Professional Documents
Culture Documents
100 Years of Insuinm
Uploaded by
João Guilherme HazinCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
100 Years of Insuinm
Uploaded by
João Guilherme HazinCopyright:
Available Formats
Journal of PJ Martens et
al. Arresting or curing type 1 249:2 T1–T11
Endocrinology diabetes
THEMATIC REVIEW
100 YEARS OF INSULIN
Arresting or curing type 1 diabetes: an elusive
goal, but closing the gap
Pieter-Jan Martens, Conny Gysemans and Chantal Mathieu
Clinical and Experimental Endocrinology (CEE), KU Leuven, Leuven, Belgium
Correspondence should be addressed to C Mathieu: chantal.mathieu@uzleuven.be
This paper forms part of a special section on 100 years of insulin. The guest editors for this section were James Cantley & Decio Eizirik
Abstract
Type 1 diabetes is one of the most common chronic diseases in children and Key Words
adolescents, but remains unpreventable and incurable. The discovery of insulin, already ff type 1 diabetes
100 years ago, embodied a lifesaver for people with type 1 diabetes as it allowed the ff beta cell
replacement of all functions of the beta cell. Nevertheless, despite all technological ff biomarkers
advances, the majority of type 1 diabetic patients fail to reach the recommended ff heterogeneous
target HbA1c levels. The disease-associated complications remain the true burden of ff immunotherapy
affected individuals and necessitate the search for disease prevention and reversal. The
recognition that type 1 diabetes is a heterogeneous disease with an etiology in which
both the innate and adaptive immune system as well as the insulin-producing beta cells
intimately interact, has fostered the idea that treatment to specific molecular or cellular
characteristics of the patient groups will be needed. Moreover, robust and reliable
biomarkers to detect type 1 diabetes in the early (pre-symptomatic) phases are wanted
to preserve functional beta cell mass. The pitfalls of past therapeutics along with the
Journal of Endocrinology
perspectives of current therapies can open up the path for future research. (2021) 249, T1–T11
Introduction
The year 2021 will celebrate the 100th anniversary of the but also acute complications like hypoglycemic
clinical use of insulin. This embodied a lifesaver for people attacks, episodes of severe hyperglycemia and diabetic
living with type 1 diabetes (T1D), the most common ketoacidosis. As a result, despite major advances in tools
chronic disease in children and young adolescents. But it to measure glucose levels and insulin therapy, life years
is not a cure, it is merely a part of our attempts to replace are still lost due to T1D. At present, people with T1D are
all functions of the beta cells that are destroyed in T1D. often treated with insulin analogs and use continuous
This means that therapy is based on symptom control glucose monitoring systems that can even be integrated
with glucose monitoring and administration of insulin with sensors and insulin pumps (i.e. hybrid closed-loop
according to algorithms based on food intake, exercise systems) resulting in important steps forward in therapy.
and other external factors. In many people with T1D, Despite these technical advancements, the hope of
tight glycemic control remains an elusive goal, resulting prevention and a cure for T1D remains. The fact that this
in long-term micro- and macrovascular complications, has not been achieved to date, is not for a lack of trying.
https://joe.bioscientifica.com © 2021 Society for Endocrinology
https://doi.org/10.1530/JOE-20-0552 Published by Bioscientifica Ltd.
Printed in Great Britain Downloaded from Bioscientifica.com at 01/03/2022 05:54:45PM
via free access
Journal of PJ Martens et al. Arresting or curing type 1 249:2 T2
Endocrinology diabetes
In the process, important lessons have been learned. Here, T cells (Tregs) are amongst the primary regulators of T1D
we describe some of these lessons and open up the path (Holohan et al. 2019). Translational errors have been
for future research. described as a potential source of antigenic peptides to
which central immune tolerance is lacking, but to which
cytotoxic T cells in the circulation of T1D patients are
Type 1 diabetes: a mistake of the present, causing destruction of the insulin-producing beta
insulin-producing beta cells, the immune cells (Kracht et al. 2017). In addition to mishaps in the
system or both? central immune system, in T1D, the peripheral immune
regulation appears defective as T cell receptor (TCR)
The dogma that the immune system in T1D mistakenly revision increases the T cell repertoire in the periphery.
destroys healthy insulin-producing beta cells in the Especially CD40-expressing CD4+ T cells alter their TCR
pancreas, leading to absolute insulin deficiency (Atkinson repertoire to become auto-aggressive (Wagner 2016,
& Eisenbarth 2001), is being challenged in recent years. Vaitaitis et al. 2017). Moreover, beta cell-specific CD8+ T
Dr Bottazzo in 1986 and Dr Atkinson in 2016 debated cells are present in equal numbers in the peripheral blood
the question: 'Death of a beta cell: homicide or suicide?' of healthy individuals and T1D patients but are found
(Bottazzo 1986, Atkinson et al. 2011). The definitive exclusively in the pancreas of T1D patients (Skowera
answer remains unknown, but both sides have strong et al. 2015, Culina et al. 2018). Yet, despite numerical
arguments. correlates, the phenotypic profile looks different in T1D
The classic hypothesis, first introduced by Dr with hallmarks of an antigen-driven expansion of beta
Eisenbarth in 1986, proposes that in an individual with a cell-specific CD8+ T cells (Skowera et al. 2015). This
predisposing genetic risk (mostly carried by specific types observation is supported by the exhaustion of these CD8+
of major histocompatibility complex (MHC) or human T cells in slow disease progressors (Wiedeman et al. 2020).
leucocyte antigen (HLA) genes), activation of the immune Another argument is that the HLA region, which enables
system by one or multiple environmental triggers results in antigen recognition by antigen-presenting cells, confers
a rapid destruction of the pancreatic beta cells (Eisenbarth the greatest contributor to the genetic susceptibility of
1986). This implies a malfunction of the immune system T1D (Mathieu et al. 2018).
as the culprit. The discovery of pancreatic islet cell If, on the other hand, abnormal pancreatic beta cells
autoantibodies (ICA), appearing in the period between would be the culprit, it would imply a normal function
immune activation and the onset of clinical symptoms, of the immune system as it then needs to clear these
proved to be a landmark discovery in two important dysfunctional cells. In this perspective, T1D etiology
aspects. First, it provided a method to predict the onset becomes comparable to effective anti-tumor immunity.
of diabetes. Furthermore, as different autoantigens (i.e. Several arguments support a primary defect in insulin-
insulin, glutamic acid decarboxylase (GAD), protein producing beta cells. First, recent observations suggest
tyrosine phosphatase (IA-2 or ICA512), zinc transporter 8 smaller pancreatic volumes in those affected or at risk
(ZnT8) and tetraspanin) were discovered, it became clear of T1D (Campbell-Thompson et al. 2019, Virostko et al.
that beta cell-specific proteins and peptide fragments were 2019). Second, clear signs of beta cell stress can be detected
targeted by the immune system (Bonifacio 2015). Another in those on their way to develop T1D, as illustrated by
strong argument that the immune system may be the an increased proinsulin-to-insulin ratio (Wasserfall et al.
causing factor in T1D came from the early observation 2017). This increased ratio suggests abnormalities in
that transplantation of non-T cell-depleted bone marrow insulin processing and vesicular trafficking (Rodriguez-
precipitated diabetes (Lampeter et al. 1993). Calvo et al. 2017). Moreover, non-specific triggers, like
In this hypothesis, as T1D is due to the aberrant increased metabolic demand or viral infections, have
recognition of autoantigens, the most likely cause would been shown to stress beta cells, inducing endoplasmic
be a failure of central tolerance. However, as thymic reticulum (ER) stress and have been associated with
involution occurs in mammals at puberty, this would imply T1D (Eizirik et al. 2013). ER stress eventually results in
that T1D would only occur prior to or soon after puberty components of the folding process being hampered,
(Wagner 2016). Moreover, thymic selection appears to be initiating the unfolded protein response (UPR) in order to
quantitatively similar between healthy individuals and optimize the folding capacity of the ER. However, if this
those with T1D (Culina et al. 2018). Yet, there seems to be a is unsuccessful, the beta cell is marked as dysfunctional
major qualitative difference, as thymus-derived regulatory and apoptosis is set in motion. However, UPR by itself
https://joe.bioscientifica.com © 2021 Society for Endocrinology
https://doi.org/10.1530/JOE-20-0552 Published by Bioscientifica Ltd.
Printed in Great Britain Downloaded from Bioscientifica.com at 01/03/2022 05:54:45PM
via free access
Journal of PJ Martens et al. Arresting or curing type 1 249:2 T3
Endocrinology diabetes
has the potential to trigger an inflammatory response First identified as a key regulator of Tregs, it was thought
that attracts immune cells and initiates the entire cascade to be yet another argument of a deficient immune system
leading to T1D (Eizirik et al. 2013). Moreover, ER stress in T1D (Roychoudhuri et al. 2013). Later, it was shown
may again increase the visibility of the beta cells to the that BACH2 has an essential anti-apoptotic role in the
immune system (Thomaidou et al. 2020). Therefore, protection of the insulin-producing beta cells against
ER stress constitutes a major contributory factor to the cytokine-mediated killing (Marroqui et al. 2014). It
beta cell dysfunction in early T1D (Eizirik et al. 2013). appears that BACH2 is moreover downregulated by pro-
As hyperglycemia stresses the beta cells even further, inflammatory cytokines, resulting in a chain of events in
this may result in a vicious circle, as was proven by the beta cells, already under immune assault (Marroqui et al.
observation that the decline in beta cell function was less 2014). Therefore, downregulation of BACH2 may result in
in intensively insulin-treated T1D patients (The Diabetes both a failing beta cell and immune system, or just be the
Control and Complications Trial Research Group 1998). result of evolving T1D. This illustrates the complexity of
The argument of ER stress as an etiologic factor of T1D the pathogenesis of T1D (Fig. 1).
was reinforced by the observation that in a T1D animal
model, the non-obese diabetic (NOD) mouse, avoidance
of ER stress resulted in T1D protection (Engin et al. 2013). Type 1 diabetes is a heterogeneous disease
In this 'beta cell centric hypothesis', once the beta
cell is under attack, a cascade is set into motion, as Despite T1D always resulting in the same clinical
this inflammatory environment seems to result in the endpoint of insulin deficiency and requiring lifelong
release of additional pro-inflammatory cytokines and exogenous insulin substitution, it is actually a collective
chemokines by the beta cells, thus attracting more cells of term of a heterogeneous disease. Clinicians recognize this
the immune system (Cardozo et al. 2003). Interestingly, in heterogeneity, with some people being diagnosed early in
the presence of inflammation, beta cells overexpress HLA life, others late in life; some being isolated cases, others
class I molecules creating an additional homing beacon having a family history of T1D; some having T1D in the
for cytotoxic T cells (Richardson et al. 2016). Recently, it context of multiple autoimmune diseases, others having
has been shown that stressed beta cells not only misfold just T1D; some losing all C-peptide (reflecting functional
insulin, but also misprocess other proteins and peptides, beta cell mass) in a few months, while others preserving
leading to the formation of neo-antigens generating novel it life-long.
epitopes for the immune system. These neo-antigens can At present, over 60 loci are associated with an
even cause epitope spreading in the immune reaction, increased susceptibility to T1D, with the HLA region as a
as demonstrated by the presence of antibodies against major contributor (Bakay et al. 2019). The ever-expanding
these neo-epitopes in people with T1D (James et al. 2018). number of associated loci supports the heterogeneity of
Inflamed beta cells can furthermore release exosomes T1D with, as discussed above, some genes linked to beta
(containing, i.e. proinsulin, GAD65, and IA-2), which cell dysfunction and others to immune cell dysfunction.
also have the potential to trigger autoimmune responses The genetic complexity is illustrated by the fact that
(Cianciaruso et al. 2017). A final argument pointing to despite the 15-fold increase in the risk of T1D in individuals
the beta cell as the true culprit is the fact that current having a first-degree relative with T1D, the majority of
immunotherapies are able to only temporarily slow the new T1D diagnoses are made in individuals having no
decline in beta cell function, suggesting that residual known family history for T1D (Pociot & Lernmark 2016).
pathogenic mechanisms remain untargeted (Mallone & In addition, many people carrying the highest risk HLA
Eizirik 2020). haplotypes do not develop T1D (Skyler et al. 2017). These
Most probably the answer lays in the middle, data, together with the observation that the presentation
with T1D being the result of a complex network of of T1D is changing, with rapid increases in T1D numbers
dysfunctions both in the beta cell and the immune and a shift toward younger ages at disease diagnosis,
system, with defects in both innate and adaptive immune suggest the presence of external triggers that can differ
regulation, creating ‘the perfect storm’ (Peters et al. 2019). between different individuals. In an attempt to better
An example of how both sides of the story are connected understand the nature of these environmental triggers,
in T1D is demonstrated by genetic polymorphisms The Environmental Determinants of Diabetes in the Young
within a single locus encoding the transcription factor (TEDDY) study was initiated. This is a large prospective
basic leucine zipper transcription factor 2 (BACH2). cohort study in children – beginning at birth, with high-
https://joe.bioscientifica.com © 2021 Society for Endocrinology
https://doi.org/10.1530/JOE-20-0552 Published by Bioscientifica Ltd.
Printed in Great Britain
Downloaded from Bioscientifica.com at 01/03/2022 05:54:45PM
via free access
Journal of PJ Martens et al. Arresting or curing type 1 249:2 T4
Endocrinology diabetes
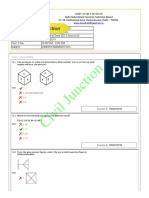
Figure 1
The vicious circle of dying beta cells in type 1 diabetes and therapeutic opportunities to interfere at different disease stages. In a genetically predisposed
individual, undefined factor(s) (depicted in orange) will trigger type 1 diabetes by the induction of beta cell stress, leading to compensatory responses
that ultimately are deleterious for the beta cells, and by activation of inappropriate immune responses toward the beta cells (stage 0). Once pancreatic
beta cells are failing, a vicious circle advances as a result of the release of (neo)antigens and cytokines/chemokines (stages 1–2), reinforcing the ongoing
autoimmune responses and contributing to (complete) destruction of functional pancreatic beta cells (stage 3). The constant interaction between beta
cells and immune system may vary in individuals at risk, leading to disease heterogeneity. As this destruction process is highly immunogenic, it is by itself
a trigger to reinitiate this cascade in adjoining (so far) healthy islets. This figure again emphasizes the need for the identification of robust and reliable
biomarkers (depicted in green) as their implementation would offer an opportunity to detect type 1 diabetes in early disease stages, resulting in a better
efficacy of therapeutics. Therapeutic approaches (depicted in purple) can be designed for each disease stage. As to date, none has shown prevention or
long-term disease reversal, indicating that lasting prevention and/or cure will depend on combination therapies. GAD, glutamic acid decarboxylase;
GADA, glutamic acid decarboxylase antibodies; IA-2A, tyrosine phosphatase-related islet antigen 2; IAA, insulin autoantibodies.
risk genotypes – aiming to identify environmental factors and TEDDY trials, have provided major insights into
that influence islet autoimmunity and T1D onset (TEDDY the meaning of antibody appearance in the evolution
Study Group 2008). Yet, despite all these efforts, predicting toward symptom onset. Mostly, T1D evolution starts with
T1D in a reliable way remains a challenge as a recent 8-year the appearance of one autoantibody. This is possible as
progress report showed that although risk factors can be early as 3 months of age, peaking at the age of 9 months
associated with islet autoimmunity and T1D, they are not (Krischer et al. 2015). IAA or GADA are most frequently
precise predictors (Krischer et al. 2019). the first autoantibodies, appearing a median period of
At present, the best predictor of progression toward 7 months before the second autoantibody. Yet, the rate
T1D in genetically predisposed individuals, but also in of progression is highly dependent on the hierarchy of
the general population, is the presence of autoantibodies antibody appearance (Vehik et al. 2020), with a consensus
(Primavera et al. 2020). An array of autoantibodies has that the positivity of two or more islet autoantibodies
been described, with heterogeneity in their appearance. confers a high risk of developing symptomatic T1D
Whereas in children insulin autoantibodies (IAA) are most (Insel et al. 2015). In longitudinal studies, only 15% of
prevalent, in adults GAD autoantibodies (GADA) are the children with one islet autoantibody developed T1D
most frequent ones. Again, heterogeneity exists, as the within 10 years, compared to 70% of those with at least
risk depends on antibody titer, affinity, immunoglobulin two islet autoantibodies (Ziegler et al. 2013). The 30%
subclasses and target epitopes on single or multiple of high-risk patients that do not progress to T1D within
islet autoantigens (Bonifacio & Achenbach 2019). 10 years are termed 'slow progressor' (Long et al. 2018).
Therefore, when using islet autoantibodies in the To complicate things even more, even reversion of islet
prediction of T1D onset, it is important to understand autoantibody positivity (seroconversion) is possible
their implication. Prospective birth-cohort studies in (Vehik et al. 2016). The islet autoantibodies epitomize the
high-risk children, including the BABYDIAB, DIPP, DAISY disease heterogeneity of T1D as according to which islet
https://joe.bioscientifica.com © 2021 Society for Endocrinology
https://doi.org/10.1530/JOE-20-0552 Published by Bioscientifica Ltd.
Printed in Great Britain Downloaded from Bioscientifica.com at 01/03/2022 05:54:45PM
via free access
Journal of PJ Martens et al. Arresting or curing type 1 249:2 T5
Endocrinology diabetes
autoantibody appears first and possibly even disappears; by the dazzling list of studies already performed in
the aggressiveness of the autoimmune response can be people with new-onset T1D or unaffected high-risk
predicted. Thus, although autoantibodies are at present family members. Large consortia have been established
the ‘best biomarker’, finding better biomarkers is a priority worldwide to perform multicenter trials. Examples are the
on the path to T1D prevention or cure (see below). Type 1 Diabetes TrialNet (an in 2001 established National
Heterogeneity also exists in the functional pancreatic Institutes of Health (NIH)-funded and Juvenile Diabetes
beta cell mass both at T1D onset and during disease Research Foundation (JDRF)-supported international
progression (Campbell-Thompson et al. 2016). A general clinical trial network that emerged from the Diabetes
observation is that children lose their functional beta Prevention Trial Type 1 (DPT-1)) and the more recent
cell mass, as measured by C-peptide, more rapidly than INNODIA consortium (a European partnership between
adults do. Some individuals with longstanding T1D academic institutions, industrial partners and patient
retain measurable levels of serum C-peptide and harbor organizations) (Mathieu 2018). Most interventions to
insulin-positive islets in their pancreas even decades after date have either targeted the immune system (by general
diagnosis (Keenan et al. 2010, Wasserfall et al. 2017). Some or specific immune suppression or modulation), or were
arguments exist to suggest that in some individuals beta based on strategies aimed at the induction of tolerance
cells can proliferate, be generated from ductal cells or toward proteins or peptides relevant to T1D.
transdifferentiate from other islet cells like alpha cells, but Non-antigen-specific immunotherapy, based on
no clear explanation is available for the heterogeneity of immunosuppression, is the oldest of these approaches.
beta cell mass (Saunders & Powers 2016, Lam et al. 2017). Cyclosporine A was the first drug to show the ability
Finally, also in the infiltration type around the beta to induce disease remission in people with new-onset
cells (i.e. insulitis) heterogeneity can be seen. Whereas T1D. However, it was also the first to expose the major
initiatives like nPOD show that most individuals with obstacles associated with this strategy, namely disease
T1D have only subtle infiltration, in contrast to the recurrence and adverse effects associated with systemic
observations on massive infiltration in the NOD mouse, immunosuppressive drugs (reviewed in Flores et al.
heterogeneity in the composition of the infiltrate has been 2019). A flurry of immune-modulatory agents has been
described (Atkinson et al. 2020). Recently, two distinct tested that allowed drawing important conclusions. As
profiles, according to the proportion of CD20+ B cells, such, it has become apparent that anti-inflammatory
were observed in the immune infiltrate, related to the age interventions, targeting single cytokines (like TNF-α
of the person and the rate of beta cell loss. The proportion or IL-1) are not successful in T1D (Donath et al. 2019).
of B cells in the immune infiltrate and the associated rate In a recent meta-analysis, it was demonstrated that of
of beta cell loss was higher in younger patients (diagnosed all interventions, two are by far the most successful in
before the age of 7 years) and lower in older patients preventing functional beta cell decline: anti-thymocyte
(diagnosed after the age of 13 years) (Leete et al. 2016). globulin (ATG) and teplizumab (anti-CD3 antibody)
The same pattern of two distinct profiles was also detected (Jacobsen et al. 2020).
in the peripheral blood as both pro-inflammatory (defined ATG is an old immune modulator widely used
by multi-autoantibody and interferon-(IFN)-γ positivity) in organ transplantation. However, the doses of ATG
and controlled (defined by pauci-autoantibody and that proved to be effective in delaying beta cell loss in
interleukin (IL)-10 positivity) responses were observed new-onset T1D patients were lower than those used
in newly diagnosed T1D patients (Arif et al. 2014). This for transplantation. Indeed, higher doses (6.5 mg/kg)
translates to younger patients having approximately were not effective in contrast to low doses (2.5 mg/kg)
10–15% of residual insulin-containing islets at the time (Gitelman et al. 2016, Haller et al. 2019). A possible
of T1D diagnosis to 40% in older patients (Leete et al. explanation for the protective effect of the low dose is
2016). Moreover, it implicates a significant role of beta that low doses cause a transient T cell depletion followed
cell dysfunction rather than death in these patients. by T cell reconstitution, resulting in a shift toward
tolerance induction as demonstrated by an increase in
Tregs (Lu et al. 2011).
Lessons learned from intervention studies Teplizumab fits in the concept of using more specific
anti-T cell antibodies in this T cell-mediated autoimmune
Why have we not cured T1D yet? Our plea starts by saying disease. First used in animals in 1988 and a first-in-
that we have not tried our very best. This is supported men trial (safety testing) already in 1989, the story of
https://joe.bioscientifica.com © 2021 Society for Endocrinology
https://doi.org/10.1530/JOE-20-0552 Published by Bioscientifica Ltd.
Printed in Great Britain
Downloaded from Bioscientifica.com at 01/03/2022 05:54:45PM
via free access
Journal of PJ Martens et al. Arresting or curing type 1 249:2 T6
Endocrinology diabetes
anti-CD3 monoclonal antibodies is a prime example of administered orally or GAD in aluminium hydroxide
the importance of choosing the correct study protocol (alum) administered subcutaneously (Beam et al. 2017).
and endpoints (reviewed in Chatenoud 2019). After all, it Despite the fact that none demonstrated convincingly
started as a success story showing complete and permanent beta cell protection, the major lesson learned from these
remission of T1D in animals. The initial clinical trials trials is that the antigen-specific interventions tested were
using humanized anti-CD3 monoclonal antibodies (i.e. safe (Roep et al. 2019). To obtain superior antigen-based
teplizumab or the aglycosylated otelixizumab) were tolerance induction, trials have been designed to combine
encouraging, showing preservation of beta cell function antigen therapy with low-grade immune modulation. For
(Herold et al. 2002, Keymeulen et al. 2005). Large phase proinsulin, based on successful animal trials (Takiishi
III trials for both should have been the icing on the et al. 2017, Cook et al. 2020), this is the ongoing study
cake, but failed. For otelixizumab, this was the DEFEND by Precigen ActoBio, combining teplizumab with AG019
trial and was unsuccessful most probably as a result of Actobiotics™, an oral capsule consisting of genetically
the decision to reduce the dose to 15 times less than engineered Lactococcus lactis, modified to deliver human
the one previously proven to be effective (Ambery et al. proinsulin together with the tolerance inducing cytokine
2014, Aronson et al. 2014). It was later suggested that the human IL-10 (clinical trial identifier: NCT03751007,
maximum target engagement was only achieved at a dose EudraCT 2017-002871-24).
6 times higher than the one used in the original DEFEND As GAD in alum administered subcutaneously did
trial, but it was the end of otelixizumab (Vlasakakis et al. not result in convincing results, this concept was revived
2019). The large phase III trial for teplizumab was the in the DIAGNODE-1 trial, designed to administer GAD
PROTÉGÉ trial and also failed. This time, the probable in alum into lymph nodes (a more targeted approach),
reason for failing was the study population and the choice but also in combination with vitamin D for low-grade
of the endpoint (insulin requirement) (Sherry et al. 2011). immunomodulation (Tavira et al. 2018). Based on
Later, the AbATE trial chose its endpoints more wisely relatively promising results, GAD in alum is now being
and was able to demonstrate that teplizumab preserved tested in combination with ibuprofen (DIABGAD;
C-peptide in people with new-onset T1D with even up clinical trial identifier: NCT01785108), etanercept
to 7 years after diagnosis a reduced decline in C-peptide (EDCR; clinical trial identifier: NCT02464033), or GABA
in responders (Hagopian et al. 2013, Perdigoto et al. (GABA/Diamyd; clinical trial identifier: NCT02002130)
2019). Predicting the response to teplizumab remains as anti-inflammatory component. To elucidate the
challenging and underlines the complexity of T1D and immunomodulatory role of vitamin D in DIAGNODE-1,
the need for biomarkers of therapeutic success. Still, the further research is ongoing (clinical trial identifier:
early start of therapy (at a moment when more beta cells NCT03345004).
are still present) positively impacted therapeutic response
(Herold et al. 2013). Furthermore, responders were shown
to express a class of partially exhausted T cells (defined by Road to a cure – need for biomarkers
the expression of EOMES and inhibitory factors like TIGIT
and KLRG1) (Long et al. 2017). The signs of exhaustion As the majority of pancreatic beta cell destruction happens
might serve as a signature of prevention of disease during the pre-symptomatic stage, this emphasizes that
deterioration. Moreover, the induction of exhaustion therapeutic approaches should preferentially start during
was also demonstrated to be a hallmark in distinguishing the pre-symptomatic period (Atkinson & Eisenbarth
slow and fast disease progressors (Wiedeman et al. 2020). 2001). To date, the standard biomarkers are genetic
Recently, aiming to preserve even more pancreatic markers and autoantibodies. Genetic biomarkers in T1D
beta cells, teplizumab was given to non-diabetic, high- are mainly based on HLA typing with the highest HLA-DR
risk relatives of people with T1D (defined by two or more and -DQ, that is HLA-DR3/4 and HLA-DQ8, genotypes
diabetes-related autoantibodies – stage 2) and this was present in 30–40% of T1D individuals, increasing
able to delay progression to symptom onset in T1D up to the risk over 10-fold compared to the background
3 years (Herold et al. 2019, Sims et al. 2020). population (present in 2–3%) (Mathieu et al. 2018).
The final goal in T1D is the re-establishment of antigen- Autoantibodies are, as described above, robust biomarkers
specific tolerance. Thus, many trials have been conducted only useful for discriminating T1D from other types of
in an attempt to introduce T1D-relevant antigens to induce diabetes and by itself predict an increased risk for T1D as
specific tolerance. Some of these trials have used insulin the significance of the presence of ICA is dependent on
https://joe.bioscientifica.com © 2021 Society for Endocrinology
https://doi.org/10.1530/JOE-20-0552 Published by Bioscientifica Ltd.
Printed in Great Britain Downloaded from Bioscientifica.com at 01/03/2022 05:54:45PM
via free access
Journal of PJ Martens et al. Arresting or curing type 1 249:2 T7
Endocrinology diabetes
the a priori probability of a true result (e.g. genetic high- design together with the long duration and large sample
risk individual) (Bonifacio & Achenbach 2019). size needed for robust clinical trial design. Here, adaptive
This highlights the need for true biomarkers in T1D trial designs on the backbone of a master protocol may
and makes it the major focus of research in INNODIA. be the answer. In INNODIA, a Master Protocol has been
Over 50 clinical centers in Europe, both pediatric and designed that will be the guide for all studies in INNODIA,
adult clinics, are collecting samples from new-onset T1D allowing comparison between studies and allowing
patients and from unaffected family members of people adaptive trial design (Dunger et al. 2020). As such, the
living with T1D. In a natural history study, spanning INNODIA Master Protocol uses the same inclusion criteria,
several years, modular interrogation platforms for analysis visit schedule, duration, sample collection for standardized
of cellular and molecular features of beta cell and immune efficacy and mechanistic studies throughout all studies.
cell biomarkers have been established. These include The inclusion/exclusion criteria can be adapted to the
proteomes, lipidomes, and metabolomes, as well as a full requirements of specific interventions, but the clinical
immunomes and RNA analyses. INNODIA is in the final and mechanistic evaluations remain largely unchanged,
stages of performing an integrated multi-omics natural providing the primary outcomes and the potential for
history study on samples of new-onset T1D individuals. a more detailed analysis of variability in intervention
Of importance, these biomarker analyses are also included response. Additional study visits and sample collection
in the clinical trials running in the INNODIA network, allow studies of toxicology and pharmacokinetic or
thus not only opening the path to biomarkers of disease, dynamic analyses. Appealing in T1D to drive progress
but also raising hope for the discovery of biomarkers of are adaptive trial design strategies such as dose finding,
therapeutic effect and success of interventions. dropping study arms, inclusion of additional treatments,
Based on the observations described above, suggesting options to share controls and potentially inclusion of data
a role in the pathogenesis of T1D for both the beta cells from the natural history studies.
and the immune system, interventions with the highest Trials should be conducted in the most relevant
probability of success should be based on combinations of populations: young adults, adolescents and in particular
interventions. The most straightforward is as previously children. We must admit that by drawing conclusions
described the combination of immune modulation with on interventions in adults, where the course of the
antigen-based tolerance induction. Other appealing disease is very different from that in children (see part on
combinations would be agents improving beta cell health heterogeneity), we may be missing some interventions that
together with immune modulators. As such, a recent could have worked in children. Thus, we, as researchers and
study combined liraglutide, a GLP-1 receptor agonist and clinicians, need to convince regulators and industry that
an antibody targeting the cytokine IL-21. Results were even early-phase trials should be conducted in children,
intriguing, with additive effects observed during therapy, of course, taking into account all possible safety measures.
but all effect was lost after stopping the agents (Von Finally, a robust definition of therapeutic success is
Herrath et al. 2020). needed. This definition may be different at different stages
To reduce inflammation at the onset, anti- of the disease: in people with just a genetic risk, success
inflammatory drugs may be added to the treatment could be the prevention of autoimmunity (defined by
regimens. A combination of abatacept and rituximab prevention of biomarker appearance, e.g. autoantibodies)
is currently being tested in T1D prevention (stage 2) whereas in people with new-onset T1D success could
(clinical trial identifier: NCT03929601, UC4DK117009), be prevention of decline in functional beta cell mass as
as both abatacept and rituximab were shown to slow the measured by stimulated C-peptide. In the latter group,
decline of beta cell function in new-onset T1D, driven by the presence of C-peptide is associated with fewer
an effect seen early after treatment initiation (Pescovitz complications in the long-term and a smoother glycemic
et al. 2009, Orban et al. 2011). However, not always control in the immediate term.
does a combination therapy result in a better efficacy as
demonstrated by the addition of pegylated granulocyte
colony-stimulating factor (GCSF) to low-dose ATG, which Conclusion
seemed to diminish the benefits provided by low-dose
ATG (Haller et al. 2019). Type 1 diabetes is one of the most common and severe
The Achilles heel in the design of novel studies is the chronic diseases in children, adolescents and young adults,
lack of strong animal models for T1D to guide clinical trial and in desperate need of disease-modifying therapy. For
https://joe.bioscientifica.com © 2021 Society for Endocrinology
https://doi.org/10.1530/JOE-20-0552 Published by Bioscientifica Ltd.
Printed in Great Britain
Downloaded from Bioscientifica.com at 01/03/2022 05:54:45PM
via free access
Journal of PJ Martens et al. Arresting or curing type 1 249:2 T8
Endocrinology diabetes
100 years now, the gold standard treatment consists of Atkinson MA, Bluestone JA, Eisenbarth GS, Hebrok M, Herold KC,
Accili D, Pietropaolo M, Arvan PR, Von Herrath M, Markel DS, et al.
lifelong insulin treatment with the aim to maintain a
2011 How does type 1 diabetes develop?: the notion of homicide
normal glucose homeostasis. The discovery of insulin was or beta-cell suicide revisited. Diabetes 60 1370–1379. (https://doi.
pioneering, transforming T1D from a quickly fatal disease org/10.2337/db10-1797)
Atkinson MA, Campbell-Thompson M, Kusmartseva I & Kaestner KH
to an incurable, chronic disease. However, as the majority
2020 Organisation of the human pancreas in health and in diabetes.
of T1D patients fail to reach recommended target HbA1c Diabetologia 63 1966–1973. (https://doi.org/10.1007/s00125-020-
levels, the burden of disease-associated complications 05203-7)
Bakay M, Pandey R, Grant SFA & Hakonarson H 2019 The genetic
remains important. This should stimulate the search for
contribution to type 1 diabetes. Current Diabetes Reports 19 116.
disease-modifying therapies. As this review describes, we (https://doi.org/10.1007/s11892-019-1235-1)
have already traveled a long way, but the road remains Beam CA, Maccallum C, Herold KC, Wherrett DK, Palmer J, Ludvigsson J
& Type 1 Diabetes TrialNet Study Group 2017 GAD vaccine reduces
long and full of obstacles, the most important being the
insulin loss in recently diagnosed type 1 diabetes: findings from
unidentified culprit of T1D (beta cell or immune system or a Bayesian meta-analysis. Diabetologia 60 43–49. (https://doi.
both). Moreover, even if we can identify the culprit, we still org/10.1007/s00125-016-4122-1)
Bonifacio E 2015 Predicting type 1 diabetes using biomarkers. Diabetes
need to discover the exact mechanism that sets everything
Care 38 989–996. (https://doi.org/10.2337/dc15-0101)
in motion. Nevertheless, progress in our understanding is Bonifacio E & Achenbach P 2019 Birth and coming of age of islet
made and results of clinical intervention trials are promising, autoantibodies. Clinical and Experimental Immunology 198 294–305.
(https://doi.org/10.1111/cei.13360)
showing a temporary deferral of disease onset or transient
Bottazzo GF 1986 Lawrence lecture. Death of a beta cell: homicide
preservation of functional beta cell mass (as defined by or suicide? Diabetic Medicine 3 119–130. (https://doi.
C-peptide) by several interventions. Temporary or transient org/10.1111/j.1464-5491.1986.tb00722.x)
Campbell-Thompson M, Fu A, Kaddis JS, Wasserfall C, Schatz DA,
mostly means a couple of months to even a couple of years,
Pugliese A & Atkinson MA 2016 Insulitis and beta-cell mass in the
but for now, to many people living with T1D these carefree natural history of type 1 diabetes. Diabetes 65 719–731. (https://doi.
couple of months to years already mean a lot. org/10.2337/db15-0779)
Campbell-Thompson ML, Filipp SL, Grajo JR, Nambam B, Beegle R,
Middlebrooks EH, Gurka MJ, Atkinson MA, Schatz DA & Haller MJ
2019 Relative pancreas volume is reduced in first-degree relatives of
Declaration of interest patients with type 1 diabetes. Diabetes Care 42 281–287. (https://doi.
The authors declare that there is no conflict of interest that could be org/10.2337/dc18-1512)
perceived as prejudicing the impartiality of this review. Cardozo AK, Proost P, Gysemans C, Chen MC, Mathieu C & Eizirik DL
2003 IL-1beta and IFN-gamma induce the expression of diverse
chemokines and IL-15 in human and rat pancreatic islet cells, and in
islets from pre-diabetic nod mice. Diabetologia 46 255–266. (https://
doi.org/10.1007/s00125-002-1017-0)
Funding Chatenoud L 2019 A future for CD3 antibodies in immunotherapy of
This work did not receive any specific grant from any funding agency in type 1 diabetes. Diabetologia 62 578–581. (https://doi.org/10.1007/
the public, commercial or non-profit sector that could be perceived as s00125-018-4808-7)
prejudicing the impartiality of the research reported. Cianciaruso C, Phelps EA, Pasquier M, Hamelin R, Demurtas D, Alibashe
Ahmed M, Piemonti L, Hirosue S, Swartz MA, De Palma M, et al.
2017 Primary human and rat beta-cells release the intracellular
autoantigens GAD65, IA-2, and proinsulin in exosomes together
with cytokine-induced enhancers of immunity. Diabetes 66 460–473.
References (https://doi.org/10.2337/db16-0671)
Ambery P, Donner TW, Biswas N, Donaldson J, Parkin J & Dayan CM Cook DP, Cunha JPMCM, Martens PJ, Sassi G, Mancarella F, Ventriglia G,
2014 Efficacy and safety of low-dose otelixizumab anti-CD3 Sebastiani G, Vanherwegen AS, Atkinson MA, Van Huynegem K, et al.
monoclonal antibody in preserving c-peptide secretion in adolescent 2020 Intestinal delivery of proinsulin and IL-10 via Lactococcus lactis
type 1 diabetes: defend-2, a randomized, placebo-controlled, double- combined with low-dose anti-CD3 restores tolerance outside the
blind, multi-centre study. Diabetic Medicine 31 399–402. (https://doi. window of acute type 1 diabetes diagnosis. Frontiers in Immunology 11
org/10.1111/dme.12361) 1103. (https://doi.org/10.3389/fimmu.2020.01103)
Arif S, Leete P, Nguyen V, Marks K, Nor NM, Estorninho M, Kronenberg- Culina S, Lalanne AI, Afonso G, Cerosaletti K, Pinto S, Sebastiani G,
Versteeg D, Bingley PJ, Todd JA, Guy C, et al. 2014 Blood and islet Kuranda K, Nigi L, Eugster A, Osterbye T, et al. 2018 Islet-reactive
phenotypes indicate immunological heterogeneity in type 1 diabetes. CD8(+) T cell frequencies in the pancreas, but not in blood,
Diabetes 63 3835–3845. (https://doi.org/10.2337/db14-0365) distinguish type 1 diabetic patients from healthy donors. Science
Aronson R, Gottlieb PA, Christiansen JS, Donner TW, Bosi E, Bode BW, Immunology 3 eaao4013. (https://doi.org/10.1126/sciimmunol.
Pozzilli P & DEFEND Investigator Group 2014 Low-dose otelixizumab aao4013)
anti-CD3 monoclonal antibody DEFEND-1 study: results of the Donath MY, Dinarello CA & Mandrup-Poulsen T 2019 Targeting innate
randomized phase III study in recent-onset human type 1 diabetes. immune mediators in type 1 and type 2 diabetes. Nature Reviews:
Diabetes Care 37 2746–2754. (https://doi.org/10.2337/dc13-0327) Immunology 19 734–746. (https://doi.org/10.1038/s41577-019-0213-9)
Atkinson MA & Eisenbarth GS 2001 Type 1 diabetes: new perspectives on Dunger DB, Bruggraber SF, Mander AP, Tree T, Jaroslaw Chmura P,
disease pathogenesis and treatment. Lancet 358 221–229. (https://doi. Knip MJ, Schulte AM & Mathieu C 2020 Innodia master protocol
org/10.1016/S0140-6736(01)05415-0) for the evaluation of investigational medicinal products in children,
https://joe.bioscientifica.com © 2021 Society for Endocrinology
https://doi.org/10.1530/JOE-20-0552 Published by Bioscientifica Ltd.
Printed in Great Britain Downloaded from Bioscientifica.com at 01/03/2022 05:54:45PM
via free access
Journal of PJ Martens et al. Arresting or curing type 1 249:2 T9
Endocrinology diabetes
adolescents and adults with newly diagnosed type 1 diabetes. In Paper recent-onset type 1 diabetes. Diabetes Technology and Therapeutics 22
presented at: European Association for the Study of Diabetes 56th Annual 948–953. (https://doi.org/10.1089/dia.2020.0305)
Meeting; 21–25 September 2020; Virtual. (available at: https://www. James EA, Pietropaolo M & Mamula MJ 2018 Immune recognition of
innodia.eu/downloads/pdf/2020-easd-overview.pdf) beta-cells: neoepitopes as key players in the loss of tolerance. Diabetes
Eisenbarth GS 1986 Type I diabetes mellitus. A chronic autoimmune 67 1035–1042. (https://doi.org/10.2337/dbi17-0030)
disease. New England Journal of Medicine 314 1360–1368. (https://doi. Keenan HA, Sun JK, Levine J, Doria A, Aiello LP, Eisenbarth G, Bonner-
org/10.1056/NEJM198605223142106) Weir S & King GL 2010 Residual insulin production and pancreatic
Eizirik DL, Miani M & Cardozo AK 2013 Signalling danger: endoplasmic ss-cell turnover after 50 years of diabetes: Joslin medalist study.
reticulum stress and the unfolded protein response in pancreatic islet Diabetes 59 2846–2853. (https://doi.org/10.2337/db10-0676)
inflammation. Diabetologia 56 234–241. (https://doi.org/10.1007/ Keymeulen B, Vandemeulebroucke E, Ziegler AG, Mathieu C, Kaufman L,
s00125-012-2762-3) Hale G, Gorus F, Goldman M, Walter M, Candon S, et al. 2005 Insulin
Engin F, Yermalovich A, Nguyen T, Hummasti S, Fu W, Eizirik DL, needs after CD3-antibody therapy in new-onset type 1 diabetes. New
Mathis D & Hotamisligil GS 2013 Restoration of the unfolded protein England Journal of Medicine 352 2598–2608. (https://doi.org/10.1056/
response in pancreatic beta cells protects mice against type 1 diabetes. NEJMoa043980)
Science Translational Medicine 5 211ra156. (https://doi.org/10.1126/ Kracht MJ, Van Lummel M, Nikolic T, Joosten AM, Laban S, Van Der
scitranslmed.3006534) Slik AR, Van Veelen PA, Carlotti F, De Koning EJ, Hoeben RC, et al.
Flores C, Fouquet G, Moura IC, Maciel TT & Hermine O 2019 Lessons to 2017 Autoimmunity against a defective ribosomal insulin gene
learn from low-dose cyclosporin-A: a new approach for unexpected product in type 1 diabetes. Nature Medicine 23 501–507. (https://doi.
clinical applications. Frontiers in Immunology 10 588. (https://doi. org/10.1038/nm.4289)
org/10.3389/fimmu.2019.00588) Krischer JP, Lynch KF, Schatz DA, Ilonen J, Lernmark Å, Hagopian WA,
Gitelman SE, Gottlieb PA, Felner EI, Willi SM, Fisher LK, Moran A, Rewers MJ, She JX, Simell OG, Toppari J, et al. 2015 The 6 year
Gottschalk M, Moore WV, Pinckney A, Keyes-Elstein L, et al. 2016 incidence of diabetes-associated autoantibodies in genetically at-risk
Antithymocyte globulin therapy for patients with recent-onset children: the teddy study. Diabetologia 58 980–987. (https://doi.
type 1 diabetes: 2 year results of a randomised trial. Diabetologia 59 org/10.1007/s00125-015-3514-y)
1153–1161. (https://doi.org/10.1007/s00125-016-3917-4) Krischer JP, Liu X, Vehik K, Akolkar B, Hagopian WA, Rewers MJ, She JX,
Hagopian W, Ferry Jr RJ, Sherry N, Carlin D, Bonvini E, Johnson S, Toppari J, Ziegler AG, Lernmark Å, et al. 2019 Predicting islet cell
Stein KE, Koenig S, Daifotis AG, Herold KC, et al. 2013 Teplizumab autoimmunity and type 1 diabetes: an 8-year teddy study progress
preserves c-peptide in recent-onset type 1 diabetes: two-year results report. Diabetes Care 42 1051–1060. (https://doi.org/10.2337/dc18-
from the randomized, placebo-controlled protege trial. Diabetes 62 2282)
3901–3908. (https://doi.org/10.2337/db13-0236) Lam CJ, Jacobson DR, Rankin MM, Cox AR & Kushner JA 2017 Beta
Haller MJ, Long SA, Blanchfield JL, Schatz DA, Skyler JS, Krischer JP, cells persist in T1D pancreata without evidence of ongoing beta-
Bundy BN, Geyer SM, Warnock MV, Miller JL, et al. 2019 Low-dose cell turnover or neogenesis. Journal of Clinical Endocrinology and
anti-thymocyte globulin preserves c-peptide, reduces HbA1c, and Metabolism 102 2647–2659. (https://doi.org/10.1210/jc.2016-3806)
increases regulatory to conventional T-cell ratios in new-onset type 1 Lampeter EF, Homberg M, Quabeck K, Schaefer UW, Wernet P,
diabetes: two-year clinical trial data. Diabetes 68 1267–1276. (https:// Bertrams J, Grosse-Wilde H, Gries FA & Kolb H 1993 Transfer of
doi.org/10.2337/db19-0057) insulin-dependent diabetes between hla-identical siblings by bone
Herold KC, Hagopian W, Auger JA, Poumian-Ruiz E, Taylor L, marrow transplantation. Lancet 341 1243–1244. (https://doi.
Donaldson D, Gitelman SE, Harlan DM, Xu D, Zivin RA, et al. org/10.1016/0140-6736(93)91148-f)
2002 Anti-CD3 monoclonal antibody in new-onset type 1 diabetes Leete P, Willcox A, Krogvold L, Dahl-Jorgensen K, Foulis AK,
mellitus. New England Journal of Medicine 346 1692–1698. (https://doi. Richardson SJ & Morgan NG 2016 Differential insulitic profiles
org/10.1056/NEJMoa012864) determine the extent of beta-cell destruction and the age at onset
Herold KC, Gitelman SE, Ehlers MR, Gottlieb PA, Greenbaum CJ, of type 1 diabetes. Diabetes 65 1362–1369. (https://doi.org/10.2337/
Hagopian W, Boyle KD, Keyes-Elstein L, Aggarwal S, Phippard D, db15-1615)
et al. 2013 Teplizumab (anti-CD3 mAb) treatment preserves c-peptide Long SA, Thorpe J, Herold KC, Ehlers M, Sanda S, Lim N,
responses in patients with new-onset type 1 diabetes in a randomized Linsley PS, Nepom GT & Harris KM 2017 Remodeling T cell
controlled trial: metabolic and immunologic features at baseline compartments during anti-CD3 immunotherapy of type 1
identify a subgroup of responders. Diabetes 62 3766–3774. (https:// diabetes. Cellular Immunology 319 3–9. (https://doi.org/10.1016/j.
doi.org/10.2337/db13-0345) cellimm.2017.07.007)
Herold KC, Bundy BN, Long SA, Bluestone JA, Dimeglio LA, Dufort MJ, Long AE, Wilson IV, Becker DJ, Libman IM, Arena VC, Wong FS,
Gitelman SE, Gottlieb PA, Krischer JP, Linsley PS, et al. 2019 An Steck AK, Rewers MJ, Yu L, Achenbach P, et al. 2018 Characteristics
anti-CD3 antibody, teplizumab, in relatives at risk for type 1 of slow progression to diabetes in multiple islet autoantibody-
diabetes. New England Journal of Medicine 381 603–613. (https://doi. positive individuals from five longitudinal cohorts: the snail study.
org/10.1056/NEJMoa1902226) Diabetologia 61 1484–1490. (https://doi.org/10.1007/s00125-018-
Holohan DR, Van Gool F & Bluestone JA 2019 Thymically-derived foxp3+ 4591-5)
regulatory T cells are the primary regulators of type 1 diabetes in the Lu Y, Suzuki J, Guillioli M, Umland O & Chen Z 2011 Induction of
non-obese diabetic mouse model. PLoS ONE 14 e0217728. (https:// self-antigen-specific FOXP3+ regulatory T cells in the periphery by
doi.org/10.1371/journal.pone.0217728) lymphodepletion treatment with anti-mouse thymocyte globulin
Insel RA, Dunne JL, Atkinson MA, Chiang JL, Dabelea D, Gottlieb PA, in mice. Immunology 134 50–59. (https://doi.org/10.1111/j.1365-
Greenbaum CJ, Herold KC, Krischer JP, Lernmark Å, et al. 2015 2567.2011.03466.x)
Staging presymptomatic type 1 diabetes: a scientific statement Mallone R & Eizirik DL 2020 Presumption of innocence for beta cells:
of JDRF, the Endocrine Society, and the American Diabetes why are they vulnerable autoimmune targets in type 1 diabetes?
Association. Diabetes Care 38 1964–1974. (https://doi.org/10.2337/ Diabetologia 63 1999–2006. (https://doi.org/10.1007/s00125-020-
dc15-1419) 05176-7)
Jacobsen LM, Bundy BN, Greco MN, Schatz DA, Atkinson MA, Marroqui L, Santin I, Dos Santos RS, Marselli L, Marchetti P & Eizirik DL
Brusko TM, Mathews CE, Herold KC, Gitelman SE, Krischer JP, 2014 BACH2, a candidate risk gene for type 1 diabetes, regulates
et al. 2020 Comparing beta cell preservation across clinical trials in apoptosis in pancreatic beta-cells via jnk1 modulation and crosstalk
https://joe.bioscientifica.com © 2021 Society for Endocrinology
https://doi.org/10.1530/JOE-20-0552 Published by Bioscientifica Ltd.
Printed in Great Britain
Downloaded from Bioscientifica.com at 01/03/2022 05:54:45PM
via free access
Journal of PJ Martens et al. Arresting or curing type 1 249:2 T10
Endocrinology diabetes
with the candidate gene PTPN2. Diabetes 63 2516–2527. (https://doi. beta-Cell-specific CD8 T cell phenotype in type 1 diabetes reflects
org/10.2337/db13-1443) chronic autoantigen exposure. Diabetes 64 916–925. (https://doi.
Mathieu C 2018 Are we there yet? Finding ways to work together on org/10.2337/db14-0332)
T1D. Diabetes Care 41 667–669. (https://doi.org/10.2337/dci17-0065) Skyler JS, Bakris GL, Bonifacio E, Darsow T, Eckel RH, Groop L,
Mathieu C, Lahesmaa R, Bonifacio E, Achenbach P & Tree T 2018 Groop PH, Handelsman Y, Insel RA, Mathieu C, et al. 2017
Immunological biomarkers for the development and progression of Differentiation of diabetes by pathophysiology, natural history, and
type 1 diabetes. Diabetologia 61 2252–2258. (https://doi.org/10.1007/ prognosis. Diabetes 66 241–255. (https://doi.org/10.2337/db16-0806)
s00125-018-4726-8) Takiishi T, Cook DP, Korf H, Sebastiani G, Mancarella F, Cunha JP,
Orban T, Bundy B, Becker DJ, Dimeglio LA, Gitelman SE, Goland R, Wasserfall C, Casares N, Lasarte JJ, Steidler L, et al. 2017 Reversal of
Gottlieb PA, Greenbaum CJ, Marks JB, Monzavi R, et al. 2011 diabetes in nod mice by clinical-grade proinsulin and IL-10-secreting
Co-stimulation modulation with abatacept in patients with Lactococcus lactis in combination with low-dose anti-CD3 depends
recent-onset type 1 diabetes: a randomised, double-blind, placebo- on the induction of FOXP3-positive T cells. Diabetes 66 448–459.
controlled trial. Lancet 378 412–419. (https://doi.org/10.1016/S0140- (https://doi.org/10.2337/db15-1625)
6736(11)60886-6) Tavira B, Barcenilla H, Wahlberg J, Achenbach P, Ludvigsson J & Casas R
Perdigoto AL, Preston-Hurlburt P, Clark P, Long SA, Linsley PS, 2018 Intralymphatic glutamic acid decarboxylase-alum administration
Harris KM, Gitelman SE, Greenbaum CJ, Gottlieb PA, Hagopian W, induced th2-like-specific immunomodulation in responder patients: a
et al. 2019 Treatment of type 1 diabetes with teplizumab: clinical pilot clinical trial in type 1 diabetes. Journal of Diabetes Research 2018
and immunological follow-up after 7 years from diagnosis. 9391845. (https://doi.org/10.1155/2018/9391845)
Diabetologia 62 655–664. (https://doi.org/10.1007/s00125-018- TEDDY Study Group 2008 The environmental determinants of diabetes
4786-9) in the young (teddy) study. Annals of the New York Academy of Sciences
Pescovitz MD, Greenbaum CJ, Krause-Steinrauf H, Becker DJ, 1150 1–13. (https://doi.org/10.1155/2018/9391845)
Gitelman SE, Goland R, Gottlieb PA, Marks JB, Mcgee PF, Moran AM, The Diabetes Control and Complications Trial Research Group 1998
et al. 2009 Rituximab, B-lymphocyte depletion, and preservation of Effect of intensive therapy on residual beta-cell function in patients
beta-cell function. New England Journal of Medicine 361 2143–2152. with type 1 diabetes in the diabetes control and complications trial. A
(https://doi.org/10.1056/NEJMoa0904452) randomized controlled tiral. Annals of Internal Medicine 128 517–523.
Peters L, Posgai A & Brusko TM 2019 Islet-immune interactions in type 1 (https://doi.org/10.7326/0003-4819-128-7-199804010-00001)
diabetes: the nexus of beta cell destruction. Clinical and Experimental Thomaidou S, Kracht MJL, Van Der Slik A, Laban S, De Koning EJ,
Immunology 198 326–340. (https://doi.org/10.1111/cei.13349) Carlotti F, Hoeben RC, Roep BO & Zaldumbide A 2020 beta-Cell stress
Pociot F & Lernmark Å 2016 Genetic risk factors for type 1 diabetes. shapes ctl immune recognition of preproinsulin signal peptide by
Lancet 387 2331–2339. (https://doi.org/10.1016/S0140- posttranscriptional regulation of endoplasmic reticulum aminopeptidase.
6736(16)30582-7) Diabetes 69 670–680. (https://doi.org/10.2337/db19-0984)
Primavera M, Giannini C & Chiarelli F 2020 Prediction and prevention Vaitaitis GM, Waid DM, Yussman MG & Wagner Jr DH 2017 CD40-
of type 1 diabetes. Frontiers in Endocrinology 11 248. (https://doi. mediated signalling influences trafficking, T-cell receptor expression,
org/10.3389/fendo.2020.00248) and T-cell pathogenesis, in the NOD model of type 1 diabetes.
Richardson SJ, Rodriguez-Calvo T, Gerling IC, Mathews CE, Kaddis JS, Immunology 152 243–254. (https://doi.org/10.1111/imm.12761)
Russell MA, Zeissler M, Leete P, Krogvold L, Dahl-Jorgensen K, et al. Vehik K, Lynch KF, Schatz DA, Akolkar B, Hagopian W, Rewers M, She JX,
2016 Islet cell hyperexpression of hla class I antigens: a defining Simell O, Toppari J, Ziegler AG, et al. 2016 Reversion of beta-cell
feature in type 1 diabetes. Diabetologia 59 2448–2458. (https://doi. autoimmunity changes risk of type 1 diabetes: TEDDY study. Diabetes
org/10.1007/s00125-016-4067-4) Care 39 1535–1542. (https://doi.org/10.2337/dc16-0181)
Rodriguez-Calvo T, Zapardiel-Gonzalo J, Amirian N, Castillo E, Vehik K, Bonifacio E, Lernmark Å, Yu L, Williams A, Schatz D, Rewers M,
Lajevardi Y, Krogvold L, Dahl-Jorgensen K & Von Herrath MG 2017 She JX, Toppari J, Hagopian W, et al. 2020 Hierarchical order of
Increase in pancreatic proinsulin and preservation of beta-cell mass in distinct autoantibody spreading and progression to type 1 diabetes
autoantibody-positive donors prior to type 1 diabetes onset. Diabetes in the TEDDY study. Diabetes Care 43 2066–2073. (https://doi.
66 1334–1345. (https://doi.org/10.2337/db16-1343) org/10.2337/dc19-2547)
Roep BO, Wheeler DCS & Peakman M 2019 Antigen-based immune Virostko J, Williams J, Hilmes M, Bowman C, Wright JJ, Du L, Kang H,
modulation therapy for type 1 diabetes: the era of precision medicine. Russell WE, Powers AC & Moore DJ 2019 Pancreas volume declines
Lancet: Diabetes and Endocrinology 7 65–74. (https://doi.org/10.1016/ during the first year after diagnosis of type 1 diabetes and exhibits
S2213-8587(18)30109-8) altered diffusion at disease onset. Diabetes Care 42 248–257. (https://
Roychoudhuri R, Hirahara K, Mousavi K, Clever D, Klebanoff CA, doi.org/10.2337/dc18-1507)
Bonelli M, Sciume G, Zare H, Vahedi G, Dema B, et al. 2013 BACH2 Vlasakakis G, Napolitano A, Barnard R, Brown K, Bullman J, Inman D,
represses effector programs to stabilize t(reg)-mediated immune Keymeulen B, Lanham D, Leirens Q, Macdonald A, et al. 2019 Target
homeostasis. Nature 498 506–510. (https://doi.org/10.1038/ engagement and cellular fate of otelixizumab: a repeat dose escalation
nature12199) study of an anti-CD3epsilon mab in new-onset type 1 diabetes
Saunders D & Powers AC 2016 Replicative capacity of beta-cells and mellitus patients. British Journal of Clinical Pharmacology 85 704–714.
type 1 diabetes. Journal of Autoimmunity 71 59–68. (https://doi. (https://doi.org/10.1111/bcp.13842)
org/10.1016/j.jaut.2016.03.014) Von Herrath MG, Bain SC, Bode BW, Clausen JO, Coppieters K,
Sherry N, Hagopian W, Ludvigsson J, Jain SM, Wahlen J, Ferry Jr RJ, Gaysina L, Gumprecht J, Hansen TK, Mathieu C, Portillo CM,
Bode B, Aronoff S, Holland C, Carlin D, et al. 2011 Teplizumab for et al. 2020 278-or: efficacy and safety of anti-interleukin (IL)-21 in
treatment of type 1 diabetes (Protégé study): 1-year results from a combination with liraglutide in adults recently diagnosed with type 1
randomised, placebo-controlled trial. Lancet 378 487–497. (https:// diabetes. Diabetes 69 278-OR. (https://doi.org/10.2337/db20-278-OR)
doi.org/10.1016/S0140-6736(11)60931-8) Wagner DH 2016 Of the multiple mechanisms leading to type 1 diabetes,
Sims EK, Bundy BN, Stier KD, Serti E, Lim N, Nepom GT, Evans-Molina C T cell receptor revision may play a prominent role (is type 1 diabetes
& Herold KC 2020 277-or: teplizumab reverses the loss of c-peptide in more than a single disease?). Clinical and Experimental Immunology
relatives at risk for type 1 diabetes. Diabetes 69 277-OR. 185 271–280. (https://doi.org/10.1111/cei.12819)
Skowera A, Ladell K, Mclaren JE, Dolton G, Matthews KK, Gostick E, Wasserfall C, Nick HS, Campbell-Thompson M, Beachy D, Haataja L,
Kronenberg-Versteeg D, Eichmann M, Knight RR, Heck S, et al. 2015 Kusmartseva I, Posgai A, Beery M, Rhodes C, Bonifacio E, et al.
https://joe.bioscientifica.com © 2021 Society for Endocrinology
https://doi.org/10.1530/JOE-20-0552 Published by Bioscientifica Ltd.
Printed in Great Britain Downloaded from Bioscientifica.com at 01/03/2022 05:54:45PM
via free access
Journal of PJ Martens et al. Arresting or curing type 1 249:2 T11
Endocrinology diabetes
2017 Persistence of pancreatic insulin mrna expression diabetes progression. Journal of Clinical Investigation 130 480–490.
and proinsulin protein in type 1 diabetes pancreata. Cell (https://doi.org/10.1172/JCI126595)
Metabolism 26 568.e3–575.e3. (https://doi.org/10.1016/j. Ziegler AG, Rewers M, Simell O, Simell T, Lempainen J, Steck A,
cmet.2017.08.013) Winkler C, Ilonen J, Veijola R, Knip M, et al. 2013 Seroconversion
Wiedeman AE, Muir VS, Rosasco MG, Deberg HA, Presnell S, Haas B, to multiple islet autoantibodies and risk of progression to diabetes
Dufort MJ, Speake C, Greenbaum CJ, Serti E, et al. 2020 Autoreactive in children. JAMA 309 2473–2479. (https://doi.org/10.1001/
CD8+ T cell exhaustion distinguishes subjects with slow type 1 jama.2013.6285)
Received in final form 12 November 2020
Accepted 9 March 2021
Accepted Manuscript published online 16 March 2021
https://joe.bioscientifica.com © 2021 Society for Endocrinology
https://doi.org/10.1530/JOE-20-0552 Published by Bioscientifica Ltd.
Printed in Great Britain
Downloaded from Bioscientifica.com at 01/03/2022 05:54:45PM
via free access
You might also like
- Complementary and Alternative Medical Lab Testing Part 14: ImmunologyFrom EverandComplementary and Alternative Medical Lab Testing Part 14: ImmunologyNo ratings yet
- Insulitis en La DMT1Document6 pagesInsulitis en La DMT1Psico AstralNo ratings yet
- Cellular and Molecular Pathophysiology of Type 1 Diabetes MellitusDocument8 pagesCellular and Molecular Pathophysiology of Type 1 Diabetes Mellitussofia.rvvvNo ratings yet
- Hdac Inhibition As A Novel Treatment For Diabetes MellitusDocument14 pagesHdac Inhibition As A Novel Treatment For Diabetes MellitusgreatmaleksNo ratings yet
- Reviews: Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failureDocument14 pagesReviews: Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failureJESSICA CELESTE LUNA PEÑANo ratings yet
- Reviews: Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failureDocument14 pagesReviews: Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failureMónika MikeNo ratings yet
- Fimmu 09 01086Document6 pagesFimmu 09 01086leorocha06No ratings yet
- 01.A model for type I diabetes in an HIV-infected patient under highlyactive antir...Document16 pages01.A model for type I diabetes in an HIV-infected patient under highlyactive antir...AidNo ratings yet
- Type 1 Diabetes A Chronic Anti-Self-Inflammatory ResponseDocument10 pagesType 1 Diabetes A Chronic Anti-Self-Inflammatory ResponseIda YulianaNo ratings yet
- Autoimmune Disorders Associated To Type 1Document10 pagesAutoimmune Disorders Associated To Type 1Ina SimacheNo ratings yet
- 6Document12 pages6KIU PUBLICATION AND EXTENSIONNo ratings yet
- 1 s2.0 S221287782200134X MainDocument18 pages1 s2.0 S221287782200134X MainErika WulandariNo ratings yet
- GWAS Data Analysis of Type 1 Diabetes Using Pathway and Network ApproachesDocument38 pagesGWAS Data Analysis of Type 1 Diabetes Using Pathway and Network ApproachesathayafebNo ratings yet
- Denyer 2021Document9 pagesDenyer 2021marparolaNo ratings yet
- Inflammageing and MetaflammationDocument17 pagesInflammageing and MetaflammationJosé GaldamesNo ratings yet
- NOD Transfection Protocol PDFDocument13 pagesNOD Transfection Protocol PDF이원빈No ratings yet
- Taking A Daily Vitamin To Prevent Type 1 Diabetes?: Clive Wasserfall and Mark A. AtkinsonDocument2 pagesTaking A Daily Vitamin To Prevent Type 1 Diabetes?: Clive Wasserfall and Mark A. AtkinsonHamdyGhazallyNo ratings yet
- T Cell ApoptosisDocument9 pagesT Cell ApoptosisVidho RiveraNo ratings yet
- Molecular and Cellular Mechanism of Cholera and Pertussis ToxinDocument10 pagesMolecular and Cellular Mechanism of Cholera and Pertussis ToxinSreedevi NandakumarNo ratings yet
- Adipose Tissue, Inlammation (Meta-Inlammation) and Obesity ManagementDocument18 pagesAdipose Tissue, Inlammation (Meta-Inlammation) and Obesity ManagementHelena FabianiNo ratings yet
- Immune Response After Autologous Hematopoietic Stem Cell Transplantation in Type 1 Diabetes MellitusDocument10 pagesImmune Response After Autologous Hematopoietic Stem Cell Transplantation in Type 1 Diabetes Mellitusaini nazilaNo ratings yet
- Immune Mechanisms in Type 1 Diabetes: Maja Wa Llberg and Anne CookeDocument9 pagesImmune Mechanisms in Type 1 Diabetes: Maja Wa Llberg and Anne CookeJosé Fernández MejíaNo ratings yet
- 19Document17 pages19KIU PUBLICATION AND EXTENSIONNo ratings yet
- Type 1 Diabetes Mellitus POSTERDocument1 pageType 1 Diabetes Mellitus POSTERLeandro FigueiraNo ratings yet
- Hope Injections: The Promises of Regenerative Medicine in Curing Type 1 Diabetes MellitusDocument6 pagesHope Injections: The Promises of Regenerative Medicine in Curing Type 1 Diabetes Mellitusfernando arriolaNo ratings yet
- Anti-IL-21 Monoclonal Antibody Combined With Liraglutide Effectively Reverses Established Hyperglycemia in Mouse Models of Type 1 Diabetes.Document10 pagesAnti-IL-21 Monoclonal Antibody Combined With Liraglutide Effectively Reverses Established Hyperglycemia in Mouse Models of Type 1 Diabetes.rafaelpires85No ratings yet
- 1-s2.0-S2376060523001700-mainDocument3 pages1-s2.0-S2376060523001700-mainValentinaNo ratings yet
- Functional Foods Modulating Inflammation and Metabolism in Chronic Diseases A Systematic Review, 2022Document23 pagesFunctional Foods Modulating Inflammation and Metabolism in Chronic Diseases A Systematic Review, 2022JessNo ratings yet
- International Journal of Health Sciences and Research: Immune Dysfunction in Diabetes Mellitus (DM)Document20 pagesInternational Journal of Health Sciences and Research: Immune Dysfunction in Diabetes Mellitus (DM)Elis FatmayantiNo ratings yet
- Type 1 Diabetes: Basis of Causes and Away of PreventionDocument11 pagesType 1 Diabetes: Basis of Causes and Away of PreventionOpenaccess Research paperNo ratings yet
- Immunoinformatics in DiabetesDocument8 pagesImmunoinformatics in DiabetesMio CaguiclaNo ratings yet
- Jurnal Internasional 8Document6 pagesJurnal Internasional 8Mutiara Anak NegeriNo ratings yet
- IAPP and Type 1 Diabetes: Implications For Immunity, Metabolism and Islet TransplantsDocument19 pagesIAPP and Type 1 Diabetes: Implications For Immunity, Metabolism and Islet TransplantsRoberto GómezNo ratings yet
- Cell DiabetesDocument8 pagesCell DiabetesSusana Calderón ToledoNo ratings yet
- JDRF Progress Report December 2011 FinalDocument9 pagesJDRF Progress Report December 2011 Finalapi-22735876No ratings yet
- Cellular Immunology of Type 1 DiabetesDocument10 pagesCellular Immunology of Type 1 DiabetesNiko Hizkia SimatupangNo ratings yet
- Prevalence of ZnT8 Antibody in Turkish Children and AdolescentsDocument5 pagesPrevalence of ZnT8 Antibody in Turkish Children and AdolescentsFairuza NafilahNo ratings yet
- NIH Public Access: Author ManuscriptDocument17 pagesNIH Public Access: Author ManuscriptFeli FelNo ratings yet
- John P. Williams, MD, MBA Jonathan A. Meyers, FSA, MAAA: (Am J Manag Care. 2002 8:S664-S681)Document18 pagesJohn P. Williams, MD, MBA Jonathan A. Meyers, FSA, MAAA: (Am J Manag Care. 2002 8:S664-S681)wdmukaNo ratings yet
- An Update On Diabetes Mellitus: June 2018Document12 pagesAn Update On Diabetes Mellitus: June 2018Siti AnisaNo ratings yet
- Clinical and Experimental Treatment of Type 1 Diabetes - Clin&ExpImmunol 210 (2) November 2022, pp105-113Document9 pagesClinical and Experimental Treatment of Type 1 Diabetes - Clin&ExpImmunol 210 (2) November 2022, pp105-113mapache0705No ratings yet
- Zhang 2017Document25 pagesZhang 2017hayNo ratings yet
- Current and Future Therapies For Type 1 Diabetes: Diabetologia (2021) 64:1037-1048Document12 pagesCurrent and Future Therapies For Type 1 Diabetes: Diabetologia (2021) 64:1037-1048Mauricio VidalNo ratings yet
- DTSCH Arztebl Int-118 0680bDocument3 pagesDTSCH Arztebl Int-118 0680bkeisy MarquezNo ratings yet
- Artículo 2 InmunoDocument20 pagesArtículo 2 InmunoEmmanuel UriosoNo ratings yet
- Models of T1DDocument5 pagesModels of T1DMiguel Angel Barajas VelezNo ratings yet
- Immune mechanisms and environmental factors in type 1 diabetesDocument9 pagesImmune mechanisms and environmental factors in type 1 diabetesNiko Hizkia SimatupangNo ratings yet
- The Role of Reactive Oxygen Species and Proinflammatory Cytokines in Type 1 Diabetes PathogenesisDocument20 pagesThe Role of Reactive Oxygen Species and Proinflammatory Cytokines in Type 1 Diabetes PathogenesisGuido BoggiNo ratings yet
- Cells 10 02681 v2Document14 pagesCells 10 02681 v2LýDiệuNo ratings yet
- New-Onset Diabetes in Covid-19: Eloise Baudou, M.D. Anne Lespine, PH.DDocument3 pagesNew-Onset Diabetes in Covid-19: Eloise Baudou, M.D. Anne Lespine, PH.DMaya Indri LaraswatiNo ratings yet
- Examination of The TIGIT, CD226, CD112, and CD155 ImmuneDocument15 pagesExamination of The TIGIT, CD226, CD112, and CD155 ImmuneNurul HidayahNo ratings yet
- Review Article: Biomarkers For Type 1 DiabetesDocument19 pagesReview Article: Biomarkers For Type 1 Diabetessalman672003No ratings yet
- Inflammatorybowel Disease: Anne Walsh,, John Mabee,, Kashyap TrivediDocument18 pagesInflammatorybowel Disease: Anne Walsh,, John Mabee,, Kashyap Trivediangeldavid26No ratings yet
- Terapias Emergentes en Artritis Reumatoide: Emergent Therapies For Rheumatoid ArthritisDocument8 pagesTerapias Emergentes en Artritis Reumatoide: Emergent Therapies For Rheumatoid ArthritisVALDE86No ratings yet
- Reading 10Document20 pagesReading 10Loredana DobreaNo ratings yet
- Novel Avenues of Drug Discovery and BiomarkersDocument39 pagesNovel Avenues of Drug Discovery and BiomarkersTakdirtahirNo ratings yet
- GH 12 572Document3 pagesGH 12 572Ahmad JunaediNo ratings yet
- InTech-Animal Models For Study of Diabetes Mellitus PDFDocument26 pagesInTech-Animal Models For Study of Diabetes Mellitus PDFArinda Rani AstutiNo ratings yet
- Is There Any Difference in Tetanus IgG Levels of Diabetic Patients With Respect To The Presence of Foot Ulcers - (#576028) - 733396Document6 pagesIs There Any Difference in Tetanus IgG Levels of Diabetic Patients With Respect To The Presence of Foot Ulcers - (#576028) - 733396ZainNo ratings yet
- NaviauxHealingCycle 2018 v2Document20 pagesNaviauxHealingCycle 2018 v2I JohanssonNo ratings yet
- Diabetes Pregestacional ACOGDocument21 pagesDiabetes Pregestacional ACOGarturoNo ratings yet
- Diabetes Mellitus Screaning and DiagnosisDocument7 pagesDiabetes Mellitus Screaning and DiagnosisMcd Svd FabricioNo ratings yet
- Pathophysiology of Type 1 Diabetes MellitusDocument13 pagesPathophysiology of Type 1 Diabetes MellitusPelle MozzaNo ratings yet
- Special Course: Team-Based Learning: Today's Clinical Case 1: Type I Diabetes MellitusDocument3 pagesSpecial Course: Team-Based Learning: Today's Clinical Case 1: Type I Diabetes MellitusAnanda DitaNo ratings yet
- E12 0330Document8 pagesE12 0330Khanh Trung VuNo ratings yet
- Diabetes in Pregnancy: A Guide to ManagementDocument11 pagesDiabetes in Pregnancy: A Guide to ManagementAlana CaballeroNo ratings yet
- Module 8 Assessment and Management of Patients With DiabetesDocument44 pagesModule 8 Assessment and Management of Patients With DiabetesBlessed GarcianoNo ratings yet
- Fphar 12 807548Document16 pagesFphar 12 807548Aurora Putri LatifahNo ratings yet
- Case Study!!!Document12 pagesCase Study!!!kaitlynne lambertNo ratings yet
- Association Between Breastfeeding Patterns and Type 1 Diabetes Among ChildrenDocument6 pagesAssociation Between Breastfeeding Patterns and Type 1 Diabetes Among ChildrenHarun joel tatipataNo ratings yet
- Endocrinology QuestionsDocument3 pagesEndocrinology Questionstoby hojojhNo ratings yet
- Diabetes Mellitus SeminarDocument35 pagesDiabetes Mellitus SeminarAnkush SinglaNo ratings yet
- Clinical Case Studies DiabetesDocument8 pagesClinical Case Studies Diabetesapi-434982019No ratings yet
- Hyper - and HypoglycemiaDocument3 pagesHyper - and HypoglycemiaaerugiNo ratings yet
- Diabetes Cheat Sheet Copyright BNDocument2 pagesDiabetes Cheat Sheet Copyright BNJeshan Yanong BeltranNo ratings yet
- Journal of Ethnopharmacology PDFDocument68 pagesJournal of Ethnopharmacology PDFAdyBorsosNo ratings yet
- Insulin Glargine 300 Vs 100 IU - INSTRIDE 1 - 2 StudiesDocument31 pagesInsulin Glargine 300 Vs 100 IU - INSTRIDE 1 - 2 StudiesSiddiq MohammedNo ratings yet
- Unit III. Yoga As Preventive Measure For Lifestyle Disease - Class-12Document37 pagesUnit III. Yoga As Preventive Measure For Lifestyle Disease - Class-12hhh klpNo ratings yet
- Diabetes and MassageDocument23 pagesDiabetes and MassagemassagekevinNo ratings yet
- Diabetes ManagementDocument11 pagesDiabetes ManagementNirav SharmaNo ratings yet
- Nutrients: Vitamin D Deficiency in India: Prevalence, Causalities and InterventionsDocument47 pagesNutrients: Vitamin D Deficiency in India: Prevalence, Causalities and Interventionssuheena.CNo ratings yet
- Coping With Chronic Illness in Childhood and AdoleDocument28 pagesCoping With Chronic Illness in Childhood and AdoleJOSE AYALANo ratings yet
- Dolfi Herscovici, Jr. (Eds.) - The Surgical Management of The Diabetic Foot and Ankle (2016, Springer International Publishing)Document204 pagesDolfi Herscovici, Jr. (Eds.) - The Surgical Management of The Diabetic Foot and Ankle (2016, Springer International Publishing)Pranitha PaidiNo ratings yet
- JBDS Diabetes at The Front Door Updated September 2021Document26 pagesJBDS Diabetes at The Front Door Updated September 2021jihanNo ratings yet
- National Guideline On Diabetes Mellitus, First Edition 2023Document116 pagesNational Guideline On Diabetes Mellitus, First Edition 2023Zohra AfrozNo ratings yet
- The Artificial Pancreas How Will This Benefit Patiens With DIabetesDocument3 pagesThe Artificial Pancreas How Will This Benefit Patiens With DIabetesRebeca UrseNo ratings yet
- Take One Nursing Final Coaching Ms CriticalDocument29 pagesTake One Nursing Final Coaching Ms Criticalnot your medz duranNo ratings yet
- Diabetes Mellitus Type 2Document16 pagesDiabetes Mellitus Type 2MTs MIFDANo ratings yet
- Endo Test Bank 1Document6 pagesEndo Test Bank 1mildred alidon100% (1)
- DSSSB Je Ae Civil All 22 PapersDocument980 pagesDSSSB Je Ae Civil All 22 Papersatul meenaNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionFrom EverandThe Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionRating: 4 out of 5 stars4/5 (811)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Tales from Both Sides of the Brain: A Life in NeuroscienceFrom EverandTales from Both Sides of the Brain: A Life in NeuroscienceRating: 3 out of 5 stars3/5 (18)
- All That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesFrom EverandAll That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesRating: 4.5 out of 5 stars4.5/5 (397)
- Crypt: Life, Death and Disease in the Middle Ages and BeyondFrom EverandCrypt: Life, Death and Disease in the Middle Ages and BeyondRating: 4 out of 5 stars4/5 (3)
- The Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindFrom EverandThe Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindRating: 4.5 out of 5 stars4.5/5 (93)
- Good Without God: What a Billion Nonreligious People Do BelieveFrom EverandGood Without God: What a Billion Nonreligious People Do BelieveRating: 4 out of 5 stars4/5 (66)
- This Is Your Brain On Parasites: How Tiny Creatures Manipulate Our Behavior and Shape SocietyFrom EverandThis Is Your Brain On Parasites: How Tiny Creatures Manipulate Our Behavior and Shape SocietyRating: 3.5 out of 5 stars3.5/5 (31)
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessFrom Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessRating: 4 out of 5 stars4/5 (33)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsFrom EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsRating: 4.5 out of 5 stars4.5/5 (4)
- Who's in Charge?: Free Will and the Science of the BrainFrom EverandWho's in Charge?: Free Will and the Science of the BrainRating: 4 out of 5 stars4/5 (65)
- The Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorFrom EverandThe Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorNo ratings yet
- The Lives of Bees: The Untold Story of the Honey Bee in the WildFrom EverandThe Lives of Bees: The Untold Story of the Honey Bee in the WildRating: 4.5 out of 5 stars4.5/5 (44)
- Undeniable: How Biology Confirms Our Intuition That Life Is DesignedFrom EverandUndeniable: How Biology Confirms Our Intuition That Life Is DesignedRating: 4 out of 5 stars4/5 (11)
- Human: The Science Behind What Makes Your Brain UniqueFrom EverandHuman: The Science Behind What Makes Your Brain UniqueRating: 3.5 out of 5 stars3.5/5 (38)
- Wayfinding: The Science and Mystery of How Humans Navigate the WorldFrom EverandWayfinding: The Science and Mystery of How Humans Navigate the WorldRating: 4.5 out of 5 stars4.5/5 (18)
- The Second Brain: A Groundbreaking New Understanding of Nervous Disorders of the Stomach and IntestineFrom EverandThe Second Brain: A Groundbreaking New Understanding of Nervous Disorders of the Stomach and IntestineRating: 4 out of 5 stars4/5 (17)
- Superlative: The Biology of ExtremesFrom EverandSuperlative: The Biology of ExtremesRating: 4.5 out of 5 stars4.5/5 (51)
- Buddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomFrom EverandBuddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomRating: 4 out of 5 stars4/5 (215)
- Eels: An Exploration, from New Zealand to the Sargasso, of the World's Most Mysterious FishFrom EverandEels: An Exploration, from New Zealand to the Sargasso, of the World's Most Mysterious FishRating: 4 out of 5 stars4/5 (30)
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceFrom EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceRating: 4.5 out of 5 stars4.5/5 (515)
- Human Errors: A Panorama of Our Glitches, from Pointless Bones to Broken GenesFrom EverandHuman Errors: A Panorama of Our Glitches, from Pointless Bones to Broken GenesRating: 3.5 out of 5 stars3.5/5 (56)
- Darwin's Dangerous Idea: Evolution and the Meaning of LifeFrom EverandDarwin's Dangerous Idea: Evolution and the Meaning of LifeRating: 4 out of 5 stars4/5 (523)
- The Mind & The Brain: Neuroplasticity and the Power of Mental ForceFrom EverandThe Mind & The Brain: Neuroplasticity and the Power of Mental ForceNo ratings yet
- The Dragons of Eden: Speculations on the Evolution of Human IntelligenceFrom EverandThe Dragons of Eden: Speculations on the Evolution of Human IntelligenceRating: 4 out of 5 stars4/5 (632)