Professional Documents
Culture Documents
Nob 30073
Nob 30073
Uploaded by
maroua aouadi0 ratings0% found this document useful (0 votes)
11 views4 pagesCopyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views4 pagesNob 30073
Nob 30073
Uploaded by
maroua aouadiCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 4
Ss
Spinal Neurosarcoidosis Mimicking an Idiopathic
Inflammatory Demyelinating Syndrome
Necraj Kumar, MD; Elliot M, Frohman, MD, PhD
Background: Intramedullary neurosarcoidosis may
be the first and only manifestation of the disease
and may mimic an idiopathic inflammatory demyelin-
ling syndrome both clinically and on neuroimaging
results,
Metheds and Results: Two patients who were seen
initially witha relapsing-remitting neurologic course and
1 cervical intramedullary lesion on magnetic resonance
imaging findings are reported. Both proved to have net-
rosarcoidosis. A computed axial tomographic scan of the
chest showed hilar adenopathy, which provided a clue
to the diagnosis,
Conelustons: Symptoms duc to an intramedullary cer
vical lesion ean be the first manifestation of neurosarcotd-
sis, The clinical course can mimic a demyelinating ill-
ness. high index of suspicion and a search for sarcoidosis
atextraneural sites are required foran early diagnosis, Se-
roid treatment is associated with a favorable outcome.
“Arch Neurol. 2004;61:586-589
From the Department of
Neurology, Mayo Clini
Rochester, Minn (Dr Kumar)
and the Department of
Neurology and Ophthalmology
The University of Texas
Southiestern Medical Center at
Dallas (Dr Frohman).
Downloaded From: https:
LINICAL INVOLVEMENT OF
the central and/or periph-
eral nervous system ac
ccurs in 5% of patients with
sarcoidosis.' On autopsy
about L4 bof patients with sarcoidosis have
central nervous system involvement Ap-
proximately 50% of patients with neuro-
sarcoidosis initially have neurologic mani-
{estations. In the remainder of patients, the
neurologic manifestations appear within 2
ars of the diagnosis of sarcoidosis.’ The
‘most common sites of involvement in sar
coidosis are the lungs and pulmonary
lymph nodes. Neurosarcoidosis is most
commonly associated with granuloma-
tous infiltrates involving the meninges, hy-
pothalamus, pituitary gland, and cranial
nerves.” Spinal sarcoidosis is relatively un-
common and can manifest as intramedul-
lary lesions, intradural extramedullary oF
extradural lesions, cauda equina syn-
drome, and arachnoidiis." We report 2 pa-
tients with a cervical cord lesion in con-
junction with clinical manifestations
suggestive of a myelopathy. In both pa-
tients, a diagnosis of an idiopathic inflam-
matory demyelinating syndrome was con-
sidered likely. Further, the results of
‘magnetic resonance imaging (MRI) showed
characteristics that were distinctively con-
spicuous for an intra-axial process with a
concomitant leptomeningeal component.
(aepnuyreo) ARCH NEDROUNOUaT, APE Sor
ees J
CASE L
27-year-old African American woman
‘was symptomatic with numbness involy-
ing the right arm, trunk, and leg in De
cember 1997. This resolved spontane-
ously in 2 weeks. In September 1998, she
developed numbness involving the me-
dial aspect of both hands, The MRI r.
sults ofthe cervical spine showed a gado-
liniui-cnhancing lesion within the spinal
cord at Co-7 (Figure 1). the lesion ap-
peared tobe localized to the posterior
pect of the spinal cord. On sagittal s
quences, i was dificult to differentiate
Whether the lesion was exclusively intra
tial or whether there vas @ component
of leptomeningcal involvement. The MRI
resulls of the brain were normal. Cere-
brospinal fluid studies; levels of anti-
nuclear antibodies, angiotensin-con-
verting enzymes, and vitamin Bs syphilis
and Lyme serologies; and chest radio-
griphic and purified protein derivativeskin
test results were all normal. The patient
was treated with intravenous methylpred-
nisolone (1 g daily for 3 days) and im-
proved significantly. She was diagnosed as
having an idiopathic inflammatory demsy-
clinating syndrome. In February 1999, she
developed an episode of right facial murmb-
(©2004 American Medical Association, All rights reserved.
jamanetwork.comy on 02/22/2021
Downloaded From: https:
Figure 4. SagitalT-wightad (A) and axial (8
that appar to Rae abroad tase verte surlace fhe cord
ness with right facial hypesthesia, which resolved spon-
taneously in a few days. Her general medical and neu-
rologic examination results were unremarkable. Repeated
cervical spine MRI results showed persistent enhance-
ment ofthe cervical cord lesion, Repeated brain MRI re-
sults Were again unremarkable
‘A computed axial tomographic scan ofthe chest re-
vealed hilar adenopathy, and diffuse echogenic lesions
were scen in the liver and spleen on the abdominal com-
puted axial tomographic scan, A repeated angiotensin-
converting enzyme level test showed values were el-
evated at 121 U/L (reference range, 7-46 U/L)
Transbronchial biopsy results identified noncaseating
grinulomas consistent with sarcoidosis, She was pre-
scribed oral prednisone at 60 mg/d. She developed no re
currence of neurologic symptoms; the spinal cord le-
sion and anglotensin-converting enzyme levels decreased,
and the prednisone was tapered across 1 year.
CASE 2
‘A 3o-year-old man had been symptomatic since July 1999
With slowly progressive numbness involving the hands and
feet, Cervical spine MRI results were remarkable for an en
hancing intramedullary lesion at C4-C5. A biopsy of the
lesion was performed, and a review of the slides revealed
evidence of mild acute inflaammation and benign Hbrous
Uissue, He was given steroids in the postoperative period,
(aepeay TED) TECH NEDROUVOL@T APES
cl cord magnate reanance mages shoving dos lated enhancing nama estan (rons)
and his paresthesias showed significant improvement. In
October 1999, he developed a recurrence ofthe paresthe-
sias, which progressed slowly intially and then more rap-
ily for the months prior to his evaluation, He was symp-
tomatic with numbness below the neck and decreased
ability to appreciate hot and cold sensations, on the right
side more than the elt, He had difficulty opening jars and
some coordination difficulty with his legs, His neuro-
logic examination results showed decreased perception of
pinprick, temperature, and touch from C4 downward, on
the right side more than the left. Strength, tone, and co-
ordination were intact. His reflexes were symmetrically
brisk, and the plantar responses were flexor. His gait was,
normal, and Romberg test resuils were negative
Cervical spine MRL results (Figure 2) revealed a 2-cm
lesion inthe dorsal part ofthe cervical cord at C4-C5. The
lesion appeared to be infiltrated over the posterior cord
surface and showed pronounced contrast enhancement.
Also noted were anterior and posterior leplomeningeal
enhancements, Brain and thoracic cord MRI results were
normal, Normal values were obtained from a hemo-
gram, and for vitamin B,,, folate, liver enzymes, angio-
tensin-converting enzymes, immunoelectrophoresis, thy-
rolropin, and antinuclear antibodies. Evoked potential
studies (brainstem, visual, and somatosensory) and re
sults of spinal fluid analysis were normal.
A computed axial tomographic scan of the chest
showed bilateral hilar and mediastinal adenopathy. The
figure 2. SopitalT-usightd cena cord magne reeonacs image soning a hyactaee2-m lion with
ervieacorda te C4 lees. 8, Pesigadonium Twit magts resonates age shang protouced conta,
‘hamid ard dol portions
fethaneeent wih ane and pater plomeningel nksnesmen ar).
bronchoalveolar lavage showed numerous macrophages
and sparse inflammatory cells, predominantly histio-
cytes, Transbronchial biopsy results showed a compact,
well-cireumscribed noncaseatin
Langerhans and foreign body-type multinucleated giant
cells with abundant eosinophilic cytoplasin,
eb}
Wis rare for intramedullary spinal sarcoidosis to be thei
snuloma composed of
Uial or only manifestation of the disease.** In our 2 re-
ported cases, there were no systemic symptoms. Never-
theless, both had hilar adenopathy, which led to the
diagnosis of neurosarcoidosis, The age range for intra-
medullary sarcoidosis s 15 1068 years (median, 35 years).
In spinal sarcoidosis, the cervical region is most com-
monly involved.* The clinical picture is usually that of «
myelopathy with paraparesis, quadriparesis, hypesthe-
sias, and bladder and bowel dysfunction all being well-
described symptoms.” Intramedullary neurosarcoidosis is
known to mimic a spinal cord tumor both clinically and
radiologically. Spontaneous remissions and relapses and
steroid-induced improvement can lead to a clinical pic-
lure that resembles an inflammatory demyelinating dis-
case, This is well illustrated by the 2 cases presented,
Both patients had an enhancing cervical cord le-
sion that appeated to infiltrate over the posterior cord
surface, The second ease described had ev
terior and posterior leptomeningeal enhancement. It has
been suggested that with early inflammation there is lin-
cat leptomeningeal enhancement along the surface of the
spinal cord.” Spread of the leptomeningeal inflamma-
Lory process to the Virchow-Robin spaces is believed to
resull in parenchymal involvement, which appearsas di
butragular margin (trou) win
> With consolida-
fuse cord enlargement on MRI results
don, 1 of more discrete masses form, and with resoli-
tion ofthe inflammatory phase, the cord returns to normal
Ultimately, these processes eat culminate in spi-
nal cord atrophy.” The MRI characteristics of spinal new-
rosarcoid lesions depend on the stage ofthe illness, Most
findings can be relatively nonspecific, but the presence
of an infiltrating lesion with meningeal and intramedul-
lary enhancement should increase the suspicion for sar-
coidosis or other granulomatous diseases. Enhance-
ment patterns are variable and can include linear
leplomeningeal enhancement or focal, multifocal, oF dif
fuse intraparenchymal enhancement; often, there is a
broad base on the cord surface and the enhancement does
not involve the full cord thickness.™™ A decrease in MRI
enhancement can be seen as patients improve.”
In neurosarcoidosts, extradural spinal disease is rare
and can involve the vertebral bodies." Sarcoid spon-
dylodiseitis and paraspinal mass have been reported,
Enlarged cervical nerve roots, not evident om MRI re-
sults but evident on a myelogram, have been de-
scribed." Intradural extramedullary space occupying the
leston'” and intraspinal epidural mass secondary to sat-
coidosis can occur, Intradural extramedullary findings
include pial enhancement, root nodules, and clumping,
Enhancing cauda equina lesions mim-
fcking subarachnoid tumor seeding can occur." Intra-
appear as an enhancing
intramedullary lesion, cord enlargement, cord atrophy
oF diffuse and focal T2-weighted signal hyperintensi-
ties.” The only abnormality may be abnormal enhance:
ment with normal cord appearance on T1- and T
weighted images.” Multiple small nodules on enhanced
T1-weighted cervical cord MRI results ean occur." Cases
medullary disease can intially
‘of spinal sarcoidosis with unique MRI findings due to he-
mosiderin deposition®? and caleification” in the lesion
have been described. Also described is a case of spinal
sarcoidosis mimicking syringomyelia on MRI results.”
1m both our patients, the diagnosis was provided by
transbronchial biopsy results. Infact, in our second pa-
tient, the spinal cord biopsy’ results did not provide the di-
agnosis, The granulomas inthe spinal cord and brain are
‘often poorly formed, are smaller than the systemic le-
sions, and have fewer giant cells For this reason, the
spinal cord lesions can mimic an intramedullary tumor on
frozen section.** Further attempts at wide surgical exei-
sion can lead to increased morbidity. Case reports of pax
tients undergoing spinal cord biopsy in intramedullary spi-
nal sarcoidosis suggest a high morbidity and mortality."
Intramedullary spinal sarcoidosis should be care
fully considered as a possibility in a patient with known
sarcoidosis who develops a radiculopathy or myelopa-
thy. On rare occasions, intramedullary spinal sarcoid~
‘osis may be the initial manifestation of sarcoidosis, Mani-
festation mimicking a cord neoplasm is more common,
bbut a relapsing-remitting neurologic course can occur.
‘An infiltrating intramedullary cord lesion with lepto-
meningeal enhancement should bring to mind the pos-
sibility of sarcoidosis. A systematic search for evidence
of extrancural sites of involvement should be manda-
tory in such cases. Even inthe absence of systemic symp-
toms, targeting such sites for potential biopsy can result
in the identification ofthe disease process with substan-
tially less morbidity than sampling neural tissue. A high
index of suspicion for the diagnosis is required because
carly intervention is associated with a favorable out-
‘come. Progressive deterioration, nontesponsiveness 10 ste-
roids, and an enlarging cord mass should prompt recon-
LaF, Gasman Ro atc inthe haan pi: pect of
anes ard aoa response'o strod hap. Am Jura
sone 15 47208,
a AL, ype GW Spal ord scsi, Ann Heol 197717085,
unger 88S 8 Ler SR. Spo , Mari MssoF nearer spinal
‘stolons cncal nd mae sunaes magi crc, Nev
oy 0868-35-97,
Sse J, Dotan FO, Sonal TE ta Sota spialcorl sarcoiais wit
oer maniestain of ssa sods. Cin maging 19721172
Mags, Oeubo K Shins Sacovei th pil od epea an a
topy sas and ravi ote hate, te Patlagcs ponte. 06535
sar 122.
Nett MMe GM, Baler HL bral ML, Sedat BY, Spica cort
‘staios ane nding tM imaging wh G4-TPR erase ad
yy 1080173850808,
‘gboqu BN, Stem Bl, Sel Cane. Thecapeutie considerations inpatients
th eacry euosareacsis Ach Mel 1005527597
Fier A, ia A Kies I, Hoa CD MR imaging changes andar
verbal saraiosis, JR A jorge. 100,75 354-356,
Franco aseronC. Tei, Vet, Beis, Longer radograpic
fala ap naps wihetosra sree oth spa nd pl a
ham nl Ea 1008 5585-50.
hia KO, Paterna , Wack Al, own WO, Shute HS. Secs
‘fhe pil cod wth cn vrtbal evant ce repo. Cont
‘Med iagig Graph 085188346,
ana CG i. MR oso ponds. J Comput Asst,
Tomogr 188216880652
naga, Hara Yamoto M, Yoshida. Acae of sad oases:
hye ve roo sling dems mysegahy pines. Fi
sho Shia. 109232384360,
Barua Glsuer FE, SR, Sih GH. acids ofthe carve pial e-
rales ep. Nevosurpey 1783216218
Weissmen Lage Kel BaeaK Abel. nasi piu saci
is case report Neursurgey 19869-17918,
uz Post MD, Gas Wt Infanmstay nits pr
vil pte. Nerimagng Cin A195 40-25.
ace MK Tats, Tusa S Kong, Tuoinen lad newoss-
ois: MR ings ad pablo colton. Acta Fala 2002
Ser.
ine Ese AD. Sarcoidosis of te cna neous syst, Neroimagng
‘lin, 10-114- 158
oft
an Wang prs regener ae
sideration of the diagnosis. In such cases, performing a Mra Src es pergasaycramet
biopsy of neural tissue may be inevitable 21 Yona Yu Stel Hope Sha Ac
sets pn essing
Accepted for publication August 13,2003. sacar
Thathorcontbutions: Sid concept and design (Drs 2 Wate Sa Tank Wl AR np otras
Kumarand Frohman); acquisition of data (Drs Kumar and Men Ra DOR TES TET
: 2 Wan Mae oa AB Gn. tanta
Frohman); analysis ard interpretation of data (Dts Kumar" MGM E ewe Sone bo erate
and Frohman): drafingfthe manuscript (Drs Kumar and 2 Wane ace hes Asal ewe pdr oping
Frobinan); crt revision ofthe manuscript or important htt pasa asian icing speech
intellectual content (Dr Frohman); administrative, techni- os eee Shih Eusabe Alsen Spins eord sacoidoss WY
‘al, and material support (Dr Kumar); study supervision (De (esha erie Cn
Frohman) 25 Sar Path Ks DA Mopaticmsaroos gps ae
Corresponding author Eliot M. Frohman, MD, PhD, > ates i ay 1 DBT
Deparment of Newolagy and Ophthalmology, The Unie 2 Tanna owe at aman asa, Ys Si
‘caper pre myepny. ipa 7
re of ne Souter ade Ceterat Dall 5229 ag. Ler oar ote 8 mans ros
elliot jrohman@utsouthwestern. cd). Sime se Soin snare tsuen: N27
22 Sonn pet Rhu Semen pr sei
fpr na 7 29 86
EE itn 0, ce ena aed sari
Sis mpl acoA Ararat ab 708
1 Sams Kn A ne, Sat as Sanco: 5 faa Ser Lamy odo fic pots
inane Ao hr hes 7 in negate eas
2. Rr Cal Seco cneptingereen neh, 92a ater an et anti st
gee aap. Ann Pa S672 ropa rey Pc errr
(©2004 American Medical Ass
‘Downloaded From: https:/jamanetwork.com/ on 02/22/2021
lation, All rights reserved.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- La Checklist de La Médecine VasculaireDocument304 pagesLa Checklist de La Médecine Vasculairemaroua aouadi100% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 1 Diagnostic D'une Fievre D'origine IndetermineDocument8 pages1 Diagnostic D'une Fievre D'origine Indeterminemaroua aouadiNo ratings yet
- 16le Syndrome PneumorenaleDocument12 pages16le Syndrome Pneumorenalemaroua aouadiNo ratings yet
- #Critères de Diagnostic Des Myosites Idiopathiques EULARDocument2 pages#Critères de Diagnostic Des Myosites Idiopathiques EULARmaroua aouadiNo ratings yet
- Tumeur CarcinoideDocument14 pagesTumeur Carcinoidemaroua aouadi100% (1)
- Atpp 9782294728341Document10 pagesAtpp 9782294728341maroua aouadiNo ratings yet
- ZonaDocument25 pagesZonamaroua aouadiNo ratings yet
- DR Aouadi Maroua Neurosarcoidose 2021Document42 pagesDR Aouadi Maroua Neurosarcoidose 2021maroua aouadiNo ratings yet
- AbecedaireendoscopieDocument218 pagesAbecedaireendoscopiemaroua aouadiNo ratings yet
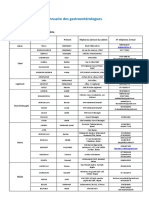
- Annuaire Des GastroenterologuesDocument14 pagesAnnuaire Des Gastroenterologuesmaroua aouadiNo ratings yet
- Variétés Anatomo-Pathologiques Du Granulome Aspects PathologiquesDocument48 pagesVariétés Anatomo-Pathologiques Du Granulome Aspects Pathologiquesmaroua aouadiNo ratings yet
- Introduction To Data Science: For-Ian V. Sandoval Asst. Professor II Laguna State Polytechnic UniversityDocument62 pagesIntroduction To Data Science: For-Ian V. Sandoval Asst. Professor II Laguna State Polytechnic Universitymaroua aouadiNo ratings yet
- 2494-Article Text-21383-1-10-20210317Document431 pages2494-Article Text-21383-1-10-20210317maroua aouadiNo ratings yet
- Item 207 SARCOIDOSE-dDocument16 pagesItem 207 SARCOIDOSE-dmaroua aouadiNo ratings yet
- 101 Cas Cliniques Observés Dans Un Cabinet de Médecine Interne DR Bouferroum Partie 01Document272 pages101 Cas Cliniques Observés Dans Un Cabinet de Médecine Interne DR Bouferroum Partie 01maroua aouadi100% (1)
- Erythème NoueuxDocument36 pagesErythème Noueuxmaroua aouadiNo ratings yet
- Diarrhées Chroniques - PPTX Cours 2019Document51 pagesDiarrhées Chroniques - PPTX Cours 2019maroua aouadiNo ratings yet
- Erythème NoueuxDocument36 pagesErythème Noueuxmaroua aouadiNo ratings yet