Professional Documents
Culture Documents
TRAQUEOSTOMIA. Decanulacon
Uploaded by
Camilla BahamondeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
TRAQUEOSTOMIA. Decanulacon
Uploaded by
Camilla BahamondeCopyright:
Available Formats
Tracheostomy Decannulation
Kent L Christopher MD RRT
Introduction
Decannulation Decision Making
Deflated-Cuff Tracheostomy Occlusion Procedure
Benefits of Decannulation
Protocol-Guided Decannulation
Physiologic Effects of Decannulation
Pre-Decannulation Steps
Summary
The respiratory therapist plays an integral role in tracheostomy tube decannulation. Removal of the
tracheostomy tube should be considered only if the original upper-airway obstruction is resolved,
if airway secretions are controlled, and if mechanical ventilation is no longer needed. Predictors of
success include ability to produce a vigorous cough and the absence of aspiration. Tracheostomy
decannulation requires caution, particularly following a prolonged period of tracheostomy use. The
tracheostomy tube decannulation process is well suited for therapist-implemented protocols. Key
words: tracheostomy, decannulation, acute respiratory failure, secretion clearance, airway care, artifi-
cial airways. [Respir Care 2005;50(4):538 –541. © 2005 Daedalus Enterprises]
Introduction ability to produce a vigorous cough and the absence of
aspiration. Heffner1 notes that the presence of purulent
The respiratory therapist (RT) plays an integral role in secretions may warrant prudent antibiotic therapy. Aspi-
tracheostomy-tube decannulation. No matter how fre- ration can be obvious and overtly disastrous or chronic and
quently a given procedure is performed, it is of great value subtle. It may be helpful to check for a gag reflex prior to
to have the essential elements distilled to a very practical, decannulation. However, up to 20% of normal individuals
simple, and straightforward approach. An article by Hef- may have no gag reflex.1 The absence of this reflex does
fner1 presents criteria for tracheostomy tube decannulation not reliably predict abnormal swallow. A formal swallow
and practical measures to prevent failure. In brief, it is evaluation should be considered, particularly in patients
advised that one consider decannulation only if the origi- with prolonged tracheostomy or those at high risk for as-
nal upper-airway obstruction is resolved, if airway secre- piration.
tions are controlled, and if mechanical ventilation is no
longer needed. Additional predictors of success include Decannulation Decision Making
The decision process prompting decannulation for man-
Kent L Christopher MD RRT is affiliated with the Division of Pulmonary
agement of an acute upper-airway obstruction is very dif-
Sciences and Critical Care Medicine, Department of Medicine, Univer-
sity of Colorado Health Sciences Center, Denver, Colorado. ferent than assessment for removal of a tracheostomy tube
that was placed for long-term management of complex
Kent L Christopher MD RRT presented a version of this paper at the 20th airway abnormalities or for prolonged mechanical venti-
Annual New Horizons Symposium at the 50th International Respiratory
lation (PMV). For example, if tracheostomy was performed
Congress, held December 4–7, 2004, in New Orleans, Louisiana.
for an acute upper-airway obstruction, it may be prudent
Correspondence: E-mail: drkchristopher@comcast.net. for the patient to have an upper-airway endoscopic examina-
538 RESPIRATORY CARE • APRIL 2005 VOL 50 NO 4
TRACHEOSTOMY DECANNULATION
tion to confirm that the abnormality has substantially im- marize, the patient should be on an appropriate monitoring
proved or resolved. If a patent airway is reestablished, prompt device, with pulse oximetry as the recommended mini-
decannulation and appropriate post-procedure monitoring and mum. The procedure should be explained to the patient.
clinical assessment may be the best intervention. Following full deflation of the tracheostomy-tube cuff, a
Examples of acute upper-airway obstruction include life- gloved finger briefly occludes the tracheostomy-tube open-
threatening aspirated foreign body, angioedema. and epi- ing and the clinician carefully notes if breathing through
glottitis. Occasionally, what seemed to be an acute airway the mouth and/or nose is present. The clinician should
obstruction due to an organic etiology may subsequently observe for objective signs of respiratory distress and en-
be attributed to a nonorganic, psychological disorder. Pa- courage phonation. For patients who have not breathed
tients with psychogenic vocal-cord dysfunction may ap- through the upper airway for a number of weeks or months,
pear to have an acute life-threatening organic upper-air- it is relatively common for these individuals to have con-
way obstruction2 that prompts emergency tracheotomy. cern about a different breathing sensation. This should be
Vocal-cord dysfunction should be considered when no or- clinically distinguished from distress due to substantial
ganic etiology is identified and post-tracheotomy endo- upper-airway obstruction. The presence of stridor, mini-
scopic examination is remarkably normal. Clinical expe- mal or absent breath sounds upon auscultation over the
rience indicates that tracheotomy is unnecessary in patients upper neck, absence of airflow at the nose or mouth, su-
with psychogenic vocal-cord dysfunction, and patients tend praclavicular or intercostal retractions, labored breathing,
to have difficulty during the decannulation process with diaphoresis, and prolonged inspiratory phase are signs con-
worsening vocal-cord dysfunction signs and symptoms. sistent with potential severe upper-airway obstruction. If
The clinician should be familiar with the distinct endo- findings suggest upper-airway obstruction, promptly re-
scopic glottic findings seen during episodes of vocal-cord turn the patient to breathing through the tracheostomy tube,
dysfunction.2 with appropriate supplemental humidified oxygen or me-
Decannulation of patients with prolonged tracheostomy chanical ventilatory support. Endoscopic examination
is not as straightforward as tube removal following a re- should identify the site of obstruction. If no lesions are
solved acute upper-airway obstruction. Patients recently present, consider whether the tube may be too large for the
weaned from PMV have prolonged critical illness, multi- trachea to allow for adequate flow through the upper air-
ple medical comorbidities, and a marginal respiratory sta- way; a trial following tracheostomy-tube change may be in
tus. During the post-mechanical-ventilation period, patients order.
are predisposed to respiratory muscle fatigue, abnormal
ventilatory drive, and another episode of respiratory fail-
Benefits of Decannulation
ure. Individuals with a long-term tracheostomy are at risk
for upper-airway obstruction due to complications of tra-
cheostomy. The numerous upper-airway abnormalities en- Though decannulation is not without some risk, there
countered with tracheostomy have been presented by Ep- are clear-cut benefits to tracheostomy-tube removal. The
stein in the preceding paper.3 Upper-airway complications tracheostomy tube is a foreign body that may cause bron-
of tracheostomy or prior endotracheal intubation may make chorrhea or excessive cough. Tracheostomy tubes may
it very difficult to safely decannulate the tracheostomy impair swallowing. Normal physiology requires that the
tube. Under certain clinical conditions it may not be wise trachea is elevated during the swallowing maneuver, al-
to even consider decannulation. Additionally, there may lowing the larynx to abut against the epiglottis, thus pre-
be upper-airway abnormalities that were initially unappre- venting aspiration of food or secretions. The presence of a
ciated or unrecognized at the time of decannulation. Pa- tracheostomy tube impairs normal tracheal elevation dur-
tients may subsequently experience life-threatening air- ing swallowing.
way compromise requiring emergency reinsertion of the Diverting breathing away from the upper airway and
tracheostomy tube. The clinician must have a high index through the tracheostomy lumen has substantial deleteri-
of suspicion for these disorders. Routine endoscopic eval- ous effects. The physiologic benefit of pursed-lips breath-
uation has been advised by some,4 and surgical or medical ing is eliminated. The vocal cords are bypassed, and there
interventions are often necessary for identified airway ob- is no “laryngeal blast” to facilitate effective cough. Fur-
struction prior to considering decannulation. thermore, the larynx is an important physiologic regulator
of breathing. Partial closure of the vocal cords maintains a
Deflated-Cuff Tracheostomy Occlusion Procedure subglottic pressure referred to as “physiologic PEEP” (pos-
itive end-expiratory pressure). Partial glottic closure has
Over the years, RTs have found the deflated-cuff tra- been shown to occur in patients with intrathoracic airflow
cheostomy occlusion procedure to be a practical bedside obstruction5,6 and appears to be a compensatory mecha-
screen for evaluation for upper-airway obstruction. To sum- nism during bronchoconstriction.6 Similarly, subglottic
RESPIRATORY CARE • APRIL 2005 VOL 50 NO 4 539
TRACHEOSTOMY DECANNULATION
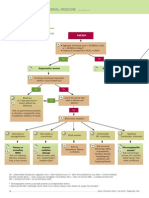
pressure may improve the swallowing mechanism and re- Table 1. Protocol Criteria for Tracheostomy Decannulation Attempt
duce the risk for aspiration. Following Successful Liberation From Prolonged
Mechanical Ventilation
Most importantly, patients are unable to speak when the
tracheostomy tube bypasses the larynx. There are pro- Absence of distress and stable arterial blood gases on prolonged
found consequences of inability to speak. Aphonia pre- mechanical ventilation for 5 days
sents a barrier to the patient’s participation in care. Care is Stable clinical condition indicated by factors such as:
further compromised when the patient is unable to express -Hemodynamic stability
symptoms that would normally prompt further investiga- -Absence of fever, sepsis, or active infection
tion or intervention. Clinical assessment is compromised -PaCO2 ⬍ 60 mm Hg
when mental status cannot be appropriately assessed be- Normal endoscopic examination or revealing stenotic lesions
occupying ⬍ 30% of the airway
cause of the lack of verbal communication. Inability to
Absence of delirium or psychiatric disorders
speak impairs informed consent and patient advance di- Adequate swallowing evaluated by gag reflex, blue dye, and video
rective. The inability to speak brings a sense of isolation, fluoroscopy
frustration, anxiety, and depression, particularly in patients Patient able to expectorate on request
recovering from PMV who have been unable to speak for Maximum expiratory pressure ⱖ 40 cm H2O
weeks to months. Related agitation is often managed with
(Adapted from Reference 9.)
anxiolytics or hypnosedatives, which can have a negative
impact on rehabilitation and recovery.
Protocol-Guided Decannulation not customarily used in the United States, the Minitrach is
a device that is not intended for ventilation, but allows
Evidence-based guidelines have confirmed the benefit tracheal access for periodic suctioning. The Minitrach was
of weaning protocols.7 RT-implemented weaning proto- removed if suctioning requirements became ⬍ 2 times per
cols have been shown to be efficacious in weaning trache- day and if the patient was able to demonstrate spontaneous
ostomized patients from PMV.8 Intuitively it would seem expectoration through the mouth. The alternative path of
that protocol implementation for decannulation from long- the protocol underlines Heffner’s1 emphasis on the impor-
term tracheostomy may have value. Ceriana et al9 con- tance of the mechanical requirements to generate effective
ducted a prospective outcomes evaluation of implementa- cough and the ability to clear secretions.
tion of a protocolized decisional flow chart for tracheostomy
decannulation following successful liberation from PMV. Physiologic Effects of Decannulation
Remarkably, reintubation rate at 3 months was only 3%.
Over 18 months, a total of 108 patients with diverse There are a few studies that have evaluated the physi-
causes for ventilator dependence were evaluated. Charac- ologic effects of decannulation in tracheostomized patients.
teristic of this chronically critically ill PMV population,7 Chadda et al10 evaluated the physiology of decannulation
60% had comorbidities, only 60% successfully weaned in 9 neuromuscular tracheostomized patients. Selection of
from PMV, and 33% died while on PMV. Decannulation patients with neuromuscular disease was an important part
failures could be attributed to uncontrolled secretions and of the study design, because confounding factors due to
severe glottic stenosis. Table 1 has been adapted to present lung, cardiac disease, or upper-airway obstruction were
the Ceriana et al9 criteria for consideration for decannula- excluded. Breathing through the tracheostomy tube was
tion. compared to breathing through the upper airway, with the
According to the Ceriana protocol, if all criteria were tracheostomy tube lumen occluded (similar to the common
met, the tracheostomy tube was downsized to a tracheos- practice of cuff deflation with tracheostomy-tube capping
tomy tube with an inner diameter of ⱕ 6 mm. The patient as a trial prior to decannulation). Unfenestrated 7-mm or
was then decannulated after 4 days if arterial blood gases 8-mm inner diameter tracheostomy tubes were used. Flow,
showed a pH of ⬎ 7.35 with ⬍ 5% increase in PaCO2. esophageal pressure, expired gas analysis, and arterial blood
Ceriana et al realized that certain patients might meet gas results were measured. Compared to breathing through
most criteria to be considered for tracheostomy decannu- the tracheostomy tube, results showed an increased tidal
lation, but might have risk indicators that would qualify volume with breathing through the upper airway (330 mL
for decannulation by an alternative path in the protocol. and 400 mL, respectively) and that ventilation increase
The 2 indicators were poor cough reflex and ability to was due to an increase in physiologic dead space (156 mL
generate only a marginal peak expiratory pressure, be- and 230 mL, respectively). There were no changes in up-
tween 20 and 40 cm H2O. The protocol alternative path per-airway resistance, dynamic pulmonary compliance, or
called for interim placement of the Minitrach (Portex, intrinsic positive end-expiratory pressure when patients
Hythe, United Kingdom) for at least one week. Though were switched from breathing through the tracheostomy
540 RESPIRATORY CARE • APRIL 2005 VOL 50 NO 4
TRACHEOSTOMY DECANNULATION
tube to breathing through the upper airway. However, the upper airway and through the tracheostomy. The trial of a
change from tracheostomy-tube breathing to upper-airway “functional decannulation” may not be achieved, and the
breathing resulted in increased work of breathing (6.9 to clinician may be inappropriately reassured that speech and
9.1 J/min), transdiaphragmatic pressure (10.4 to 12.5 cm absence of distress confirm the presence of a patent upper
H2O), diaphragmatic pressure-time product (214 to 271 airway.
cm H2O 䡠 s/L), and oxygen uptake (206 to 229 mL/min).
This study suggests that tracheal decannulation, in the ab- Summary
sence of underlying upper-airway obstruction, results in
increased dead space, with no other detectable loading. The skills and knowledge of the RT are essential to the
The authors conclude that work of breathing may be in- spectrum from airway management through mechanical
creased by ⬎ 30%, due to higher ventilatory requirements. ventilation and tracheostomy decannulation. As we start,
so must we finish. Based upon experience with liberation
Pre-Decannulation Steps from mechanical ventilation, tracheostomy decannulation
appears to be ideally positioned for RT-implemented pro-
For patients with long-term tracheostomy, it is common tocols. Additional guidance by scientific insight is sorely
practice to take an intermediate step prior to completely needed. Involvement of the RT in a team approach to
removing the tracheostomy tube. The interim trial of a scientific study of current and new approaches to trache-
“physiologic decannulation” allows the clinician additional ostomy decannulation is likely to improve quality of care
time to monitor cough effectiveness, swallow, voice qual- and outcomes.
ity, and the patient’s ability to adequately breathe through
the upper airway.
Heffner1 describes the use of the tracheostomy button. REFERENCES
Others have been proponents of use of the capped fenes- 1. Heffner JE. The technique of weaning from tracheostomy: criteria
trated tube with the cuff deflated. Hussy and Bishop11 for weaning; practical measures to prevent failure. J Crit Illn 1995;
studied an adult trachea and mechanical lung model to 10(10):729–733.
compare pressures required to breathe, utilizing a number 2. Christopher KL, Wood RP 2nd, Eckert RC, Blager FB, Raney RA,
Souhrada JF. Vocal-cord dysfunction presenting as asthma. N Engl
of different-size fenestrated and unfenestrated, cuff- J Med 1983;308(26):1566–1570.
deflated tracheostomy tubes. Though still a matter of clin- 3. Epstein SK. Anatomy and physiology of tracheostomy. Respir Care
ical opinion, the authors concluded that the model sug- 2005;50(4):476–482.
gested that effort to breathe in the absence of a fenestrated 4. Lee TS, Wu Y. Bedside fiberoptic bronchoscopy for tracheostomy
tube may be substantial. It was also the authors’ opinion decannulation. Respir Med 1995;89(8):571–575.
5. Higenbottam T, Payne J. Glottis narrowing in lung disease. Am Rev
that, unless the tube was small (eg, 4 mm inner diameter), Respir Dis 1982;125(6):746–750.
a fenestrated tube was recommended. The clinician must 6. Collet PW, Brancatisano T, Engel LA. Changes in the glottic apera-
be aware that granulation tissue or other tracheal abnor- ture during bronchial asthma. Am Rev Respir Dis 1983;128(4):719–
malities may obstruct the fenestrations, defeating the in- 723.
tended design. On occasion, abnormal tissue may herniate 7. MacIntyre NR, Cook DJ, Ely EW Jr, Epstein SK, Fink JB, Heffner
JE, et al; American College of Chest Physicians; American Associ-
through the fenestrations, resulting in trauma and diffi- ation for Respiratory Care; American College of Critical Care Med-
culty in inner-cannula insertion and removal, as well as icine. Evidence-based guidelines for weaning and discontinuing ven-
subsequent bleeding. tilatory support: a collective task force facilitated by the American
Another common practice is to use a downsized, cuff- College of Chest Physicians; the American Association for Respi-
deflated, unfenestrated or fenestrated tube with a standard ratory Care; and the American College of Critical Care Medicine.
Chest. 2001;120(6 Suppl):375S–395S.
cap as an intermediate trial prior to decannulation. The 8. Scheinhorn DJ, Chao DC, Stearn-Hassenpflug M, Wallace WA. Out-
clinician should be aware that a downsized tube has a comes of post-ICU mechanical ventilation: a therapist-implemented
smaller outer diameter and inner diameter and is designed weaning protocol. Chest 2001;119(1):236–242.
for a patient of smaller stature, with respect to tube length, 9. Ceriana P, Carlucci A, Navalesi P, Rampulla C, Delmastro M, Piaggi
curvature, and inflated-cuff dimensions. Additionally, un- G, et al. Weaning from tracheotomy in long-term mechanically ven-
tilated patients: feasibility of a decisional flowchart and clinical out-
like thermoplastics that conform to the contour of the pa- come. Intensive Care Med 2003;29(5):845–848.
tient’s airway, smaller tubes with fixed and rigid plastics 10. Chadda K, Louis B, Benaı̈ssa L, Annane D, Gajdos P, Raphaël JC,
designed for patients with larger stature may present prob- Lofaso F. Physiological effects of decannulation in tracheostomized
lems. patients. Intensive Care Med 2002;28(12):1761–1767.
An additional interim step to decannulation is the speak- 11. Hussey JD, Bishop MJ. Pressures required to move gas through the
native airway in the presence of a fenestrated vs a nonfenestrated
ing valve, previously discussed by Hess.12 Though speech tracheostomy tube. Chest 1996;110(2):494–497.
and subglottic pressure are restored, the low-resistance 12. Hess DR. Facilitating speech in the patient with a tracheostomy.
valve may preferentially divert inspiration away from the Respir Care 2005;50(4):519–525.
RESPIRATORY CARE • APRIL 2005 VOL 50 NO 4 541
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5796)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Urology Lecture 7. UTIDocument99 pagesUrology Lecture 7. UTIAwani PatelNo ratings yet
- Multimodal PDFDocument11 pagesMultimodal PDFCarlos CahuayaNo ratings yet
- Circular No. 041 - COVID-19 Patient RecoveryDocument1 pageCircular No. 041 - COVID-19 Patient RecoveryJerry OchocoNo ratings yet
- Schizophrenia Case StudyDocument3 pagesSchizophrenia Case StudyKumar Suryavanshi100% (1)
- Customer List Ulfah Jabar 1Document10 pagesCustomer List Ulfah Jabar 1MIhsanBudimanNo ratings yet
- Paul Farmer, Pioneer of Global Health, Dies at 62Document3 pagesPaul Farmer, Pioneer of Global Health, Dies at 62ALFINo ratings yet
- Hydatidiform MoleDocument18 pagesHydatidiform Molejean thereseNo ratings yet
- NCM 116 Medical SurgicalDocument9 pagesNCM 116 Medical SurgicalIvan A. EleginoNo ratings yet
- ACL Repair-HAMSTRING Graft ProtocolDocument4 pagesACL Repair-HAMSTRING Graft ProtocolmishbehavedNo ratings yet
- Appendix For Pgmee Vol 3 PDFDocument45 pagesAppendix For Pgmee Vol 3 PDFeeyas MachiNo ratings yet
- Anemia - Pato ClinicaDocument2 pagesAnemia - Pato ClinicaJean Pierre Loli PinNo ratings yet
- Axa Emedic: 1. 1 What Is This Product About?Document4 pagesAxa Emedic: 1. 1 What Is This Product About?Afiq de WinnerNo ratings yet
- Eating Disoder Anorxia NervosaDocument12 pagesEating Disoder Anorxia Nervosaapi-315334709No ratings yet
- 6e - Thyroid Dysfunction in Pregnancy A Literature Review (Perbaiki Dafpus)Document5 pages6e - Thyroid Dysfunction in Pregnancy A Literature Review (Perbaiki Dafpus)KESEBELASAN RESOG 2023No ratings yet
- Organizational Chart PDFDocument1 pageOrganizational Chart PDFCandy San DiegoNo ratings yet
- Delusional Jealusy - FullDocument17 pagesDelusional Jealusy - FullnicolasNo ratings yet
- OCD Skin Picking Disorder Fact SheetDocument2 pagesOCD Skin Picking Disorder Fact SheetboobusNo ratings yet
- Medication Error Reporting Form Pindaan 2Document2 pagesMedication Error Reporting Form Pindaan 2hanselMD100% (2)
- S. NO. Name & Address of The Hospital CityDocument34 pagesS. NO. Name & Address of The Hospital CityThe Indian Express33% (3)
- Cranial Mri With GadoliniumDocument2 pagesCranial Mri With GadoliniumPolo Gabriel MendiolaNo ratings yet
- Lesson 6 Alternative TreatmentDocument10 pagesLesson 6 Alternative Treatmentkim chi 04No ratings yet
- HIS Patient Visits ZFC-ZM427Document2 pagesHIS Patient Visits ZFC-ZM427Hazem NusiratNo ratings yet
- Adverse Drug ReactionDocument24 pagesAdverse Drug ReactionGopal pokhrelNo ratings yet
- Final Position Paper - Legalization of Marijuana in The PhilippinesDocument7 pagesFinal Position Paper - Legalization of Marijuana in The PhilippinesJhelboy BarabadNo ratings yet
- What Are The Different Types of Stress?Document2 pagesWhat Are The Different Types of Stress?Полина КосьминаNo ratings yet
- Science and TechnologyDocument8 pagesScience and TechnologyJoven Cubio CrystalNo ratings yet
- Biomedicines 10 00675Document17 pagesBiomedicines 10 00675tasialalalaNo ratings yet
- Pengaruh Terapi Cermin Terhadap Kemampuan Gerak Pada Pasien Stroke Di Wilayah Kerja Puskesmas Kumpulan Kabupaten Pasaman Tahun 2018Document5 pagesPengaruh Terapi Cermin Terhadap Kemampuan Gerak Pada Pasien Stroke Di Wilayah Kerja Puskesmas Kumpulan Kabupaten Pasaman Tahun 2018CachaNo ratings yet
- Metabical Harvard Case StudyDocument56 pagesMetabical Harvard Case StudyVaibhav Singh100% (3)
- Fracture of Radius, Ulna, and HumerusDocument21 pagesFracture of Radius, Ulna, and HumeruspunikaNo ratings yet