Professional Documents
Culture Documents
Pone 0210716
Uploaded by
Gemala AdillawatyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pone 0210716
Uploaded by
Gemala AdillawatyCopyright:
Available Formats
RESEARCH ARTICLE
A cross-sectional study on the prevalence of
antibiotic use prior to laboratory tests at two
Ghanaian hospitals
Gracious Yoofi Donkor ID1☯*, Ebenezer Dontoh1☯, Alex Owusu-Ofori2
1 Department of Medical Laboratory Technology, Kwame Nkrumah University of Science and Technology,
Kumasi, Ghana, 2 Department of Clinical Microbiology, School of Medical Sciences, Kwame Nkrumah
University of Science and Technology, Kumasi, Ghana
☯ These authors contributed equally to this work.
* roknod19@hotmail.com
a1111111111 Abstract
a1111111111
a1111111111 There has been a significant rise in global antibiotic use in recent years. Development of
a1111111111 resistance has been linked to easy accessibility, lack of regulation of sale, increased ten-
a1111111111
dency to self-medicate and the lack of public knowledge. The increase in antibiotic misuse,
including self-medication, has not been well documented in developing countries. Antibiotic
use prior to visiting health facilities has been found to be prevalent in developing countries. It
has been identified by some studies to increase the likelihood of missed diagnoses and influ-
OPEN ACCESS
ence the outcome of bacteriological tests. This study is aimed at determining the prevalence
Citation: Donkor GY, Dontoh E, Owusu-Ofori A of prior antibiotic use through a cross-sectional survey of patients undergoing laboratory
(2019) A cross-sectional study on the prevalence
tests at two health facilities in Ghana. Face-to-face questionnaires were used to interview
of antibiotic use prior to laboratory tests at two
Ghanaian hospitals. PLoS ONE 14(1): e0210716. 261 individuals chosen by random sampling of patients visiting the bacteriology laboratory
https://doi.org/10.1371/journal.pone.0210716 of the hospitals within a two-month period. The questionnaire investigated participant demo-
Editor: Thomas Webster, Northeastern University, graphic characteristics, knowledge about antibiotics and the nature of antibiotic use. Antibi-
UNITED STATES otic property detection bioassay was performed on patient’s urine sample using a disk
Received: June 13, 2018 diffusion method to accurately determine antibiotic use within 72 hours. Culture results were
used as an index to evaluate the effect of prior antibiotic use on bacteriological tests. Out of
Accepted: January 1, 2019
a 261 participants enrolled, 19.9% (95% CI, 14.9–24.9) acknowledged using antibiotics
Published: January 15, 2019
prior to their visit to the laboratory during the study period. On the contrary, 31.4% (95% CI,
Copyright: © 2019 Donkor et al. This is an open 25.7–37.5) of participants’ urine samples were positive for antimicrobial activity. Participants
access article distributed under the terms of the
within the age ranges of 20–30, 31–40 and 41–50 years had significantly lower odds of urine
Creative Commons Attribution License, which
permits unrestricted use, distribution, and antimicrobial activity. Participants who had urine antimicrobial activity were more likely to
reproduction in any medium, provided the original have no growth on their culture plates than participants who had no urine antimicrobial activ-
author and source are credited.
ity [OR 2.39(1.37–4.18), p = 0.002]. The most commonly used antibiotics were the penicil-
Data Availability Statement: All relevant data are lins, fluoroquinolones and metronidazole. Although, majority of the participant (54.8%) had
within the paper and its Supporting Information
knowledge of antibiotics, most of them had inadequate information on their proper use. The
files.
commonest indications for antibiotic use were aches and pains (30.3%), diarrhoea (43.3%)
Funding: The authors received no specific funding
and urinary tract infections (28.0%). Prior antibiotic use was found to increase the likelihood
for this work.
of obtaining a culture negative result and can affect the outcome of bacteriological tests.
Competing interests: The authors have declared
that no competing interests exist.
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 1 / 12
Prior antibiotic use at two Ghanaian hospitals
Introduction
Antibiotic use has risen markedly in recent years. A report by the Centre for Disease Dynam-
ics, Economics and Policy (CDDEP) showed that global antibiotic consumption rose by more
than 30% from 2000 to 2010 [1]. According to the report, increased access due to growing
incomes and the increased use of antibiotics in agriculture are two major factors that have con-
tributed to the rise in antibiotic consumption [1]. High consumption rates are further wors-
ened in developing countries by the inadequate enforcement of laws limiting non-prescription
sale of antibacterial agents [2–4]. Unsurprisingly, the highest increase in global antibiotic con-
sumption was observed in developing countries. In India for example, it is estimated that anti-
biotics administered in hospitals account for 20% of antibiotic use while community use
(prescribed or unprescribed) contributes to the rest [5]. Inevitably, rampant use of antibiotics
has had grave repercussions in the form of widespread antibiotic resistance. Today, antibiotic
resistance accounts for more than 23,000 deaths a year in the United States alone[6].
Prior antibiotic use amongst patients visiting health facilities has risen, especially in devel-
oping countries [2,7,8]. A study in Ghana by Lerbech et al. (2014) detected antimicrobial
agents in the urine of 64% out-patients reporting to two hospitals [9]. Prior antibiotic use has
been associated with several serious consequences in some studies. One of such studies found
that prior antibiotic exposure was associated with greater length of stay at hospitals following
the onset of Gram-negative bacteraemia complicated by severe sepsis [10]. Another study
showed that recent antibiotic treatment prior to tests such as blood culture, could reduce cul-
ture sensitivity by as much as 62 to 73 percent [11]. Paz et al. 2015, also showed, that prior anti-
biotic medication can significantly reduce synovial fluid culture positivity by 23% [12]. With
antibiotics being one of the most frequently prescribed drugs in Ghana [13,14], prior adminis-
tration before laboratory investigations could potentially reduce the accuracy of cultures and
other laboratory tests. Unfortunately, there is a lack of research concerning the prevalence of
antibiotic use before such laboratory tests in Ghana.
We therefore investigated the prevalence of patient antibiotic use prior to bacteriological
laboratory tests at two hospitals. Furthermore, we investigated public knowledge and use of
antibiotics. Finally, we assessed the influence of prior antibiotic use on culture results.
Materials and methods
Ethics statement
Ethical clearance was obtained from the Committee on Human Research Publication and Eth-
ics, School of Medical Sciences, Kwame Nkrumah University of Science and Technology. Per-
mission was also obtained from the administrators of both facilities prior to the study. Study
participants were also informed of the study and written consent obtained before being
included in the study. Consent was obtained from the parents or legal guardians of underage
participants before they were enrolled in the study.
Study design, site and population
This study was a cross-sectional study conducted from March to April 2017 at 2 health facili-
ties in different regions of Ghana; the Bomso Clinic and St. Dominic Hospital. These two facil-
ities represent major health providers outside of government owned hospitals. The Bomso
Clinic is 150-bed privately owned health facility in the Ashanti region, that provides routine
and specialist services for inhabitants in and around Bomso. St. Dominic’s Hospital is a
450-bed capacity Catholic-funded hospital in the Eastern Region of Ghana. It serves as a refer-
ral point for other nearby hospital and also as a facility for training interns and residents.
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 2 / 12
Prior antibiotic use at two Ghanaian hospitals
Patient interviews were conducted at the front desks of the medical laboratory. Eligible
patients were first provided oral and written information on the study. Consenting patients
were then interviewed with the questionnaire and requested to provide urine samples. Process-
ing of samples and all test procedures were conducted at bacteriology section of the medical
laboratory of the various facilities.
Study population and sample size
The target population of this study was all patients visiting the medical laboratory to undergo
bacteriological laboratory tests within the study period. 100 out-patients were randomly sam-
pled at the Bomso Clinic. 161 patients consisting of 62 out-patients and 99 in-patients were
also randomly sampled from the St. Dominic’s hospital. Participant ages ranged from 6 to 94
years.
Data collection methods
Questionnaire interview. The survey was conducted using an anonymous face-to-face
questionnaire. Patients visiting the hospital’s laboratory were interviewed with the question-
naire. The questionnaire was developed based upon surveys from earlier literature review and
tailored to suit the population and the nature of the research. It consisted of three sections;
demographic characteristics, knowledge about antibiotics and nature of antibiotic use.
The demographics section examined the characteristics of participants including age, sex,
level of education and access to health.
The section concerning knowledge about antibiotics and their use, ascertained the partici-
pants’ awareness about antibiotics and their use. This section determined participants’ aware-
ness of antibiotics, the antibiotics they were familiar with and had used before, and the
indications antibiotics could be used to treat. The pattern of antibiotic use was also assessed by
identifying factors such as the preferred source of antibiotics and the antibiotics frequently
used by participants.
The concluding section investigated information such as frequency of antibiotic use prior
to visiting a health facility and antibiotic use prior to visiting the laboratory.
Disk diffusion bioassay. Prior antibiotic use was evaluated by determining antimicrobial
activity in the patient’s urine sample, using a disk diffusion bioassay. Urine was the preferred
specimen since it has higher concentrations of chemical compounds than plasma or serum
[15]. The protocol for the disk diffusion bioassay was developed based on previous similar
studies [15–17].
• Sample collection for disk diffusion bioassay:
Participants were given a sterile, dry container to provide a urine sample. They were
instructed to collect midstream urine while ensuring as minimal contamination as possible.
The container was then labelled with his or her hospital code. Samples for in-patients were col-
lected by ward nurses immediately upon admission.
• Protocol for disk diffusion bioassay:
a. Reference organisms, i.e. Staphylococcus aureus (ATCC 25923) and Escherichia coli
(ATCC 25922), were inoculated unto a plate of Mueller-Hinton agar. This was done by
collecting 3–5 well isolated colonies of the reference organism with a sterile wire loop,
and emulsifying in 4 ml of sterile physiological saline and the turbidity adjusted to 0.5
McFarland. A sterile cotton tipped swab was used to streak the inoculum onto the sur-
face of the Mueller-Hinton agar.
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 3 / 12
Prior antibiotic use at two Ghanaian hospitals
b. Sterile filter paper discs (6mm diameter) were impregnated with 20 μl patient’s urine
using a pipette. The discs were dried at 56˚ C in an incubator. The discs were then placed
on the previously inoculated Mueller-Hinton agar plate, with sterile forceps. Commer-
cial antibiotic discs and filter paper soaked in sterile saline were added to each plate as
positive and negative controls respectively
c. After 24 hours’ incubation at 35–37˚C, the plates were read. The appearance of growth
inhibition around the disc was deemed as evidence of urine antimicrobial activity.
Duplicate measurements of the zone of inhibition were made with a ruler and the aver-
age was recorded. The diameter was recorded as 0mm when bacterial growth extended
unto the disc or there was no visible area of inhibition around the disc.
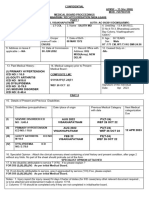
Each agar plate was used to test for the antibiotic activity in six samples together with the
positive and negative controls (Fig 1). This was consistent with the method used by Driscoll
et al., 2012, which tested for 2–8 samples on the same plate. As shown in Fig 1, the arrange-
ment and processes were duplicated for each sample on both plates.
Data analysis
Data collected from the study was entered, coded in Excel and exported into SPSS version22
for analysis. Descriptive statistics such as proportions, means and standard deviation were
used to describe the results of the study. The Pearson χ2 test was used to assess significant asso-
ciation between the study variables (p<0.05). Logistic regression was used to identify the pre-
dictors of urine antimicrobial activity.
Results
Socio-demographic profile
Two-thirds of the participants enrolled in the study were female (76.6%). Age distribution was
similar across both facilities with majority of the respondents were aged between 20–30 years
with a mean age of 36.26 (±SD 14.94). Although, the highest level of education attained by
respondents was tertiary education, there were considerably more tertiary educated respon-
dents at Bomso Clinic than at St. Dominic’s Hospital (Table 1).
Knowledge and use of antibiotics
More than half of the respondents (54.8%) had knowledge of antibiotics and the purpose they
served (Table 2). About one-third of the respondents were found to have previously used
Fig 1. A model for the arrangement of filter paper and antibiotics discs on the agar plates. (A) Escherichia coli plate
(ATCC 25922) (B) Staphylococcus aureus (ATCC 25923) plate.
https://doi.org/10.1371/journal.pone.0210716.g001
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 4 / 12
Prior antibiotic use at two Ghanaian hospitals
Table 1. Sociodemographic characteristics of study participants.
Category Health Facility Total
Bomso, N = 100 St. Dominic’s, N = 161 N = 261
Sex
Female 70 (70) 130 (80.7) 200 (76.6)
Age
<20 years 7 (7) 12 (7.5) 19 (7.3)
20–30 years 38 (38) 52 (32.3) 90 (34.5)
31–40 years 31 (31) 49 (30.4) 80 (30.7)
41–50 years 12 (12) 21 (13.0) 33 (12.6)
51–60 years 6 (6) 11 (6.8) 17 (6.5)
>60 years 6 (6) 16 (9.9) 22 (8.4)
Department
Outpatient 100 (100) 62 (38.5) 162 (62.1)
In-patient 0 (0) 99 (61.5) 99 (37.9)
Educational status
No formal education 3 (3) 12 (7.4) 15 (5.7)
Basic School 11 (11) 27 (16.8) 38 (14.6)
Junior High School 19 (19) 48 (29.8) 67 (25.7)
Senior High School 23 (23) 47 (29.2) 70 (26.8)
Tertiary 44 (44) 27 (16.8) 71 (27.2)
Relative in Health work
Yes 33 (33) 85 (52.8) 118 (45.2)
Access to health
Good 44 (44) 107 (66.5) 151 (57.9)
Moderate 36 (36) 46 (28.6) 82 (31.4)
Poor 20 (20) 8 (4.9) 28 (10.7)
https://doi.org/10.1371/journal.pone.0210716.t001
antibiotics while knowing what they were. However, a considerable portion (43.7%) were also
discovered to have used antibiotics without knowing what they actually were (Table 2). The
most popular source of antibiotics amongst respondents was physician prescription (75.1%)
and the most common indications for antibiotics were diarrhoea (43.3%), aches and pains
(30.3%) and Urinary Tract Infection (UTI) (23.0%) (Table 2).
Penicillin (i.e. amoxicillin, cloxacillin, flucoxacillin and penicillin) antibiotics were the most
commonly used antibiotic in both study locations. The fluoroquinolones and metronidazole
were the next most commonly used antibiotics according to the respondents (Fig 2).
Prior use of antibiotics
One-third of the respondents (33.3%) had used antibiotics before a hospital visit. Out of 261
respondents, 19.9% had used antibiotics prior to their current laboratory visit. About one-
third (31.4%) of the respondents tested positive for urine antimicrobial activity. The positivity
rate for urine antimicrobial activity was significantly higher at St. Dominic’s hospital than at
the Bomso clinic (Table 3).
Culture and sensitivity results
The most commonly isolated organisms were Escherichia coli (11.07%) and Candida spp.
(8.02%), making up 19.09% of the culture results (Table 4).
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 5 / 12
Prior antibiotic use at two Ghanaian hospitals
Table 2. Study participants’ knowledge and use of antibiotics.
Variable Health Facility Total
Bomso, N = 100 St. Dominic’s, N = 161 N = 261
Knowledge of antibiotics
Yes 65 (65.0) 108 (67.1) 143 (54.8)
Used antibiotic
Yes 67 (67.0) 26 (16.2) 93 (35.6)
No 3 (3.0) 51 (31.7) 54 (20.7)
Unknowingly 30 (30.0) 84 (52.1) 114 (43.7)
Source of antibiotic
Prescription 78 (78.0) 118 (73.3) 196 (75.1)
Relative advice 6 (6.0) 4 (2.5) 10 (6.2)
Pharmacist 24 (24.0) 0 (0) 24 (14.9)
Self-medication 41 (41.0) 92 (57.1) 133 (70.2)
Advertisement 2 (2.0) 0 (0) 2 (1.2)
On admission 13 (13.0) 0 (0) 13 (8.1)
Left over drug 2 (2.0) 7 (4.3) 9 (5.6)
Indication for antibiotic
Cough 8 (8.0) 30 (18.6) 38 (14.6)
Nasal congestion 26 (26.0) 1 (0.6) 27 (10.3)
Runny nose 19 (19.0) 0 (0) 38 (7.3)
Sore throat 34 (34.0) 1 (0.6) 35 (13.4)
Fever 17 (17.0) 0 (0) 17 (6.5)
Vomiting 4 (4.0) 2 (1.2) 6 (2.3)
Diarrhoea 34 (34.0) 79 (49.1) 113 (43.3)
Aches and pains 35 (35.0) 44 (27.3) 79 (30.3)
Skin wounds 30 (30.0) 41 (25.5) 71 (27.2)
Boils 17 (17.0) 8 (5.0) 25 (9.6)
Urinary Tract Infections 11 (11.0) 62 (38.5) 73 (28.0)
Others 10 (10.0) 6 (3.7) 16 (6.1)
https://doi.org/10.1371/journal.pone.0210716.t002
Fig 2. Antibiotic classes used by respondents stratified by location.
https://doi.org/10.1371/journal.pone.0210716.g002
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 6 / 12
Prior antibiotic use at two Ghanaian hospitals
Table 3. Prior antibiotic use stratified by location.
Variable Health Facility Total p-value
Bomso St. Dominic’s
Used antibiotic prior to a hospital visit 0.177
Yes 28 (28.0) 59 (36.6) 87 (33.3)
Used antibiotics prior to 0.1511
current visit
Yes 15 (15.0) 37 (23.0) 52 (19.9)
Time of prior use
1–12 hours 0 (0) 3 (1.9) 3 (1.1)
12–24 hours 5 (5.0) 29 (18.0) 34 (13.0)
24–48 hours 3 (3.0) 5 (3.1) 8 (3.1)
48–72 hours 3 (3.0) 0 (0) 3 (1.1)
72 hours and above 4 (4.0) 0 (0) 4 (1.5)
None 85 (0) 124 (47.5) 209 (80.1)
Bioassay detected <0.0001
Positive 14 (14.0) 68 (42.2) 82 (31.4)
https://doi.org/10.1371/journal.pone.0210716.t003
The majority of antibiotics tested against the isolated organisms (both gram positive and
gram negative) were generally ineffective. Majority of isolates were resistant to tetracycline
(95.4%), nalidixic acid (90.7%), cefuroxime (85%), cotrimoxazole (93%) and ampicillin
(97.7%). The aminoglycosides, amikacin and gentamicin were the most effective antibiotics,
showing 25.6% and 54.5% resistance respectively among the total isolates. Escherichia coli was
most sensitive to amikacin (n = 24), gentamicin (n = 14) and nitrofurantoin (n = 14) and was
most resistant to ampicillin (n = 0), cotrimoxazole (n = 1) and tetracycline (n = 1) (Table 5).
Influence of prior antibiotic use on culture results
Out of the 82 participants who tested positive for urine antimicrobial activity, 58 participants
had no growth on their culture plates. Similarly, out of 179 that did not have any antimicrobial
activity, 90 were culture negative. Participants who were positive for the bioassay were more
likely to have a culture negative result compared to participants who tested negative (OR 2.39
95% CI 1.37–4.18).
Table 4. Results of participants’ culture tests.
Culture results Frequency Percentage(%)
No growth 128 48.85
Insignificant growth 70 26.72
Significant growth 65 24.43
Isolate
Escherichia coli 29 11.07
Staphylococcus spp 2 0.76
Proteus mirabilis 3 1.15
Klebsiella spp. 5 1.90
Enterococcus 1 0.38
Enterobacteria 3 1.15
Candida spp. 21 8.02
https://doi.org/10.1371/journal.pone.0210716.t004
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 7 / 12
Prior antibiotic use at two Ghanaian hospitals
Table 5. Bacterial isolates and their susceptibility patterns among participants.
CIP NIT AMK AUG CXM GEN NAL PPA CTZ AMP TET
Bacterial isolates N n (%) n (%) n (%) n (%) n (%) n (%) n (%) n (%) n(%) n (%) n (%)
E. coli 29 7(24.1) 14(48.3) 24 (82.8) 2(14.2) 5(17.2) 14(48.3) 3(10.3) 7(24.1) 1(3.4) 0(0) 1(3.4)
Klebsiella spp 5 1(20) 1(20) 4(80) 0(0) 0(0) 2(40) 0(0) 1(20) 0(0) 0(0) 0(0)
P. mirabilis 3 2(66.7) 1(33.3) 2(66.7) 1(33.3) 1(33.3) 2(66.7) 1(33.3) 1(33.3) 2(66.7) 0(0) 0(0)
Enterobacteria 3 1(33.3) 1(33.3) 1(33.3) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0) 0(0)
Enterococcus spp 1 1(100) 1(100) 0(0) 1(100) 0(0) 0(0) 0(0) 0(0) 0(0) 1(100) 1(100)
Staphylococcus spp 2 1(50) 0(0) 1(50) 1(50) 1(50) 2(100) 0(0) 0(0) 0(0) 0(0) 0(0)
E. coli = Escherichia coli, P. mirabilis = Proteus mirabilis, Klebsiella spp. = Klebsiella pneumonia and Klebsiella spp., Staphylococcus spp = Staphylococcus aureus and
Coagulase Negative Staphylococcus, CIP = Ciprofloxacin, NIT = Nitrofurantoin, AMK = Amikacin, AUG = Augmentin, CXM = Cefuroxime, GEN = Gentamicin,
NAL = Nalidixic acid, PPA = Pipemidic acid, CTZ = Cotrimoxazole, AMP = Ampicillin, TET = Tetracycline.
https://doi.org/10.1371/journal.pone.0210716.t005
Determinants of antibiotic use prior to laboratory visit
The influence of sociodemographic characteristics of study participants on antibiotic use prior
to laboratory visit (as determined by bioassay) was analysed by binary logistic regression at
95% CI. Participants with the age ranges of 20–30, 31–40 and 41–50 years with adjusted odds
ratio of 0.29 (0.12–0.97), 0.28 (0.08–0.91) and 0.19 (0.05–0.74) respectively were less likely to
have had urine antimicrobial activity. An evaluation of the various levels of education did not
show any increased likelihood of prior antibiotic use.
Again, the effect of other factors including knowledge of antibiotics and the source of anti-
biotics on antibiotic use prior to laboratory visit were also evaluated with binary logistic regres-
sion. Although, participants who self-medicated with antibiotics had higher odds of urine
antimicrobial activity [1.70(0.88–3.30)], this association was not significant (p>0.05).
Discussion
Our study found that 19.9% (95% CI, 14.9–24.9) of patients in two Ghanaian health facilities
reported using antibiotics prior to their laboratory visit during the study period. This rate was
lower than the 31.4% (95% CI, 25.7–37.5) of patients whose urine samples were positive for
antimicrobial activity by the bioassay, indicating prior antibiotic use. Comparatively, a similar
study conducted by Y. Lui et al. 1999, found a slightly lower prevalence of urine antimicrobial
activity (25.1%) amongst 203 out-patients in Taiwan [17]. Another study conducted in North-
ern Uganda showed a much higher prevalence of reported antibiotic use of 62.2% but a similar
urine antibacterial activity prevalence of 30.4%. This considerable difference in reported use
could likely be as a result of the high prevalence of non-prescription use of antimicrobials in
Northern Uganda (75.7%) [18]. Again, another study at two hospitals in Ghana found a higher
prevalence of antibiotics in urine (64%)[9]. The significant pervasiveness of prior antibiotic
use found in this study and other studies in Ghana could be attributed to the proliferation of
antibiotic sources, lax drug regulatory legislation and insidious exposure to antibiotics used in
agriculture [19–22]. This increased and inappropriate use of antibiotics has serious implica-
tions since it contributes to selective pressure, favouring the development antibiotic resistance
[23,24]. Considering that increasing occurrences of antimicrobial resistant bacterial pathogens
have been reported in Ghana [25], further studies are required to investigate antibiotic use.
This would provide essential information to direct policies on the regulation of antibiotic con-
sumption and the implementation of antibiotic stewardship programmes.
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 8 / 12
Prior antibiotic use at two Ghanaian hospitals
This study found significantly increased culture negative results in patients who were posi-
tive for urine antibiotic activity. Participants who had urine antimicrobial activity were more
likely to have no growth on their culture plates than participants who had no urine antimicro-
bial activity. This indicates that prior antibiotic use could increase the likelihood of obtaining
culture negative results (no growth on culture plate) and influence the outcome of bacteriolog-
ical laboratory tests. However, it must be noted that urine antimicrobial activity was not found
to have a significant relationship with significant culture results. These findings concur with a
study by Paz et al. 2015, which found that prior antibiotic administration reduced synovial
fluid culture positivity[12] and another study by Arya & Agarwal, which found that the senis-
tivity of culture results was limited in prior antibiotic consumption [16]. This occurrence was
attributed to the fact that prior antibiotic use could compromise the recovery of bacterial path-
ogens and their accurate colony count, resulting in false-negative results and diagnostic dilem-
mas, especially in symptomatic patients [16].
From the study, it was found that more than half of the study population (54.8%) were
aware of antibiotics and the purpose they served. However, most participants reported that
antibiotics could be used to treat aches and pains, diarrhoea and UTIs. More of the partici-
pants who admitted to using antibiotics for aches and pains were females who reported that
they used them for stomach aches or abdominal cramps. These findings point towards an
underlying issue of poor knowledge on the appropriate use of antibiotics which could have sig-
nificant implications on the development of antibiotic resistance.
A little over a third of the study population (35.6%) admitted to knowingly using an antibi-
otic at some point prior to the study. Disturbingly, 43.7% of the participants had used an anti-
biotic before but they did so unaware that the drug was an antibiotic. Antibiotic usage was
more common at the St. Dominic’s Hospital, where majority of the subjects had low levels of
education. This findings highlight the gravity of illiteracy in the increasing inappropriate use
of antibiotics in developing countries [26][2]. Penicillin (β-lactam) use far outstripped the use
of the other classes of antibiotics amongst participants. According to several studies, penicilins
are either the most or amongst the commonly used antibiotics by the public in developing
countries [5,18,27–29] and it undoubtedly has serious implication on the emergence of peni-
cillin resistance in such regions. Predictably, resistance to penicillins (β-lactams) is high in
Ghana according to studies conducted [30][25].
While a majority of the participants reported that they obtained their antibiotics via physi-
cian prescription, a considerable portion admitted to self-medicating with antibiotics at some
point prior to the study. Although legislation in Ghana demands that antibiotics be obtained
only by prescription, antibiotics are still easily obtained over the counter [29]. This could
explain the high rate of self-medication with antibiotics in the study population.
The most commonly isolated organisms were Escherichia coli (n = 29) and Candida spp.
(n = 21). The higher prevalence of Escherichia coli is understandable since it is the most com-
mon urinary pathogen [31]. More than two-thirds (75.6%) of the cultures performed either
showed no growth or had insignificant growth after 48 hours’ incubation. Majority of the iso-
lated organisms were generally resistant against most of the tested antibiotics. The highest
resistance was against tetracycline (95.4%), nalidixic acid (90.7%), cefuroxime (85%), cotri-
moxazole (93%) and ampicillin (97.7%). The least resistance was found with the aminoglyco-
sides such as amikacin, gentamicin and levofloxacin. This data is consistent with the
nationwide surveillance report on antibiotic resistance in Ghana [25].
It must be noted that the study was limited by small sample size and short duration (2
months). Thus the results are not comprehensive enough to make it generalizable. Another
limitation was the inability to include in-patients at the Bomso Clinic, which could also have
had an effect on the data analysis.
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 9 / 12
Prior antibiotic use at two Ghanaian hospitals
Conclusion
This study has shown that nearly a third of patients had used antibiotics prior to their bacterio-
logical laboratory tests. It has also shown that prior antibiotic use (as determined by urine anti-
microbial activity) increases the likelihood of obtaining culture negative results and thus
influences the outcome of laboratory results. These findings confirm the need for health work-
ers to advise patients against using antibiotics before seeking healthcare for any illness. It also
re-emphasizes the need for clinicians to obtain their samples for bacteriology cultures before
giving antibiotics.
The discrepancy between patients reporting of antibiotic use and the bioassay results shows
that patient are unlikely to give an accurate history of their antibiotic use. Thus, a more accu-
rate method such as the disk diffusion bioassay can be used in identifying prior antibiotic use
in patients presenting to health facilities. There is the possibility that some patients may not
actually know that the drug they had taken was an antibiotic. Furthermore, it may also be pos-
sible that patients were afraid of some unknown repercussions if they revealed that they had
taken antibiotics. Health care providers should ensure that patients are very relaxed in their
presence and should encourage patients to provide accurate information and at the same time
reassuring patients that they will not suffer any consequences if they give only the right
information.
Penicillins were the most commonly used class of antibiotics amongst patients in the study.
Another important finding of the study was that although a considerable number of the
participants were aware of antibiotics and their purpose, they have poor knowledge on the
proper use of antibiotics.
Supporting information
S1 File. Study dataset.
(XLSX)
S2 File. Questionnaire.
(DOCX)
Acknowledgments
We would like to express our gratitude directors of the Bosmo Clinic and St. Dominic’s Hospi-
tal for permitting us to conduct our studies at their facilities. We also appreciate the staff of the
medical laboratories of both hospitals for their able support during the study.
Author Contributions
Conceptualization: Gracious Yoofi Donkor, Ebenezer Dontoh, Alex Owusu-Ofori.
Formal analysis: Gracious Yoofi Donkor, Ebenezer Dontoh.
Investigation: Gracious Yoofi Donkor, Ebenezer Dontoh.
Methodology: Gracious Yoofi Donkor, Ebenezer Dontoh, Alex Owusu-Ofori.
Resources: Ebenezer Dontoh, Alex Owusu-Ofori.
Supervision: Alex Owusu-Ofori.
Writing – original draft: Gracious Yoofi Donkor, Ebenezer Dontoh.
Writing – review & editing: Alex Owusu-Ofori.
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 10 / 12
Prior antibiotic use at two Ghanaian hospitals
References
1. CDDEP. State of the world’s antibiotics, 2015, CDDEP: Washington, D. C. 2015;
2. Okeke IN, Lamikanra A, Edelman R. Socioeconomic and behavioral factors leading to acquired bacte-
rial resistance to antibiotics in developing countries. Emerg Infect Dis. 1999; 5(1):18–27. https://doi.org/
10.3201/eid0501.990103 PMID: 10081668
3. Van Boeckel TP, Gandra S, Ashok A, Caudron Q, Grenfell BT, Levin SA, et al. Global antibiotic con-
sumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis [Internet].
2014; 3099(14):1–9. Available from: http://dx.doi.org/10.1016/S1473-3099(14)70780-7
4. Laxminarayan R, Heymann DL. Challenges of drug resistance in the developing world. Bmj. 2012; 344
(apr03 2):e1567–e1567. https://doi.org/10.1136/bmj.e1567 PMID: 22491075
5. Kotwani A, Holloway K. Trends in antibiotic use among outpatients in New Delhi, India. BMC Infect Dis
[Internet]. 2011 Jan [cited 2016 May 18]; 11:99. Available from: http://www.pubmedcentral.nih.gov/
articlerender.fcgi?artid=3097160&tool=pmcentrez&rendertype=abstract https://doi.org/10.1186/1471-
2334-11-99 PMID: 21507212
6. European Centre for Disease Prevention and Control (ECDC). Summary of the latest data on antibiotic
resistance in the European Union. Euro-Cdc. 2012;(November):1–4.
7. Ocan M, Manabe YC, Baluku H, Atukwase E, Ogwal-Okeng J, Obua C. Prevalence and predictors of
prior antibacterial use among patients presenting to hospitals in Northern Uganda. BMC Pharmacol
Toxicol [Internet]. 2015; 16(26):1–8. Available from: http://dx.doi.org/10.1186/s40360-015-0027-8
8. Khennavong M, Davone V, Vongsouvath M, Phetsouvanh R, Silisouk J, Rattana O, et al. Urine antibi-
otic activity in patients presenting to Hospitals in Laos: Implications for worsening antibiotic resistance.
Am J Trop Med Hyg. 2011; 85(2):295–302. https://doi.org/10.4269/ajtmh.2011.11-0076 PMID:
21813851
9. Lerbech AM, Opintan JA, Bekoe SO, Ahiabu MA, Tersbøl BP, Hansen M, et al. Antibiotic exposure in a
low-income country: Screening urine samples for presence of antibiotics and antibiotic resistance in
coagulase negative staphylococcal contaminants. PLoS One. 2014; 9(12):1–18.
10. Micek S, Johnson MT, Reichley R, Kollef MH. An institutional perspective on the impact of recent antibi-
otic exposure on length of stay and hospital costs for patients with gram-negative sepsis. BMC Infect
Dis [Internet]. 2012; 12(1):56. Available from: http://www.biomedcentral.com/1471-2334/12/56
11. Berkley J a, Lowe BS, Mwangi I, Williams T, Bauni E, Mwarumba S, et al. Bacteremia among children
admitted to a rural hospital in Kenya. N Engl J Med. 2005; 352(1):39–47. https://doi.org/10.1056/
NEJMoa040275 PMID: 15635111
12. Paz Z, Lieber SB, Moore A, Zhu C, Fowler ML, Robert H. The Impact of Prior Antibiotic Treatment on
Culture Results of Patients with Septic Arthritis. 2015;5–7.
13. Yevutsey SK, Buabeng KO, Aikins M, Anto BP, Biritwum RB, Frimodt-Møller N, et al. Situational analy-
sis of antibiotic use and resistance in Ghana: Policy and regulation. BMC Public Health [Internet]. 2017
Dec 23 [cited 2018 Feb 20]; 17(1):896. Available from: https://bmcpublichealth.biomedcentral.com/
articles/10.1186/s12889-017-4910-7 PMID: 29169340
14. Ahiabu M-A, Tersbøl BP, Biritwum R, Bygbjerg IC, Magnussen P. A retrospective audit of antibiotic pre-
scriptions in primary health-care facilities in Eastern Region, Ghana. Health Policy Plan [Internet]. 2016
Mar [cited 2016 May 18]; 31(2):250–8. Available from: http://www.pubmedcentral.nih.gov/articlerender.
fcgi?artid=4748131&tool=pmcentrez&rendertype=abstract https://doi.org/10.1093/heapol/czv048
PMID: 26045328
15. Driscoll AJ, Bhat N, Karron RA, O’Brien KL, Murdoch DR. Disk diffusion bioassays for the detection of
antibiotic activity in body fluids: Applications for the pneumonia etiology research for child health project.
Clin Infect Dis. 2012; 54(SUPPL. 2):159–64.
16. Arya SC, Agarwal N. Apropos “Antibiotic screening of urine culture as a useful quality audit.” J Infect
Dev Ctries. 2011; 5(9):677–8. PMID: 21918311
17. Liu YC, Huang WK, Huang TS, Kunin CM. Extent of antibiotic use in Taiwan shown by antimicrobial
activity in urine. Lancet. 1999; 354(9187):1360. https://doi.org/10.1016/S0140-6736(99)07446-2 PMID:
10533872
18. Ocan M, Bwanga F, Bbosa GS, Bagenda D, Waako P, Ogwal-Okeng J, et al. Patterns and predictors of
self-medication in northern Uganda. PLoS One. 2014; 9(3):1–7.
19. Seiter A, Gyansa-lutterodt M. Policy Note: The Pharmaceutical Sector in Ghana November 2009. 2009;
(November):1–36. Available from: http://apps.who.int/medicinedocs/documents/s16765e/s16765e.pdf
20. Radyowijati A, Haak H. Improving antibiotic use in low-income countries: An overview of evidence on
determinants.
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 11 / 12
Prior antibiotic use at two Ghanaian hospitals
21. Okeke IN, Aboderin OA, Byarugaba DK, Ojo KK, Opintan JA. Growing problem of multidrug-resistant
enteric pathogens in Africa. Emerg Infect Dis. 2007; 13(11):1640–6. https://doi.org/10.3201/eid1311.
070674 PMID: 18217545
22. VE B, C A, H O, A D. Antibiotic Practices and Factors Influencing the Use of Antibiotics in Selected Poul-
try Farms in Ghana. J Antimicrob Agents [Internet]. 2016 [cited 2017 Jun 14]; 2(2):1–8. Available from:
https://www.omicsonline.org/open-access/antibiotic-practices-and-factors-influencing-the-use-of-
antibiotics-inselected-poultry-farms-in-ghana-antimicro-1000120.php?aid=74711
23. Vila J. Update on Antibacterial Resistance in Low-Income Countries: Factors Favoring the Emergence
of Resistance~!2009-12-24~!2010-06-01~!2010-09-14~! Open Infect Dis J [Internet]. 2010; 4(2):38–54.
Available from: http://www.bentham-open.org/pages/content.php?TOIDJ/2010/00000004/00000002/
38TOIDJ.SGM
24. Dougherty TJ, Pucci MJ. Antibiotic discovery and development. Dougherty TJ, Pucci MJ, editors. Antibi-
otic Discovery and Development. 2014. 1–1127 p.
25. Opintan JA, Newman MJ, Arhin RE, Donkor ES, Gyansa-Lutterodt M, Mills-Pappoe W. Laboratory-
based nationwide surveillance of antimicrobial resistance in Ghana. Infect Drug Resist. 2015; 8:379–
89. https://doi.org/10.2147/IDR.S88725 PMID: 26604806
26. Kimang’a AN. A situational analysis of antimicrobial drug resistance in Africa: are we losing the battle?
Ethiop J Heal Sci [Internet]. 2012; 22(2):135–43. Available from: http://www.ncbi.nlm.nih.gov/pmc/
articles/PMC3407837/pdf/EJHS2202-0135.pdf
27. Donkor ES, Tetteh-Quarcoo PB, Nartey P, Agyeman IO. Self-medication practices with antibiotics
among tertiary level students in Accra, Ghana: A cross-sectional study. Int J Environ Res Public Health.
2012; 9(10):3519–29. https://doi.org/10.3390/ijerph9103519 PMID: 23202760
28. Rhodes J, Hyder JA, Peruski LF, Fisher C, Jorakate P, Kaewpan A, et al. Antibiotic use in Thailand:
quantifying impact on blood culture yield and estimates of pneumococcal bacteremia incidence. Am J
Trop Med Hyg [Internet]. 2010 Aug [cited 2016 May 18]; 83(2):301–6. Available from: http://www.
pubmedcentral.nih.gov/articlerender.fcgi?artid=2911175&tool=pmcentrez&rendertype=abstract
https://doi.org/10.4269/ajtmh.2010.09-0584 PMID: 20682872
29. Adu-Sarkodie YA. Antimicrobial self medication in patients attending a sexually transmitted diseases
clinic. Int J STD AIDS. 1997; 8:456–8. https://doi.org/10.1258/0956462971920343 PMID: 9228594
30. Newman MJ, Frimpong E, Donkor ES. Resistance to antimicrobial drugs in Ghana. 2011;215–20.
31. Behzadi P, Elham B, Hodjjat Y, Aghapour R. A survey on urinary tract infections associated with the
three most common uropathogenic bacteria. Maedica—A J Cinical Med. 2010; 5(67):111–5.
PLOS ONE | https://doi.org/10.1371/journal.pone.0210716 January 15, 2019 12 / 12
You might also like
- Logotherapy To Treat Substance Abuse As PDFDocument77 pagesLogotherapy To Treat Substance Abuse As PDFAan AndreanNo ratings yet
- Paget Disease, Fibrous Dysplasia, Osteosarcoma DiffrentiationDocument3 pagesPaget Disease, Fibrous Dysplasia, Osteosarcoma Diffrentiationreason131No ratings yet
- Awareness of Antibiotic Usage and Antibiotic Resistance - A Case Study in Selangor, MalaysiaDocument9 pagesAwareness of Antibiotic Usage and Antibiotic Resistance - A Case Study in Selangor, MalaysiaNoor NordinNo ratings yet
- Diabetes Mellitus Lesson PlanDocument6 pagesDiabetes Mellitus Lesson Planramzan aliNo ratings yet
- Caregiving Final 2nd Sem ExamDocument3 pagesCaregiving Final 2nd Sem ExamRichard CortezNo ratings yet
- Anatomy and Physiology of Adrenal GlandDocument26 pagesAnatomy and Physiology of Adrenal GlandYAMINIPRIYANNo ratings yet
- Petechiae Purpura and VasculitisDocument70 pagesPetechiae Purpura and VasculitisoktafNo ratings yet
- Abnormal Female Puberty 2016Document281 pagesAbnormal Female Puberty 2016MustafaAwaad100% (1)
- Antimicrobialstewardship Approachesinthe Intensivecareunit: Sarah B. Doernberg,, Henry F. ChambersDocument22 pagesAntimicrobialstewardship Approachesinthe Intensivecareunit: Sarah B. Doernberg,, Henry F. ChambersecaicedoNo ratings yet
- Point Prevalence Study of Antibiotics Use in Paediatric Wards of A Tertiary Health Facility in Kaduna NigeriaDocument8 pagesPoint Prevalence Study of Antibiotics Use in Paediatric Wards of A Tertiary Health Facility in Kaduna NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Thu 2012Document5 pagesThu 2012Nadila Hermawan PutriNo ratings yet
- Rab 6Document11 pagesRab 6Belia DestamaNo ratings yet
- Access To Antibiotics Not A Problem in Some LMICsDocument2 pagesAccess To Antibiotics Not A Problem in Some LMICsdinNo ratings yet
- Ispub 6078Document5 pagesIspub 6078elsseNo ratings yet
- Antibiotics AngeleDocument12 pagesAntibiotics Angeleyehouenou carineNo ratings yet
- Glaser 2017Document7 pagesGlaser 2017Dicky StefanusNo ratings yet
- 2020 Article 5771Document11 pages2020 Article 5771Nindie AulhieyaNo ratings yet
- Assessing The Construct Validity and Reliability of The Parental Perception On Antibiotics (PAPA) ScalesDocument9 pagesAssessing The Construct Validity and Reliability of The Parental Perception On Antibiotics (PAPA) ScalesAl ANo ratings yet
- Athal ResearchDocument6 pagesAthal ResearchHafsa TareenNo ratings yet
- Antibiotics Self MedicationDocument6 pagesAntibiotics Self Medicationcristanlacano07No ratings yet
- Tropical Med Int Health - 2017 - Barber - Prevalence and Correlates of Antibiotic Sharing in The Philippines AntibioticDocument9 pagesTropical Med Int Health - 2017 - Barber - Prevalence and Correlates of Antibiotic Sharing in The Philippines AntibioticNessy Nicholle SatruionNo ratings yet
- Determinants Impacting The Use of Antibiotics Among Patients Visiting The Dental Clinic at Kampala International University Teaching Hospital in Bushenyi-Ishaka Municipality, WesteDocument15 pagesDeterminants Impacting The Use of Antibiotics Among Patients Visiting The Dental Clinic at Kampala International University Teaching Hospital in Bushenyi-Ishaka Municipality, WesteKIU PUBLICATION AND EXTENSIONNo ratings yet
- Venugopalan2016 PDFDocument7 pagesVenugopalan2016 PDFSyahidatul Kautsar NajibNo ratings yet
- Community Knowledge Study on Antibiotic UseDocument6 pagesCommunity Knowledge Study on Antibiotic UseanantanabilaismiNo ratings yet
- 15684-Article Text-51937-1-10-20220301Document12 pages15684-Article Text-51937-1-10-20220301omniyaNo ratings yet
- Rab 8Document21 pagesRab 8Belia DestamaNo ratings yet
- Assessment of Public Knowledge of Antibiotic Use and Antimicrobial Resistance in Gusau NigeriaDocument4 pagesAssessment of Public Knowledge of Antibiotic Use and Antimicrobial Resistance in Gusau NigeriaAbdullahi ManirNo ratings yet
- Zakaael Din2018Document9 pagesZakaael Din2018anantanabilaismiNo ratings yet
- Study of Antibiotic Prescription in A Pharmacy in The City of Batna (Algeria)Document3 pagesStudy of Antibiotic Prescription in A Pharmacy in The City of Batna (Algeria)International Journal of Innovative Science and Research TechnologyNo ratings yet
- The Impact of Stewardship Programmes On Antibiotic Consumption PatternsDocument20 pagesThe Impact of Stewardship Programmes On Antibiotic Consumption PatternsRaphael AmponsahNo ratings yet
- Knowledge, Attitude and Practice of Antibiotics: A Questionnaire Study Among 2500 Chinese StudentsDocument9 pagesKnowledge, Attitude and Practice of Antibiotics: A Questionnaire Study Among 2500 Chinese StudentsAnonim musNo ratings yet
- Antibiotics 12 00560Document12 pagesAntibiotics 12 00560Rone yefer quezada peñaNo ratings yet
- Resistensi AntibiotikDocument21 pagesResistensi AntibiotikMaruliTuaNo ratings yet
- Antibiotic in PicuDocument4 pagesAntibiotic in PicuVickha Dian HapsariNo ratings yet
- antibiotics-11-00308 (2)Document17 pagesantibiotics-11-00308 (2)Beatrice BănicăNo ratings yet
- Antibiotic 02Document4 pagesAntibiotic 02Arslan ShahNo ratings yet
- Antibiotic Use and Resistance in ChildrenDocument15 pagesAntibiotic Use and Resistance in ChildrenAnastasia PasaribuNo ratings yet
- RRL Antibiotic 2 PDFDocument3 pagesRRL Antibiotic 2 PDFElaiza Mae MedidasNo ratings yet
- Evaluation of Prescribing Patterns of Antibiotics in General Medicine Ward in A Tertiary Care HospitalDocument6 pagesEvaluation of Prescribing Patterns of Antibiotics in General Medicine Ward in A Tertiary Care HospitalEditor IJTSRDNo ratings yet
- Antibiotics 11 00074Document10 pagesAntibiotics 11 00074fahira amandaNo ratings yet
- Access To Antibiotics Through Prescription and NonDocument17 pagesAccess To Antibiotics Through Prescription and NonBrandon TanNo ratings yet
- Chapter-1Document48 pagesChapter-1placalus nimbusNo ratings yet
- Antibioticknowledge AJICarticle 2017Document5 pagesAntibioticknowledge AJICarticle 2017Ruliana WatiNo ratings yet
- Antibiotics Use and Misuse in Children: A Knowledge, Attitude and Practice Survey of Parents in IndiaDocument4 pagesAntibiotics Use and Misuse in Children: A Knowledge, Attitude and Practice Survey of Parents in IndiaWahidNo ratings yet
- PR1 Chapter 1 2Document15 pagesPR1 Chapter 1 2hhahahaahahahahaha72No ratings yet
- Antimicrobial Stewardship: Attempting To Preserve A Strategic ResourceDocument7 pagesAntimicrobial Stewardship: Attempting To Preserve A Strategic Resourcem1k0eNo ratings yet
- Environment International: A B A A B D A A A C A BDocument9 pagesEnvironment International: A B A A B D A A A C A Bduverney.gaviriaNo ratings yet
- 1589 8705 4 PBDocument8 pages1589 8705 4 PBMbamali ChukwunenyeNo ratings yet
- IJCP 9999 E14081Document11 pagesIJCP 9999 E14081Gayathiri GovindarajuNo ratings yet
- Evaluation of Outpatient Antibiotic Use in Beijing General Hospitals in 2015Document9 pagesEvaluation of Outpatient Antibiotic Use in Beijing General Hospitals in 2015UdtjeVanDerJeykNo ratings yet
- Journal PNTD 0006822Document22 pagesJournal PNTD 0006822Ade margusNo ratings yet
- Antibiotics 11 00791 v2Document16 pagesAntibiotics 11 00791 v2Retno WahyuningrumNo ratings yet
- Dental Practitioner's Knowledge and Practices Regarding Antibiotic Prescription and Development of Resistance: A Cross Sectional StudyDocument5 pagesDental Practitioner's Knowledge and Practices Regarding Antibiotic Prescription and Development of Resistance: A Cross Sectional StudyClaypella MaskNo ratings yet
- Parents' Knowledge, Attitude and Practice of Antibiotic Use For Upper Respiratory Tract Infections in Children in The United Arab EmiratesDocument10 pagesParents' Knowledge, Attitude and Practice of Antibiotic Use For Upper Respiratory Tract Infections in Children in The United Arab EmiratesWahidNo ratings yet
- Prevalence and Determinants of Innapropiate Antibiotic E004993.fullDocument11 pagesPrevalence and Determinants of Innapropiate Antibiotic E004993.fullDava AsoiNo ratings yet
- ENTDocument9 pagesENTsurendra Prasad GuptaNo ratings yet
- This Study Resource WasDocument2 pagesThis Study Resource WasferzaNo ratings yet
- Knowledge, Attitude and Practices of Antibiotic Usage Among Students From Mumbai UniversityDocument5 pagesKnowledge, Attitude and Practices of Antibiotic Usage Among Students From Mumbai UniversityFiji IndahNo ratings yet
- en The Influence of Pharmaceutical Care IntDocument7 pagesen The Influence of Pharmaceutical Care IntMiftahul Jannah MNo ratings yet
- Evaluasi Kualitatif Terapi Antibiotik Pada Pasien Pneumonia Di Rumah Sakit Pendidikan Surabaya IndonesiaDocument5 pagesEvaluasi Kualitatif Terapi Antibiotik Pada Pasien Pneumonia Di Rumah Sakit Pendidikan Surabaya IndonesiadeskaNo ratings yet
- Self Medication and Indiscriminate Use oDocument12 pagesSelf Medication and Indiscriminate Use oMr AggarwalNo ratings yet
- 2018 Aisyah Faunavol31n3p194Document5 pages2018 Aisyah Faunavol31n3p194HellcroZNo ratings yet
- Preventive Veterinary MedicineDocument13 pagesPreventive Veterinary MedicineAbdul Wahab Assya RoniNo ratings yet
- Principi 2016Document8 pagesPrincipi 2016RaffaharianggaraNo ratings yet
- Longitudinal Clinical Evaluation of Antibiotic Use Among Patients With InfectionDocument11 pagesLongitudinal Clinical Evaluation of Antibiotic Use Among Patients With InfectionMITA RESTINIA UINJKTNo ratings yet
- New England Journal Medicine: The ofDocument13 pagesNew England Journal Medicine: The ofSorina ElenaNo ratings yet
- Jadwal Bimbingan PersonalDocument1 pageJadwal Bimbingan PersonalGemala AdillawatyNo ratings yet
- Jamainternal Tamma 2017 Oi 170042Document8 pagesJamainternal Tamma 2017 Oi 170042Gemala AdillawatyNo ratings yet
- Tormj 8 66 PDFDocument8 pagesTormj 8 66 PDFdalilaa13No ratings yet
- Heart Failure TreatmentDocument3 pagesHeart Failure TreatmentDaniel AndinoNo ratings yet
- Combined Use of Antibiotics As A Risk Factor For HDocument15 pagesCombined Use of Antibiotics As A Risk Factor For HGemala AdillawatyNo ratings yet
- Heart Failure TreatmentDocument3 pagesHeart Failure TreatmentDaniel AndinoNo ratings yet
- Meta AnalysisDocument6 pagesMeta AnalysisGemala AdillawatyNo ratings yet
- Toxicologic Emergencies, 11th Goldfrank's 2019Document10 pagesToxicologic Emergencies, 11th Goldfrank's 2019RenéNo ratings yet
- Parasitology Guide Questions 1Document2 pagesParasitology Guide Questions 1Cess LacatangoNo ratings yet
- 10 Science Imp Ch8 1Document8 pages10 Science Imp Ch8 1Rohan SenapathiNo ratings yet
- Effect of Punarnava and Bhumyamalaki in Physiological JaundiceDocument7 pagesEffect of Punarnava and Bhumyamalaki in Physiological JaundiceMulayam Singh YadavNo ratings yet
- Chemical Carcinogenesis: Metabolic Activation, DNA Adducts, Multistage ModelDocument85 pagesChemical Carcinogenesis: Metabolic Activation, DNA Adducts, Multistage ModelNidyaletchmy ReddyNo ratings yet
- Jurnal SkripsiDocument10 pagesJurnal Skripsinorma. nlmhNo ratings yet
- Nanotech MedDocument12 pagesNanotech MedDaphane Kate AureadaNo ratings yet
- Section 1: Organizing Data: Line List Line ListingDocument45 pagesSection 1: Organizing Data: Line List Line ListingFareeha KhanNo ratings yet
- Recat Medical BoardDocument5 pagesRecat Medical BoardNavara Naveen kumarNo ratings yet
- Segamat District Muet Final Year Lower 6 Exam-Govin2Document20 pagesSegamat District Muet Final Year Lower 6 Exam-Govin2govinjementah100% (1)
- LEAK REPAIR PROGRAMSDocument2 pagesLEAK REPAIR PROGRAMSPradip GuptaNo ratings yet
- Necrotizing InfectionsDocument57 pagesNecrotizing InfectionsRuffaeelJabrNo ratings yet
- Recommendations For The Use of Immunoglobulin Therapy For Immunomodulation and Antibody ReplacementDocument7 pagesRecommendations For The Use of Immunoglobulin Therapy For Immunomodulation and Antibody ReplacementChih-I LeeNo ratings yet
- Hair NailsDocument4 pagesHair Nailsapi-26570979No ratings yet
- 10 Surprising Health Benefits of NeemDocument5 pages10 Surprising Health Benefits of NeemMichel AdamNo ratings yet
- Trend Analysis of Exponential Increase of COVID-19 Cases in Pakistan: An InterpretationDocument21 pagesTrend Analysis of Exponential Increase of COVID-19 Cases in Pakistan: An InterpretationBongoNo ratings yet
- Gram Positive Cocci Bacteriology ChartDocument2 pagesGram Positive Cocci Bacteriology ChartIsabella CeaNo ratings yet
- Liu2011 PDFDocument6 pagesLiu2011 PDFAnonymous cUzAJWocPCNo ratings yet
- Applications of Calcium and Its Supplement Derived From Marine OrganismsDocument8 pagesApplications of Calcium and Its Supplement Derived From Marine OrganismsDewi SariNo ratings yet
- AS 1680.0-1998 Interior Lighting-Safe MovementDocument17 pagesAS 1680.0-1998 Interior Lighting-Safe Movementvxzvzxvzv0% (1)
- IOC Investors' Report Final 16 Aug 2019Document21 pagesIOC Investors' Report Final 16 Aug 2019Amri Satria NugrahaNo ratings yet
- Lund-Browder Chart Estimates Burn ExtentDocument7 pagesLund-Browder Chart Estimates Burn ExtentMarco1998No ratings yet
- Typhoid Fever Epidemics in the Philippines: Contaminated Wells as Risk FactorDocument5 pagesTyphoid Fever Epidemics in the Philippines: Contaminated Wells as Risk Factorjessica_nava_8No ratings yet