Professional Documents
Culture Documents
Pregnancy Exercise and Nutrition With Smartphone.10
Pregnancy Exercise and Nutrition With Smartphone.10
Uploaded by
Diego BelloOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pregnancy Exercise and Nutrition With Smartphone.10
Pregnancy Exercise and Nutrition With Smartphone.10
Uploaded by
Diego BelloCopyright:
Available Formats
Original Research
Pregnancy Exercise and Nutrition With
Smartphone Application Support
A Randomized Controlled Trial
Maria A. Kennelly, MRCPI, Kate Ainscough, MSc, Karen L. Lindsay, PhD, Elizabeth O’Sullivan, PhD,
Eileen R. Gibney, PhD, Mary McCarthy, PhD, Ricardo Segurado, PhD, Giuseppe DeVito, PhD,
Downloaded from http://journals.lww.com/greenjournal by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdtwnfKZBYtws= on 10/01/2021
Orla Maguire, PhD, Thomas Smith, PhD, Mensud Hatunic, MD,
and Fionnuala M. McAuliffe, MD, FRCOG
OBJECTIVE: To evaluate the effect of a healthy lifestyle 506 women would be required to have 80% power to
package (an antenatal behavior change intervention detect this effect size at a significance of .05, that is,
supported by smartphone application technology) on 253 in each group.
the incidence of gestational diabetes mellitus (GDM) in RESULTS: Between March 2013 and February 2016, 565
overweight and obese women. women were recruited with a mean BMI of 29.3 and
METHODS: Women with body mass indexes (BMIs) 25– mean gestational age of 15.5 weeks. The incidence of
39.9 were enrolled into this randomized controlled trial. GDM did not differ between the two groups, 37 of 241
The intervention consisted of specific dietary and exer- (15.4%) in the intervention group compared with 36 of
cise advice that addressed behavior change supported by 257 (14.1%) in the control group (relative risk 1.1, 95% CI
a tailor-designed smartphone application. Women in the 0.71–1.66, P5.71).
control group received usual care. The primary outcome CONCLUSIONS: A mobile health-supported behavioral
was the incidence of GDM at 28–30 weeks of gestation. intervention did not decrease the incidence of GDM.
To reduce GDM from 15% to 7.2%, we estimated that
CLINICAL TRIAL REGISTRATION: ISRCTN registry,
https://www.isrctn.com/, ISRCTN29316280.
From the UCD Perinatal Research Centre, Obstetrics and Gynaecology, School of
Medicine, the UCD Institute of Food and Health, UCD CSTAR, and the School (Obstet Gynecol 2018;131:818–26)
of Public Health, Physical & Sports Sciences, Health Sciences Centre, University DOI: 10.1097/AOG.0000000000002582
College Dublin, Dublin, the Department of Management & Marketing, Univer-
G estational diabetes mellitus (GDM) is “glucose
sity College Cork, Cork, and the Department of Endocrinology, St. Vincent’s
University Hospital, and the Department of Endocrinology, National Maternity
Hospital, Dublin, Ireland. intolerance first recognized during pregnancy”1
This trial was funded by the National Maternity Hospital medical fund. The
and is associated with up to a 70% risk of type 2
funding source did not have a role in the trial design or manuscript preparation. diabetes in later life.2 A family history of type 2 dia-
Presented at the Society for Reproductive Investigation, March 15–18, 2017, betes, maternal adiposity, and excess gestational
Orlando, Florida; and at the British Society for Maternal Fetal Medicine, March weight gain seem to confer the greatest risk.3,4 Despite
30–31, 2017, Amsterdam, the Netherlands. pregnancy being considered a “teachable moment,”
The authors thank the mothers of the National Maternity Hospital who partic- overweight and obese women often find it difficult
ipated in the study.
to change dietary and physical activity behaviors dur-
Each author has indicated that he or she has met the journal’s requirements for
authorship.
ing pregnancy.5 Recently published studies describing
combined nutrition and exercise interventions have
Corresponding author: Fionnuala M. McAuliffe, FRCOG, FRCPI, Chair and
Professor of Obstetrics & Gynaecology, University College Dublin Head, reported only some success in reducing GDM.2,6–9
Women’s and Children’s Health, University College Dublin University College The reason for this could be attributed to the lack of
Dublin, National Maternity Hospital, Holles Street, D2, Dublin, Ireland; email: emphasis on psychologic theories in their methodol-
fionnuala.mcauliffe@ucd.ie.
ogies that are imperative for changing lifestyle behav-
Financial Disclosure
The authors did not report any potential conflicts of interest. iors in an already potentially unmotivated group.
Therefore, it is now recommended that lifestyle inter-
© 2018 by American College of Obstetricians and Gynecologists. Published by
Wolters Kluwer Health, Inc. All rights reserved. ventions should incorporate behavior change theories
ISSN: 0029-7844/18 into study design and methodology.10
818 VOL. 131, NO. 5, MAY 2018 OBSTETRICS & GYNECOLOGY
Copyright Ó by American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
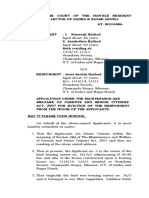
Fig. 1. Consolidated Standards of Reporting Trials flow diagram. BMI, body mass index; OGTT, oral glucose tolerance test.
Kennelly. Pregnancy Exercise and Nutrition. Obstet Gynecol 2018.
Mobile health or “mHealth” technologies are trial steering committee met bimonthly. An indepen-
becoming commonplace to assist in the management dent data monitor reviewed recruitment and safety data
of chronic illnesses and support behavior change.11 after 250 patients had been enrolled.
Considering that more than 70% of Irish pregnant Details of the full study protocol, including
women use smartphones,12 mobile health offers an eligibility criteria, recruitment and enrollment, and
opportunity to improve health behaviors in preg- data collection, have been previously published.14
nancy. This article describes a multifaceted “healthy Briefly, singleton pregnant women between 10 and
lifestyle package” for overweight and obese pregnant 15 weeks of gestation with body mass indexes (BMIs,
women, consisting of personalized low glycemic calculated as weight (kg)/[height (m)]2) between 25.0
index nutritional and physical activity advice under- and 39.9 and in possession of a smartphone were re-
pinned by behavior change theories with reinforce- cruited at their first antenatal visit. Participants re-
ment through a specifically designed smartphone turned for their first study visit within 2 weeks for
application. We hypothesized that this lifestyle inter- randomization to either the intervention or control
vention would reduce the incidence of GDM per the group. Randomization was performed using a com-
International Association of Diabetes and Pregnancy puter-generated sequence in a ratio of one to one.
Study Group diagnostic criteria.13 The biostatistician prepared sequentially numbered,
sealed opaque envelopes, which were opened at the
MATERIALS AND METHODS first study visit. Randomized participants were strati-
This was a single-center randomized controlled trial fied by BMI to ensure equal numbers of overweight
with ethical approval and maternal written consent and obese women in each group. As a result of the
conducted at the National Maternity Hospital, Dublin, nature of the intervention, neither participants nor
Ireland. Recruitment ran from March 2013 to February researchers were blinded to the intervention or
2016. The final delivery occurred in August 2016. The outcomes.
VOL. 131, NO. 5, MAY 2018 Kennelly et al Pregnancy Exercise and Nutrition 819
Copyright Ó by American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 1. Characteristics of Participants at Baseline
Characteristic Intervention Group (n5278) Control Group (n5287)
Age (y) 32.864.6 32.164.2
Nulliparous 138 (49.6) 154 (53.7)
Multiparous 140 (50.4) 133 (46.3)
Height (cm) 164.266.5 163.9611.9
Weight (kg) 79.5611.3 78.6611
BMI (kg/m2) 29.4263.6 29.1263.3
BMI category
Overweight (25–29.9) 182 (65.5) 194 (67.6)
Obese class I (30–34.9) 68 (24.4) 67 (23.3)
Obese class II (35–39.9) 28 (10.1) 26 (9.1)
Midupper arm circumference (cm) 31.462.8 31.362.8
Educational attainment
Some high school 7/262 (2.7) 6/277 (2.2)
Completed high school or 35/262 (13.4) 35/277 (12.6)
its equivalent
Some college education 67/262 (25.6) 46/277 (16.6)
Completed college education 153/262 (58.4) 190/277 (68.6)
Family history of type 2 DM 55 (19.8) 64 (22.3)
Ethnicity
Caucasian 259 (93.2) 256 (89.2)
Non-Caucasian 19 (6.8) 31 (10.8)
Glycemic index* 58.864.8 58.764.9
Glycemic load 134.9636.5 136636.3
Physical activity (METS)† 518.96496.3 507.46442.6
DM, diabetes mellitus; METS, metabolic equivalent of task.
Data are mean6SD or n (%).
P values calculated by independent-samples t tests or x2 tests.
* Dietary data available for 224 women in the intervention group and 210 in the control group at baseline.
†
Physical activity data available for 228 women in the intervention group and 236 in the control group.
Women allocated to the control group received this education session was reinforced through the fol-
standard antenatal care, which in Ireland does not lowing delivery channels: a smartphone application,
consist of any uniform advice on diet, exercise, or emails every 2 weeks (sent by the research team), and
weight gain in pregnancy. Participants allocated to the two follow-up face-to-face hospital visits at 28 and 34
intervention group received standard antenatal care weeks of gestation. The content of the emails were
plus a “Healthy Lifestyle Package.” The “Healthy standardized to a specific theme on a 2-week basis with
Lifestyle Package” began with a single face-to-face some discourse between the researchers and partici-
education session conducted individually or in pairs. pants where individuals had specific questions. The
This education session was delivered at the first study specifically designed smartphone application was
visit and centered on targeted nutrition and physical downloaded during the education session from the
activity advice. The nutritional component of the iTunes or Google player website free of charge and con-
intervention focused on healthy eating in pregnancy. sisted of three components: a comprehensive database of
Participants were encouraged to swap high glycemic low glycemic index recipes, an exercise advice section,
index foods for low glycemic index alternatives and and a homepage comprising daily nutritional and exer-
were informed about healthy carbohydrate portions. cise tips and an encouraging thought of the day. Focus
The recommended diet was approximately eucaloric groups conducted before study inception guided the con-
to their typical diet.15 The exercise component of the tent and design of the application (see Appendix 1, avail-
intervention focused on promoting the benefits and able online at http://links.lww.com/AOG/B90). The
safety of physical activity in pregnancy. Women were education session and its delivery channels were
advised to exercise per the American College of Ob- informed by two main behavior change theories: control
stetricians and Gynecologists’ guidance,16 that is 30 mi- theory and social cognitive theory.18,19 Goal setting for
nutes of moderate exercise 5–7 days per week, divided dietary and exercise targets was individualized and based
into two 15-minute or three 10-minute periods to max- on the “SMART” (Specific, Measurable, Achievable,
imize metabolic benefit.17 The information received at Relevant, and Time-specific) goals principle.18
820 Kennelly et al Pregnancy Exercise and Nutrition OBSTETRICS & GYNECOLOGY
Copyright Ó by American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 2. Maternal Primary and Secondary Outcomes
Control Mean
Intervention Group Risk Ratio Difference Adjusted
Outcome Group (n5278) (n5287) (95% CI) (95% CI) P P
Primary outcome
GDM 37/241 (15.4) 36/257 (14) 1.1 (0.71– — .71
1.66)
Secondary outcomes
Gestational weight gain results
Baseline to 34 wk of gestation (kg) 8.964.8 1064.8 — 21.08 (21.96 to .015 .13
20.21)
Baseline to term (kg) 11.365.6 12.665.6 — 21.3 (22.49 to .027 .13
20.15)
Physical activity postintervention— 638.76436.4 464.86328 — 174 (0.04–0.17) .001 .02
METS*
Glycemic index postintervention† 56.464.5 57.964.8 — 21.47 (22.56 to .009 .13
20.37)
Glycemic load postintervention 117.5633.4 131.7636.1 — 214.24 (222.3 to .001 .02
26.19)
Exploratory analyses
OGTT results at 28 wk of gestation
(mmol/L)†
Fasting glucose, mmol/L (mg/dL) 4.4360.58 4.4360.55 — 20.002 (20.1 to .95 .95
(79.7610.4) (79.769.9) 0.09)
Glucose 1-h pp, mmol/L (mg/dL) 7.3661.9 7.4261.8 — 20.06 (20.39 to .72 .81
(132.5634) (133.6632) 0.27)
Glucose 2-h pp, mmol/L (mg/dL) 5.8161.4 5.7461.3 — 0.08 (20.16 to .52 .71
(104.4625) (103.3623) 0.31)
IOM GWG guidelines
Below guidelines 29 (17.0) 28 (14.9) 0.84 (0.56–
1.26)
Met guidelines 55 (32.2) 40 (21.3) Reference — .03 .13
Exceeded guidelines 87 (50.9) 120 (63.8) 0.82 (0.70– —
0.96)
Safety analyses
Labor and delivery outcomes (n5270) (n5275)
PET or PIH 22 (8.1) 15 (5.5) 1.4 (0.79– — .21
2.81)
Onset of labor
Spontaneous 143 (53) 156 (56.7) Reference — .56
Induction 93 (34.4) 83 (30.2) 1.13 (0.90– —
1.44)
Cesarean delivery as primary 34 (12.6) 36 (13.1) 1.02 (0.67– —
procedure 1.56)
Duration of labor (min) 258.76219.8 250.96207 — 7.8 (20.08 to .80
0.11)
Epidural 129 (47.8) 141 (51.3) 0.93 (0.78– — .44
1.1)
3rd-degree tear 4 (1.5) 4 (1.5) 1.02 (0.25– — 1.00
4.03)
Mode of delivery
Spontaneous vaginal 168 (62.2) 167 (60.7) Reference — .95
Instrumental 28 (10.4) 32 (11.6) 0.89 (0.56– —
1.42)
Elective cesarean 24 (8.9) 23 (8.4) 1.03 (0.60– —
1.76)
Emergency cesarean 50 (18.5) 48 (17.5) 1.03 (0.73– —
1.46)
Maternal metabolic parameters
Fasting glucose (mmol/L)
Baseline (mg/dL) 81.769 80.569 — 1.3 (20.4 to 2.9) .13
28 wk of gestation (mg/dL) 79.7610.8 79.769 — 20.1 (21.8 to 1.6) .95 1.00
Difference from baseline to 28 wk of 22.265.9 20.965.4 — 21.1 (22.2 to .02 .13
gestation (mg/dL) 20.1)
(continued )
VOL. 131, NO. 5, MAY 2018 Kennelly et al Pregnancy Exercise and Nutrition 821
Copyright Ó by American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 2. Maternal Primary and Secondary Outcomes (continued )
Control Mean
Intervention Group Risk Ratio Difference Adjusted
Outcome Group (n5278) (n5287) (95% CI) (95% CI) P P
Insulin (pmo/L)
Baseline 65629.3 65.4640.5 — 20.51 (26.71 to .87
5.7)
28 wk of gestation 90647.2 98679.5 — 28.1 (220.3 to .19 .48
4.1)
Difference from baseline to 28 wk of 24.3631 35.9672.7 — 211.6 (222.4 to .03 .13
gestation 20.73)
C-peptide (nmol/L)
Baseline 0.4860.24 0.6360.73 — 20.001 (20.04 to .59
0.04)
28 wk of gestation 0.6360.33 0.6860.33 — 20.04 (20.1 to .21 .50
0.02)
Difference from baseline to 28 wk of 0.1460.29 0.2160.33 20.069 (20.13 to .03 .13
gestation 0.008)
HOMA2-IR index
Baseline 1.1960.54 1.1560.53 — 0.03 (20.06 to .48
0.13)
28 wk of gestation 1.6160.81 1.6760.84 — 20.05 (20.21 to .45 .71
0.09)
Difference from baseline to 28 wk of 0.4160.58 0.5460.73 — 20.13 (20.26 to .04 .13
gestation 20.003)
Total cholesterol (mmol/L)
Early (mg/dL) 207.3635 210.7639 — 25 (213.6 to .29
3.71)
28 wk of gestation, mmol/L (mg/dL) 255.6646 260647 — 20.31 (20.88 to .26 .53
0.26)
Difference from baseline to 28 wk of 48.3627 49.4635 — 20.85 (27 to 5.3) .78 .82
gestation, mmol/L (mg/dL)
Triglycerides (mmol/L)
Early (mg/dL) 132.8661 124643 — 7.1 (22.13 to .13
15.9)
28 wk of gestation (mg/dL) 186655 186660 — 20.53 (29.66 to .92 .94
10.8)
Difference from baseline to 28 wk of 57.5643 60.2640 — 22.56 (210.5 to .51 .71
gestation (mg/dL) 5.22)
HDL (mmol/L)
Early (mg/dL) 57.2617 60616.2 — 22.71 (20.54 to .07
0.27)
28 wk of gestation (mg/dL) 53.3620.5 53.3619.7 — 0.07 (23.71 to .53 .71
3.75)
Difference from baseline to 28 wk of 23.75615.8 25.41615.1 21.66 (21.31 to .27 .53
gestation (mg/dL) 4.64)
LDL (mmol/L)
Early (mg/dL) 126.1638 127.2639 21.35 (28.19 to .69
5.5)
28 wk of gestation (mg/dL)‡ 163646.7 169.3648 26.8 (215.7 to .14 .40
2.18)
Difference from baseline to 28 wk of 37.5636 40.6643 20.2.86 (210.5 to .46 .71
gestation (mg/dL) 4.75)
GDM, gestational diabetes mellitus; METS, metabolic equivalent of task; OGTT, oral glucose tolerance test; pp, postprandial; IOM, Institute
of Medicine; GWG, gestational weight gain; PET, preeclampsia; PIH, pregnancy-induced hypertension; HOMA2-IR, homeostatic model
assessment; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Data are n/N (%), n (%) or mean6SD unless otherwise specified.
P values calculated by independent-samples t tests, Fishers (n,10) or x2 tests. Adjusted P values were calculated for efficacy endpoints using
the Benjamin-Hochberg procedure.
Bold indicates statistically significant values.
* Physical activity data available for 165 women in the intervention group and 170 in the control group.
†
Dietary data available for 159 women in the intervention group and 161 in the control group.
‡
Glucose tolerance test based on Hyperglycemia and Adverse Pregnancy Outcome (HAPO) criteria.
Both study groups had a formal antenatal research had the following anthropometric measurements and
consultation at baseline and 28 and 34 weeks of blood samples collected: weight, height, BMI, midupper
gestation. At baseline and the 28-week visit, all patients arm circumference, and body composition (using
822 Kennelly et al Pregnancy Exercise and Nutrition OBSTETRICS & GYNECOLOGY
Copyright Ó by American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 3. Neonatal Outcomes
Intervention Control Risk Ratio Mean Difference Adjusted
Outcome (n5270) (n5275) (95% CI) (95% CI) P P
Birth weight (g) 3,6016551 3,6696553 — 267.9 (2160.9 to .15 .40
25.03)
4,500 or greater 8 (3) 15 (5.5) 0.54 (0.23– — .69 .80
1.26)
4,000 or greater 58 (21.5) 67 (24.4) 0.88 (0.64–1.2) — .47 .71
2,500 or less 8 (3) 4 (1.5) 2.3 (0.62–6.7) — .38 .50
LGA
90th centile or greater 11 (4.1) 24 (8.7) 0.46 (0.23– — .03 .13
0.93)
95th centile or greater 3 (1.1) 11 (4) 0.28 (0.07– — .05 .15
0.98)
SGA
10th centile or less 28 (10.4) 26 (9.5) 1.09 (0.66– — .77 .82
1.82)
5th centile or less 16 (5.9) 13 (4.7) 1.2 (0.61–2.5) — .57 .72
Safety analyses
NICU admission 44 (16.3) 35 (12.7) 1.28 (0.85– — .27
1.93)
Cord blood analysis
Cord glucose (mg/dL) 73.8622 75.6622 — 20.8 (26.1 to 4.5) .76 .82
Cord insulin (pmo/L) 44.6642 49.6646 — 24.9 (216 to 6.2) .62* .76
C-peptide (nmol/L) 0.1360.17 0.1160.15 — 0.01 (20.02 to 0.05) .48* .71
Total cholesterol (mg/ 68.1622 69.2624 — 21.2 (26.9 to 4.6) .68 .80
dL)
Triglycerides (mg/dL) 53.1621 49.6623 — 3.5 (22.65 to 8.9) .25 .53
HDL (mg/dL) 21.267 22.867 — 21.93 (23.8 to 20.08) .04 .13
LDL (mg/dL) 37.5625 34.4624 — 3.1 (23.3 to 9.43) .34 .64
LGA, large for gestational age; SGA, small for gestational age; NICU, neonatal intensive care unit; HDL, high-density lipoprotein; LDL, low-
density lipoprotein.
P values calculated by independent-samples t tests, Fisher (n,10), or x2 tests. Adjusted P values were calculated for efficacy endpoints using
the Benjamini-Hochberg procedure centiles calculated per gestation-related optimal weight (GROW) birth weight centiles.
Data are mean6SD or n (%) unless otherwise specified.
* Log-transformed P value.
Impedimed SFB7 Bio-electrical Impedance Analysis). cutaneous tissue, and fetal thigh circumference as reported
Maternal weight was recorded at each antenatal consul- previously.14 At delivery, cord blood was taken and neo-
tation. The last measured weight taken before delivery nates’ birth weight, length, and head circumference were
was recorded from medical charts and used to compute recorded to calculate the Ponderal index (1003mass in
total gestational weight gain. Fasting blood samples were g/height in cm3). The Gestation Network’s Bulk Calcula-
collected for measurement of glucose, insulin, C-pep- tor 6.2.3 UK was used to calculate birth weight centiles.
tide, and lipids and at 28 weeks of gestation, these blood The following data were also obtained from medical re-
samples were followed by a 2-hour oral glucose cords: time of labor onset, mode of delivery, adverse
tolerance test performed according to the International maternal events, and admissions to the neonatal unit.
Association of Diabetes and Pregnancy Study Groups All participants in both groups were provided
criteria.13 Gestational diabetes mellitus was confirmed if with two 3-day food diaries to quantify glycemic index
at least one glucose value was at or above the following: and glycemic load intakes and two validated preg-
fasting 92 mg/dL or greater, 1 hour 180 mg/dL or nancy exercise and lifestyle surveys to ascertain
greater, and 2 hour 153 mg/dL or greater. Additional self-reported physical activity levels20—at baseline
data were recorded from the medical charts, including (preintervention) and in the third trimester (postinter-
relevant medical and family history of diabetes. vention). The glycemic index and glycemic load of
At 34 weeks of gestation, maternal weight was foods were calculated from food diaries analyzed with
recorded. We assessed fetal biometry ultrasonographi- Nutritics Professional 3.09. The glycemic load of food
cally at 34 weeks of gestation including a measurement of pertains to a number that approximates how much
fetal anterior abdominal wall width, fetal midthigh sub- a particular food will increase an individual’s blood
VOL. 131, NO. 5, MAY 2018 Kennelly et al Pregnancy Exercise and Nutrition 823
Copyright Ó by American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
glucose level after consuming it. The glycemic index glucose tolerance test and could be assessed for the
is a measure of how foods that contain carbohydrates primary outcome. Mean BMI of participants was 29.3
increase blood glucose levels. and mean gestational age 15.5 weeks. The groups had
The prespecified primary outcome was incidence similar demographic characteristics (Table 1).
of GDM at 28–30 weeks of gestation. Prespecified Mean6SD of participants in the intervention group
maternal secondary outcomes were: gestational who used the application was, on average, 2.462.8
weight gain, glycemic index, glycemic load, and self- times per week and for an average of 16.268 weeks.
reported exercise levels in the third trimester. Other The primary study outcome (incidence of GDM)
secondary outcomes collected for exploratory and did not differ between the two groups, 37 of 241
subgroup analysis included neonatal birth weight, (15.4%) in the intervention group compared with 36
Ponderal index, and the incidence of large for gesta- of 257 (14.1%) in the control group (relative risk 1.1,
tional age (LGA), that is, birth weight greater than the 95% CI 0.71–1.66, P5.71).
90th centile. Women in the intervention group had signifi-
The rate of GDM in those with BMIs greater than cantly less gestational weight gain (Table 2). The inter-
25 is 12–15%.21 To reduce GDM to a rate of 7.2%, we vention resulted in lower dietary glycemic index and
estimated that 506 women would be required to have glycemic load and increased exercise compared with
80% power to detect this effect size at a significance of women in a control group (Table 2). However, only
.05, that is, 253 in each arm. The Finnish Gestational differences in dietary glycemic load and exercise par-
Diabetes Prevention (RADIEL) study was a random- ticipation persisted after multiple correction testing.
ized controlled trial of a lifestyle intervention in the After the intervention, there was no difference
pregnancies of obese women and reduced the inci- between the groups in midupper arm circumference
dence of GDM from 21.6% to 13.9%, that is, (31.563 cm vs 31.762.7 cm, P5.5), but less whole
a 35.6% reduction.2 Therefore, we considered that body fat mass in the intervention group compared
a reduction from 15% to 7.2% could be achievable with women in the control group, in the third trimes-
in this population. All statistical analyses were per- ter (30.967.3 kg vs 33.368.3 kg, P5.04, adjusted
formed using IBM SPSS for Windows 22.0. Partici- P5.12). There was no difference between the groups
pants were analyzed per their originally assigned in mean6SD blood loss at delivery (449.56275.4 mL
groups. Variables were graphically assessed for nor- vs 433.16245.7 mL, P5.82), postpartum hemorrhage
mality using histograms. Primary analysis was per- (blood loss greater than 500 mL) (19.5% vs 19.6%,
formed with a x2 test with GDM as the primary P5.99), antenatal admissions (34.2% vs 32.1%
outcome. Independent-sample t tests were used for P5.59), or other labor and delivery outcomes
comparison of means and x2 and Fisher exact tests (Table 3). There was no difference in maternal lipid
used to compare categorical variables between the profile and markers of glucose homeostasis between
two groups. Treatment effects for binary endpoints groups (Table 2).
are expressed as risk ratios (relative risk) with 95% There was no difference between the groups in
CIs and mean differences with 95% CIs for continu- the following prenatal and postnatal characteristics:
ous variables. Analysis of the mean change in mater- estimated fetal weight at 34 weeks of gestation
nal anthropometric and metabolic measurements was (2,520.46292 g vs 2,535.36283.8 g, P5.57), Ponderal
performed using independent-sample t tests. We index (2.7160.3 vs 2.7560.5, P5.38), birth weight,
apply a correction to control the false discovery rate and cord blood parameters (Table 3). There was one
over 47 secondary and exploratory efficacy tests using unexplained stillbirth at greater than 37 weeks of ges-
the Benjamini-Hochberg procedure. This is a less con- tation and one preterm delivery with subsequent neo-
servative procedure than the common Bonferroni cor- natal death in the intervention group. There was one
rection; it controls the number of false-positive results miscarriage in the intervention group and two in the
rather than the probability of at least one false-positive control group.
(Appendix 1, http://links.lww.com/AOG/B90).22
DISCUSSION
RESULTS This multifaceted behavioral lifestyle intervention
Between March 2013 and February 2016, 1,858 incorporating dietary and physical activity advice
women were assessed for eligibility and 565 women with reinforcement using mobile health technology
were recruited and randomized (278 in the interven- did not lower the rate of GDM. However, among
tion and 287 in the control arm) (Fig. 1). A total of 241 prespecified secondary outcomes, the intervention
(87%) and 257 (90%) women completed the oral was found to exert a beneficial influence on lifestyle
824 Kennelly et al Pregnancy Exercise and Nutrition OBSTETRICS & GYNECOLOGY
Copyright Ó by American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
behaviors by way of reducing dietary glycemic load of these results, however, have to be interpreted
and increasing exercise participation. with caution because they did not persist after mul-
Because glucose is important both in the devel- tiple testing corrections.
opment of GDM and for fetal growth, attenuation of Few studies have looked at the effect of mobile
maternal glucose in pregnancy by manipulation diet health technology to improve pregnancy outcomes.
and exercise is a reasonable clinical target for inter- This trial was well designed with stratified randomi-
vention trials. However, it is possible that the magni- zation ensuring equal numbers of overweight and
tude of the observed dietary and physical activity obese women in each group. Enrollment rates and
changes in this lifestyle intervention was insufficient to prespecified sample sizes were also achieved. This
alter GDM rates. Our results are consistent with study is also novel in its incorporation of mobile
others; two recently published large randomized health technology and behavior change techniques in
controlled trials were unsuccessful in showing a posi- the intervention. We argue the adjustment for multi-
tive effect of a behavioral lifestyle intervention on ple testing for secondary and exploratory efficacy
GDM.9,23 Recent interest has focused on pharmaco- outcomes gives us more reassurance that the inter-
logic interventions, but two recent studies did not find vention effect on exercise and glycemic load is robust.
that metformin-supported lifestyle interventions We note that this interpretation of the adjusted P val-
reduced GDM rates (Balani J, Hyer S, Shehata H. ues is in contrast to a more traditional Bonferroni
Metformin versus placebo in obese pregnant women correction. The false discovery rate procedure enables
without diabetes [letter]. N Engl J Med one to take the unadjusted P,.05 level and inspect the
2016;374:2502.).24 Interventions during the precon- adjusted P value as a direct estimate of the proportion
ception period may hold potential to reduce expected to be false below that threshold given the
GDM25; however, considerable work is required to number of tests conducted. Although not a solution
show that prepregnancy interventions are effective. for the multiplicity problem, this approach frames the
This intervention did result in greater self- problem for the reader and gives them more useful
reported exercise participation by the third trimes- information with which to make a determination of
ter. This is important because physical activity tends “significance.” The primary limitation of the study is
to decline with advancing gestation. The interven- that dietary intake and exercise behaviors were self-
tion involved a face-to-face education session and reported and potentially subject to underreporting or
incorporated SMART goals, techniques that have overreporting. Also, the absence of access to a smart-
been shown to improve exercise behaviors in phone potentially excluded 30% of lesser affluent and
pregnancy.10 This intervention also resulted in able women. Additionally, we may have had a slightly
lower dietary glycemic load intakes by the third tri- different cohort and study results if early pregnancy
mester. A low glycemic index dietary intervention screening for diabetes was performed. However, rou-
has been shown previously to improve maternal tine practice in many countries does not involve
dietary intakes,26 reduce GWG, and improve glu- screening for diabetes early in pregnancy based on
cose homeostasis.20 Future dietary analysis in this risk factors.
cohort will confirm whether women improved other Although this mobile health-supported interven-
macro- and micronutrient intakes. Initial unadjusted tion did not affect GDM rates, it did result in some
analysis showed that the mean gestational weight maternal benefits. This study used mobile health
gain in the intervention group was significantly technology to support a traditional face-to-face con-
lower than the control group. In addition, a post sultation and facilitated positive behavior change. The
hoc exploratory analysis revealed fewer neonates use of mobile health technology supporting a low
in the intervention group were born LGA. Because glycemic index diet and physical activity intervention
this was not a prespecified outcome, this finding with routine antenatal care in at-risk women is
awaits replication. A potential reduction in LGA is a simple, safe, and effective measure to improve
important because neonates at the higher end of the maternal exercise levels and improve dietary glyce-
birth weight centile have increased rates of child- mic load.
hood obesity and future cardiovascular and meta-
bolic morbidity.27 Our preliminary findings are
supported by the results of the LIMIT study, which REFERENCES
noted lower rates of neonates born at greater than 4 1. Metzger BE, Coustan DR. Summary and recommendations of
the Fourth International Workshop-Conference on Gestational
kg,23 and the Nelli study, which reported lower Diabetes Mellitus. The Organizing Committee. Diabetes Care
birth weight and fewer neonates born LGA.8 All 1998;21(suppl 2):B161–7.
VOL. 131, NO. 5, MAY 2018 Kennelly et al Pregnancy Exercise and Nutrition 825
Copyright Ó by American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
2. Koivusalo SB, Rönö K, Klemetti MM, Roine RP, Lindström J, 14. Kennelly MA, Ainscough K, Lindsay K, Gibney E, Mc Carthy
Erkkola M, et al. Gestational diabetes mellitus can Be prevented M, McAuliffe FM. Pregnancy, exercise and nutrition research
by lifestyle intervention: the Finnish gestational diabetes pre- study with smart phone app support (Pears): study protocol of
vention study (RADIEL): a randomized controlled trial. Diabe- a randomized controlled trial. Contemp Clin Trials 2015;46:
tes Care 2016;39:24–30. 92–9.
3. Baci Y, Üstüner I, Keskin HL, Ersoy R, Avşar AF. Effect of 15. Dietary reference values for food energy and nutrients for the
maternal obesity and weight gain on gestational diabetes melli- United Kingdom. Report of the Panel on Dietary Reference
tus. Gynecol Endocrinol 2013;29:133–6. Values of the Committee on Medical Aspects of Food Policy.
Rep Health Soc Subj (Lond) 1991;41:1–210.
4. Anand SS, Gupta M, Teo KK, Schulze KM, Desai D, Abdalla
N, et al. Causes and consequences of gestational diabetes in 16. Artal R, O’Toole M. Guidelines of the American College of
South Asians living in Canada: results from a prospective Obstetricians and Gynecologists for exercise during pregnancy
cohort study. CMAJ Open 2017;5:E604–11. and the postpartum period. Br J Sports Med 2003;37:6–12.
5. Sui Z, Moran LJ, Dodd JM. Physical activity levels during preg- 17. Kessler HS, Sisson SB, Short KR. The potential for high-
nancy and gestational weight gain among women who are over- intensity interval training to reduce cardiometabolic disease
weight or obese. Health Promot J Austr 2013;24:206–13. risk. Sports Med 2012;42:489–509.
6. Vinter CA, Jensen DM, Ovesen P, Beck-Nielsen H, Jørgensen 18. Carver CS, Scheier MF. Control theory: a useful conceptual
JS. The LiP (Lifestyle in Pregnancy) study: a randomized con- framework for personality-social, clinical, and health psychol-
trolled trial of lifestyle intervention in 360 obese pregnant ogy. Psychol Bull 1982;92:111–35.
women. Diabetes Care 2011;34:2502–7. 19. Bandura A. Health promotion by social cognitive means.
7. Korpi-Hyövälti EA, Laaksonen DE, Schwab US, Vanhapiha Health Educ Behav 2004;31:143–64.
TH, Vihla KR, Heinonen ST, et al. Feasibility of a lifestyle 20. Walsh JM, McGowan CA, Mahony R, Foley ME, McAuliffe FM.
intervention in early pregnancy to prevent deterioration of glu- Low glycaemic index diet in pregnancy to prevent macrosomia
cose tolerance. BMC Public Health 2011;11:179. (ROLO study): randomised control trial. BMJ 2012;345:e5605.
8. Luoto R, Kinnunen TI, Aittasalo M, Kolu P, Raitanen J, Ojala 21. Torloni MR, Betrán AP, Horta BL, Nakamura MU, Atallah
K, et al. Primary prevention of gestational diabetes mellitus and AN, Moron AF, et al. Prepregnancy BMI and the risk of ges-
large-for-gestational-age newborns by lifestyle counseling: tational diabetes: a systematic review of the literature with meta-
a cluster-randomized controlled trial. PLoS Med 2011:8: analysis. Obes Rev 2009;10:194–203.
e1001036. 22. Glickman ME, Rao SR, Schultz MR. False discovery rate con-
9. Poston L, Bell R, Croker H, Flynn AC, Godfrey KM, Goff L, trol is a recommended alternative to Bonferroni-type adjust-
et al. Effect of a behavioural intervention in obese pregnant ments in health studies. J Clin Epidemiol 2014;67:850–7.
women (the UPBEAT study): a multicentre, randomised con- 23. Dodd JM, Turnbull D, McPhee AJ, Deussen AR, Grivell RM,
trolled trial. Lancet Diabetes Endocrinol 2015;3:767–77. Yelland LN, et al. Antenatal lifestyle advice for women who are
10. Currie S, Sinclair M, Murphy MH, Madden E, Dunwoody L, overweight or obese: LIMIT randomised trial. BMJ 2014:348:
Liddle D. Reducing the decline in physical activity during preg- g1285.
nancy: a systematic review of behaviour change interventions. 24. Chiswick C, Reynolds RM, Denison F, Drake AJ, Forbes S,
PLoS One 2013;8:e66385. Newby DE, et al. Effect of metformin on maternal and fetal
11. Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. outcomes in obese pregnant women (EMPOWaR): a rando-
The effectiveness of mobile-health technology-based health mised, double-blind, placebo-controlled trial. Lancet Diabetes
behaviour change or disease management interventions for Endocrinol 2015;3:778–86.
health care consumers: a systematic review. PLoS Med 2013; 25. Zhang C, Tobias DK, Chavarro JE, Bao W, Wang D, Ley SH,
10:e1001362. et al. Adherence to healthy lifestyle and risk of gestational dia-
12. O’Higgins A, Murphy OC, Egan A, Mullaney L, Sheehan S, betes mellitus: prospective cohort study. BMJ 2014;349:g5450.
Turner MJ. The use of digital media by women using the mater- 26. McGowan CA, Walsh JM, Byrne J, Curran S, McAuliffe FM.
nity services in a developed country. Ir Med J 2014;107:313–5. The influence of a low glycemic index dietary intervention on
13. International Association of Diabetes and Pregnancy Study maternal dietary intake, glycemic index and gestational weight
Groups Consensus Panel, Metzger BE, Gabbe SG, Persson B, gain during pregnancy: a randomized controlled trial. Nutr J
Buchanan TA, Catalano PA, et al. International association of 2013;12:140.
diabetes and pregnancy study groups recommendations on the 27. Hermann GM, Dallas LM, Haskell SE, Roghair RD. Neonatal
diagnosis and classification of hyperglycemia in pregnancy. macrosomia is an independent risk factor for adult metabolic
Diabetes Care 2010;33:676–82. syndrome. Neonatology 2010;98:238–44.
826 Kennelly et al Pregnancy Exercise and Nutrition OBSTETRICS & GYNECOLOGY
Copyright Ó by American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
You might also like
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Focus Data Action ResponseDocument3 pagesFocus Data Action ResponseSitty Aizah MangotaraNo ratings yet
- Kardex: GCS: 12-13/15 (M:5, V:4-5, E:3)Document11 pagesKardex: GCS: 12-13/15 (M:5, V:4-5, E:3)Dienizs Labini TadenaNo ratings yet
- Journal Homepage: - : IntroductionDocument8 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- HypoglycemiaDocument19 pagesHypoglycemiaJesus PadillaNo ratings yet
- Case Study #3 Diabetes MellitusDocument2 pagesCase Study #3 Diabetes MellitusAvyNo ratings yet
- Nur 111 Session 13 Sas 1Document8 pagesNur 111 Session 13 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- LibreView Guide - Italian PaperDocument12 pagesLibreView Guide - Italian PaperJesus MuñozNo ratings yet
- Frederick Classification of HyperlipidemiaDocument2 pagesFrederick Classification of HyperlipidemiaBilly BuswayNo ratings yet
- HbA1c InsertDocument2 pagesHbA1c InsertMaximiliano GitahNo ratings yet
- Pre Assessment Diabetes Nursing CareDocument4 pagesPre Assessment Diabetes Nursing CareHabib UllahNo ratings yet
- 2018-National Diabetes Nursing Knowledge and Skills Framework 2018Document90 pages2018-National Diabetes Nursing Knowledge and Skills Framework 2018ZH. omg sarNo ratings yet
- Lecture 2 Clinical BiochemistryDocument41 pagesLecture 2 Clinical BiochemistryTilihoi Doru Jr.No ratings yet
- The Influence of Glucose Self-Monitoring On Glycaemic Control in Patients With Diabetes Mellitus in SudanDocument5 pagesThe Influence of Glucose Self-Monitoring On Glycaemic Control in Patients With Diabetes Mellitus in SudanZam-zam RsiNo ratings yet
- Blood Sugar TestDocument2 pagesBlood Sugar TestAlif AlifNo ratings yet
- Drugs of DiabetesDocument42 pagesDrugs of Diabeteskwennybiang100% (1)
- Regulations - Addressing Complaints - Student1Document13 pagesRegulations - Addressing Complaints - Student1danushaNo ratings yet
- Diabetes: EndocrinologyDocument8 pagesDiabetes: EndocrinologyZhanyar Omer Mustafa F210050No ratings yet
- Blood Glucose MonitoringDocument30 pagesBlood Glucose MonitoringVictoria Castillo TamayoNo ratings yet
- هاله خالد عطا الله عرارDocument2 pagesهاله خالد عطا الله عرارHala ArarNo ratings yet
- ML Minor MayDocument5 pagesML Minor Maygovind kumarNo ratings yet
- Jurnal Ekstrak MethanolicDocument6 pagesJurnal Ekstrak MethanolicMoses FernandoNo ratings yet
- Glicosimetro - FreeStyle OptiumH - ART20287 - Rev-BDocument29 pagesGlicosimetro - FreeStyle OptiumH - ART20287 - Rev-BAdriano MartinsNo ratings yet
- DiabetesMellitus NiKadeWahyuParamitha SeniCaturPuspa PutriSintaHasanah FirmansyahAliLukmanDocument16 pagesDiabetesMellitus NiKadeWahyuParamitha SeniCaturPuspa PutriSintaHasanah FirmansyahAliLukmanKade Wahyu ParamithaNo ratings yet
- CBG ChecklistDocument5 pagesCBG Checklistchandria0026No ratings yet
- PM 2019 426Document54 pagesPM 2019 426Dnyaneshwar AlhatNo ratings yet
- 09. ĐỀ VIP 9 - Soạn chuẩn cấu trúc minh họa BGD năm 2023 - Môn TIẾNG ANH - Bản word có giải TN4) .Image.MarkedDocument10 pages09. ĐỀ VIP 9 - Soạn chuẩn cấu trúc minh họa BGD năm 2023 - Môn TIẾNG ANH - Bản word có giải TN4) .Image.MarkedPhạm Tiến LongNo ratings yet
- Neonatal HypoglycemiaDocument5 pagesNeonatal Hypoglycemiadiana rossNo ratings yet
- Senior Citizen Application Before TribunalDocument5 pagesSenior Citizen Application Before TribunalUrvashi Dhonde100% (1)
- Diabetes MellitusDocument8 pagesDiabetes MellitusJaja RamosNo ratings yet
- Continuous Subcutaneous Insulin InfusionDocument6 pagesContinuous Subcutaneous Insulin Infusiondonny elhamdouniNo ratings yet