100% found this document useful (2 votes)
2K views7 pagesComprehensive Geriatric Assessment
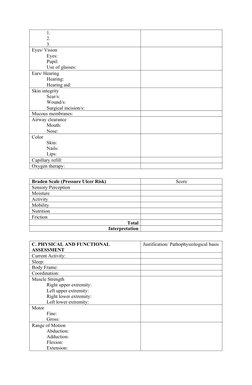
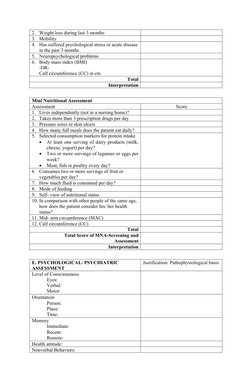
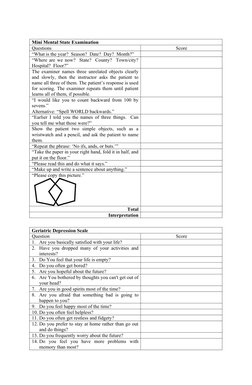
This document contains a comprehensive geriatric assessment form that collects information in 6 sections: personal data, medical, physical and functional, nutritional, psychological/psychiatric, and social-environmental assessments. The form includes scales and tests to evaluate risks such as for pressure ulcers, falls, malnutrition, depression, and cognitive impairment. It aims to provide a holistic view of older adult patients' health, functioning, and social support systems.
Uploaded by
Julien BulauanCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
100% found this document useful (2 votes)
2K views7 pagesComprehensive Geriatric Assessment
This document contains a comprehensive geriatric assessment form that collects information in 6 sections: personal data, medical, physical and functional, nutritional, psychological/psychiatric, and social-environmental assessments. The form includes scales and tests to evaluate risks such as for pressure ulcers, falls, malnutrition, depression, and cognitive impairment. It aims to provide a holistic view of older adult patients' health, functioning, and social support systems.
Uploaded by
Julien BulauanCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd