, National Institute of
[Neurological Disorders and Stroke, ethesda, Md (Dr Mathews).
(©2002 American Med
1 Association, All rights reserved.
most half (43%) of all patients in the Stroke After Sel-
“ares Study experienced a setzure within the first 24 hours
alter stroke In a series restricted to early-onset sei-
‘zures, 00% of the 30 patients had ictal activity within the
first 24 hours."® Most seizures associated with hemor-
rhagie stroke also aceur at onset or within the first 24
hours."
During acute ischemic injury, accumulation of in-
tracellular caleium and sodium may result in depolar-
ization of the transmembrane potential and other ealeiurn-
mediated effects. These local ionic shifts may lower the
seizure threshold.* Glutamate excitotoxicity is a well-
established mechanism of cell death in the experimen-
tal stroke model. Antiglutamatergic drugs may also have
‘4 neuroprotective role in ischemic settings, aside from,
the role of treating seizures.
The size of regional metabolic dysfunction may also
bbe relevant in causing early-onset seizures. In the setting
‘of large regions of ischemic hypoxia, high levels of exct-
totoxie neurotransmitters may be released extracellu-
larly. tn studies of the postischemic brain in experimen-
talanimal models, neuronal populations i the neocortex”
and hippocampus" have altered membrane properties and
increased excitability, which presumably lower the thresh-
‘old for seizure initiation, The ischemic penumbra, a re
‘gion of viable issue adjacent to the infarcted core in is
cchemic stroke, contains electrically irritable tissue that may
bbe a focus for seizure activity
In addition to focal ischemia, global hypoperfusion,
‘can cause seizure activity. Hypoxic-ischemic encepha-
lopathy is one of the most common causes of status epi-
lepticus and carries a poor prognosis, Particularly vul-
nerable to ischemic insult is the hippocampus, which is
‘an especially epileptogenic area
In late-onset seizures, by contrast, persistent changes
in neuronal excitability occur. Replacement of healthy
cell parenchyma by neuroglia and immune cells may play
‘role in maintaining these changes. A gliotic scarring has
‘been implicated as the nidus for late-onset seizures, just
4s the meningocerebral cieatrix may be responsible for
late-onset post-traumatic epilepsy
‘An underlying permanent lesion appears to ex-
plain the higher frequency of epilepsy in patients with
late- than early-onset seizures. Asin post-traumatic epi-
lepsy,! late aceurrence ofa first seizure appears to carry
«shigher risk for epilepsy. In patients with ischemic stroke,
epilepsy developed in 35% of patients with early-onset
seizures and in 90% of patients with late-onset sei-
ures." The risk for epilepsy was comparable in pa-
tients with hemorrhagic stroke; epilepsy developed in 2%
of patients with early-onset seizures vs 03% with late
The concept that cardiogenic emboli to the brain are
more likely to cause seizures acutely iscontroversial, with
few supporting data. Among 1640 patients with cere-
bral ischemia," events attributed to a cardiae source were
most commonly associated with early-onset seizures
(26.6%), even compared with supratentorial hemato-
mas (162%). However, the definition of cardiogenic
mechanisin in this series was often based on nonspe-
cific criteria, Several authors have questioned the asso-
ciation of seizures with cardioembolic events." Sei-
(©2002 American Med
zures at onset were not a criterion in a data bank study
of the cardiac causes of stroke." Intuitively, there is no
reason to suspect that cardigembolie lesions would be
more likely than emboli from large-vessel sources to cause
seizures, as eardiac and large-vessel emboli frequently in-
volve lesions to distal cortical branches. The mecha-
nism by which cortical emboli preeipitate seizures is un-
certain," but possibilities include depolarization within
an ischemic penumbra, rapid reperfusion after the frag-
‘mentation and distal migration ofthe embolus,” ora com
bination of both.
Cortical location isamong the most reliable risk fae-
tors for poststroke seizures. Poststroke seizures were more
likely to develop in patients with larger lesions involv-
ing multiple lobes ofthe brain than in those with single
lobar involvement.® However, any'stroke, including those
with only subcortical involvement, may occasionally be
associated with seizures» Earlier studies, relying on less
sensitive neuroimaging techniques, may not have de-
tected concomitant small cortical lesions that could cause
ictal activity. The mechanism by which deep hemi-
spheric subcortical lesions, most commonly due to small-
vessel disease, cause seizures is not understood.”
‘Analogous to cortical involvement in ischemic stroke,
a lobar site is considered to be the most epileptogenic lo-
cation in patients with intracerebral hemorrhage. Ina se-
ries of 123 patients,” seizure incidence was highest with
bleeding into lobar cortical structures (54%), low with
basal ganglionic hemorrhage (199%), and absent with tha-
lamic hemorrhage. Caudate involvement ofthe basal gan-
glia and temporal or parietal involvement within the cor-
tex predicted seizures.” Hemorthage due to cerebral
venous thrombosis also commonly presents with sei-
zures. Parenchymal, often cortieal, hemorrhage resull-
ing from local venous congestion isthe likely cause of
seizure activity
The mechanism of seizure initiation by hemorrhage
fs not established. Products of blood metabolism, such as
hhemosiderin, may eause «focal cerebral irritation leading
to seizures, analogous to the animal model of focal epi-
lepsy produced by iron deposition on the cerebral cor-
tex." In subarachnoid hemorthage, there is often exten-
sive hemorrhage into the basal cisterns, which direetly
contacts the frontal and temporal lobes. Patients with sub-
arachnoid hemorrhage also may have an intraparenchy-
‘mal component to the hemorrhage (Figure 1).
The only’ clinical predictor for seizures alter ische-
rie stroke isthe severity of the initial neurologic deficit.
Greate initial stroke severity” or stroke disability: pre-
dicted seizures. By contrast, in the Oxfordshire Commu-
nity Stroke Project, only 3% of 225 patients who were in-
dependent 1 month after a stroke experienced a seizure
between 1 month and 5 years. Patients presenting with
greater neurologic impairment tend to have larger strokes
that involve wider cortical areas
‘In retrospective studies, risk factors for seizures af-
ter subarachnoid hemorthage included middle cerebral
artery aneurysms,” intraparenchymal hematoma,”
rebralinfaretion,”*a history of hypertension.” and thick-
ness of the cisternal clot." By contrast, clinical predic-
tors forseizures alter intraparenchymal hemorthage have
been lacking.
1 Association, All rights reserved.
eae a egal
Fare one
vay
THR r
ae [
ChE aban
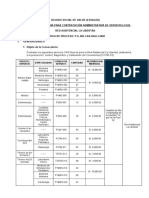
Figure 1. Sevres after intracerebral and sbarachnodhemarthage An 2-ya-od woman presented with sudden-onsat headache, dysphasa and ight
hemiparesis hie rcehing antecaglatn thrpy for choi ta filter Computed anograpi (CT) scan at admission A) damonstates an aut et
{umporal lobe ntaparenchymal hams, vith adjacent eur a subaachnadhemerroge The respenibl leon, an aneurysm te mid abr
ty, was wate sural. During the postopera ped, she ad ep
hemisphere. et inde rtrence
Vascular lesions may cause seizures by other mechs-
nisms. Seizures die to arteriovenous malformations and
aneurysms typically occur when these lesions rupture,
but these vascular lesions may cause seizures by di-
rectly irritating adjacent brain parenchyma (Figure 2)
Finally, seizures associated with vascular lesions oc-
‘cur in the setting of significant reperfusion after revasci-
larization procedures, most commonly carotid endarter-
‘ectomy for chronic severe extracranial catotid stenosis, The
5 of right-sided facal wing assocated wih anton worsening lhe aphasia
(CT scan 3 mri tr (6) showed 2 hypadance sion a the mtrpoal le inthe mil cranial fossa. Ele
onataed focal sie waves, consent th seizure act, flawed by focal slowng and proc erazingepepiorm discharge inet
capalographi (EEG).
reperfusion syndrome, first described by Sundt and col-
leagues.” includes transient focal seizure activity, atypical
‘migrainous phenomena, and intracerebral hemorrhage, al-
though the clinical triad is often incomplete. Onset ofthis
rare syndrome ranges from several days to 3 weeks alter
revascularization® and often is signaled by a new ipsila
cral headache.” Surgical conection ofan arteriovenous mal-
formation may also cause intraoperative oF postoperative
hyperemia, with subsequent seizures or hemorrhage."
Figure 2. Mass lesion causing oa seizures. 8-yar-old woman
presantedt the amargancy department afr fecal anstght-sied loi
Imovemens, alowed by lesa consciousness. Computed fmegspic
‘Stan with contrast mans a giant anourysm of the mi cerebral
Str wih adjacent coer adaa, corre pt ot the aur, nd
Shaan raion whch trom has formed The patent unde
‘ces crantomy. wth thambetemy and aneurysm cing.
By contrast, arteriovenous malformations located in border-
zone regions subject. relatively low flow rates have a lower
risk for hemorrhage.”
The reperfusion syndrome has been attributed to im-
paired cerebral autoregulation.” In the setting of chronic
hypoperfusion due to high-grade carotid stenosis, the ar-
terioles responsible for normal autoregulation in the
downstream cerebral hemisphere become chronically di-
lated. Subsequently, when perfusion is improved by are
vascularization procedure, the vessels are incapable of
vasoconstriction, and the brain parenchyma is sub-
jected to a massive augmentation of blood flow. The re-
lease of vasoactive neuropeptides from perivascular sen-
sory nerves may contribute to the development of the
reperfusion syndrome,” to oxidants that develop before
revascularization,” and to an inflammatory response to
the reestablishment of circulation.”
(CLINICAL MANIFESTATIONS
Given that most poststroke seizures are caused by a fo-
cal lesion, poststroke seizures are typically focal at on-
set. In a study of early-onset seizures in 90 patients,
‘imple partial seizures were the most common type (61%),
followed by secondarily generalized seizures (289%). In
other series," early-onset seizures were more likely to
be partial, whereas late-onset seizures were more likely
to generalize secondarily. Most recurrent seizures are of
the same type as the presenting episode, and they tend
to recur within 1 year on average
In a large series of patients with poststroke sei-
‘zures, 9% had status epilepticus.” The only associated,
finding was higher functional disability; status epilepti-
‘cus was not associated with higher mortality rate, stroke
(©2002 American Medi
ype (ischemic or hemorrhagic), topography (cortical in-
volvement), lesion size, or eectroencephalographic (EEG)
patterns,
The phenomenological features of the reperfusion,
syndrome are similar in that focal onset with occasional
secondary generalization is the rule. Seizure activity
always oceurs in the ipsilateral vascular territory of the
surgically treated internal carotid artery.® Occasion-
ally, status epilepticus ensues (Figure 3)
DIAGNOSTIC STUDIES
Holmes found that patients with periodic lateralizing
epileptiform discharges and bilateral independent pe
codkic lateralizing epileptiform discharges on EEG alter
stroke were especially prone to the development of sei
ures, Those patients with focal spikes also had a high
risk of 75%. Focal slowing, diffuse slowing, and normal
findings on EEG, by contrast, were associated with rela-
Lively low risks of 20%, 10%, and 5%, respectively. Other
work found that cortical involvement on results of
neuroanatomical imaging studies was more predictive
of epilepsy than any single EEG finding,"
Focal slowing on EEG may simply reflect a wide re-
gion of ischemic or infarcted tissue involving the cer
bral cortex or subcortical territory. In addition to neu-
roimaging, EEG may be helpful in the early evaluation
of poorly defined poststroke focal neurologic symp-
toms. Inselected patients, focal slowing may confirm the
clinical impression of hemispheric ischemia and argue
against ongoing seizures as an explanation for an acute
neurologic syndrome, The absence of EEG abnormal
ies does not definitively exclude cerebral ischemia, par-
Uicularly in subcortical or subtentorial structures, oF
Uncommon
faction on neuroimaging findings. Lansberg etal” recently
described several actite magnetic resonance imaging find-
{ngs in 3 patients with partial status epilepticus. Thesestud-
les showed cortical hyperintensity on diffusion-weighted
imaging and T2-weighted sequences and a corresponding,
area of low apparent diffusion coefficient. However, these
findings were readily differentiated from typical ischemic
stroke in their nonvascular distributions, increased signal
of the ipsilateral middle cerebral artery on magnetic reso-
nance angiography, atid leptomeningeal enhancement on
posicontrast magnetic resonance imaging. Another study
showed a hyperintensity on dilfusion-weighted images in
the dorsolateral portion of the ipsilateral thalamus in 2
patients (Figure 3).""
seizures may mimic ischemia and in-
DIFFERENTIAL DIAGNOSIS
The differential diagnosis of ischemia-induced seizures in-
cludes secondary seizures due to other causes, Medica-
tions, drug therapy withdrawal (eg, benzodiazepines), and
metabolic disturbances (eg, glucose abnormalities) typi-
cally cause generalized seizures, unless an underlying le-
sion is already present. Migraine-related focal phenom-
ena and transient ischemic attacks may produce focal
slowing on EEG findings. Among these entities, glucose
abnormalities should not be overlooked
1 Association, All rights reserved.
a Facey nero
fon J
Frm
Tr
01 hs
mie
Ra
ar 7
pot
rem “
rary, ee k
rare) |p ee ' t
poe el etn
Bet oR BCE
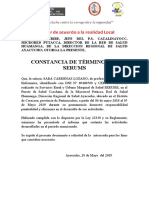
Figure 3. Satu eplepicus dt th repartusion syndrome. 65-year-old onan underwent an athervise uncompllatd right cared endartractomy for
‘Seymptomatic extcranl cr artery dace 3 cys cri. She awoke witha headache flan ylet-arm clan movement. These progressed o
(zteralaed, tonic-clonic sours, which wor not bora by adrinstaton of loazapam and phonon sodium ray. The contruousslecomeephalograpic
{E25} maniar shove perdi stead eploporndschargs occuring every 2b 9 rues, sing ae scores (A). Subsoquant 12- and
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Formato1 2Document6 pagesFormato1 2GustavoZapataNo ratings yet
- Flash ENAM - Examen Simulacro - Resolución - OnlineDocument9 pagesFlash ENAM - Examen Simulacro - Resolución - OnlineGustavoZapataNo ratings yet
- Enlace Mundial Empresa Nro 1Document5 pagesEnlace Mundial Empresa Nro 1GustavoZapataNo ratings yet
- Ba 002 Cas Ralli 2020Document12 pagesBa 002 Cas Ralli 2020GustavoZapataNo ratings yet
- Eco Tour Machu Picchu Empresa Nro 3 Parte 1Document3 pagesEco Tour Machu Picchu Empresa Nro 3 Parte 1GustavoZapataNo ratings yet
- RM 20 F1 - Cardiología 2 - OnlineDocument32 pagesRM 20 F1 - Cardiología 2 - OnlineGustavoZapataNo ratings yet
- Viaje Peru Tours Empresa Nro 2Document5 pagesViaje Peru Tours Empresa Nro 2GustavoZapataNo ratings yet
- RM 20 F1 - Cardiología 1 - Online-DesbloqueadoDocument27 pagesRM 20 F1 - Cardiología 1 - Online-DesbloqueadoGustavoZapataNo ratings yet
- RM 20 F1 - Cardiología 2 - Online-DesbloqueadoDocument32 pagesRM 20 F1 - Cardiología 2 - Online-DesbloqueadoGustavoZapataNo ratings yet
- DynaMed Plus - Enteric Fever (Typhoid and Paratyphoid Fever)Document26 pagesDynaMed Plus - Enteric Fever (Typhoid and Paratyphoid Fever)GustavoZapataNo ratings yet
- HUANTADocument4 pagesHUANTAGustavoZapataNo ratings yet
- Flashcards 2Document28 pagesFlashcards 2GustavoZapataNo ratings yet
- 4 - Traumatismo AbdominalDocument3 pages4 - Traumatismo AbdominalGustavoZapataNo ratings yet
- Flashcards 3Document6 pagesFlashcards 3GustavoZapataNo ratings yet
- 6) Dr. Vargas - Patología Benigna y Maligna de Tiroides y ParatiroidesDocument4 pages6) Dr. Vargas - Patología Benigna y Maligna de Tiroides y ParatiroidesGustavoZapata100% (1)
- Traumatismos y FX MaxilofacialDocument5 pagesTraumatismos y FX MaxilofacialGustavoZapata100% (1)