Professional Documents
Culture Documents
The Concept of Mental Pain: Editorial
Uploaded by
Philip SpurrellOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Concept of Mental Pain: Editorial
Uploaded by
Philip SpurrellCopyright:
Available Formats
Editorial
Psychother Psychosom 2013;82:67–73 Received: April 18, 2012
Accepted after revision: August 26, 2012
DOI: 10.1159/000343003
Published online: December 22, 2012
The Concept of Mental Pain
Eliana Tossani
Laboratory of Psychosomatics and Clinimetrics, Department of Psychology, University of Bologna, Bologna, Italy
Mental pain is no less real than other types of pain re- inadequacy. When negative outcomes fall far below one’s
lated to parts of the body, but does not seem to get ade- standards of the ideal self and aspirations, and outcomes
quate attention. A major problem is the lack of agreement are attributed to the self, that person experiences mental
about its distinctive features, conceptualization and op- pain. The basic emotion in mental pain is, thus, self-dis-
erational definition. I will examine some suggested de- appointment.
scriptions of mental pain, its association with psychiatric Shneidman [5] defined psychache as an acute state of
disorders and grief, its assessment and the implications intense psychological pain associated with feelings of
that research in this field may entail. guilt, anguish, fear, panic, angst, loneliness and helpless-
ness. The primary source of severe psychache ‘is frus-
trated psychological needs’ [6]. Psychache is the mental
Definition of Mental Pain pain of being perturbed [7]. Perturbation refers to one’s
inner turmoil, or being upset or mentally disturbed [7].
In the literature, terms such as mental pain, psychic Bolger [8] defined emotional pain as a state of ‘feeling
pain, psychological pain, emptiness, psychache, internal broken’ that involved the experience of being wounded,
perturbation, and psychological quality of life have been loss of self, disconnection, and critical awareness of one’s
used to refer to the same construct. more negative attributes.
Bakan [1] observed that the individual feels psycho- Essential characteristics of emotional pain were de-
logical pain at the moment when he/she becomes sepa- scribed as a sense of loss or incompleteness of self and an
rated from a significant other. From his perspective, pain awareness of one’s own role in the experience of emo-
is the awareness of a disruption in the person’s tendency tional pain [8].
towards maintaining individual wholeness and social Orbach et al. [9, 10] have defined mental pain as ‘a wide
unity. Sandler [2, 3] defined psychological pain as the af- range of subjective experiences characterized as a percep-
fective state associated with discrepancy between ideal tion of negative changes in the self and its function that
and actual perception of self. Baumeister [4] referred to is accompanied by strong negative feelings’. Intense ‘un-
mental pain indirectly in his theory on suicide. He viewed bearable’ mental (psychological) pain is defined as an
mental pain as an aversive state of high self-awareness of emotionally based extremely aversive feeling which can
© 2012 S. Karger AG, Basel Eliana Tossani, PhD
0033–3190/13/0822–0067$38.00/0 Department of Psychology, University of Bologna
Fax +41 61 306 12 34 Viale Berti Pichat 5
E-Mail karger@karger.ch Accessible online at: IT–40127 Bologna (Italy)
www.karger.com www.karger.com/pps E-Mail eliana.tossani2 @ unibo.it
be experienced as torment. It can be associated with a term ‘suffering’ contains nonphysical dimensions – so-
psychiatric disorder or with a severe emotional trauma cial, psychological, cultural, spiritual – associated with
such as the death of a child. Psychological pain has many being a person that are relatively unaddressed in medical
metaphors borrowed from physical pain (e.g. heartache, training [24]. As Sensky [25] noted, the term ‘suffering’,
broken heart). however, may mean different things to different people.
Expressions such as ‘suffering from intense pain’, ‘suffer-
ing from a terminal illness’ or even ‘suffering a hangover’
Borderlands with Suffering and Other Types of Pain are indicative of these ambiguities.
The borderland between mental pain and pain re-
The International Association for the Study of Pain ferred to the body is also of difficult definition, since pain
[11] defined pain as ‘an unpleasant sensory and emotion- always involves a psychological component [26]. Engel
al experience associated with actual or potential tissue [26, p. 45] defines pain ‘as a psychological experience in-
damage, or described in terms of such damage’. The ex- volving the concepts of injury and suffering, but not con-
istence of many types of pain can be understood by the tingent on actual physical injury. The idea of injury as
identification of four broad categories: nociception, per- well as the need to suffer may lead to pain, just as may a
ception of pain, suffering, and pain behaviors [12]. Lo- real lesion or injury. Similarly, the need not to suffer or
eser [13] underlined that ‘suffering can be the result of not to accept the fact that injury may render a ‘‘painful’’
pain, or it can be engendered by many other states, such injury painless.’
as fear, anxiety, depression, hunger, fatigue, or loss of
loved objects. Suffering exists only in the mind and the
events that lead to suffering will differ from one patient Mental Pain and Depression
to another. There are no physical examination clues or
laboratory tests or imaging studies that reveal its pres- Klein [27] developed a dimensional model of unipolar,
ence. We must ask the patient and listen to his or her nar- endogenomorphic depression based on three specific
rative to find suffering’. neurobiologic factors: inhibited central pleasure, disin-
Frankl [14] viewed suffering as a form of emptiness hibited central pain, and inhibited psychomotor facilita-
due to loss of meaning in life, underlining that cause of tory mechanisms. Inhibited central pleasure represents
psychological problems originates from existential frus- an inability to respond to positive internal and external
tration. He added that ‘… existential frustration is in itself stimuli and results in anhedonia, lowered self-esteem,
neither pathological nor pathogenic. A person’s concern, and hopelessness. Disinhibited central pain can be de-
even his despair, over the worthwhileness of life is an ex- scribed as ‘psychic pain’ and represents an overresponse
istential distress but by no means a mental disease’ (p. to negative images and stimuli. Subjects feel unhappy,
123). The individual basic concern should not be to avoid guilty, agitated, and experience painful ruminations. Fi-
pain or gain pleasure, but to see meaning in life [15]. Suf- nally, inhibited psychomotor facilitatory mechanism is
fering terminates at the moment a meaning is found for synonymous with psychomotor retardation, decreased
it [16]. energy, and slowed thinking.
Saunders [17, 18] emphasized the connection between Carroll [28, 29] extended Klein’s model to characterize
physical pain and mental suffering: ‘If physical symptoms mood states in bipolar disorder. His model included four
are alleviated then mental pain is often lifted also’. neurobiologic components (consummatory reward, in-
This view has many similarities with Cassell’s [19, 20] centive reward, central pain, and psychomotor function).
definition of suffering. According to Cassell [19], suffer- Central pain is increased in depression, as reflected by
ing can be defined as a state of severe distress associated agitation, pathologic guilt and hopelessness. In the de-
with events that threaten the intactness of the person, pressed phase, this system is seen as disinhibited; stimu-
that occurs when an impending destruction of the person li that were previously nonaversive are experienced as dis-
is perceived. ‘Suffering is experienced by persons, not tressing. On this basis, the depressed patient perceives
merely by bodies, and has its source in challenges that neutral events as catastrophic. Changes in self-image due
threaten the intactness of the person as a complex social to central pain dysregulation go beyond feelings of in-
and psychological entity’ [19]. Suffering alienates the suf- competence and devaluation. The depressed patient per-
ferer from self and society [21], and may engender a ‘crisis ceives himself/herself as bad, unworthy, and guilty. In
of meaning’ [22] and a disintegration of hope [23]. The manic patients, a disinhibition of central pleasure repre-
68 Psychother Psychosom 2013;82:67–73 Tossani
sents an overresponse to positive images and stimuli, re- cape from intolerable suffering. Pain threshold and pain
sulting in inflated self-esteem, grandiosity, increased en- tolerance are highly and negatively correlated with per-
joyment of the environment, excessive activity, intrusive- sonal distress in suicidal persons [42–44]. In nonsuicidal
ness, and unrealistic optimism about the future. Inhib- persons, intense mental pain is associated with high sen-
ited central pain, proposed to occur in mania, results in sitivity to bodily pain. Conversely, among suicidal per-
an inability to perceive the negative qualities of oneself sons, intense mental anguish is associated with low sen-
and one’s environment. Clinical symptoms include in- sitivity to bodily pain.
flated self-esteem, elation, a disregard for the painful con-
sequences of one’s behavior, and overoptimism about the
future. Mental Pain and Other Psychiatric Disorders
Indeed, several psychopathologists [e.g. 30] have em-
phasized that the patients with endogenous depression Patients with borderline personality disorder have a
may manifest a ‘distinct quality’ of dysphoric mood. This range of intense dysphoric affects, sometimes experi-
feature was recognized by early clinicians [31, 32] and was enced as aversive tension, including rage, sorrow, shame,
described as a uniquely aversive, anguished, or uncom- panic, terror, and chronic feelings of emptiness and lone-
fortable experience that is characterized by painful ten- liness. These individuals can be distinguished from other
sion and torment [31]. groups by the overall degree of their multifaceted emo-
The study of van Heeringen et al. [33] reported chang- tional pain [45, 46]. This emotional pain has been inter-
es in brain functioning in association with mental pain preted as a response attempting to adapt to repetitive
in depressed patients. The results showed that levels of traumatic experiences in childhood such as the loss of a
mental pain do not correlate with severity of depression parent, parental mental illness, witnessed violence, emo-
but are associated with an increased risk of suicide. The tional, physical and sexual abuse [47]. Emotional pain is
severity of mental pain in these depressed patients was described as intense by women who suffer from border-
associated with changes in cerebral blood flow in areas of line personality disorder, and has been associated with a
the brain that are involved in the processing of emotions. high prevalence of reported childhood abuse [48].
The observation that depressed individuals become sui- Leibenluft et al. [49] conceptualized self-mutilation as
cidal when they perceive their emotional state as painful a need to feel a real physical pain as opposed to just an
and incapable of change [34] suggests a strong and per- emotional pain. However this conceptualization is not
sisting emotional input at the prefrontal level. Even congruent with the consistent reports of no pain upon
though the findings of van Heeringen et al. [33] indicate self-mutilation. It has also been suggested that deliberate
that dorsolateral hyperactivity is associated with in- self-harm provides physical stimulation (i.e., pain) suffi-
creased levels of mental pain, the interpretation of this ciently compelling to divert the individual’s attention
association needs further study. from painful emotional arousal; deliberate self-harm
may serve to shift attentional focus away from emotional
pain and toward physical pain [50].
Mental Pain and Suicide Mental pain has also been examined in the setting of
post-traumatic stress disorder. Avoidance has been pos-
Psychological pain is a common construct for under- tulated to involve strategic, effortful processes aimed at
standing suicide [5, 9, 35–37]. Suicide risk is much higher avoiding trauma stimuli, whereas numbing has been the-
when the general psychological and emotional pain orized to be a form of conditioned ‘emotional analgesia’
reaches intolerable intensity [38], particularly in the con- that results from exposure to uncontrollable and unpre-
text of major mood disorders [39]. Shneidman [5] consid- dictable aversive stimuli [51]. If an emotional pain site is
ered psychache to be the main ingredient of suicide and ‘anesthetized’, it is difficult to recognize emotions, much
reported that psychological pain may be correlated to the less discriminate, describe, or regulate these emotions. In
fact that, if suffering individuals could somehow stop a study involving 85 veterans, Monson et al. [52] assessed
consciousness and still live, they would opt for that solu- the relationships among emotion content and process
tion [40]. Shneidman [41] further postulated that psych- variables and post-traumatic stress disorder symptom-
ache is intolerable because it results from basic needs that atology with military-related trauma; they suggested that
have been thwarted. Suicide occurs when the psychache depression may be a secondary effect of numbing recog-
is deemed by that individual to be unbearable. It is an es- nition rather than vice versa.
Mental Pain Psychother Psychosom 2013;82:67–73 69
Grief needs) but does not include items relevant to the inten-
sity of psychological pain. The Psychache Scale is a 13-
Engel [53] underlined that grief is the characteristic item self-report scale used to assess psychache; items
response to the loss of a valued object, be it a loved per- are coded on a 5-point Likert-type scale. Good con-
son, a cherished possession, a job, status, home, country, struct validity and internal consistency have also been
an ideal, a part of the body, etc. Further, Engel pointed reported [62]. The Psychache Scale can successfully dif-
out that grief is a cause of mental pain, produces a vari- ferentiate between suicide attempters and nonattempt-
ety of bodily and psychological symptoms and it inter- ers [61].
feres with our ability to function effectively. Indeed, the The Orbach and Mikulincer Mental Pain Scale [9]
most prominent characteristic of grief is its painfulness consists of 44 self-rated items, and draws on a conceptu-
[54]. The pain of depression is similar to grief as are alization of mental pain as a perception of negative feel-
other depressive symptoms such as low energy, inward ings. The items of the Orbach and Mikulincer Mental
turning, preoccupation, guilt, and self-criticism. How- Pain Scale are divided into 9 factors: (1) irreversibility, (2)
ever, grief is less often characterized by low self-esteem, loss of control, (3) narcissist wounds, (4) emotional flood-
pessimism, and hopelessness. Losses of resources, in- ing, (5) freezing, (6) self-estrangement, (7) confusion, (8)
cluding health, material resources, territory, status, re- social distancing, and (9) emptiness. Subjects rate each
lationships or kin, cause comparable emotional pain. item on a 5-point Likert scale, with higher values reflect-
Kato and Mann [55] have suggested, for example, that ing greater mental pain. The Orbach and Mikulincer
the loss of a spouse is often conceptualized as a loss of Mental Pain Scale demonstrated high internal consisten-
the emotional, instrumental, and financial aspects of cy and test-retest reliability [9] and strong association
social support. with suicidality [10].
The Mee-Bunney Psychological Pain Assessment
Scale [63] is a 10-item self-rating inventory, where items
Assessment of Mental Pain uniformly used the term ‘psychological pain’ to measure
intensity of the pain (ranging from none to unbearable)
Several instruments have been developed to measure and frequency (ranging from never to always). The intent
mental pain or related constructs. of this scale is to provide the clinician with a quick and
The Psychological Pain Assessment Scale [5] was in- reliable assessment of psychological pain in psychiatric
fluenced in content and structure by the Thematic Ap- and nonpsychiatric populations. The Mee-Bunney Psy-
perception Test. It incorporates a written essay compo- chological Pain Assessment Scale demonstrated conver-
nent and requires a trained operator to administer the gent validity, known-groups validity and internal reli-
test and interpret the results. It is reported to have modest ability. Moreover, major depressive episode subjects with
validity [56, 57]. elevated scores on the Mee-Bunney Psychological Pain
The Multiple Visual Analog Scale [58] consists of 23 Assessment Scale had higher suicidality ratings and had
Visual Analog Scale items based on the Carroll-Klein an increased likelihood of having a past history of suicide
model of manic depressive illness. Each item is present- attempts [63].
ed as a 100-mm line visual analog scale, with appropri- Büchi et al. [64, 65] have devised a measure called the
ate anchor statements describing the manic and depres- Pictorial Representation of Self-Measure which, in vali-
sive extremes of each symptom. Of the 23 items, 7 rep- dation studies [65], behaves as expected of a measure of
resent each of the major dimensions of the Carroll-Klein suffering and fits well with Cassell’s conceptualization of
model (consummatory reward, central pain, and psy- suffering [19, 20]. This measure does not rely on language
chomotor regulation) and 2 items represent incentive skills and can be used to rapidly elicit patients’ appraisals
reward. Results from clinical studies demonstrated high of their suffering [66].
test-retest reliability of the Multiple Visual Analog Scale All these scales contribute to quantifying mental pain.
in depressed subjects [59] and good concurrent validity However, clinicians tend not to ask their patients about
[60]. their mental pain or suffering [25] and the most widely
The Psychache Scale [61] was based on Shneidman’s used interview-based instruments seem to ignore this as-
[5] definition of psychache that was associated with sui- pect. Clinimetrics offers important opportunities for as-
cidality (i.e., chronic, free-floating, non-situation-spe- sessing clinical phenomena such as mental pain [67, 68].
cific psychological pain caused by frustration of vital Table 1 illustrates how information on mental pain can
70 Psychother Psychosom 2013;82:67–73 Tossani
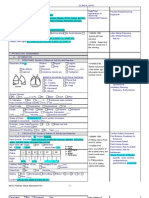
Table 1. Clinical assessment scale for mental pain (copyright Fava GA, Tossani E, 2012)
This refers to patient’s verbal expressions which indicate the characteristics of mental pain experienced by the
person (description, intensity, temporal patterns, associated physiological and behavioral processes that
aggravate or alleviate the pain).
‘Do you feel mental pain and suffering that goes beyond what one may experience in life from time to time?
How would you describe it? How does it compare with physical pain? Does it hurt all the time or in specific
moments? Does it occur every day or less frequently? Is there anything that makes it worse? Is there anything
that makes it better? Do you want to die when you feel it? Do you think that only death will stop it?’
Scores:
1 = Absent
2 = Very mild or occasional
3 = Mild (it comes at moments, and goes away)
4 = Moderate (it tends to be steady, even though it may also
occur in specific moments)
5 = Marked (it hurts all the time and does not get better)
6 = Severe (it is unbearable)
7 = Extreme (it makes you feel you want to die)
be obtained during an interview and can be rated. The tem that interprets the negative emotional signifi-
format of the questions and ratings are modeled upon cance of cognitions, with particular reference to the
Paykel’s Clinical Interview for Depression [69, 70], the role of amygdala and basal ganglia [28].
most comprehensive and sensitive assessment tool for af- – assessment of mental pain may have important impli-
fective disorders. cations in intervention research, particularly in psy-
chopharmacology. For instance, depressed patients
frequently report that treatment with antidepressant
Clinical and Research Implications drugs yields substantial relief of their mental pain. Un-
fortunately, in psychopharmacology research the ef-
There is pressing need of research on mental pain, af- fects of drugs are measured on a limited range of
ter decades of neglect. Some areas that appear to be par- symptoms [76].
ticularly important are: Clinical and research attention to the issue of mental
– even though mental pain always has an individual pain may produce important developments in psychiatry
meaning, consensus should be developed on its opera- and is in line with recent emphasis on patient-reported
tional definition; outcomes, defined as any report coming directly from
– mental pain may provide the clinical threshold that is patients, without interpretation of physicians or others,
essential for determining the amount of distress that about how they function or feel in relation to a health
is worthy of clinical attention, in conjunction with di- condition or its therapy [67].
agnostic criteria. It may offer a better specification of
the criterion on ‘clinically significant distress’ that fre-
quently recurs in DSM-IV [34]; Acknowledgment
– the balance between mental pain and psychological
I am very grateful to Professors Giovanni A. Fava and Tom
well-being [71, 72] deserves attention. Engel [73], in his
Sensky for their invaluable help and comments.
formulation of the pain-prone personality, outlined
how, in some instances, somatic pain is clearly protect-
ing the patient from more intense depression and even
suicide, and the psychological profile of the need to
suffer;
– the neurobiology of mental pain is a fascinating topic
that has been addressed only by a very limited amount
of research [33, 37, 74, 75]. It may unravel the brain sys-
Mental Pain Psychother Psychosom 2013;82:67–73 71
References
1 Bakan D: Disease, Pain, and Sacrifice: To- 23 Kearsley JH: The therapeutic use of self and 43 Orbach I, Stein D, Palgi Y, Asherov J, Har-
ward a Psychology of Suffering. Chicago, the relief of suffering. Cancer Forum 2010; Even D, Elizur A: Perception of physical pain
Beacon Press, 1968. 34:98–101. in accident and suicide attempt patients: self-
2 Sandler J: Psychology and psychoanalysis. Br 24 Egnew TR: Suffering, meaning, and healing: preservation vs self-destruction. J Psychiatr
J Med Psychol 1962;35:91–100. challenges of contemporary medicine. Ann Res 1996;30:307–320.
3 Sandler J: Trauma, strain, and development; Fam Med 2009;7:170–175. 44 Orbach I, Mikulincer M, Cohen D, King R,
in Furst SS (ed): Psychic Trauma. New York, 25 Sensky T: Suffering. Int J Integr Care 2010; Stein D: Thresholds and tolerance of physical
Basic Books, 1967, pp 154–174. 10:66–68. pain in suicidal and nonsuicidal adolescents.
4 Baumeister RF: Suicide as escape from self. 26 Engel GL: Pain; in Mac Bryde CM (ed): Signs J Consult Clin Psychol 1997;65:646–652.
Psychol Rev 1990;97:90–113. and Symptoms. Applied Pathological Physi- 45 Zanarini MC, Frankenburg FR, DeLuca CJ,
5 Shneidman ES: Suicide as psychache. J Nerv ology and Clinical Interpretation. Philadel- Hennen J, Khera GS, Gunderson JG: The
Ment Dis 1993;181:145–147. phia, Lippincott, 1969, pp 44–61. pain of being borderline: dysphoric states
6 Shneidman ES: The Suicidal Mind. New 27 Klein DF: Endogenomorphic depression: a specific to borderline personality disorder.
York, Oxford University Press, 1998. conceptual and terminological revision. Harv Rev Psychiatry 1998;6:201–207.
7 Shneidman ES: The psychological pain as- Arch Gen Psychiatry 1974;31:447. 46 Lieb K, Zanarini MC, Schmahl C, Linehan
sessment scale. Suicide Life Threat Behav 28 Carroll BJ: Psychopathology and neurobiol- MM, Bohus M: Borderline personality disor-
1999;29:287–294. ogy of manic-depressive disorders; in Car- der. Lancet 2004;364:453–461.
8 Bolger EA: Grounded theory analysis of roll BJ, Barrett JE (eds): Psychopathology and 47 Goodwin JM: Redefining borderline syn-
emotional pain. Psychother Res 1999;9:342– the Brain. New York, Raven Press, 1991, pp dromes as posttraumatic and rediscovering
362. 265–285. emotional containment as a first stage in
9 Orbach I, Mikulincer M, Sirota P, Gilboa- 29 Carroll BJ: Brain mechanisms in manic de- treatment. J Interpers Violence 2005; 20: 20–
Schechtman E: Mental pain: a multidimen- pression. Clin Chem 1994;40:303–308. 25.
sional operationalization and definition. 30 Mendels J, Cochrane C: The nosology of de- 48 Meerwijk EL: We need to talk about psycho-
Suicide Life Threat Behav 2003;33:219–230. pression: the endogenous-reactive concept. logical pain. Issues Ment Health Nurs 2012;
10 Orbach I, Mikulincer M, Gilboa-Schecht- Am J Psychiatry 1968;124:1–11. 33:263–265.
man E, Sirota P: Mental pain and its relation- 31 Kraepelin E: Manic-Depressive Insanity and 49 Leibenluft E, Gardner DL, Cowdry RW: The
ship to suicidality and life meaning. Suicide Paranoia (transl Barclay RM).. Edinburgh, inner experience of the borderline self-muti-
Life Threat Behav 2003;33:231–241. E&S Livingstone, 1921. lator. J Pers Disord 1987;1:317–324.
11 International Association for the Study of 32 Gillespie RD: Discussion on manic-depres- 50 Chapman AL, Gratz KL, Brown MZ: Solving
Pain: Pain terms: a list with definitions and sive psychosis. BMJ 1926;2:878–879. the puzzle of deliberate self-harm: the expe-
notes on usage. Recommended by the IASP 33 van Heeringen K, Van den Abbeele D, Ver- riential avoidance model. Behav Res Ther
Subcommittee on Taxonomy. Pain 1979; 6: vaet M, Soenen L, Audenaert K: The func- 2006;44:371–394.
249. tional neuroanatomy of mental pain in de- 51 Foa EB, Zinbarg R, Rothbaum BO: Uncon-
12 Loeser JD, Melzack R: Pain: an overview. pression. Psychiatry Res 2010;181:141–144. trollability and unpredictability in post-
Lancet 1999;353:1607–1069. 34 American Psychiatric Association: Diagnos- traumatic stress disorder: an animal model.
13 Loeser JD: Pain and suffering. Clin J Pain tic and Statistical Manual of Mental Disor- Psychol Bull 1992;112:218–238.
2000;16:S2–S6. ders, ed 4, Text Revision (DSM-IV-TR). 52 Monson CM, Price JL, Rodriguez BF, Ripley
14 Frankl VE: Man’s Search for Meaning. New Washington, American Psychiatric Press, MP, Warner RA: Emotional deficits in mili-
York, First Washington Square Press, 1963. 2000. tary-related PTSD: an investigation of con-
15 Frankl VE: Logotherapy and the challenge of 35 Leenaars AA: Clinical evaluation of suicide tent and process disturbances. J Trauma
suffering; in Hoeller K (ed): Readings in Ex- risk. Psychiatry Clin Neurosci 1995; 49:S61– Stress 2004;17:275–279.
istential Psychology and Psychiatry. Seattle, S68. 53 Engel GL: Is grief a disease? Psychosom Med
Review of Existential Psychology and Psy- 36 Valente SM: Messages of psychiatric patients 1961;23:18–22.
chiatry, 1961, pp 63–67. who attempted or committed suicide. Clin 54 Nesse RM: An evolutionary framework for
16 Frankl VE: Psychiatry and man’s quest for Nurs Res 1994;3:316–333. understanding grief; in Carr D, Nesse R,
meaning. J Relig Health 1962;1:93–103. 37 Mee S, Bunney BG, Reist C, Potkin SG, Bun- Wortman CB (eds): Late Life Widowhood in
17 Saunders C: The treatment of intractable ney WE: Psychological pain: a review of evi- the United States. New York, Springer, 2005,
pain in terminal cancer. Proc Royal Soc Med dence. J Psychiatr Res 2006;40:680–690. pp 195–226.
1963;56:195–197. 38 Berlim MT, Mattevi BS, Pavanello DP, 55 Kato PM, Mann T: A synthesis of psycholog-
18 Saunders C: Distress in dying. BMJ 1963; 2: Caldieraro MA, Fleck MP, Wingate LR, Join- ical interventions for the bereaved. Clin Psy-
746. er TE: Psychache and suicidality in adult chol Rev 1999;19:275–296.
19 Cassell EJ: The nature of suffering and the mood disordered outpatients in Brazil. Sui- 56 Leenaars AA: A note on Schneidman’s psy-
goals of medicine. N Engl J Med 1982; 306: cide Life Threat Behav 2003;33:242–248. chological pain assessment scale. OMEGA
639–645. 39 Joiner TE Jr, Brown JS, Wingate LR: The psy- 2004;50:301–307.
20 Cassell EJ: Diagnosing suffering: a perspec- chology and neurobiology of suicidal behav- 57 Pompili M, Lester D, Leenaars A, Tatarelli R,
tive. Ann Intern Med 1999;131:531–534. ior. Annu Rev Psychol 2005;56:287–314. Girardi P: Psychache and suicide: a prelimi-
21 Gillies J, Neimeyer RA: Loss, grief and the 40 Shneidman ES: Aphorisms of suicide and nary investigation 2008;38:116–121.
search for significance: towards a model of some implications for psychotherapy. Am J 58 Ahearn EP, Cassidy F, Kelley L, Weisler RH,
meaning reconstruction in bereavement. J Psychother 1984;38:319–328. Carroll BJ: Dimensions of self-rated mood in
Construct Psychol 2006;19:31–65. 41 Shneidman ES: Definition of Suicide. New depressed, manic, and normal subjects.
22 Barrett DA: Suffering and the process of York, Wiley, 1985. Compr Psychiatry 2001;42:196–201.
transformation. J Pastoral Care 1999; 53: 42 Orbach I, Palgi Y, Stein D, Har-Even D, 59 Ahearn EP, Carroll BJ: Short-term variability
461–472. Lotem-Peleg M, Asherov J, Elizur A: Toler- of mood ratings in unipolar and bipolar de-
ance of physical pain in suicidal individuals. pressed patients. J Affect Disord 1996; 36:
Death Stud 1996;20:327–340. 107–115.
72 Psychother Psychosom 2013;82:67–73 Tossani
60 Ahearn EP, Cassidy F, Kelley L, Weisler RH, 65 Büchi S, Buddeberg C, Klaghofer R, Russi 71 Ryff CD: Challenges and opportunities at the
Carroll BJ: Dimensions of self-rated mood in EW, Brandli O, Schlosser C, Stoll T, Villiger interface of aging, personality and well-be-
depressed, manic, and normal subjects. PM, Sensky T: Preliminary validation of ing; in John OP, Robins RW, Pervin LA (eds):
Compr Psychiatry 2001;42:196–201. PRISM (Pictorial Representation of Illness Handbook of Personality: Theory and Re-
61 Holden R, Mehta K, Cunningham E, McLeod and Self Measure) – A brief method to assess search. New York, Guilford Press 2008, pp
L: Development and preliminary validation suffering. Psychother Psychosom 2002; 71: 399–418.
of a scale of psychache. Can J Behav Sci 2001; 333–341. 72 Fava GA, Tomba E: Increasing psychological
33:224–232. 66 Büchi S, Sensky T: PRISM: Pictorial Repre- well-being and resilience by psychothera-
62 Mills JF, Green K, Reddon JR: An evaluation sentation of Illness and Self Measure. A brief peutic methods. J Pers 2009;77:1903–1934.
of the psychache scale on an offender popu- nonverbal measure of illness impact and 73 Engel GL: Psychogenic pain and pain-prone
lation. Suicide Life-Threat 2005, 35:570–580. therapeutic aid in psychosomatic medicine. patient. Am J Med 1959;26:899–918.
63 Mee S, Bunney BG, Bunney WE, Hetrick W, Psychosomatics 1999;40:314–320. 74 Eisenberger NI, Lieberman MD, Williams
Potkin SG, Reist C: Assessment of psycho- 67 Fava GA, Tomba E, Sonino N: Clinimetrics: KD: Does rejection hurt? An fMRI study of
logical pain in major depressive episodes. J the science of clinical measurements. Int J social exclusion. Science 2003;302:290–292.
Psychiatr Res 2011;45:1504–1510. Clin Pract 2012;66:11–15. 75 Schmahl C, Bohus M, Esposito F, Treede RD,
64 Büchi S, Sensky T, Sharpe L, Timberlake N: 68 Tomba E, Bech P: Clinimetrics and clinical Di Salle F, Greffrath W, Ludaescher P, Jo-
Graphic representation of illness: a novel psychometrics. Psychother Psychosom 2012; chims A, Lieb K, Scheffler K, Hennig J, Sei-
method of measuring patients’ perceptions 81: 333–343. fritz E: Neural correlates of antinociception
of the impact of illness. Psychother Psycho- 69 Guidi J, Fava GA, Bech P, Paykel E: The clin- in borderline personality disorder. Arch Gen
som 1998;67:222–225. ical interview for depression. Psychother Psychiatry 2006;63:659–667.
Psychosom 2011;80:10–27. 76 Fava GA: Clinical judgment in psychiatry:
70 Bech P: Mood and anxiety in the medically requiem or reveille? Nord J Psychiatry 2012,
ill. Adv Psychosom Med 2012;32:118–132. E-pub ahead of print.
Mental Pain Psychother Psychosom 2013;82:67–73 73
You might also like
- Yocan Evolve D User ManualDocument1 pageYocan Evolve D User ManualPhilip SpurrellNo ratings yet
- Free Will in The Many-Worlds Interpretation of Quantum MechanicsDocument21 pagesFree Will in The Many-Worlds Interpretation of Quantum MechanicsPhilip SpurrellNo ratings yet
- Abstract Book 2ndISMP3!11!2010Document180 pagesAbstract Book 2ndISMP3!11!2010Philip SpurrellNo ratings yet
- The Qa Im and Qiyama Doctrines in The THDocument69 pagesThe Qa Im and Qiyama Doctrines in The THPhilip SpurrellNo ratings yet
- Charles M. Stang - Our Divine Double-Harvard University Press (2016)Document320 pagesCharles M. Stang - Our Divine Double-Harvard University Press (2016)Philip Spurrell100% (7)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5796)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Social Psychology of Aggression 2nd Edition by Barbara KrahéDocument376 pagesThe Social Psychology of Aggression 2nd Edition by Barbara KrahéveroNo ratings yet
- Nursing Care Plan For Ineffective Tissue PerfusionDocument19 pagesNursing Care Plan For Ineffective Tissue Perfusionbrenhood78% (9)
- It Is Important For School-Aged Children To Be Educated About PubertalDocument3 pagesIt Is Important For School-Aged Children To Be Educated About PubertalCher Angel BihagNo ratings yet
- Nursing Process in Psychiatric NursingDocument11 pagesNursing Process in Psychiatric Nursinglissa_permataNo ratings yet
- Suicide Prevention, Intervention, and Postvention For Educators (Educator Module 80Document41 pagesSuicide Prevention, Intervention, and Postvention For Educators (Educator Module 80Cristy PestilosNo ratings yet
- Ensayo - El Impacto de Las Redes Sociales en Los JóvenesDocument4 pagesEnsayo - El Impacto de Las Redes Sociales en Los JóvenesLaura RodriguezNo ratings yet
- Child Sexual AbuseDocument12 pagesChild Sexual AbuseBayu Adi SNo ratings yet
- Mage The Awakening (RP Web Rotes)Document513 pagesMage The Awakening (RP Web Rotes)John Antonio Von TrappNo ratings yet
- BorderlineDocument12 pagesBorderlineksqvrkz4dmNo ratings yet
- Dialectical Behavior Therapy For Borderline Personality DisorderDocument27 pagesDialectical Behavior Therapy For Borderline Personality DisorderSalma MentariNo ratings yet
- The Effectiveness of 6 Versus 12-Months of DBTDocument16 pagesThe Effectiveness of 6 Versus 12-Months of DBTPechopalomo 90No ratings yet
- N 509 MaterialsDocument128 pagesN 509 MaterialsgdomagasNo ratings yet
- PDF - The DBT Hierarchy Prioritizing Treatment TargetsDocument16 pagesPDF - The DBT Hierarchy Prioritizing Treatment TargetsSana SheikhNo ratings yet
- Mental Health Act - Guide Book - 2016 PDFDocument124 pagesMental Health Act - Guide Book - 2016 PDFDanielle JenkinsNo ratings yet
- Clinical Case Reviews 2016Document34 pagesClinical Case Reviews 2016johnNo ratings yet
- CentreforMentalHealth MissedOpportunitiesDocument120 pagesCentreforMentalHealth MissedOpportunitiesMahmood ArafatNo ratings yet
- Cognitive Behavioral Play Therapy Play Therapy: Why Learn More About CBT?Document47 pagesCognitive Behavioral Play Therapy Play Therapy: Why Learn More About CBT?Anita Di Frangia100% (1)
- Documentation in School CounselingDocument8 pagesDocumentation in School Counselingapi-400733990100% (1)
- Nursing Care Plan For A Patient With Bipolar DisorderDocument20 pagesNursing Care Plan For A Patient With Bipolar Disordermjk2100% (4)
- What Not To Say If A Child Is Self-HarmingDocument2 pagesWhat Not To Say If A Child Is Self-HarmingPooky KnightsmithNo ratings yet
- Rehabilitation After Traumatic Injury PDF 66143770162117Document135 pagesRehabilitation After Traumatic Injury PDF 66143770162117Yilianeth Mena DazaNo ratings yet
- PPDCDocument12 pagesPPDCBernadette AycochoNo ratings yet
- Incentive Plus CatalogueDocument100 pagesIncentive Plus CatalogueIncentive PlusNo ratings yet
- Definition of A Stress: Crisis Management WorkshopDocument22 pagesDefinition of A Stress: Crisis Management WorkshopTubocurareNo ratings yet
- Suicidal Ideation and Behavior in AdultsDocument37 pagesSuicidal Ideation and Behavior in AdultsAna Luz AlvarezNo ratings yet
- Original PDFDocument3 pagesOriginal PDFmaxalves77No ratings yet
- Academic JournalDocument33 pagesAcademic JournalAddie SantosNo ratings yet
- Wombtwin Survivors IntroDocument16 pagesWombtwin Survivors IntroAlthea hayton100% (2)
- First Prompt FileDocument4 pagesFirst Prompt FileMahdi BanjakNo ratings yet
- Suicide: Risk Factors, Assessment, Methodological Problems: Sweta Sheth Chair: Dr. Rajesh GopalakrishnanDocument59 pagesSuicide: Risk Factors, Assessment, Methodological Problems: Sweta Sheth Chair: Dr. Rajesh GopalakrishnanpriyagerardNo ratings yet