Professional Documents
Culture Documents
Editor in Chief,+EJMED 670
Editor in Chief,+EJMED 670
Uploaded by
Genaro MendozaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Editor in Chief,+EJMED 670
Editor in Chief,+EJMED 670
Uploaded by
Genaro MendozaCopyright:
Available Formats
CASE REPORT
European Journal of Medical and Health Sciences
www.ejmed.org
Usefulness of Pirfenidone in Covid Lung: A Case Series
Abdul Basit Ibne Momen, Farhana Khan, Sadia Saber, Amrin Sultana, Rafa Faaria Alam,
Sheikh Golam Raihan, Mohammad Monower Hossain, and Md Tarek Alam
ABSTRACT
The year 2020 has been plagued by the COVID‑19 pandemic that has
Published Online: January 19, 2021
resulted in an additional 1,800,000 deaths worldwide. Many patients who
recover from Covid-19 later present with shortness of breath and fibrosis ISSN: 2593-8339
of the lungs, while some take a long time to recover from the initial
DOI: 10.24018/ejmed.2021.3.1.670
infection. A drug such as pirfenidone, which has been used for the
treatment of idiopathic pulmonary fibrosis, could offer additional benefits
by reverting pulmonary fibrotic damage. Here we describe a case series of Abdul Basit Ibne Momen*
five patients where addition of this drug showed marked improvement in Registrar, Department of Medicine,
symptoms and radiological findings. Apart from the efforts regarding Bangladesh Medical College, Dhaka,
Bangladesh.
understanding the pathophysiology of this new disease, we must also (e-mail: abdulbasit17@gmail.com)
evaluate the proportion of patients that develop chronic lung disease due to F. Khan
fibrosis following COVID-19 recovery. Certainly, more attention should be Senior Lecturer, Department of
given to new studies to determine the actual benefit of pirfenidone in Pharmacology, Ad-Din Women’s Medical
patients with pulmonary fibrosis as a result of Covid-19 infection. College, Dhaka, Bangladesh.
(e-mail: farhanakhan488@gmail.com)
S. Saber
Assistant Professor, Department of
Keywords: COVID-19, Pirfenidone, Pulmonary Fibrosis. Medicine, Bangladesh Medical College,
Dhaka, Bangladesh.
(e-mail: sadiasaber201477@gmail.com)
A. Sultana
Assistant Registrar, Department of
Medicine, Bangladesh Medical College,
Dhaka, Bangladesh.
(e-mail: amrinsultana2014@gmail.com)
R. F. Alam
Assistant Registrar, Department of
Medicine, Bangladesh Medical College,
Dhaka, Bangladesh.
(e-mail: rafa.alam27@gmail.com)
S. G. Raihan
Medical officer, Department of
Transfusion Medicine, Bangladesh
Medical College, Dhaka, Bangladesh.
(e-mail: raidenzero2008@gmail.com)
M. M. Hossain
Medical officer, Department of Medicine,
Bangladesh Medical College, Dhaka,
Bangladesh.
(e-mail: mhhossain44@gmail.com)
M. T. Alam
Professor and Head, Department of
Medicine, Bangladesh Medical College,
Dhaka, Bangladesh.
(e-mail: mtarekalam16@gmail.com)
*Corresponding Author
asymptomatic or barely symptomatic with slight sore throat,
I. INTRODUCTION the second and third stages include inflammation of the
SARS-CoV-2 infection may be mild for most but for a lungs and respiratory distress syndrome respectively [3].
few it has devastating consequences, starting from tissue Many patients who seem to recover from mild COVID-19
hyper inflammation, fibrosis and scarring of the lungs, lung later present with shortness of breath and fibrosis of the
collapse, multi-organ dysfunction, and even death [1]. Until lungs, while some take a long time to recover from the
now, there are no proven antiviral drugs against SARS- initial infection. The second and third stages are the most
CoV-2, so it is very vital to lower the aggressiveness of the crucial; in order to prevent formation of fibrotic tissue there
viral infection [2]. SARS-CoV-2 infection is divided into needs to be a well-timed immunomodulatory and anti-
three stages, in the first stage the patient being inflammatory treatment. A drug that is currently indicated
DOI: http://dx.doi.org/10.24018/ejmed.2021.3.1.670 Vol 3 | Issue 1 | January 2021 24
CASE REPORT
European Journal of Medical and Health Sciences
www.ejmed.org
for pulmonary fibrosis, such as pirfenidone, could offer C. Case 3
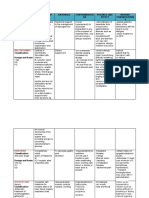
great additional benefits both during viral infection and in A 60-year-old COVID-19 positive man presented with
the recovery phase with remaining pulmonary fibrotic severe breathlessness and high fever; his condition was
damage [4]. severe enough to warrant admission to ICU. He was put on
high flow oxygen and the standard treatment started. Given
the severity of the patient’s lung involvement (Fig. 5)
II. CASE REPORT pirfenidone was started at a dose of 267 mg 1+1+1. After 45
A. Case 1 days the patient was fit for discharge, considering his overall
health and improvement of chest X-ray (Fig. 6).
A 46-year-old Covid-19 positive man was admitted with
the complaints of fever and malaise for 12 days and severe
difficulty in breathing for 7-8 days. On admission his
saturation was 90% and he was immediately started on
supplemental oxygen therapy and standard of care. His
condition improved but he remained short of breath while
performing daily activities and his oxygen saturation
remained at 94% and his chest X-ray (Fig. 1) showed
interstitial involvement, which did not resolve even after 20
days of supportive care. After that he was put on pirfenidone
267 mg 1+0+1. After 2 months his symptoms improved,
oxygen saturation was around 97% and his X-ray (Fig. 2)
had clearly improved.
Fig. 5. Patient 3, before anti- Fig. 6. Patient 3, after anti-
fibrotic. fibrotic.
D. Case 4
A 48-year-old Covid-19 positive man was admitted to the
hospital feeling shortness of breath after exertion. He said
that he had cough and a mild fever of 2 days and was given
standard of care. On the 14th day he became negative and
was discharged. Soon after discharge he started having
increasing shortness of breath, severe dry cough and low
oxygen saturation level. A CT scan of the chest (Fig. 7)
Fig. 1. Patient 1, before anti- Fig. 2. Patient 1, after anti-fibrotic. revealed bilateral ground glass opacities indicating
fibrotic. pulmonary fibrosis. The patient was started on pirfenidone
267 mg 1+1+1. And after 7 days the dose was increased to
B. Case 2 2+2+2. The repeat CT scan after 6 weeks (Fig. 8) showed
significant radiological improvement.
A 40-year-old COVID-19 positive man presented with
low grade fever, cough, and severe breathlessness; he had an
oxygen saturation of 94% with 10L supplemental oxygen on
admission. As with Patient 1, patient 2 also improved with
standard care but at a much slower rate and his X-rays
showed persistent interstitial infiltrates (Fig. 3). He was also
started on pirfenidone 267 mg 1+0+1. After 40 days the
patient had improved enough to be discharged and his X-ray
(Fig. 4) the day before discharge was improved as well.
Fig. 7. Patient 4, before anti- Fig. 8. Patient 4, after anti-
fibrotic. fibrotic.
E. Case 5
A 53-year-old man with severe Covid-19 was admitted to
the ICU and was on 60L of oxygen by high flow nasal
cannula. CT chest (Fig. 9) showed more than 70%
Fig. 3. Patient 2, before anti-fibrotic. Fig. 4. Patient 2, after anti-fibrotic. involvement bilaterally. He was started on pirfenidone 267
mg 1+1+1, and then the dose was increased to 801 mg
DOI: http://dx.doi.org/10.24018/ejmed.2021.3.1.670 Vol 3 | Issue 1 | January 2021 25
CASE REPORT
European Journal of Medical and Health Sciences
www.ejmed.org
1+1+1 and continued for 3 months. CT chest (Fig. 10) after IV. CONCLUSION
3 months showed significant improvement. We acknowledge the limitations of these case reports and
recognize that additional studies are needed to determine the
actual benefit from pirfenidone. Finally, only a well-
designed double-blind randomized controlled test is the
accepted technique to analyze this hypothesis.
REFERENCES
[1] Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of
SARS‐CoV2 may play a role in the respiratory failure of COVID‐19
patients. Journal of medical virology. 2020 Jun;92(6):552-5. Zhu N,
Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W,
Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W,
Fig. 9. Patient 5, before Fig. 10. Patient 5, after
China Novel Coronavirus Investigating and Research Team (2020) A
anti-fibrotic. anti-fibrotic.
novel coronavirus from patients with pneumonia in China, 2019. N
Engl J Med 382:727–733.
[2] Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H,
Lei CL, Hui DSC, du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang
III. DISCUSSION CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng
Pirfenidone was approved as an anti-fibrotic in China in YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G,
Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS, China Medical
December 2013 for the treatment of idiopathic pulmonary Treatment Expert Group for Covid-19 (2020) Clinical characteristics
fibrosis (IPF) [5]. The reduction in the over expression of of coronavirus disease 2019 in China. N Engl J Med 382:1708–1720
TGF-β, connective tissue growth factor (CTGF), platelet- [3] King CS, Nathan SD. Idiopathic pulmonary fibrosis: effects and
optimal management of comorbidities. The Lancet Respiratory
derived growth factors (PDGF), and tumour necrosis factor Medicine. 2017 Jan 1;5(1):72-84.
(TNF)- α in inflammatory diseases plays a key role in the [4] Maher TM, Corte TJ, Fischer A, Kreuter M, Lederer DJ, Molina-
anti-fibrotic activity of pirfenidone [6]. Like many patients Molina M, Axmann J, Kirchgaessler KU, Samara K, Gilberg F, Cottin
with post covid-19 fibrosis the five patients mentioned V. Pirfenidone in patients with unclassifiable progressive fibrosing
interstitial lung disease: a double-blind, randomised, placebo-
above also developed pulmonary fibrosis after covid-19 controlled, phase 2 trial. The Lancet Respiratory Medicine. 2020 Feb
which did not improved with standard care and necessitated 1;8(2):147-57.
the use of an anti-fibrotic such as pirfenidone. Addition of [5] Yang Y, Ye Y, Lin X, Wu K, Yu M. Inhibition of pirfenidone on
TGF-beta2 induced proliferation, migration and epithlial-
which showed marked improvement of both the patient’s mesenchymal transition of human lens epithelial cells line SRA01/04.
symptoms and improvement of the radiological finings. PloS one. 2013 Feb 21;8(2): e56837.
Some other studies showed similar findings, likewise, [6] Lancaster LH, de Andrade JA, Zibrak JD, Padilla ML, Albera C,
Nathan SD, Wijsenbeek MS, Stauffer JL, Kirchgaessler KU, Costabel
highlighted the shared danger of Coronavirus and IPF, and U. Pirfenidone safety and adverse event management in idiopathic
referenced that the weight of lung fibrosis following pulmonary fibrosis. European respiratory review. 2017 Dec
COVID-19 is probably going to be high; they presumed that 31;26(146).
[7] George PM, Wells AU, Jenkins RG. Pulmonary fibrosis and COVID-
given the size of the pandemic, the worldwide weight of 19: the potential role for antifibrotic therapy. The Lancet Respiratory
fibrotic lung sickness will presumably increase Medicine. 2020 May 15.
impressively. They additionally recommended a remedy like [8] Ferrara F, Granata G, Pelliccia C, La Porta R, Vitiello A. The added
value of pirfenidone to fight inflammation and fibrotic state induced
Pirfenidone and nintedanib as an anti-fibrotic treatment [7]. by SARS-CoV-2. European Journal of Clinical Pharmacology. 2020
Another study shows an anti-fibrotic drug like Nov;76(11):1615-8.
pirfenidone as monotherapy or together with anti- [9] Li Y, Li H, Liu S, Pan P, Su X, Tan H, Wu D, Zhang L, Song C, Dai
inflammatory drugs will be (acting early, at the proper doses M, Li Q. Pirfenidone ameliorates lipopolysaccharide-induced
pulmonary inflammation and fibrosis by blocking NLRP3
and at the proper time) therapeutically effective to avoid inflammasome activation. Molecular immunology. 2018 Jul 1;
serious complications during virus infection. The identical 99:134-44.
approach can even be effective as post-infection therapy in [10] Saha A, Vaidya PJ, Chavhan VB, Achlerkar A, Leuppi JD, Chhajed
PN. Combined pirfenidone, azithromycin and prednisolone in post-
patients with residual pulmonary fibrotic damage [8]. H1N1 ARDS pulmonary fibrosis. Sarcoidosis, Vasculitis, and Diffuse
It can be suggested that pirfenidone cause reduction of Lung Diseases. 2018;35(1):85.
lung injury based on a published data which shows that
pirfenidone decreases Lipo-polysaccharide (LPS) -induced
lung injury and subsequent fibrosis by suppressing NLRP3
inflammatory reaction [9].
Moreover, there's evidence of potential use of
pirfenidone, azithromycin and prednisolone within the
management of pulmonary fibrosis post-H1N1 ARDS,
supported data from a case report of three patients (young
males aged between 40-59 years) [10].
DOI: http://dx.doi.org/10.24018/ejmed.2021.3.1.670 Vol 3 | Issue 1 | January 2021 26
You might also like
- Mashaba FilesDocument1,268 pagesMashaba FilesGugu TeoNo ratings yet
- Member ListDocument16 pagesMember ListHappy AyichNo ratings yet
- Case Write Up - Dengue FeverDocument22 pagesCase Write Up - Dengue FevervijayaNo ratings yet
- ManuscriptDocument21 pagesManuscriptRipon MahmudNo ratings yet
- AbstractDocument2 pagesAbstractILul Hidayat ARNo ratings yet
- 1770-Article Text-3323-1-10-20210324Document16 pages1770-Article Text-3323-1-10-20210324priya selvarajNo ratings yet
- Proforma For Registration of Subject For Dissertation in M.D (Ayurveda) PanchakarmaDocument4 pagesProforma For Registration of Subject For Dissertation in M.D (Ayurveda) PanchakarmaKaamini WasadeNo ratings yet
- 1 - Nasim Mosarraf Hossain Thesis-11 DEC - 14-12-23Document69 pages1 - Nasim Mosarraf Hossain Thesis-11 DEC - 14-12-23shaf haqueNo ratings yet
- Original ArticleDocument12 pagesOriginal ArticleMiguel Ángel Ramírez AmbrízNo ratings yet
- Final DestinationDocument4 pagesFinal DestinationHartish LodheNo ratings yet
- LC MS ShinorineDocument23 pagesLC MS ShinorinerinjaniNo ratings yet
- E - APPROVAL OF BOARD OF EXAMINERSDocument1 pageE - APPROVAL OF BOARD OF EXAMINERSriyadh ahmedNo ratings yet
- Step On To Paediatrics 4th EditionDocument376 pagesStep On To Paediatrics 4th EditionTawhid Zihad100% (1)
- Ritesh Bachar CVDocument3 pagesRitesh Bachar CVsaifur riponNo ratings yet
- Dental BookDocument2 pagesDental BookrockyNo ratings yet
- Notification Draft For DME Website 12032024-1 1710329206504Document6 pagesNotification Draft For DME Website 12032024-1 1710329206504Rajender BNo ratings yet
- PDF DocumentsDocument4 pagesPDF DocumentsBharat RautNo ratings yet
- Application For BMRC Thesis GrantDocument2 pagesApplication For BMRC Thesis GrantYousuf SawdagorNo ratings yet
- Gizi - Prof. Dr. Dr. Haerani Rasyid, M.kes - SP.PD-KGH.,SP - GKDocument12 pagesGizi - Prof. Dr. Dr. Haerani Rasyid, M.kes - SP.PD-KGH.,SP - GKAa BbNo ratings yet
- Course Mbbs PDFDocument17 pagesCourse Mbbs PDFvasundhara lingayatNo ratings yet
- After 12 Science (Biology Group) : CareersDocument17 pagesAfter 12 Science (Biology Group) : CareersKanmaniNo ratings yet
- Illustrated Book of Pediatrics 2ndDocument975 pagesIllustrated Book of Pediatrics 2ndCarla Tapia Norambuena100% (2)
- Program - Annual Conference 2021 - PHABDocument12 pagesProgram - Annual Conference 2021 - PHABKoushik MajumderNo ratings yet
- Congratelett Snnbasfellow Bas21Document1 pageCongratelett Snnbasfellow Bas21Shohel RanaNo ratings yet
- Dhaka National Medical CollegeDocument2 pagesDhaka National Medical CollegeSubhas DasNo ratings yet
- Radiology and Imaging Diagnosis in Undergraduate Medicine in A Curriculum Using Active Methodologies: A Systematic Review From 2011 To 2021Document5 pagesRadiology and Imaging Diagnosis in Undergraduate Medicine in A Curriculum Using Active Methodologies: A Systematic Review From 2011 To 2021Monika GuptaNo ratings yet
- Ihtesham's Resume-2Document1 pageIhtesham's Resume-2IhteshamNo ratings yet
- Faculty of Pharmacy - Brochure 2019Document5 pagesFaculty of Pharmacy - Brochure 2019patelnidhi752128No ratings yet
- Adverse Reactions in Leprosy Patients Who Underwent Dapsone Multidrug Therapy: A Retrospective StudyDocument6 pagesAdverse Reactions in Leprosy Patients Who Underwent Dapsone Multidrug Therapy: A Retrospective StudyTheva CharaanNo ratings yet
- Journal Reading AsthmaDocument1 pageJournal Reading AsthmaMoira VillarinNo ratings yet
- Full Ebook of Textbook of Tuberculosis and Nontuberculousis Mycobacterial Diseases 3Rd Edition K Surendra Sharma Online PDF All ChapterDocument70 pagesFull Ebook of Textbook of Tuberculosis and Nontuberculousis Mycobacterial Diseases 3Rd Edition K Surendra Sharma Online PDF All Chaptersteventimmerman197670No ratings yet
- Organization Wise - BJSPSAA Members - 13.mar.17Document10 pagesOrganization Wise - BJSPSAA Members - 13.mar.17Abul Hasnat M SolaimanNo ratings yet
- Rajiv Gandhi University of Health Sciences Karnataka, BangaloreDocument10 pagesRajiv Gandhi University of Health Sciences Karnataka, Bangaloreshivangi YaduvanshiNo ratings yet
- International Seminar - Advancement - ManagementDocument1 pageInternational Seminar - Advancement - Managements.dey17No ratings yet
- The Impact of Combined Administration of Surfactant and IntratrachealDocument12 pagesThe Impact of Combined Administration of Surfactant and Intratrachealfrancklinmp.2022No ratings yet
- CV of Nazmul Hasan MehadiDocument3 pagesCV of Nazmul Hasan MehadiMd Elias MondolNo ratings yet
- Signature For Md. Al Nayeem 372 18 BatchDocument4 pagesSignature For Md. Al Nayeem 372 18 BatchAl-Nayeem TarafderNo ratings yet
- Resume PritamDocument2 pagesResume Pritamronit royNo ratings yet
- Faculty CMCLudhinaDocument3 pagesFaculty CMCLudhinasingh.sodhiiNo ratings yet
- Pharmacy Education Career Opportunities Pharmacists BD PDFDocument9 pagesPharmacy Education Career Opportunities Pharmacists BD PDFA. K. MohiuddinNo ratings yet
- PPA 333111 Between Curing and Torturing Burden of Adverse Reaction inDocument11 pagesPPA 333111 Between Curing and Torturing Burden of Adverse Reaction indiana.alyNo ratings yet
- Bus 07Document2 pagesBus 07Adnan MueedNo ratings yet
- List of Facility HeadDocument2 pagesList of Facility HeadShohel RanaNo ratings yet
- PIIS2405844022004443Document5 pagesPIIS2405844022004443Hendry SusantoNo ratings yet
- ProfileDocument1 pageProfileMuhammad Shahedul IslamNo ratings yet
- 12 Va 6 MG Dexametasona CovidDocument11 pages12 Va 6 MG Dexametasona CovidAlonso Marcelo Herrera VarasNo ratings yet
- Jamadermatol 2019 3064Document6 pagesJamadermatol 2019 3064Lucia MartinezNo ratings yet
- A Multi Centriccro Ss-Sectional Study On COVID19 in BangladeshDocument9 pagesA Multi Centriccro Ss-Sectional Study On COVID19 in Bangladeshrokon.is.hereNo ratings yet
- DR Anoop Cv-CompressedDocument3 pagesDR Anoop Cv-CompressedvarunNo ratings yet
- Stress Management With Organon of Medicine PDFDocument1 pageStress Management With Organon of Medicine PDFહિરેનપ્રફુલચંદ્રજોષીNo ratings yet
- Ce 2023022115595978Document10 pagesCe 2023022115595978Davi EmerimNo ratings yet
- List of ParticipantsDocument7 pagesList of Participantsmarkus_danusantosoNo ratings yet
- Be Daqui LinaDocument10 pagesBe Daqui LinaMario Jimenez JimenezNo ratings yet
- LTD Bio 250310Document1 pageLTD Bio 250310AsmaNo ratings yet
- Semi-Open Herniorrhaphy Reduces Postoperative CompDocument6 pagesSemi-Open Herniorrhaphy Reduces Postoperative CompBibek SutradharNo ratings yet
- Prot ICF 000Document36 pagesProt ICF 000nishita biswasNo ratings yet
- Oral Decontamination TechniquesDocument6 pagesOral Decontamination TechniquesYolandaMartaLenaNo ratings yet
- Effectiveness of Convalescent Plasma Therapy For COVID-19 Patients in Hunan, ChinaDocument12 pagesEffectiveness of Convalescent Plasma Therapy For COVID-19 Patients in Hunan, Chinaslrs08.srNo ratings yet
- Voter List 1690104663Document137 pagesVoter List 1690104663prasenjitpandit4No ratings yet
- Daftar Pustaka 1Document4 pagesDaftar Pustaka 1Primiandrianza ProrenataNo ratings yet
- Combination Therapy Against Multidrug ResistanceFrom EverandCombination Therapy Against Multidrug ResistanceMohmmad Younus WaniNo ratings yet
- Recent Advances and Future Perspectives of Microbial Metabolites: Applications in BiomedicineFrom EverandRecent Advances and Future Perspectives of Microbial Metabolites: Applications in BiomedicineSurajit de MandalNo ratings yet
- Lung TumorsDocument29 pagesLung Tumorssamar yousif mohamedNo ratings yet
- Parry Romberg SyndromeDocument7 pagesParry Romberg SyndromeAlexcr199415No ratings yet
- Neuronal CommunicationDocument29 pagesNeuronal CommunicationSamantha CNo ratings yet
- Uptodte TSVDocument215 pagesUptodte TSVcrilala23No ratings yet
- HEPATITIS A DRUG STUDY FinalDocument3 pagesHEPATITIS A DRUG STUDY FinalJordz PlaciNo ratings yet
- Rheumatic Fever and Heart DiseaseDocument30 pagesRheumatic Fever and Heart DiseaseerikarobertNo ratings yet
- LovenoxDocument1 pageLovenoxAdrianne BazoNo ratings yet
- Ehaa575 Supplementary DataDocument35 pagesEhaa575 Supplementary DataDaniela Zuluaga HurtadoNo ratings yet
- Cranial Nerve 6, 7 and 8 (Short Presentation)Document33 pagesCranial Nerve 6, 7 and 8 (Short Presentation)3uvpNo ratings yet
- Lip Angioedema Swellimng and HSV Following HA InjDocument2 pagesLip Angioedema Swellimng and HSV Following HA InjOmar NagrashNo ratings yet
- Case Study Myocardial InfarctionDocument23 pagesCase Study Myocardial InfarctionJester GalayNo ratings yet
- JAUNDICE and CHOLECYSTITISDocument109 pagesJAUNDICE and CHOLECYSTITISSarah Racheal AkelloNo ratings yet
- Drug Study and NCP For StrokeDocument7 pagesDrug Study and NCP For Strokegateway1119No ratings yet
- 5 Drug StudyDocument14 pages5 Drug StudyJennyLapitan100% (2)
- Cerebral Palsy Current Opinions On Definition Epidemiology Risk Factors Classification and Treatment OptionsDocument15 pagesCerebral Palsy Current Opinions On Definition Epidemiology Risk Factors Classification and Treatment OptionsLaura RugeNo ratings yet
- AzithromycinDocument3 pagesAzithromycinnekoleanNo ratings yet
- Case Writeup Albert Labores 9.24.2010 StrokeDocument6 pagesCase Writeup Albert Labores 9.24.2010 StrokeAJ RegaladoNo ratings yet
- New Paradigms in Women's Health April 13Document28 pagesNew Paradigms in Women's Health April 13Sex & Gender Women's Health CollaborativeNo ratings yet
- !! 2020 Drug Hypersensitivity ReactionsDocument12 pages!! 2020 Drug Hypersensitivity ReactionsdregleavNo ratings yet
- KDIGO GD Guideline Key Takeaways For Clinicians Lupus NephritisDocument1 pageKDIGO GD Guideline Key Takeaways For Clinicians Lupus Nephritisadamu mohammadNo ratings yet
- DISH TreatmentDocument6 pagesDISH TreatmentBorsecNo ratings yet
- Carboplatin PaclitaxelDocument6 pagesCarboplatin PaclitaxelNida Auliya RahmahNo ratings yet
- Self Assessment Quiz - EpilepsyDocument1 pageSelf Assessment Quiz - EpilepsyJan Mariel ClementeNo ratings yet
- 4Document14 pages4rashidrahmanktk3No ratings yet
- Clinical Profile and Outcome of Pelvi-Ureteric Junction Obstruction (PUJO) in Children Presenting Above 1 YearDocument48 pagesClinical Profile and Outcome of Pelvi-Ureteric Junction Obstruction (PUJO) in Children Presenting Above 1 YearWai GyiNo ratings yet
- Lecture ISK UKI - Dr. Sahala Panggabean SP - PDDocument25 pagesLecture ISK UKI - Dr. Sahala Panggabean SP - PDBen HonorseekerNo ratings yet
- Congenital SyphilisDocument8 pagesCongenital SyphilisMini LaksmiNo ratings yet
- Effects of Coffee/caffeine On Brain Health and Disease: What Should I Tell My Patients?Document7 pagesEffects of Coffee/caffeine On Brain Health and Disease: What Should I Tell My Patients?Mher Karizze Anne R. NarcisoNo ratings yet