Professional Documents
Culture Documents
Ophthalmology How To Examine An Eye: Visual Acuity
Uploaded by
Olalekan Ogundare0 ratings0% found this document useful (0 votes)
13 views2 pagesOriginal Title
O3
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
13 views2 pagesOphthalmology How To Examine An Eye: Visual Acuity
Uploaded by
Olalekan OgundareCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
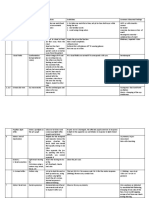
OPHTHALMOLOGY
HOW TO EXAMINE AN EYE
Visual Acuity
Use a Snellen chart. Test each eye separately at 6 meters.
Allow the patient to use glasses.
If acuity reduced use a pinhole (corrects refractive error).
If no improvement with pinhole the problem is not refractive.
Document: distance in meters/number of line read
If unable to read at 6m try 3m.
Try counting fingers if unable to read at 3m.
Check if hand movements are seen if unable to count fingers.
Cranial Nerve Examination
Pupillary responses, visual fields and eye movements.
External Eye
Inflammation.
Discharge, tearing.
Signs of trauma.
Foreign body.
Evert the eyelid if possible
foreign body but nil seen on
external exam.
Everting the Eyelid
Give local anaesthetic eye drops prior.
Ask the patient to look down throughout.
Press on the upper eyelid with cotton bud.
Rotate eyelid upwards over cotton bud.
CAP 29 HAP 32 Stephen Foley 11/10/2016
Slit Lamp Examination
- Forehead on headrest, chin on chinrest.
- Adjust height so you/patient comfortable.
- Adjust beam width/light colour with knob
above eyepieces.
- Focus by moving the joystick.
- Elevate/depress view by rotating joystick.
- Examine eyelashes, lids (and evert),
conjunctiva/sclera, cornea, anterior
chamber, iris, pupil and lens.
Tonometry
Palpating intraocular pressure by hand is
unreliable but can give a vague impression.
Apply the point of the tonometer to the
eyelid with gentle pressure.
Take three readings.
Many departments have no tonometer and
if you are unsure how to use it may be best
to leave this to the ophthalmologist.
Fundoscopy
Do not dilate the pupil if head injury or iris trauma.
Red reflex.
Optic disc - swelling, pallor
Macula
Retina and vessels
Fluorescein
Pools in corneal defects.
Defects green with blue light.
May help locating FB.
Stains clothes – catch spills!
CAP 29 HAP 32 Stephen Foley 11/10/2016
You might also like
- Assessment of Neurological SystemDocument26 pagesAssessment of Neurological SystemBatiao Camille Claire100% (1)
- Examination of AnimalDocument5 pagesExamination of Animaldharmachakra ComNo ratings yet
- SodaPDF Converted Precept 2Document6 pagesSodaPDF Converted Precept 2VINSMOKE RIKUNo ratings yet
- Clinical Skills: Cranial Nerve Examination: WWW - Osce-Aid - Co.ukDocument3 pagesClinical Skills: Cranial Nerve Examination: WWW - Osce-Aid - Co.ukssNo ratings yet
- Visual SystemDocument5 pagesVisual SystemMahmoud AbouelsoudNo ratings yet
- Physical Assessment Extra NotesDocument12 pagesPhysical Assessment Extra NotesShane ann BragaNo ratings yet
- Cranial Nerve Examination OSCE GuideDocument26 pagesCranial Nerve Examination OSCE GuideAbdullah Basheer AL-AnaziNo ratings yet
- HEAD-TO-TOE-ASSESSMENT-TOOLDocument19 pagesHEAD-TO-TOE-ASSESSMENT-TOOLJeah Mae CastroNo ratings yet
- 7 Detailed Cranial Nerve ExamDocument3 pages7 Detailed Cranial Nerve Exambsm8gf6szxNo ratings yet
- Cranial Nerve ExaminationDocument3 pagesCranial Nerve ExaminationtomodachiNo ratings yet
- Eye ExaminationDocument34 pagesEye ExaminationSashwini DheviNo ratings yet
- ProP Ophthalmic Examination Made EasyDocument5 pagesProP Ophthalmic Examination Made EasyRosario AyalaNo ratings yet
- Health Assessment - Midterm - Assessing The EyesDocument4 pagesHealth Assessment - Midterm - Assessing The Eyesaina marie templonuevoNo ratings yet
- Salcedo Ha Cu 7 Adult Assessment Eyes 24Document69 pagesSalcedo Ha Cu 7 Adult Assessment Eyes 24shaimonteverdeNo ratings yet
- L9 PediaDocument47 pagesL9 PediaNawaf AleanziNo ratings yet
- Week 3 or 4 Eye Assessment Health AssessmentDocument34 pagesWeek 3 or 4 Eye Assessment Health Assessmentaabbccss1.z71No ratings yet
- Ha Laboratory Midterm ExamDocument6 pagesHa Laboratory Midterm ExamMJ Jomoc ArejolaNo ratings yet
- Head to Toe Assessment Guide < 40 charsDocument22 pagesHead to Toe Assessment Guide < 40 charsNessa Layos MorilloNo ratings yet
- 1 Procedure Neurological Assessment (Cranial Nerves)Document7 pages1 Procedure Neurological Assessment (Cranial Nerves)Jonh Vincent DedoroNo ratings yet
- Ophthalmic Exam UpennDocument9 pagesOphthalmic Exam UpennlechamariaNo ratings yet
- Fundoscopy Tutorial: Slide 1Document26 pagesFundoscopy Tutorial: Slide 1SaraNo ratings yet
- Head To Toe AssessmentDocument21 pagesHead To Toe AssessmentZahra jane A.100% (1)
- Cranial NervesDocument2 pagesCranial NervesMARIA PALOMA MARTINEZ SENDRANo ratings yet
- Special Senses ActivityDocument8 pagesSpecial Senses ActivityJerene Denzil NacarNo ratings yet
- Osce 2Document5 pagesOsce 2George ahoy100% (1)
- Strabismus, Amblyopia & LeukocoriaDocument14 pagesStrabismus, Amblyopia & LeukocoriaMuhammad Naufal WidyatmakaNo ratings yet
- Complete Neurologic ExamDocument21 pagesComplete Neurologic ExamRaymond CruzNo ratings yet
- Visual Acuity: Opthalmology CEX StepsDocument5 pagesVisual Acuity: Opthalmology CEX StepsVanessa HermioneNo ratings yet
- 8 Part Eye Exam RevisedDocument17 pages8 Part Eye Exam RevisedpasambalyrradjohndarNo ratings yet
- Guide to Head-to-Toe Physical AssessmentDocument27 pagesGuide to Head-to-Toe Physical AssessmentLarmay dcsnNo ratings yet
- Cranial Nerve Assessment SheetDocument1 pageCranial Nerve Assessment SheetirmakrsekNo ratings yet
- Rabbit Eye Experiments FinalDocument6 pagesRabbit Eye Experiments FinalRenuka MoreNo ratings yet
- Cranial NerveDocument3 pagesCranial NerveMatty JolbitadoNo ratings yet
- Cranial Nerve Assessment: Nerve Name Function Test IDocument9 pagesCranial Nerve Assessment: Nerve Name Function Test IBecky Mariñas ReducaNo ratings yet
- Science Action Labs Health Science: Hands-On Science Activities Ready for Student UseFrom EverandScience Action Labs Health Science: Hands-On Science Activities Ready for Student UseNo ratings yet
- Examination of The Eye in The Emergency Room: Christopher Calandrella D.O - Pgy2Document104 pagesExamination of The Eye in The Emergency Room: Christopher Calandrella D.O - Pgy2Alexandra Mendoza100% (1)
- Neuro and Cranial Nerve Assessment GuideDocument1 pageNeuro and Cranial Nerve Assessment GuidepriyaNo ratings yet
- EARSEYESDocument93 pagesEARSEYESZen Gesner Kenneth G. EganaNo ratings yet
- Performing Physical Assessment of The EyeDocument14 pagesPerforming Physical Assessment of The Eyezyrine jhen100% (1)
- Physical Assessment (Normal Findings)Document31 pagesPhysical Assessment (Normal Findings)Rinki SinghNo ratings yet
- 8 Part Eye Exam REVISED PDFDocument16 pages8 Part Eye Exam REVISED PDFJerwin EstacioNo ratings yet
- Assessing Head and Neck ExamDocument4 pagesAssessing Head and Neck ExamElla RetizaNo ratings yet
- Cranial Nerve AsxDocument3 pagesCranial Nerve AsxRea Dominique CabanillaNo ratings yet
- Physical Assessment Guide of Head-To-ToeDocument9 pagesPhysical Assessment Guide of Head-To-Toeneleh gray100% (2)
- Neurological AssessmentDocument8 pagesNeurological AssessmentSachin ParamashettiNo ratings yet
- Skull, Scalp & Hair: Physical Assessment Is AnDocument10 pagesSkull, Scalp & Hair: Physical Assessment Is AnTrixie Al MarieNo ratings yet
- CN Nerves TestDocument6 pagesCN Nerves TestTosin FagbemiNo ratings yet
- NS Tests - MedicineDocument6 pagesNS Tests - Medicineangela mamauagNo ratings yet
- Neuro AssessmentDocument3 pagesNeuro AssessmentTori RolandNo ratings yet
- Language, Orientation, Memory, Attention Span and Calculation, LOCDocument7 pagesLanguage, Orientation, Memory, Attention Span and Calculation, LOCYessamin Paith RoderosNo ratings yet
- Equine ExamDocument85 pagesEquine Examياسر قاتل البزونNo ratings yet
- 06 EENT AssessmentDocument36 pages06 EENT AssessmentHerlinaNababanNo ratings yet
- TimRoot - Chapter 7 - Pediatric OphthalmologyDocument1 pageTimRoot - Chapter 7 - Pediatric OphthalmologyBaeyerNo ratings yet
- MED1 2.2 Techniques of Examination On Head and EyeDocument11 pagesMED1 2.2 Techniques of Examination On Head and Eyepraveena.pv1234No ratings yet
- Instruction: Check Under Correctly Done If Identified Skill Is Correctly Performed Incorrectly Done If Skill IsDocument12 pagesInstruction: Check Under Correctly Done If Identified Skill Is Correctly Performed Incorrectly Done If Skill IsSIR ONENo ratings yet
- 12 Cranial Nerves and AssessmentDocument10 pages12 Cranial Nerves and Assessmentapollo100% (17)
- Visual Acuity Toddler TestDocument21 pagesVisual Acuity Toddler TestDimsyafelNo ratings yet
- Examination of EyeDocument33 pagesExamination of EyeSumit YadavNo ratings yet
- Entropion, (Inverted Eyelid) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEntropion, (Inverted Eyelid) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- A Patient 'S Guide To Refractive SurgeryDocument7 pagesA Patient 'S Guide To Refractive SurgeryJon HinesNo ratings yet
- Fever: Central Nervous System ConditionsDocument14 pagesFever: Central Nervous System ConditionsthelordhaniNo ratings yet
- Baby Friendly Hospital Initiative (Bfhi)Document9 pagesBaby Friendly Hospital Initiative (Bfhi)Ankita BramheNo ratings yet
- BX42 ChipperDocument61 pagesBX42 ChipperwindoveranthonyNo ratings yet
- DM-PH&SD-GU17-HCKS2 - Health Requirements For Kids SalonsDocument13 pagesDM-PH&SD-GU17-HCKS2 - Health Requirements For Kids SalonsPraveenKatkooriNo ratings yet
- (Claim#) (Surname) (Firstname) : C1147 Psychology Services Counselling Extension ReportDocument4 pages(Claim#) (Surname) (Firstname) : C1147 Psychology Services Counselling Extension ReportDawn CasuncadNo ratings yet
- Parent Perspectives of Their Involvement in IEP Development For Children With AutismDocument11 pagesParent Perspectives of Their Involvement in IEP Development For Children With AutismGiselle ProvencioNo ratings yet
- The Benefits of Positive Emotions at WorkDocument4 pagesThe Benefits of Positive Emotions at WorkAgustina NadeakNo ratings yet
- Gingival Recession PerioDocument42 pagesGingival Recession PerioFourthMolar.com100% (3)
- UCLA Application Information Packet As of April 04 2014Document18 pagesUCLA Application Information Packet As of April 04 2014UCLA Center for Prehospital CareNo ratings yet
- NIOSH Hazardous DrugsDocument22 pagesNIOSH Hazardous DrugsjimstasonNo ratings yet
- Test Bank For Essentials of Pediatric Nursing 1st Edition Theresa KyleDocument13 pagesTest Bank For Essentials of Pediatric Nursing 1st Edition Theresa KyleAnthonyRiveraqion100% (33)
- Raise Organic HogsDocument122 pagesRaise Organic HogsDanny R. Salvador100% (2)
- Nutritious Philippine Herbs Combat MalnutritionDocument5 pagesNutritious Philippine Herbs Combat MalnutritionPeter Pantazia0% (1)
- Kimberly Haynes, DMD - June 2016 Remedial Plan Issued by Texas State Board of Dental ExaminersDocument1 pageKimberly Haynes, DMD - June 2016 Remedial Plan Issued by Texas State Board of Dental ExaminersDentist The MenaceNo ratings yet
- Review Questions DRUGSDocument7 pagesReview Questions DRUGSjoy LoretoNo ratings yet
- HKGC Booklet FinalDocument95 pagesHKGC Booklet FinalAtik Badshah SHAIKHNo ratings yet
- The History of Grandmothers in The African American Community - Jillian JimenezDocument30 pagesThe History of Grandmothers in The African American Community - Jillian JimenezClemente PennaNo ratings yet
- Cancer Screening Call ScriptDocument2 pagesCancer Screening Call Scriptjhez tel100% (1)
- Nutrition Tips For Someone With COPD: COPD Foundation's Slim Skinny Reference Guide (SSRG)Document16 pagesNutrition Tips For Someone With COPD: COPD Foundation's Slim Skinny Reference Guide (SSRG)Priscilia FooNo ratings yet
- DRUG STUDY: Lidocaine, Methocarbamol, MetaxaloneDocument28 pagesDRUG STUDY: Lidocaine, Methocarbamol, MetaxaloneLucas, Darah Angelica A.No ratings yet
- Cancer QuizDocument7 pagesCancer QuizJoshua Flores Fernan100% (1)
- Capstone SolutionDocument1 pageCapstone Solutiondave magcawasNo ratings yet
- Majalah ISO Ed. 132 PDFDocument27 pagesMajalah ISO Ed. 132 PDFFranki Hari M100% (1)
- Gronning 2017 CloningDocument4 pagesGronning 2017 CloningKlyde Orly R. YusoresNo ratings yet
- Social Work ResearchDocument15 pagesSocial Work ResearchSuresh Murugan78% (9)
- Loc BFRDocument6 pagesLoc BFRapi-290917332No ratings yet
- Rusty Moore Visual Impact For WomenDocument34 pagesRusty Moore Visual Impact For Womenchrisie00757% (7)
- Effect of Prone Positioning on Respiratory Rate and Oxygen Saturation in Infants with RDSDocument3 pagesEffect of Prone Positioning on Respiratory Rate and Oxygen Saturation in Infants with RDSAgustina VivoNo ratings yet