Professional Documents
Culture Documents
Immune Responses in The Oral Cavity
Uploaded by
Ciro GuerraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Immune Responses in The Oral Cavity
Uploaded by
Ciro GuerraCopyright:
Available Formats
Category: Organs and Tissues
Immune Responses in the
Oral Cavity
Melissa Bedard, MRC Human Immunology Unit, University of Oxford
John Taylor, Newcastle University, UK
The oral cavity is a unique anatomical structure, characterised by the juxtaposition of soft and hard tissues and
which is continuously subject to challenge by the external environment and foreign material. Diseases and
disorders caused by oral microorganisms are very common and economically important, in particular dental
caries (loss of tooth integrity caused by bacteria-derived organic acids) and periodontitis (‘gum disease’;
chronic destructive inflammation of the supporting tissues of the teeth caused by anaerobic bacteria). Also,
halitosis (oral malodour) is caused by sulphide- producing oral bacteria. Oral diseases secondary to systemic
disease, e.g. oral candidiasis, due to acquired immunodeficiency are of increasing clinical importance. Also,
several autoimmune diseases such as Sjögren’s syndrome and pemphigus vulgaris have oral manifestations.
Saliva
Saliva is a key component of the host defence against infection in the mouth and patients with xerostomia
(‘dry mouth’) have higher levels of dental plaque and an increased risk of periodontitis and candidiasis than
otherwise healthy individuals. The saliva contains many molecular elements which restrict microbial growth:
for example, lysozyme cleaves bacterial cell walls, lactoferrin complexes iron ions which are an essential
microbial nutrient, and antimicrobial peptides such as histatins inhibit the growth of Candida albicans and
Streptococcus mutans (the latter being an aetiological agent of dental caries). Salivary IgA serves to
aggregate oral bacteria such as S. mutans and prevent the formation of dental plaque, a biofilm on the
exposed surface of teeth which comprises a thriving ecosystem for oral pathogens.
Tonsils
The tonsils are immune tissues located towards the back of the mouth; they comprise the palatine-, lingual-
and tubal tonsils as well as the adenoids (pharyngeal tonsils) and are collections of lymphoid tissue
immediately beneath the epithelium. Together the different tonsillar tissues form a ring of lymphoid tissue
known as Waldeyer’s ring which serves to protect the opening to the pharynx. The tonsils are often a site of
bacterial infection, likely because the clefts in which they appear are a site of collection of debris; this can lead
to recurring chronic inflammation and tonsillar enlargement (tonsillitis).
The periodontium
The tissues which surround and support the teeth (the periodontium) are complex and susceptible to acute
and chronic inflammation caused by plaque bacteria which accumulate in the space between the tooth and
the gum (the gingival sulcus). Fortunately, the periodontium has many host defence elements including the
gingival epithelium which prevents bacterial adhesion by constantly shedding keratinocytes into the oral
cavity (‘cell turnover’) and protecting against invasion by having a substantial keratin component (unlike other
tissues of the oral and gastrointestinal mucosa). The connective tissues of the periodontium are highly
vascular, facilitating vascular leukocyte emigration in response to infection and the gingival sulcus is bathed
with a serum exudate (gingival crevicular fluid, GCF) which carries complement components as well as
antibodies, neutrophils and plasma cells necessary to prevent tissue invasion by the sub-gingival plaque
bacteria. Whereas it is clear the destructive, chronic inflammation that manifests clinically as periodontitis is
caused by an excessive and inappropriate immune response to certain pathogenic plaque bacteria, coupled
with a failure of the normal processes that limit inflammation and drive tissue repair, we don’t yet have a
holistic understanding of how the dynamic oral microbiome with its complex cellular and molecular structures
interface with the host immune response and modify disease susceptibility. Studies of the oral microbiome
will serve as another paradigm for host-microbiome interactions as determinants of health as has been
revealed by studies of the gut microbiome.
Medical relevance
Interest in oral immunology has heightened in recent years with the recognition that there are clinical
associations between periodontitis and systemic diseases other chronic inflammatory diseases of the ageing
population (e.g. rheumatoid arthritis, diabetes and cardiovascular disease). We are beginning to reveal
pathogenic links between these diseases that may inform improved patient management e.g. activation of
immune cells such as monocytes by plaque bacteria may contribute to the development of atherosclerosis.
Saliva which mixes with GCF in the oral cavity, is a rich and non-invasive source of disease biomarkers such as
cytokines, tissue destructive enzymes and pathogenic microorganisms, as well as
DNA for studies of genetic associations and pharmacogenomics.
© The copyright for this work resides with the British Society for Immunology
You might also like
- Immunity in The Oral CavityDocument1 pageImmunity in The Oral CavityRochman MujayantoNo ratings yet
- Review Article Porphyromonas Gingivalis Periodontal Infection and ItsDocument11 pagesReview Article Porphyromonas Gingivalis Periodontal Infection and ItsMitzi Carolina SierraNo ratings yet
- 1.oral Infectious DiseasesDocument68 pages1.oral Infectious DiseasesDrMohamed AssadawyNo ratings yet
- Etiology and Microbiology of Periodontal Diseasea PDFDocument7 pagesEtiology and Microbiology of Periodontal Diseasea PDFlalalalaNo ratings yet
- Litrev Draft 2 Pages VersionDocument13 pagesLitrev Draft 2 Pages Versionapi-710900838No ratings yet
- Periodontal Diseases As Bacterial Infection: Bascones Martinez A Figuero Ruiz EDocument8 pagesPeriodontal Diseases As Bacterial Infection: Bascones Martinez A Figuero Ruiz EWidaRostinaNo ratings yet
- Saliva: Histatins Inhibit The Growth of Candida Albicans and Streptococcus Mutans (The LatterDocument3 pagesSaliva: Histatins Inhibit The Growth of Candida Albicans and Streptococcus Mutans (The LatterEhab Ahmed Hussein ReyadNo ratings yet
- Normal Bacterial Flora of Humans (Page 5) : (This Chapter Has 5 Pages)Document8 pagesNormal Bacterial Flora of Humans (Page 5) : (This Chapter Has 5 Pages)yaduvansi,rajeshNo ratings yet
- Oral Microbiology Periodontitis PDFDocument85 pagesOral Microbiology Periodontitis PDFSIDNEY SumnerNo ratings yet
- Periodontal Microbiology 2017Document17 pagesPeriodontal Microbiology 2017LEENo ratings yet
- 1 s2.0 S0165247814001874 Main PDFDocument17 pages1 s2.0 S0165247814001874 Main PDFIonela MadalinaNo ratings yet
- 2000 Controlled and Targeted Drug Delivery Strategies Towards Intraperiodontal Pocket DiseasesDocument22 pages2000 Controlled and Targeted Drug Delivery Strategies Towards Intraperiodontal Pocket DiseasesK KNo ratings yet
- Interrelationship Between Periapical Lesion and Systemic Metabolic DisordersDocument28 pagesInterrelationship Between Periapical Lesion and Systemic Metabolic DisordersmeryemeNo ratings yet
- Systemic Diseases Caused by Oral InfectionDocument12 pagesSystemic Diseases Caused by Oral InfectionaninuraniyahNo ratings yet
- Pharmaceutics 14 02740Document18 pagesPharmaceutics 14 02740Robert StryjakNo ratings yet
- Periodontal Disease Research PaperDocument10 pagesPeriodontal Disease Research Paperapi-738493105No ratings yet
- 2022 - Horvat Aleksijevic - Porphyromonas Gingivalis - Pathogens-11-01173Document19 pages2022 - Horvat Aleksijevic - Porphyromonas Gingivalis - Pathogens-11-01173Ivana V SkrlecNo ratings yet
- Jcad 13 6 48Document6 pagesJcad 13 6 48neetika guptaNo ratings yet
- Atherosclerosis 1Document10 pagesAtherosclerosis 1Gustivanny Dwipa AsriNo ratings yet
- Gingivitis: November 2018Document14 pagesGingivitis: November 2018RamonaNo ratings yet
- Shweta PPT ThesisDocument10 pagesShweta PPT ThesisAKSHAY WAKTENo ratings yet
- Current Concepts in The Pathogenesis of Periodontitis: From Symbiosis To DysbiosisDocument20 pagesCurrent Concepts in The Pathogenesis of Periodontitis: From Symbiosis To DysbiosisgugicevdzoceNo ratings yet
- International Journal of Dental Science and Innovative Research (IJDSIR)Document10 pagesInternational Journal of Dental Science and Innovative Research (IJDSIR)ReshmaaRajendranNo ratings yet
- Microbiological and Immuno-Pathological Aspects of Peri-Implant DiseasesDocument25 pagesMicrobiological and Immuno-Pathological Aspects of Peri-Implant DiseasesPaul IvanNo ratings yet
- Pulp and InjuryDocument13 pagesPulp and InjuryAfin Aslihatul UmmahNo ratings yet
- JeffreyDocument26 pagesJeffreyFarinaEkaNo ratings yet
- Review of Osteoimmunology and The Host Response in Endodontic and Periodontal LesionsDocument16 pagesReview of Osteoimmunology and The Host Response in Endodontic and Periodontal LesionsNaeem MoollaNo ratings yet
- Textos Cientificos OdontologicosDocument11 pagesTextos Cientificos Odontologicosdocsamu78No ratings yet
- Gingivitis: An Overall View For Undergraduate: November 2018Document12 pagesGingivitis: An Overall View For Undergraduate: November 2018Sannia SalsabilaNo ratings yet
- Diagnostics of Oral Mucosae: Histology and Microbiology - Clinical RelevanceDocument14 pagesDiagnostics of Oral Mucosae: Histology and Microbiology - Clinical RelevanceGeorgi GugicevNo ratings yet
- CH 13 CariesDocument18 pagesCH 13 CariesRaimaa talalNo ratings yet
- RK PerioDocument17 pagesRK PerioraniNo ratings yet
- Kuretase GigiDocument6 pagesKuretase GigiAfif Fathur RahmanNo ratings yet
- Bacteriology of Most Frequent Oral Anaerobic Infections: S. PiovanoDocument7 pagesBacteriology of Most Frequent Oral Anaerobic Infections: S. PiovanoVinícius LeiteNo ratings yet
- GastroDocument77 pagesGastroMarielle RamosNo ratings yet
- Normal Oral Microbial FloraDocument17 pagesNormal Oral Microbial FloraNeeraj Rajendra MehtaNo ratings yet
- Endo-Perio Dilemma A Brief ReviewDocument16 pagesEndo-Perio Dilemma A Brief ReviewZahra Khairiza AnriNo ratings yet
- Prevalence of Periodontal Disease in Children With Leukemia and ThalassemiaDocument14 pagesPrevalence of Periodontal Disease in Children With Leukemia and ThalassemiaZackNo ratings yet
- Normal Flora of The Human BodyDocument7 pagesNormal Flora of The Human Bodyshahbaz88% (16)
- Principles and Practice Antibiotic Therapy: S. DDS, MsDocument20 pagesPrinciples and Practice Antibiotic Therapy: S. DDS, MsAlejandro LinaresNo ratings yet
- Microbiology of Periodontal Diseases A ReviewDocument7 pagesMicrobiology of Periodontal Diseases A ReviewghassanNo ratings yet
- Articulo Cientifico 2, MartesDocument7 pagesArticulo Cientifico 2, MartesValeryNo ratings yet
- Microbial Flora in Oral DiseasesDocument7 pagesMicrobial Flora in Oral DiseasesNur FadhilahNo ratings yet
- 261 773 1 PB PDFDocument8 pages261 773 1 PB PDFDr Monal YuwanatiNo ratings yet
- Lec 2Document5 pagesLec 2spo9equtabaNo ratings yet
- Detection of Trichomonas Tenax (T. Tenax) in Bad Oral Hygiene Saudi Patients in Taif CityDocument3 pagesDetection of Trichomonas Tenax (T. Tenax) in Bad Oral Hygiene Saudi Patients in Taif CityInternational Educational Applied Scientific Research Journal (IEASRJ)No ratings yet
- Brush Up Your Teeth To Brush Up Your Heart A Clinical Review On The Association of Oral Hygiene With Cardiovascular DiseasesDocument7 pagesBrush Up Your Teeth To Brush Up Your Heart A Clinical Review On The Association of Oral Hygiene With Cardiovascular DiseasesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Management and Treatment of Fungal Infection in The Oral CavityDocument4 pagesManagement and Treatment of Fungal Infection in The Oral CavityKIU PUBLICATION AND EXTENSIONNo ratings yet
- Microorganisms 11 00115Document15 pagesMicroorganisms 11 00115Mariana PalaciosNo ratings yet
- Controversies in PeriodonticsDocument56 pagesControversies in PeriodonticsReshmaa Rajendran100% (1)
- Caries Vaccine: Guided By: Presented byDocument5 pagesCaries Vaccine: Guided By: Presented byharishgnrNo ratings yet
- OWC Part16Document29 pagesOWC Part16Boby FaesalNo ratings yet
- Perio MedicineDocument90 pagesPerio MedicineAnsh Veer ChouhanNo ratings yet
- Endo-Perio Dilemma A Brief ReviewDocument10 pagesEndo-Perio Dilemma A Brief ReviewLuisNo ratings yet
- Management of Odontogenic Infection of Pulpal and Periodontal OriginDocument6 pagesManagement of Odontogenic Infection of Pulpal and Periodontal OriginNor Sakinah MNo ratings yet
- Saliva Protection and Transmissible DiseasesFrom EverandSaliva Protection and Transmissible DiseasesRating: 5 out of 5 stars5/5 (1)
- Oral Probiotics: Fighting Tooth Decay, Periodontal Disease and Airway Infections Using Nature’s Friendly BacteriaFrom EverandOral Probiotics: Fighting Tooth Decay, Periodontal Disease and Airway Infections Using Nature’s Friendly BacteriaNo ratings yet
- Clinical Periodontology and Implant Dentistry, 2 Volume SetFrom EverandClinical Periodontology and Implant Dentistry, 2 Volume SetNo ratings yet
- Female Sexual DysfunctionDocument18 pagesFemale Sexual DysfunctionRisky SetiawanNo ratings yet
- Stylohyoid LigamentDocument4 pagesStylohyoid LigamentArindom ChangmaiNo ratings yet
- 1translation and MedicineDocument202 pages1translation and MedicineMNNo ratings yet
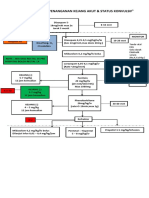
- Algoritma Penanganan Kejang AkutDocument1 pageAlgoritma Penanganan Kejang AkutEwa ClaudiaNo ratings yet
- Notes On MRI - FinalDocument16 pagesNotes On MRI - FinalAnju GuptaNo ratings yet
- Case Report: Hepatitis BDocument34 pagesCase Report: Hepatitis Bdewi sartikaNo ratings yet
- University of The PhilppinesDocument22 pagesUniversity of The PhilppinesFibi Pho0% (1)
- ID-IM-SQ-E ToolDocument9 pagesID-IM-SQ-E TooltriciacamilleNo ratings yet
- Agger NasiDocument3 pagesAgger NasiDr Saikat SahaNo ratings yet
- Paper 1Document11 pagesPaper 1api-499574410No ratings yet
- News 638228866844085591Document4 pagesNews 638228866844085591Divya Prakash KushwahaNo ratings yet
- Research Paper - Stem Cells-3Document11 pagesResearch Paper - Stem Cells-3api-549248786No ratings yet
- Chapter 1 Introduction To Biopharmaceutics and Pharmacokinetics 1Document92 pagesChapter 1 Introduction To Biopharmaceutics and Pharmacokinetics 1Marc Alamo100% (2)
- Law Exam NotesDocument11 pagesLaw Exam NotesEric Cheng100% (1)
- Report On Januvia DrugDocument10 pagesReport On Januvia DrugyogenaNo ratings yet
- DYSRHYTHMIASDocument9 pagesDYSRHYTHMIASgudobenNo ratings yet
- All India Hospital ListDocument303 pagesAll India Hospital ListwittyadityaNo ratings yet
- PreparateDocument2 pagesPreparateVasile LozinschiiNo ratings yet
- UntitledDocument14 pagesUntitledsyntacs skNo ratings yet
- Grand Rounds Facial Nerve ParalysisDocument86 pagesGrand Rounds Facial Nerve ParalysisA170riNo ratings yet
- Nursing Diagnosis - Wikipedia, The Free EncyclopediaDocument9 pagesNursing Diagnosis - Wikipedia, The Free EncyclopediaDika YolandaNo ratings yet
- Bisphosphonate Treatment Break Guidance June 2017Document2 pagesBisphosphonate Treatment Break Guidance June 2017Usman Zafar QaziNo ratings yet
- Jurnal Kesehatan Dr. SoebandiDocument6 pagesJurnal Kesehatan Dr. SoebandiHary BudiartoNo ratings yet
- Gynera: Coated TabletsDocument67 pagesGynera: Coated TabletsOdeke VascoNo ratings yet
- Jane Doe Advance DirDocument24 pagesJane Doe Advance Dirapi-224104463No ratings yet
- Hemorrhagic Disease of The NewbornDocument3 pagesHemorrhagic Disease of The NewbornDevi SuryandariNo ratings yet
- Clinical PathologyDocument13 pagesClinical Pathologyapi-19710563100% (1)
- Practice TestDocument2 pagesPractice TestMinh Châu NguyễnNo ratings yet
- Management of The Third Stage of LaborDocument12 pagesManagement of The Third Stage of Laborayu_pieterNo ratings yet
- Inion Freedom Brochure v2 12-2014Document11 pagesInion Freedom Brochure v2 12-2014Ivo van de KampNo ratings yet