An abscess (Latin: abscessus) is a collection of pus (dead neutrophils) that has accumulated in a cavity formed by the
tissue in which the pus resides on the basis of an infectious process (usually caused by bacteria or parasites) or other
foreign materials (e.g., splinters, bullet wounds, or injecting needles). It is a defensive reaction of the tissue to prevent
the spread of infectious materials to other parts of the body. One example of an abscess is a BCG-oma, which is caused
because of incorrect administration of the BCG vaccine.
The organisms or foreign materials kill the local cells, resulting in the release of cytokines. The cytokines trigger an
inflammatory response, which draws large numbers of white blood cells to the area and increases the regional blood
flow.
The final structure of the abscess is an abscess wall, or capsule, that is formed by the adjacent healthy cells in an attempt
to keep the pus from infecting neighboring structures. However, such encapsulation tends to prevent immune cells from
attacking bacteria in the pus, or from reaching the causative organism or foreign object.
Abscesses must be differentiated from empyemas, which are accumulations of pus in a preexisting rather than a newly
formed anatomical cavity.
Signs and symptoms
The cardinal symptoms and signs of any kind of inflammatory process are redness, heat, swelling, pain and loss of
function. Abscesses may occur in any kind of solid tissue but most frequently on skin surface (where they may be
superficial pustules (boils) or deep skin abscesses), in the lungs, brain, teeth, kidneys and tonsils. Major complications
are spreading of the abscess material to adjacent or remote tissues and extensive regional tissue death (gangrene).
Abscesses in most parts of the body rarely heal themselves, so prompt medical attention is indicated at the first
suspicion of an abscess. An abscess could potentially be fatal (although this is rare) if it compresses vital structures such
as the trachea in the context of a deep neck abscess. [citation needed]
Treatment
Wound abscesses do not generally need to be treated with antibiotics, but they will require surgical intervention,
debridement and curettage.[1]
Incision and drainage
The abscess should be inspected to identify if foreign objects are a cause, which may require their removal. If foreign
objects are not the cause, a doctor will incise and drain the abscess and prescribe painkillers and possibly antibiotics. [2]
Surgical drainage of the abscess (e.g., lancing) is usually indicated once the abscess has developed from a harder serous
inflammation to a softer pus stage. This is expressed in the Latin medical aphorism: Ubi pus, ibi evacua.
In critical areas where surgery presents a high risk, it may be delayed or used as a last resort. The drainage of a lung
abscess may be performed by positioning the patient in a way that enables the contents to be discharged via the
respiratory tract. Warm compresses and elevation of the limb may be beneficial for a skin abscess.
Packing
In North America, after drainage, an abscess cavity is often packed. However, there is no evidence to support this
practice and it may in fact delay healing. [3] To try to answer this question more definitely, a randomized double-blind
study was started in September 2008 and was completed in March 2010. [4] Interim analysis of data from this study
suggests that "wound packing may significantly increase the failure rates." [5] A small pilot study has found no benefit
from packing of simple cutaneous abscesses. [6]
�Primary closure
Primary closure has been successful when combined with curettage and antibiotics[7] or with curettage alone.[8] However,
another randomized controlled trial found primary closure led to 35% failing to heal primarily and primary closure longer
median number of days to closure (8.9 versus 7.8). [9]
In anorectal abscesses, primary closure healed faster, but 25% of abscesses healed by secondary intention and
recurrence was higher.[10]
Antibiotics
As Staphylococcus aureus bacteria is a common cause, an anti-staphylococcus antibiotic such as flucloxacillin or
dicloxacillin is used. With the emergence of community-acquired methicillin-resistant staphylococcus aureus MRSA,
these traditional antibiotics may be ineffective; alternative antibiotics effective against community-acquired MRSA often
include clindamycin, trimethoprim-sulfamethoxazole, and doxycycline. These antibiotics may also be prescribed to
patients with a documented allergy to penicillin. (If the condition is thought to be cellulitis rather than abscess,
consideration should be given to possibility of strep species as cause that are still sensitive to traditional anti-
staphylococcus agents such as dicloxacillin or cephalexin in patients able to tolerate penicillin). It is important to note
that antibiotic therapy alone without surgical drainage of the abscess is seldom effective due to antibiotics often being
unable to get into the abscess and their ineffectiveness at low pH levels. Whilst most medical texts advocate surgical
incision some medical doctors will treat small abscesses conservatively with antibiotics.
Recurrent infections
Recurrent abscesses are often caused by community-acquired MRSA. While resistant to most beta lactam antibiotics
commonly used for skin infections, it remains sensitive to alternative antibiotics, e.g., clindamycin (Cleocin),
trimethoprim-sulfamethoxazole (Bactrim), and doxycycline (unlike hospital-acquired MRSA that may only be sensitive to
vancomycin IV).
To prevent recurrent infections due to Staphylococcus, consider the following measures:
Topical mupirocin applied to the nares.[11] In this randomized controlled trial, patients used nasal mupirocin
twice daily 5 days a month for 1 year.
Chlorhexidine baths,[12] In a randomized controlled trial, nasal recolonization with S. aureus occurred at 12 weeks
in 24% of nursing home residents receiving mupirocin ointment alone (6/25) and in 15% of residents receiving
mupirocin ointment plus chlorhexidine baths daily for the first three days of mupirocin treatment (4/27).
Although these results did not reach statistical significance, the baths are an easy treatment.
Magnesium sulfate paste
Historically abscesses as well as boils and many other collections of pus have been treated via application of magnesium
sulfate (Epsom salt) paste. This works by drawing the infected pus to the surface of the skin before rupturing and leaking
out. After this the body will usually repair the old infected cavity. Magnesium sulfate is therefore best applied at night
with a sterile dressing covering it, the rupture itself is not painful but the drawing up may be uncomfortable. Magnesium
sulfate paste is considered a "home remedy" and is not necessarily an effective or accepted medical treatment. [citation
needed]
Perianal abscess
Perianal abscesses can be seen in patients with for example inflammatory bowel disease (such as Crohn's disease) or
diabetes. Often the abscess will start as an internal wound caused by ulceration or hard stool. This wound typically
becomes infected as a result of the normal presence of feces in the rectal area, and then develops into an abscess. This
often presents itself as a lump of tissue near the anus which grows larger and more painful with the passage of time.
�Like other abscesses, perianal abscesses may require prompt medical treatment, such as an incision and debridement or
lancing.
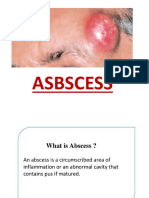
An abscess is a hollow space in the body that is filled with pus and surrounded by inflamed tissue. Abscesses can be
serious and lead to gangrene and permanent organ damage if they are not recognized and treated promptly.
An abscess forms from a bacterial infection, parasitic infection or foreign body and can develop in many places in the
body. One type of bacteria that commonly causes abscesses is Staphylococcus aureus. Examples of abscesses include
skin abscess, brain abscess, lung abscess, kidney abscess, bones abscess, abdominal abscess, rectal abscess, breast
abscess, liver abscess, spinal cord abscess and tooth abscess.
An abscess develops when harmful bacteria or parasites infect an area of body tissue, such as the gums or the skin. The
body tries to attack the infection by sending a surge of white blood cells (infection fighting cells) to the infected area.
During this process living and dead white blood cells, fluid, bacteria, and dead tissue collect within the diseased tissue
and form pus. The surrounding tissue also becomes inflamed and painful.
Symptoms and complications of an abscess vary depending on the area of the body where it develops. Symptoms often
include swelling and pain. Some types of abscesses can lead to serious, even life-threatening complications, such as
sepsis, kidney failure, shock, and death. For more information on complications and symptoms, refer to symptoms of
abscess.
People at risk for an abscess and its complications include those who have a compromised immune system due to such
diseases as HIV/AIDS or combined immunodeficiencies. People who take certain medications, such as corticosteroids or
chemotherapy, which suppress the body's natural immune response, are also at risk for contracting an abscess. Other
risk factors include having diabetes, cancer, Crohn's disease, ulcerative colitis, severe burns, or severe trauma.
Making a diagnosis of an abscess begins with taking a thorough medical history, including symptoms, and completing a
physical examination. The types of diagnostic testing performed for a suspected abscess varies depending on the
symptoms. A complete blood count (CBC) is a blood test is often performed. A complete blood count measures the
numbers of different types of blood cells, including white blood cells (WBCs). Different types of WBCs increase in
number in characteristic ways during an infectious or inflammatory process, such as an abscess.
A culture and sensitivity test (C and S) may also be performed and involves taking a small sample from the abscess and
growing it in the laboratory. This test determines the type of organism causing the abscess, as well as which antibiotics
would be most effective in treating it.
Imaging tests, such as X-ray, CT, or MRI, may be performed to assist in the diagnosis of some internal abscesses, such as
a pancreatic abscess, liver abscess or kidney abscess. Additional tests may be performed in order to rule out or confirm
other diseases that may accompany an abscess or cause similar symptoms.
It is possible that a diagnosis of an abscess can be missed or delayed because some symptoms, such as fever and
inflammation are similar to symptoms of other diseases of conditions. For more information on misdiagnosis, refer to
misdiagnosis of abscess.
Treatment of an abscess varies depending on its location and other diseases and conditions that may coexist with the
abscess.