Professional Documents
Culture Documents
2 - Diabeticfootdisease 4 - Cornerstonesoffootulcer Prevention
Uploaded by
Eva Cica SusantiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2 - Diabeticfootdisease 4 - Cornerstonesoffootulcer Prevention
Uploaded by
Eva Cica SusantiCopyright:
Available Formats
2 of 10 SCHAPER ET AL.
The authors, as members of the editorial board of the IWGDF, thickened skin (callus). The callus then leads to a further increase in
have summarized the information from these six chapters and also the loading of the foot, often with subcutaneous haemorrhage and
provide additional advice based on expert opinion in selected areas eventually skin ulceration. Whatever the primary cause of ulceration,
for which the guideline chapters were not able to provide evidence- continued walking on the insensitive foot impairs healing of the ulcer
based recommendations. We refer the reader for details and back- (see Figure 1).
ground to the six evidence-based guideline chapters1-6 and our devel- PAD, generally caused by atherosclerosis, is present in up to 50%
7
opment and methodology document ; should this summary text of patients with a diabetic foot ulcer. PAD is an important risk factor
appear to differ from information of these chapters, we suggest the for impaired wound healing and lower extremity amputation. A small
reader defer to the specific guideline chapters.1-6 Because terminol- percentage of foot ulcers in patients with severe PAD are purely
ogy in this multidisciplinary area can sometimes be unclear, we have ischaemic; these are usually painful and may follow minor trauma. The
8
developed a separate IWGDF Definitions and Criteria document. majority of foot ulcers, however, are either purely neuropathic or
The information in these practical guidelines is aimed at the global neuro-ischaemic, that is, caused by combined neuropathy and ischae-
community of health care professionals involved in the care of per- mia. In patients with neuro-ischaemic ulcers, symptoms may be absent
sons with diabetes. The principles outlined may have to be adapted or because of the neuropathy, despite severe pedal ischaemia. Recent
modified based on local circumstances, taking into account regional studies suggest that diabetic microangiopathy (so-called “small vessel
differences in the socio-economic situation, accessibility to and disease”) does not appear to be the primary cause of either ulcers or
sophistication of health care resources, and various cultural factors. of poor wound healing.
2 | DIABETIC FOOT DISEASE 4 | C O R N E R S T O NE S O F F O O T U L C ER
P RE V E N T I O N
Diabetic foot disease is among the most serious complications of dia-
betes mellitus. It is a source of major suffering and financial costs for There are five key elements that underpin efforts to prevent foot
the patient and also places a considerable burden on the patient's ulcers:
family, health care professionals and facilities, and society in general.
Strategies that include elements of prevention, patient and staff edu- 1. Identifying the at-risk foot.
cation, multidisciplinary treatment, and close monitoring as described 2. Regularly inspecting and examining the at-risk foot.
in this document can reduce the burden of diabetic foot disease. 3. Educating the patient, family, and health care professionals.
4. Ensuring routine wearing of appropriate footwear.
5. Treating risk factors for ulceration.
3 | PATHOPHYSIOLOGY
An appropriately trained team of health care professionals should
Although both the prevalence and spectrum of diabetic foot disease address these five elements as part of integrated care for people at
vary in different regions of the world, the pathways to ulceration are high risk of ulceration (IWGDF risk stratification 3).
similar in most patients. These ulcers frequently result from a person
with diabetes simultaneously having two or more risk factors, with
diabetic peripheral neuropathy and PAD usually playing a central role. 4.1 | Identifying the at-risk foot
The neuropathy leads to an insensitive and sometimes deformed foot,
often causing abnormal loading of the foot. In people with neuropa- The absence of symptoms in a person with diabetes does not exclude
thy, minor trauma (eg, from ill-fitting shoes or an acute mechanical or foot disease; they may have asymptomatic neuropathy, PAD, pre-
thermal injury) can precipitate ulceration of the foot. Loss of protec- ulcerative signs, or even an ulcer. Examine a person with diabetes at
tive sensation (LOPS), foot deformities, and limited joint mobility can very low risk of foot ulceration (IWGDF risk 0) annually for signs or
result in abnormal biomechanical loading of the foot. This produces symptoms of LOPS and PAD, to identify if they are at-risk for foot
high mechanical stress in some areas, the response to which is usually ulceration, including doing the following:
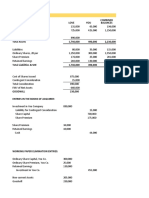
FIGURE 1 Mechanism of ulcer developing from repetitive or excessive mechanical stress
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Concepts of Personal BoundariesDocument11 pagesConcepts of Personal BoundarieshayazeNo ratings yet
- 5 Signs Showing You May Suffer From Mental Slavery' by Dr. Amos WilsonDocument4 pages5 Signs Showing You May Suffer From Mental Slavery' by Dr. Amos Wilsonebitechukwudi100% (3)
- Kripal, Debating The Mystical As The Ethical: An Indological Map, in Crossing Boundaries: Essays On The Ethical Status of Mysticism (2002) : 15-69Document28 pagesKripal, Debating The Mystical As The Ethical: An Indological Map, in Crossing Boundaries: Essays On The Ethical Status of Mysticism (2002) : 15-69Keren MiceNo ratings yet
- Science Quest 8 MatterDocument19 pagesScience Quest 8 MatterNoble_Truth100% (1)
- Pastor. The History of The Popes, From The Close of The Middle Ages. 1891. Vol. 31Document540 pagesPastor. The History of The Popes, From The Close of The Middle Ages. 1891. Vol. 31Patrologia Latina, Graeca et Orientalis100% (1)
- Business Combination 2Document3 pagesBusiness Combination 2Jamie RamosNo ratings yet
- Credit Transactions STUDENT Must ReadDocument6 pagesCredit Transactions STUDENT Must ReadLeilani Delgado MoselinaNo ratings yet
- The Life of SolomonDocument6 pagesThe Life of SolomonReste Marion MartizanoNo ratings yet
- Labyrinth Weir DesignDocument15 pagesLabyrinth Weir Designchutton681No ratings yet
- 4.3 - Educating Patients, Family, and Health Care Professionals About Foot CareDocument1 page4.3 - Educating Patients, Family, and Health Care Professionals About Foot CareEva Cica SusantiNo ratings yet
- Dmso 13 3703Document9 pagesDmso 13 3703Eva Cica SusantiNo ratings yet
- Literature Review: Foot Exercise Prevents The Risk of Neuropathy On Diabetes Mellitus PatientDocument8 pagesLiterature Review: Foot Exercise Prevents The Risk of Neuropathy On Diabetes Mellitus PatientEva Cica SusantiNo ratings yet
- TOEFL SKILL 7&9 THE TOPIC and THE ORDER ANSWERSDocument9 pagesTOEFL SKILL 7&9 THE TOPIC and THE ORDER ANSWERSEva Cica SusantiNo ratings yet
- The Parable of The Mangrove Man PoemDocument6 pagesThe Parable of The Mangrove Man PoemS MNo ratings yet
- 2012 ENGLESKI RAZNO1DocumentDocument353 pages2012 ENGLESKI RAZNO1DocumentDalibor PurhmajerNo ratings yet
- READINGDocument16 pagesREADINGRonalyn Tulabot - PasamaneroNo ratings yet
- Competency Checklist For CparDocument2 pagesCompetency Checklist For CparChristine Marie A Llanera-CadalloNo ratings yet
- VeCo12 3 Diagnostics 1 Geffers Lecture PDFDocument24 pagesVeCo12 3 Diagnostics 1 Geffers Lecture PDFGraciella Valeria Viana100% (1)
- Lesson Plan FoodDocument3 pagesLesson Plan FoodNur Aliyah Abdul RazakNo ratings yet
- What Is Political Art? What Makes Art Political?Document3 pagesWhat Is Political Art? What Makes Art Political?Abir PothiNo ratings yet
- Leif Eriksson-Annotated BibDocument7 pagesLeif Eriksson-Annotated Bibapi-308958050No ratings yet
- Chapter II Chapter II - Sanjay Shelar - 9890704605Document49 pagesChapter II Chapter II - Sanjay Shelar - 9890704605Webhub TechnologyNo ratings yet
- Chapter 5 & 6Document28 pagesChapter 5 & 6劉力僑 LIU,LI-CIAO E34116324No ratings yet
- CBSE Tuts: NCERT Class 10 Science Lab Manual - Image Formation by A Convex LensDocument16 pagesCBSE Tuts: NCERT Class 10 Science Lab Manual - Image Formation by A Convex LensVinodKumarTummalurNo ratings yet
- Teaching Third World Cinema Screen by Teshome H. GabrielDocument6 pagesTeaching Third World Cinema Screen by Teshome H. GabrielBunmi OloruntobaNo ratings yet
- 2016 GP Y5 Infopack - Media + Social Issues - FINAL PDFDocument104 pages2016 GP Y5 Infopack - Media + Social Issues - FINAL PDFMelissaNo ratings yet
- United States v. Troy Stephens, 7 F.3d 285, 2d Cir. (1993)Document8 pagesUnited States v. Troy Stephens, 7 F.3d 285, 2d Cir. (1993)Scribd Government DocsNo ratings yet
- f2f MUSICDocument44 pagesf2f MUSICRio CostalesNo ratings yet
- Assignment 1Document23 pagesAssignment 1Nguyen Tien Phat (K15 HCM)No ratings yet
- How Important Is Technology in EducationDocument3 pagesHow Important Is Technology in EducationEdilbert Bonifacio GayoNo ratings yet
- Chap6 - Mathematical StatisticsDocument3 pagesChap6 - Mathematical Statisticsalonebunny94No ratings yet
- Proposal On Comparative Study On TVS and HondaDocument7 pagesProposal On Comparative Study On TVS and HondaSatish KumarNo ratings yet
- Abc Chapter 2Document22 pagesAbc Chapter 2ZNo ratings yet
- Feeding Power To Arduino - The Ultimate GuideDocument24 pagesFeeding Power To Arduino - The Ultimate GuideMUSTAFANo ratings yet