Professional Documents
Culture Documents
Oral Manifestations Associated With SARS-COV-2: A Literature Review
Oral Manifestations Associated With SARS-COV-2: A Literature Review
Uploaded by
Alexandru Codrin-IonutOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oral Manifestations Associated With SARS-COV-2: A Literature Review
Oral Manifestations Associated With SARS-COV-2: A Literature Review
Uploaded by
Alexandru Codrin-IonutCopyright:
Available Formats
Oral manifestations associated with SARS-
COV-2: A literature review
Manifestaciones orales asociadas a SARS-COV-2: Revisión de la literatura
Manifestações orais associadas ao SARS-COV-2: Revisão da literatura
Natalia Sandoval-Gómez1 0000-0003-3120-4076
Tamara Needham-Torres1 0000-0002-9644-572X
Gisella Vásquez-Canales1 0000-0001-6401-5170
Ana María Salazar-Roa2 0000-0003-3536-9310
DOI: 10.22592/ode2021n37e304
Abstract
Objective: Identify the main oral manifestations associated with COVID19 and describe
their location in the oral cavity.
Methods: The literature search was conducted in PubMed, Medline, LILACS, LIVIVO,
Web of Science, and SciELO. The following words were searched for: oral mucosa, oral mu-
cosa lesion, oral manifestations, COVID-19, and SARS-CoV-2. Duplicate articles were elimi-
nated, and the pieces were shortlisted. Finally, inclusion and exclusion criteria were applied.
Results: This study included 47 articles. The main oral manifestations in patients with
COVID-19 are taste disorders, xerostomia, ulcers, vesicles, and others located in different
areas of the oral mucosa.
Conclusions More studies are needed to determine the potential oral etiopathogenesis of
SARS-CoV-2. Moreover, dentists play a significant role in the multidisciplinary and tele-
medicine team.
Keywords: COVID-19, oral manifestation, oral mucosa.
1 School of Dentistry, Universidad de Concepción, Chile. n475sg@gmail.com
2 Department of Pathology and Diagnostics, School of Dentistry, Universidad de Concepción, Chile
Received on: 15/Jan/2021 - Accepted on: 22/Mar/2021
Oral manifestations associated with SARS-COV-2: A literature review
1
Resumen Resumo
Objetivo: Identificar las principales mani- Objetivo: Identificar as principais manifes-
festaciones y describir su ubicación en la ca- tações e descobrir sua ubiquação na cavida-
vidad oral en pacientes COVID-19. de oral em pacientes com COVID-19.
Métodos: Se utilizaron las bases de da- Método: Foram utilizadas as bases de da-
tos PubMed, Medline, LILACS, LIVIVO, dos PubMed, Medline, LILACS, LIVIVO,
Web of Science y SciELO; utilizando los Web of Science e SciELO; utilizando os ter-
términos de búsqueda oral mucosa, oral mu- mos de pesquisa oral mucosa, oral mucosa
cosa lesion, oral manifestations, COVID-19 lesion, oral manifestations, COVID-19 e
y SARS-CoV-2. Se eliminaron duplicados, SARS-CoV-2. Duplicadas foram removi-
luego se realizó preselección de artículos, y das, depois uma pré-seleção de artigos foi
finalmente se aplicaron los criterios de in- feita, e finalmente os critérios de inclusão e
clusión y exclusión. exclusão foram aplicados.
Resultados: Se seleccionaron 47 publica- Resultados: Foram selecionadas 47 publi-
ciones, encontrando manifestaciones orales cações, encontrando manifestações orais em
en pacientes COVID-19 tales como altera- pacientes com COVID-19, tais como alte-
ción en gusto, xerostomía, úlceras, vesículas, rações no paladar, xerostomia, ulcerações,
entre otras; ubicándose en diferentes áreas vesículas, entre outros; localizando-as em
de la mucosa oral. diferentes áreas da mucosa oral.
Conclusiones: Se necesitan más estudios Conclusão: São precisos mais estudos pra
para vislumbrar la posible etiopatogenia a vislumbrar a possível etiopatogenia a nível
nivel oral del SARS-CoV-2. Además, se des- oral do SARS-CoV-2. Ademais, destaca-se o
taca el rol del odontólogo en el equipo mul- role do odontólogo na equipe multidiscipli-
tidisciplinario y en la teleconsulta. nar e na tele consulta.
Palabras clave: COVID-19, manifestación Palavras-chave: COVID-19, Manifestação
oral, mucosa oral. oral, mucosa oral.
2 Odontoestomatología 2021, 23 (38)
Introduction This literature review aims to identify the main
oral manifestations in patients with COVID19
The new infectious disease Coronavirus 2019 and to describe their location in the oral cavity.
(COVID-19), whose etiology is Severe Acute
Respiratory Syndrome Coronavirus 2 (SAR-
SCoV2), has had a massive impact worldwide Materials and methods
given its transmission rate, the resulting severe This literature review included the following
respiratory disorders, and the number of deaths stages: selecting the topic, defining the objec-
globally. All this significantly compromises tives, stating the inclusion and exclusion cri-
people’s quality of life.(1) Since it originated in teria, developing a work plan for the literature
Wuhan, China, the disease has reached a high search, selecting, and retrieving the studies that
infectivity rate. Projections estimate 47 million meet the criteria, collecting data to analyze and
cases worldwide and a mortality rate ranging summarize the results, and finally, drawing con-
from 3% to 12%. Over one million people clusions.
have died.(1-3) The search was conducted from 9 October to
The specific origin of the pandemic is not ful- 30 December 2020 in PubMed, Medline, LI-
ly understood. Although it is unclear how hu- LACS, LIVIVO, Web of Science, and SciELO.
mans acquired the disease, it is estimated that The search terms defined for the database
it involved an animal. Bats are the main wild search were: oral mucosa, oral mucosa lesion, oral
beings that are reservoirs for this type of virus. manifestations, COVID-19, and SARS-CoV-2,
A viral jump occurred between this animal and with boolean operators OR and AND. Results:
a human being in Wuhan, China, in November ((COVID-19) OR (SARS-CoV-2)) AND (mu-
2019.(2,4) cosa oral)), ((COVID-19) OR (SARS-CoV-2))
The main infection routes of SARSCoV2 AND (oral mucosa lesion)) and ((COVID-19)
in humans are saliva droplets expelled when OR (SARS-CoV-2)) AND (oral manifesta-
talking(1,2,5-9) or sneezing within a distance of tions)). The title and abstract were read to de-
two meters or when in contact with exposed termine relevance. Then, the full texts were read
surfaces.(2,6-9) Fifty percent of transmissions to determine if they met the inclusion and ex-
occur through exposure to asymptomatic peo- clusion criteria.
ple.(2) It is important to note that patients can The inclusion criteria covered articles published
transmit the infection up to two weeks after re- within the last two years that contain the search
covering from the disease.(4) terms in Spanish and English.
Current research shows that the SARSCoV2 The following articles were excluded: studies
virus invades human cells through the angio- conducted on animals, focused on treating
tensin-converting enzyme 2 (ACE2) receptor. patients infected with the SARSCoV2 virus,
(1,7,9-23)
In this way, cells with ACE2 receptor COVID19 patients without oral manifesta-
distribution can become hosts to the virus and tions, and those related to prevention and/or
cause an inflammatory response in adjacent biosafety measures that did not meet our ob-
organs and tissues, including the oral cavity.(1, jectives.
7,8,10,12,14, 16-19,21-28)
Oral manifestations associated with SARS-COV-2: A literature review
3
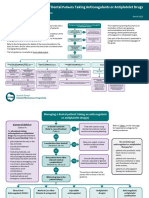
Figure 1. Flowchart of the article search, review, and selection process
Identification Number of records identified through database searches
Pubmed (n=174) Web of science (n=82)
LILACS (n=20) Medline (n=215)
LIVIVO (n=266) SciELO (n=4)
TOTAL (N=761)
Screening
Number of records after
removing duplicate citations
(n=363)
Total number of excluded
records (n=310)
Subject is not relevant (n=303)
Relevance The full text cannot be accessed
Number of records screened (n=7)
(n=53)
Number of full-text articles Number of full-text articles
evaluated for eligibility excluded
(n=53)
(n=6)
Inclusion Number of studies included in the
summary
(n=47)
Development The cases reported in the literature describe
heterogeneous lesions between patients and
Duplicate articles were discarded and studies even in the same patient.(10-13) What varies is
that met the inclusion and exclusion criteria the presentation, location, and size.(5,10,12,29)
were selected. The final selection included Oral manifestations have appeared in healthy
47 articles: 9 case reports, 1 case report with COVID-19 patients with no relevant medical
narrative literature review, 2 systematic re- history,(1,5,12,13,18,30-33) and in patients with un-
derlying conditions.(1,7,10,12,13,16,18,23,27-30,33-41)
views, 3 critical reviews, 9 narrative reviews,
The manifestations that are mentioned more
4 observational studies, and 19 letters to the frequently are taste disorders and ulcers, while
editor. In addition, information from one the least mentioned are pustules, glossitis, and
article and two websites was included in the geographic tongue. The main manifestations
introduction. found are described below (Table 1):
4 Odontoestomatología 2021, 23 (38)
Table 1: Oral manifestations reported in patients with COVID-19
Oral manifestation Type of publication References
5 case reports 30 references
Taste disorders 2 systematic reviews
7 narrative reviews (1,6-12,14,16-19,21-24,26,29,30,33,36,38,40-46)
2 critical reviews
10 letters to the editor
3 observational studies
1 case report with narrative literature review
1 case report 10 references
Burning sensation 3 narrative reviews
3 letters to the editor (6,8,12,18,27,36,39,41,44,47)
2 observational studies
1 case report with narrative literature review
2 case reports 12 references
Xerostomia 5 narrative reviews
1 critical review (5,6,8-10,16-18,24,29,36,47)
2 letters to the editor
2 observational studies
3 narrative reviews 5 references
Halitosis 2 letters to the editor (16,17,25,27,48)
4 case reports 15 references
Erythema 1 narrative review
1 systematic review (1,9-13,19,20,27,28,30,31,41,46,49)
3 critical reviews
4 letters to the editor
1 observational study
1 clinical case with narrative literature review
2 case reports 13 references
Petechias 4 narrative reviews
1 systematic review (1,5,9,11,13,15,17,18,20,26,27,31,41)
2 critical reviews
3 letters to the editor
1 clinical case with narrative literature review
2 case reports 11 references
Macules 1 narrative review
1 systematic review (10-13,17,19,20,26,29,41,47)
2 critical reviews
3 letters to the editor
1 observational study
1 clinical case with narrative literature review
3 case reports 17 references
Bulla/blisters 5 narrative reviews
1 systematic review (8,9,11,12,15-20,23,26,28,30,37,41,49)
3 critical reviews
3 letters to the editor
1 observational study
1 clinical case with narrative literature review
Oral manifestations associated with SARS-COV-2: A literature review
5
Oral manifestation Type of publication References
1 case report 4 references
Pustules 1 narrative review (13,27,31,32)
2 letters to the editor
6 case reports 30 references
Ulcers 6 narrative reviews (1,5,6,8-13,15-20,23,25-30,33-35,38,41,44-46)
1 systematic review
3 critical reviews
11 letters to the editor
2 observational studies
1 clinical case with narrative literature review
2 case reports 9 references
Desquamative gingivitis 3 narrative reviews (9,11,12,15,18,19,25,27,30)
1 systematic review
2 critical reviews
1 letter to the editor
3 narrative reviews 8 references
Salivary gland infection 2 critical reviews (8,19-21,24,28,41,45)
2 letters to the editor
1 clinical case with narrative literature review
Geographic tongue 2 references
2 letters to the editor (6,44)
3 narrative reviews 6 references
Glossitis 1 critical review (9,16,17,27,39.44)
2 letters to the editor
2 case reports 8 references
Candida 1 narrative review (5,6,10,11,17,39,41,46)
coinfection 1 systematic review
2 letters to the editor
1 observational study
1 clinical case with narrative literature review
4 case reports 14 references
Herpetiform lesions 3 narrative reviews (1,9-11,14,17,18,26,27,30,33,41,42,46)
1 systematic review
1 critical review
3 letters to the editor
1 observational study
1 clinical case with narrative literature review
The location of lesions is unspecific, but they mucosa). Lesions are also reported in the oral
appear mainly on the palate, tongue (mainly on mucosa, gingiva, and oropharynx (Table 2).
the dorsum), and also lip (inners side and semi
6 Odontoestomatología 2021, 23 (38)
Table 2: Localization of oral manifestations reported in patients with COVID-19.
Localization Type of publication References
3 case reports 22 references
Palate 4 narrative reviews (1,6,9,11-13,15,17,18,20,23,26-
1 systematic review 31,35,38,39,41,43)
2 critical reviews
10 letters to the editor
1 observational study
1 clinical case with narrative literature review
5 case reports 24 references
Tongue 2 narrative reviews (1,5,6,9-12,17,20,23,26-
1 systematic review 29,32,33,35,38,39,41,44-46,49)
2 critical reviews
11 letters to the editor
2 observational studies
1 clinical case with narrative literature review
6 case reports 23 references
Lip 4 narrative reviews (1,5,6,9,11,13,15,17,18,20,23,26-
1 systematic review 30,34,37,38,41,42,46,49)
2 critical reviews
7 letters to the editor
2 observational studies
1 clinical case with narrative literature review
2 case reports 10 references
Oral mucosa 2 narrative reviews (1,9,11,15,27,28,29,37,46.49)
1 systematic review
1 critical review
3 letters to the editor
1 observational study
1 case report 12 references (5,6,9,11,13,15,18,26-28,41,48)
Gum 3 narrative reviews
1 systematic review
1 critical review
5 letters to the editor
1 clinical case with narrative literature review
2 case reports 8 references
Oropharynx 2 narrative reviews (5,10,11,13,18,23,27,31)
1 systematic review
2 letters to the editor
1 observational study
Discussion administered for the treatment, or due to the
compromise and deterioration of the immune
Although oral mucosa lesions have been report- system,(1,6,9-12,15-17,26,27,33,34,36,38,41,45,50) which also
ed in patients infected with SARS-COV-2 vi- enables opportunistic infections.(5,6,9-11,15-18,25-
rus, it is believed that the cause is not the virus 28,33,36,39,41,42,45,48,50)
The most commonly re-
itself, but that the lesions would be secondary ported conditions are Candida albicans coin-
to the drugs(5,7,9-11,15,17,18,21,26,28,30,32,36,39,41,43,50) fections(5,6,10,11,17,39,41) and/or other viruses.
Oral manifestations associated with SARS-COV-2: A literature review
7
Despite these assump-
(1,9,10,16,17,27,33,41-43,45,46,50)
Additionally, saliva and nasal secretion could
tions, some of the studies reviewed theorize have high viral loads involved in these oral al-
about SARS-CoV-2’s vascular and thrombotic terations.(9,12)
effect on the oral mucosa.(6,9,12,15,17,23,27,29,34) Sim- Multiple authors agree on the need for
ilarly, oral mucosa lesions could be triggered by additional studies and thorough resear
factors such as stress.(5,8,18,22,25,26,32,37) ch(1,5,9-16,23,24,26,28-31,34-36,42,43,50) to determine the
We must emphasize the importance of the ACE2 pathogenic mechanisms of SARS-CoV-2 on
receptor, which is distributed in the cell mem- oral tissues and thus determine whether oral
brane of various organs and tissues, such as the mucosal lesions are directly or indirectly related
respiratory tract, the nervous system, the diges- to COVID19 progression.(1)
tive system, and the skeletal muscle.(1,9,13,23,24,27)
In the oral cavity, they appear in the oral(1,7,8,12,16-
19,21-27)
and gingival (7,14,21,23,24) mucosa epithelial Conclusion
cells. There is a strong presence in tongue ep- Oral manifestations in COVID-19 patients
ithelial cells (1,7-11,14,15,17,18,21,24,25,27,33,36) and sali- have been reported in multiple sites of the
vary glands.(1,9-12,16-20,24,27,36) Due to this high ex- oral cavity and are highly heterogeneous. The
pression,(8,9,11,14,15,18,19,21,22,24,25,27,33), the tongue is subject is so new that the prevalence of these
described as a susceptible organ.(14,19,25,33) Some manifestations is still unknown since the cas-
authors say that salivary glands(6,8,10,21,24,36) and es reported are few compared to the number
periodontal pockets(9,18,25,36,44) could act as virus of infected patients. Additionally, most cases
reservoirs. lack complementary tests, such as biopsies or
These ACE2 receptor would be the main SAR- hematology tests, which help identify the real
SCoV2 receptors, causing cells that distribute etiological agent. All this leaves unanswered
this receptor to trigger inflammatory reactions questions about the possible etiopathogenesis
in the associated organs and tissues.(1,9,10,13) or factors that might influence the develop-
Therefore, several authors state that this inter- ment of these lesions. Therefore, it is necessary
action in the tongue could explain taste disor- to conduct further research.
ders in patients with COVID19.(1,8-11,15-19,22,24) It Finally, it is essential to recognize that dentists
has also been said that the interaction between are crucial members of the health and telemed-
the virus and this receptor alters the function icine teams. Dentists should perform a careful
of oral keratinocytes and the epithelial lining oral examination to diagnose, treat, and control
of the salivary gland ducts after infection.(1) the pain caused by the lesions described.
References
1. Brandão TB, Gueiros LA, Melo TS, et al. Oral lesions in patients with SARS-CoV-2 infection:
could the oral cavity be a target organ? Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;S2212-
4403(20)31119-6.
2. World Health Organization. Coronavirus disease (COVID-19) pandemic. Situations Reports. EPI-
WIN Updates (nº 28 What we know about COVID-19). 2020 [Accessed November 05, 2020] Avai-
lable from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
3. Worldmeter [Homepage on the internet] COVID‐19 Coronavirus Pandemic. 2020 [Accessed October
21, 2020]. Available from: https://www.worldometers.info/coronavirus/.
8 Odontoestomatología 2021, 23 (38)
4. Ortiz-Prado E, Simbaña-Rivera K, Gómez-Barreno L, et al. Clinical, molecular, and epidemiological
characterization of the SARS-CoV-2 virus and the Coronavirus Disease 2019 (COVID-19), a compre-
hensive literature review. Diagn Microbiol Infect Dis. 2020;98(1):115094.
5. Corchuelo J, Ulloa FC. Oral manifestations in a patient with a history of asymptomatic COVID-19:
Case report. Int J Infect Dis. 2020;100:154-157.
6. Díaz Rodríguez M, Jimenez Romera A, Villarroel M. Oral manifestations associated with COVID-19.
Oral Dis. 2020; doi: 10.1111/odi.13555.
7. Orellana-Centeno JE, Morales-Castillo V, Guerrero SRN. Generalidades, manejos, cuidados y mani-
festaciones clínicas del SARS-CoV-2. Rev ADM. 2020;77(3):153-155.
8. Pant, B. COVID-19: Oral manifestations, impact and lessons for the future. Orthodontic Journal of
Nepal. 2020; 10(2), 52–54.
9. Parra–Sanabria EA, Bermúdez–Bermúdez M, Peña–Vega CP, Rueda–Jiménez A. Manifestaciones ora-
les y maxilofaciales asociadas a la COVID-19. a literature review Acta Odont Col. 2020; 10(Supl.
COVID-19): 60-80.
10. Amorim Dos Santos J, Normando AGC, Carvalho da Silva RL, De Paula RM, Cembranel AC, Santos-
Silva AR, Guerra ENS. Oral mucosal lesions in a COVID-19 patient: New signs or secondary mani-
festations? Int J Infect Dis. 2020;97:326-328.
11. Amorim Dos Santos J, Normando AGC, Carvalho da Silva RL, Acevedo AC, De Luca Canto G,
Sugaya N, Santos-Silva AR, Guerra ENS. Oral Manifestations in Patients with COVID-19: A Living
Systematic Review. J Dent Res. 2020;11:22034520957289.
12. Cruz Tapia RO, Peraza Labrador AJ, Guimaraes DM, Matos Valdez LH. Oral mucosal lesions in pa-
tients with SARS-CoV-2 infection. Report of four cases. Are they a true sign of COVID-19 disease?
Spec Care Dentist. 2020;1-6.
13. Ciccarese G, Drago F, Boatti M, Porro A, Muzic SI, Parodi A. Oral erosions and petechiae during
SARS-CoV-2 infection. J Med Virol. 2020;10.1002/jmv.26221.
14. Cornejo-Ovalle Marco, Espinoza-Santander Iris. COVID-19 y manifestaciones orales. Int. J. Odon-
tostomat. 2020;14( 4 ):538-539.
15. Maciel PP, Martelli Júnior H, Martelli DRB, Machado RA, Andrade PV, Perez DEC, et al. COVID-19
pandemic: oral repercussions and its possible impact on oral health. Pesqui Bras Odontopediatria Clín
Integr. 2020; 20(supp1):e0138.
16. Pedrosa MS, Sipert CR, Nogueira FN. Salivary glands, saliva and oral findings in COVID-19 infec-
tion. Pesqui Bras Odontopediatria Clín Integr. 2020; 20(supp1):e0104.
17. Nemeth-Kohanszky María Eugenia, Matus-Abásolo Carolina Paz, Carrasco-Soto Rolando Rafael. Ma-
nifestaciones Orales de la Infección por COVID-19. Int. J. Odontostomat. 2020; 14(4):555-560.
18. Gutiérrez Flores R, Zambrano Rodríguez G. Implicaciones bucales por COVID-19. Revisión de tema.
Odontol Sanmarquina.2020;23(4):419-23.
19. Capocasale G, Nocini R, Faccioni P, Donadello D, Bertossi D, Albanese M, Zotti F. How to deal with
coronavirus disease 2019: A comprehensive narrative review about oral involvement of the disease.
Clin Exp Dent Res. 2020; 10.1002/cre2.332.
20. Halboub E, Al-Maweri SA, Alanazi RH, Qaid NM, Abdulrab S. Orofacial manifestations of CO-
VID-19: a brief review of the published literature. Braz Oral Res 2020;34:e124.
21. Odeh ND, Babkair H, Abu-Hammad S, Borzangy S, Abu-Hammad A, Abu-Hammad O. COVID-19:
Present and Future Challenges for Dental Practice. Int J Environ Res Public Health. 2020;17(9):3151.
22. Abalo-Lojo JM, Pouso-Diz JM, Gonzalez F. Taste and Smell Dysfunction in COVID-19 Patients.
Annals of Otology, Rhinology & Laryngology. 2020; 129(10):1041-1042.
23. Katz J,Yue S. Increased odds ratio for COVID 19 in patients with recurrent aphthous stomatitis. J Oral
Pathol Med 2020;00:1-4.
24. Pastrian G. Presencia y expresión del receptor ACE2 (Target de SARS-CoV-2) en tejidos humanos y
cavidad oral. Posibles rutas de infección en órganos orales. Int. J. Odontostomat. 2020;14(4):501-507.
Oral manifestations associated with SARS-COV-2: A literature review
9
25. Riad A, Kassem I, Hockova B, Badrah M, Klugar M. Halitosis in COVID-19 patients. Spec Care
Dentist. 2020;1-3.
26. de Sousa FACG, Paradella TC. Considerations on oral manifestations of COVID-19. J Med Virol.
2021;93:667-668.
27. Iranmanesh B, Khalili M, Amiri R, Zartab H, Aflatoonian M. Oral manifestations of COVID ‐19
disease: A review article. Dermatologic Therapy. 2020;e14578.
28. Riad A, Klugar M, Krsek M. COVID-19-Related Oral Manifestations: Early Disease Features? Oral
Dis. 2020;00:1-3.
29. Soares CD, Carvalho RA, Carvalho KA, Carvalho MG, Almeida OP. Letter to Editor: Oral lesions in
a patient with COVID-19. Med Oral Patol Oral Cir Bucal. 2020;25(4):e563-e564.
30. Martín Carreras-Presas C, Amaro Sánchez J, López-Sánchez AF, Jané-Salas E, Somacarrera Pérez ML.
Oral vesiculobullous lesions associated with SARS-CoV-2 infection. Oral Dis. 2020;00:1-3.
31. Cebeci Kahraman F, Çaşkurlu H. Mucosal involvement in a COVID-19-positive patient: A case re-
port. Dermatol Ther. 2020;33(4):e13797.
32. Alzahrani MJ, Moussa MM, Alfaraj D. Acute Generalized Exanthematous Pustulosis After COVID-19
Infection: A Case Report From Saudi Arabia. Cureus. 2020;12(11):e11609.
33. Riad A, Kassem I, Hockova B, Badrah M, Klugar M. Tongue ulcers associated with SARS-CoV-2 in-
fection: A case series. Oral Dis. 2020;00:1-3.
34. Cebeci Kahraman F, Özen T, Elibol T. Lip necrosis in a patient with paroxysmal nocturnal hemoglobi-
nuria: Can it be triggered by COVID-19? J Cosmet Dermatol. 2020;19:3168–3170.
35. Ansari R, Gheitani M, Heidari F, Heidari F. Oral cavity lesions as a manifestation of the novel virus
(COVID-19). Oral Dis. 2020.
36. Sinjari B, D’Ardes D, Santilli M, Rexhepi I, D’Addazio G, Di Carlo P, Chiacchiaretta P, Caputi S,
Cipollone F. SARS-CoV-2 and Oral Manifestation: An Observational, Human Study. J Clin Med.
2020;9(10):3218.
37. Bakar Dertli̇oglu S. Skin rashes in COVID-19: A report of three cases. J Health Sci Med 2020; 3(4):
490-492.
38. Bemquerer LM, de Arruda JAA, Soares MPD, Mesquita RA, Silva TA. The oral cavity cannot be for-
gotten in the COVID-19 era: is there a connection between dermatological and oral manifestations?,
J American Academy Dermatol 2020; S0190-9622(20)33073-5.
39. Riad A, Gad A, Hockova B, Klugar M. Oral Candidiasis in Non-Severe COVID-19 Patients: Call for
Antibiotic Stewardship. Oral Surg. 2020; doi: 10.1111/ors.12561.
40. Passarelli PC, Lopez MA, Mastandrea Bonaviri GN, Garcia-Godoy F, D’Addona A. Taste and smell as
chemosensory dysfunctions in COVID-19 infection. Am J Dent. 2020;33(3):135-137.
41. Eghbali Zarch R, Hosseinzadeh P.COVID-19 from the perspective of dentists: A case report and brief
review of more than 170 cases. Dermatologic Therapy.2021;e14717.
42. Kitakawa D, Oliveira FE, Neves de Castro P, Carvalho LFCS. Short report - Herpes simplex lesion in
the lip semimucosa in a COVID-19 patient. Eur Rev Med Pharmacol Sci. 2020;24(17):9151-9153.
43. de Carvalho L, Kitakawa D, Cabral LAG. Oral lesions of herpes zoster in COVID-19 patients or truly
associated to the disease? Oral Dis. 2020;00:1-2.
44. Nuno-Gonzalez A, Martin-Carrillo P, Magaletsky K, Martin Rios MD, Herranz Mañas C, Artigas et
al. Prevalence of mucocutaneous manifestations in 666 patients with COVID-19 in a field hospital in
Spain: oral and palmoplantar findings. Br J Dermatol. 2020;184:158-185.
45. Abu-Hammad S, Dar-Odeh N, Abu-Hammad O. SARS-CoV-2 and oral ulcers: A causative agent or
a predisposing factor? Oral Dis. 2020;00:1-2.
46. Mascitti H, Bonsang B, Dinh A, Assan F, Perronne V, Leblanc T, Duran C, Bouchand F, Matt M, Le
Gal A, N’guyen Van Thanh J, Lanore A, Jacob L, Kiavue N, Siméon S, Bessis S, de Truchis P, Lan-
dowski S, Davido B, Moreau F, Rameix-Welti MA, Gault E, Gaillard JL, Roux AL, Sivadon-Tardy
V, Salomon E, El Sayed F, Carlier R, Emile JF, Perronne C, Bourgault-Villada I. Clinical Cutaneous
10 Odontoestomatología 2021, 23 (38)
Features of Patients Infected With SARS-CoV-2 Hospitalized for Pneumonia: A Cross-sectional Study.
Open Forum Infect Dis. 2020;7(11):ofaa394.
47. Biadsee A, Biadsee A, Kassem F, Dagan O, Masarwa S, Ormianer Z. Olfactory and Oral Manifesta-
tions of COVID-19: Sex-Related Symptoms-A Potential Pathway to Early Diagnosis. Otolaryngol
Head Neck Surg. 2020;163(4):722-728.
48. Patel J, Woolley J. Necrotizing periodontal disease: Oral manifestation of COVID-19. Oral Dis.
2020;00:1-2.
49. Aghazadeh N, Homayouni M, Sartori-Valinotti JC. Oral vesicles and acral erythema: report of a cuta-
neous manifestation of COVID-19. Int J Dermatol. 2020;59(9):1153-1154.
50. Ponce JB, Tjioe KC. Overlapping findings or oral manifestations in new SARS-CoV-2 infection. Oral
Dis. 2020;00:1-2.
Conflict of interest:
The authors declare no conflict of interest
Authorship contribution
1. Conception and design of study
2. Acquisition of data
3. Data analysis
4. Discussion of results
5. Drafting of the manuscript
6. Approval of the final version of the manuscript.
NSG has contributed in 1, 2, 3, 4, 5 and 6.
TNT has contributed in 3, 4, 5 and 6.
GVC has contributed in 2, 3, 4, 5 and 6.
AMSR has contributed in 3, 4, 5 and 6.
Acceptance note:
This article was approved by the journal’s editor, MSc Dr. Vanesa Pereira-Prado.
Oral manifestations associated with SARS-COV-2: A literature review
11
You might also like
- Natural Health Remedies From Prophets and Ahlul BaytDocument4 pagesNatural Health Remedies From Prophets and Ahlul BaytfirzangelNo ratings yet
- The Most Effective Evidence-Based Occupational Therapy Interventions For Adolescents With Bipolar Disorder A Systematic Literature ReviewDocument50 pagesThe Most Effective Evidence-Based Occupational Therapy Interventions For Adolescents With Bipolar Disorder A Systematic Literature ReviewAngela EnacheNo ratings yet
- MainDocument14 pagesMainJeancarlo Ore LazoNo ratings yet
- JCM 02881-20Document17 pagesJCM 02881-20SariSyahruniNo ratings yet
- CJRT 2020 041Document4 pagesCJRT 2020 041danelvNo ratings yet
- Manifestasi Oral Infeksi COVID-19: Yobel R. Woran, Lydia E. N. Tendean, Christy N. MintjelunganDocument5 pagesManifestasi Oral Infeksi COVID-19: Yobel R. Woran, Lydia E. N. Tendean, Christy N. MintjelunganAra EzenNo ratings yet
- 1.4 - Eposter - 12 Des 2021Document7 pages1.4 - Eposter - 12 Des 2021parmita sariNo ratings yet
- Pathogens: Differential Effects of Antiseptic Mouth Rinses On Sars-Cov-2 Infectivity in VitroDocument14 pagesPathogens: Differential Effects of Antiseptic Mouth Rinses On Sars-Cov-2 Infectivity in VitroVINKA ANJANI IRNANDANo ratings yet
- Australian Dental Journal - 2017 - Pedrosa - Oral Manifestations Related To Dengue Fever A Systematic Review of TheDocument8 pagesAustralian Dental Journal - 2017 - Pedrosa - Oral Manifestations Related To Dengue Fever A Systematic Review of TheYunita Permata Dewi NNo ratings yet
- Cetylpyridinium Chloride As A Tool Against COVID-19Document4 pagesCetylpyridinium Chloride As A Tool Against COVID-19Nicoll SQNo ratings yet
- 1 s2.0 S1198743X14610909 MainDocument5 pages1 s2.0 S1198743X14610909 MainstevaniNo ratings yet
- 2021 - Exploring The Diversity of Coronavirus in Sewage During COVID-19Document7 pages2021 - Exploring The Diversity of Coronavirus in Sewage During COVID-19Ikaro AlvesNo ratings yet
- Cleft Lip and PalateDocument14 pagesCleft Lip and Palatehasan abedNo ratings yet
- Dentistry Journal: Oral Symptoms Associated With COVID-19 and Their Pathogenic Mechanisms: A Literature ReviewDocument28 pagesDentistry Journal: Oral Symptoms Associated With COVID-19 and Their Pathogenic Mechanisms: A Literature ReviewAndrext TwoNo ratings yet
- 1-2021 HJ, ANTONIO, GIULIO, MANUEL Healthcare-10-00063Document10 pages1-2021 HJ, ANTONIO, GIULIO, MANUEL Healthcare-10-00063Palomar Dental GroupNo ratings yet
- COVID-19 Dentistry-Related Aspects: A Literature: Concise ReviewDocument6 pagesCOVID-19 Dentistry-Related Aspects: A Literature: Concise ReviewSofiaNo ratings yet
- The "Oral" History of COVID-19: Primary Infection, Salivary Transmission, and Post-Acute ImplicationsDocument11 pagesThe "Oral" History of COVID-19: Primary Infection, Salivary Transmission, and Post-Acute ImplicationsPramudya NycNo ratings yet
- The Bacteriology of Middle Meatus and Ethmoid Sinuses in Chronic Rhinosinusitis Epidemiological Analysis and Surgical ImDocument5 pagesThe Bacteriology of Middle Meatus and Ethmoid Sinuses in Chronic Rhinosinusitis Epidemiological Analysis and Surgical ImEstinovayantiNo ratings yet
- Mao 42 217Document10 pagesMao 42 217Daniel BramantyoNo ratings yet
- Gene Reports: Zaid Almubaid, Hisham Al-MubaidDocument10 pagesGene Reports: Zaid Almubaid, Hisham Al-MubaidMarielaNo ratings yet
- Science of The Total EnvironmentDocument11 pagesScience of The Total EnvironmentMeda ErtianaNo ratings yet
- PEÑA2021 Performance EvaluationDocument5 pagesPEÑA2021 Performance EvaluationOliver Viera SeguraNo ratings yet
- Journal Pre-Proof: HeliyonDocument23 pagesJournal Pre-Proof: HeliyonMohammed Shuaib AhmedNo ratings yet
- Sars-Cov-2 Rna in Dental Biofilms: Supragingival and Subgingival Findings From Inpatients in A Covid-19 Intensive Care UnitDocument10 pagesSars-Cov-2 Rna in Dental Biofilms: Supragingival and Subgingival Findings From Inpatients in A Covid-19 Intensive Care UnitDaniella NúñezNo ratings yet
- Molecular Oral Microbiology - 2023 - D Amico - Efficacy of Cetylpyridinium Chloride Mouthwash Against SARS CoV 2 ADocument10 pagesMolecular Oral Microbiology - 2023 - D Amico - Efficacy of Cetylpyridinium Chloride Mouthwash Against SARS CoV 2 Akatcharles.persoNo ratings yet
- Persistent Viral Shedding of Sars-Cov-2 in Faeces - A Rapid ReviewDocument10 pagesPersistent Viral Shedding of Sars-Cov-2 in Faeces - A Rapid ReviewÁngela Yiceth Torres CorredorNo ratings yet
- Oral and Covid 19 HealthcareDocument9 pagesOral and Covid 19 Healthcaredoc purwitaNo ratings yet
- Oral Manifestations in Patients With COVID-19: A 6-Month UpdateDocument9 pagesOral Manifestations in Patients With COVID-19: A 6-Month UpdateFeby Kuntum Mayang SariNo ratings yet
- Fungal RhinosinusitisDocument12 pagesFungal RhinosinusitisJessicaNo ratings yet
- (2021) Can Ozone Inactivate SARS-CoV-2? A Review of Mechanisms and Performance On VirusesDocument14 pages(2021) Can Ozone Inactivate SARS-CoV-2? A Review of Mechanisms and Performance On VirusesVu TranNo ratings yet
- Condição Periodontal e Caracterização Da Microbiota Subgengival em Indivíduos Com Síndrome de DownDocument15 pagesCondição Periodontal e Caracterização Da Microbiota Subgengival em Indivíduos Com Síndrome de DownTHAIS GOMES MATEUSNo ratings yet
- Aerosol Generating Procedures, Dysphagia Assessment and COVID 19 A Rapid ReviewDocument8 pagesAerosol Generating Procedures, Dysphagia Assessment and COVID 19 A Rapid ReviewvaleperoneNo ratings yet
- Pruebas Diagnosticas Covid-19Document7 pagesPruebas Diagnosticas Covid-19JADIT YASIRA MENDOZA HERNANDEZNo ratings yet
- 1.epidem I Kontrola SarsDocument7 pages1.epidem I Kontrola SarsadnanNo ratings yet
- Medoral 25 E563Document2 pagesMedoral 25 E563dentist studentNo ratings yet
- Covid19 An Overview of Diagnostic Approach and Novel Directions For Treatment StrategiesDocument4 pagesCovid19 An Overview of Diagnostic Approach and Novel Directions For Treatment StrategiesMarie Kath LeenNo ratings yet
- International ArticleDocument12 pagesInternational ArticleAbdullah Al MarzanNo ratings yet
- 2020.01.30.926477v1.full - PDF Evolucion Estimada Del 2019nCoVDocument17 pages2020.01.30.926477v1.full - PDF Evolucion Estimada Del 2019nCoVRENE RIVASNo ratings yet
- Wastewater Based SurveillanceDocument10 pagesWastewater Based SurveillanceAbdullah Al MarzanNo ratings yet
- Ozone Vs Sars Covid VirusDocument13 pagesOzone Vs Sars Covid VirusTS WongNo ratings yet
- 27 201712ThenewmarginalplaqueindexMPImayallowamorevalidassessmentofgingivalplaquelevelthantheTureskymodificationoftheQuigleyandHeinIndexTQHIDocument5 pages27 201712ThenewmarginalplaqueindexMPImayallowamorevalidassessmentofgingivalplaquelevelthantheTureskymodificationoftheQuigleyandHeinIndexTQHINisa Nafiah OktavianiNo ratings yet
- Symptoms of SARS-CoV-2Document13 pagesSymptoms of SARS-CoV-2dhairyasheelNo ratings yet
- Dental JournalDocument7 pagesDental Journaliqbal faturahmanNo ratings yet
- Clerici-2020-Sensitivity of SARS-CoV-2 DetectiDocument5 pagesClerici-2020-Sensitivity of SARS-CoV-2 DetectiNick FloresNo ratings yet
- JCM 12 03605 v2Document14 pagesJCM 12 03605 v2IgnacioCortésFuentesNo ratings yet
- The Role of Doxycycline in The Management of CRSWPDocument6 pagesThe Role of Doxycycline in The Management of CRSWPLeonNo ratings yet
- Prevalence and Nature of Fungi in Root Canal Infections: A Systematic Review and Meta-AnalysisDocument12 pagesPrevalence and Nature of Fungi in Root Canal Infections: A Systematic Review and Meta-AnalysisDavid UriosteguiNo ratings yet
- COVID-19 and The Ocular Surface A Review of Transmission and Manifestations.Document10 pagesCOVID-19 and The Ocular Surface A Review of Transmission and Manifestations.Nicolás Alejandro López AranedaNo ratings yet
- Evidence Summary For Salivary Detection of SARS CoV 2Document27 pagesEvidence Summary For Salivary Detection of SARS CoV 2Romina DatuNo ratings yet
- COVID-19 Diagnosis  A Review of Current MethodsDocument16 pagesCOVID-19 Diagnosis  A Review of Current MethodsMariana BalderramaNo ratings yet
- Detection of 2019-nCoV in Saliva and Characterization of Oral Symptoms in COVID-19 PatientsDocument28 pagesDetection of 2019-nCoV in Saliva and Characterization of Oral Symptoms in COVID-19 PatientsSyaffa Sadida ZahraNo ratings yet
- Oral Manifestations in Patients WithDocument14 pagesOral Manifestations in Patients WithWL DSCNo ratings yet
- The Establishment of Reference Sequence For Sars Cov 2 and Variation AnalysisDocument8 pagesThe Establishment of Reference Sequence For Sars Cov 2 and Variation AnalysisYulaimy BatistaNo ratings yet
- Armitage 2013 ReviewDocument17 pagesArmitage 2013 ReviewMarcoNo ratings yet
- ENT Manifestation of Covid 19: ObjectiveDocument3 pagesENT Manifestation of Covid 19: Objectiveهارون جادNo ratings yet
- Biological and Social Aspects of Coronavirus Disease 2019 (COVID-19) Related To Oral HealthDocument11 pagesBiological and Social Aspects of Coronavirus Disease 2019 (COVID-19) Related To Oral HealthXimena amayaNo ratings yet
- Presence of Mismatches Between Diagnostic PCR Assays and Coronavirus Sars-Cov-2 GenomeDocument17 pagesPresence of Mismatches Between Diagnostic PCR Assays and Coronavirus Sars-Cov-2 GenomeYulaimy BatistaNo ratings yet
- The Use of Salivary Specimen For COVID-19 Detection Using RT-PCR Assay: A Systematic ReviewDocument8 pagesThe Use of Salivary Specimen For COVID-19 Detection Using RT-PCR Assay: A Systematic ReviewIJPHSNo ratings yet
- Laryngeal Complications of COVID-19Document8 pagesLaryngeal Complications of COVID-19Mariana BarrosNo ratings yet
- Oral Candidiasis: A Retrospective Study of 276 Brazilian PatientsDocument5 pagesOral Candidiasis: A Retrospective Study of 276 Brazilian PatientsYuganya SriNo ratings yet
- 21343-Article Text-67222-1-10-20181013Document6 pages21343-Article Text-67222-1-10-20181013Indah SuryadewiNo ratings yet
- Infections of the Ears, Nose, Throat, and SinusesFrom EverandInfections of the Ears, Nose, Throat, and SinusesMarlene L. DurandNo ratings yet
- An Insight To Dental Practice Management: A Literature ReviewDocument4 pagesAn Insight To Dental Practice Management: A Literature ReviewAlexandru Codrin-IonutNo ratings yet
- Comparison of Characteristics of Dental Malpractice Trials Between Medical Malpractice and Ordinary Divisions in District CourtsDocument10 pagesComparison of Characteristics of Dental Malpractice Trials Between Medical Malpractice and Ordinary Divisions in District CourtsAlexandru Codrin-IonutNo ratings yet
- 2022 English For DentistsDocument108 pages2022 English For DentistsAlexandru Codrin-IonutNo ratings yet
- Ejd EthicsstatementDocument2 pagesEjd EthicsstatementAlexandru Codrin-IonutNo ratings yet
- 1 s2.0 S0020653920346074 MainDocument5 pages1 s2.0 S0020653920346074 MainAlexandru Codrin-IonutNo ratings yet
- Interaction of Oral and Toothbrush Microbiota Affects Oral Cavity HealthDocument9 pagesInteraction of Oral and Toothbrush Microbiota Affects Oral Cavity HealthAlexandru Codrin-IonutNo ratings yet
- 1 s2.0 S002065392036545X MainDocument6 pages1 s2.0 S002065392036545X MainAlexandru Codrin-IonutNo ratings yet
- Applied Sciences: Oral Microbiome and Host Health: Review On Current Advances in Genome-Wide AnalysisDocument16 pagesApplied Sciences: Oral Microbiome and Host Health: Review On Current Advances in Genome-Wide AnalysisAlexandru Codrin-IonutNo ratings yet
- 1588 FullDocument8 pages1588 FullAlexandru Codrin-IonutNo ratings yet
- A Randomised Clinical Study To Determine The EffecDocument12 pagesA Randomised Clinical Study To Determine The EffecAlexandru Codrin-IonutNo ratings yet
- Green Dentistry, A Metamorphosis Towards An Eco-Friendly Dentistry: A Short CommunicationDocument2 pagesGreen Dentistry, A Metamorphosis Towards An Eco-Friendly Dentistry: A Short CommunicationAlexandru Codrin-IonutNo ratings yet
- Asian Paci Fic Journal of Tropical BiomedicineDocument7 pagesAsian Paci Fic Journal of Tropical BiomedicineAlexandru Codrin-IonutNo ratings yet
- 181 ArticleText 818 1 10 20200423Document8 pages181 ArticleText 818 1 10 20200423Alexandru Codrin-IonutNo ratings yet
- Professional: The Environmental Impact of DentistryDocument6 pagesProfessional: The Environmental Impact of DentistryAlexandru Codrin-IonutNo ratings yet
- Dental Practice and The Environment: Nairn H.F. Wilson and Edward G. Bellinger Lvar A. MjorDocument6 pagesDental Practice and The Environment: Nairn H.F. Wilson and Edward G. Bellinger Lvar A. MjorAlexandru Codrin-IonutNo ratings yet
- EJHM - Volume 81 - Issue 3 - Pages 1621-1627Document7 pagesEJHM - Volume 81 - Issue 3 - Pages 1621-1627Alexandru Codrin-IonutNo ratings yet
- The Management of Dental Waste in Dental Offices and Clinics in Shiraz, Southern IranDocument6 pagesThe Management of Dental Waste in Dental Offices and Clinics in Shiraz, Southern IranAlexandru Codrin-IonutNo ratings yet
- Hospital Dental Practice in Special PatientsDocument7 pagesHospital Dental Practice in Special PatientsAlexandru Codrin-IonutNo ratings yet
- 06 Mahidol Dental Journal 39 2Document8 pages06 Mahidol Dental Journal 39 2Alexandru Codrin-IonutNo ratings yet
- Infection Control Practices at The Dental Clinics in Jeddah, Saudi ArabiaDocument7 pagesInfection Control Practices at The Dental Clinics in Jeddah, Saudi ArabiaAlexandru Codrin-IonutNo ratings yet
- Smile Line and Facial Esthetics.: January 2011Document5 pagesSmile Line and Facial Esthetics.: January 2011Alexandru Codrin-IonutNo ratings yet
- Research Article: Influence of The Smile Line On Smile Attractiveness in Short and Long Face IndividualsDocument8 pagesResearch Article: Influence of The Smile Line On Smile Attractiveness in Short and Long Face IndividualsAlexandru Codrin-IonutNo ratings yet
- Literature Review: Volume 4, Issue 1 2021Document15 pagesLiterature Review: Volume 4, Issue 1 2021Alexandru Codrin-IonutNo ratings yet
- 5 Manuscript 70 3 10 20200601Document10 pages5 Manuscript 70 3 10 20200601Alexandru Codrin-IonutNo ratings yet
- Clinical Outcomes Comparing Two Prosthetic Knee Designs in Individuals With Unilateral Transfemoral Amputation in TurkeyDocument8 pagesClinical Outcomes Comparing Two Prosthetic Knee Designs in Individuals With Unilateral Transfemoral Amputation in TurkeyAlexandru Codrin-IonutNo ratings yet
- A Mixed-Methods Study On Prosthesis Use Among Older Canadians With Lower-Limb AmputationsDocument11 pagesA Mixed-Methods Study On Prosthesis Use Among Older Canadians With Lower-Limb AmputationsAlexandru Codrin-IonutNo ratings yet
- Journal of Dentistry: M.A. Boyle, M.J. O 'Donnell, R.J. Russell, N. Galvin, J. Swan, D.C. ColemanDocument12 pagesJournal of Dentistry: M.A. Boyle, M.J. O 'Donnell, R.J. Russell, N. Galvin, J. Swan, D.C. ColemanAlexandru Codrin-IonutNo ratings yet
- Journal of Biomedical and Pharmaceutical Research: ISSN (Online) : 2279-0594 ISSN (Print) : 2589-8752Document4 pagesJournal of Biomedical and Pharmaceutical Research: ISSN (Online) : 2279-0594 ISSN (Print) : 2589-8752Alexandru Codrin-IonutNo ratings yet
- Evaluating The Dynamic Performance of Interfacial Pressure Sensors at A Simulated Body Device InterfaceDocument11 pagesEvaluating The Dynamic Performance of Interfacial Pressure Sensors at A Simulated Body Device InterfaceAlexandru Codrin-IonutNo ratings yet
- Table - Diseases Notifiable To The OIEDocument1 pageTable - Diseases Notifiable To The OIEЂорђе100% (1)
- Surface Disinfection With Chlorine (Bleach)Document2 pagesSurface Disinfection With Chlorine (Bleach)cabeaureyNo ratings yet
- Cardiovascular and Respiratory Changes During ExerciseDocument4 pagesCardiovascular and Respiratory Changes During ExerciseBrian ArigaNo ratings yet
- Bacterial MeningitisDocument2 pagesBacterial MeningitisyanNo ratings yet
- General Santos CityDocument25 pagesGeneral Santos CityVeronica HendrickNo ratings yet
- Sdcep Anticoagulants Quick Reference Guide 2nd EditionDocument5 pagesSdcep Anticoagulants Quick Reference Guide 2nd EditionMeryem LahlouNo ratings yet
- Adult Cardiac Arrest AlgorithmDocument3 pagesAdult Cardiac Arrest AlgorithmFlorence Kaye Manzano AniwerNo ratings yet
- Time Specific Objectives Teaching, Learning Activities EvaluationDocument13 pagesTime Specific Objectives Teaching, Learning Activities EvaluationDeepti KukretiNo ratings yet
- Definition-Acute Kidney InjuryDocument6 pagesDefinition-Acute Kidney Injuryashi leginNo ratings yet
- Chhiarpui Neih Tan A Ni: Hunawl Hman That Zofate Hmasawnna Ngaihtuah Kriastian Nun Dan Tha NgaihsanDocument4 pagesChhiarpui Neih Tan A Ni: Hunawl Hman That Zofate Hmasawnna Ngaihtuah Kriastian Nun Dan Tha NgaihsanchanmariansNo ratings yet
- Jurnal PKL 1 RS Wahidin Makassar Abses BrainDocument8 pagesJurnal PKL 1 RS Wahidin Makassar Abses BrainMuhammad SaqriNo ratings yet
- 5 4a Childhood Malignancy Part 1 DR Melanie Victoria G DarDocument10 pages5 4a Childhood Malignancy Part 1 DR Melanie Victoria G DarSamatha SamathaNo ratings yet
- Animal Health Product Listing BrochureDocument12 pagesAnimal Health Product Listing BrochureNona PuetriNo ratings yet
- CR1 Natharina Yolanda 27.01Document48 pagesCR1 Natharina Yolanda 27.01sugarp_3No ratings yet
- Basic ImmunologyDocument2 pagesBasic ImmunologyadibwanNo ratings yet
- Physician's Order...Document2 pagesPhysician's Order...Liiza G-GsprNo ratings yet
- Guidelines For The Table of InjuriesDocument19 pagesGuidelines For The Table of Injuriesworkcovervictim8242No ratings yet
- Bioregulatory Medicine - Chapter Two: The Future of Health and HealingDocument13 pagesBioregulatory Medicine - Chapter Two: The Future of Health and HealingChelsea Green PublishingNo ratings yet
- TG 6 Refractive ErrorDocument11 pagesTG 6 Refractive ErrorNovi AdriNo ratings yet
- COVID - 19 Incident Reporting Form - Adi Rahman SudewoDocument2 pagesCOVID - 19 Incident Reporting Form - Adi Rahman SudewocoslNo ratings yet
- Semaglutide 2 4 MG Once Weekly in Patients With Non Alcoholic Steatohepatitis Related Cirrhosis A Randomised Placebo Controlled Phase 2 TrialDocument12 pagesSemaglutide 2 4 MG Once Weekly in Patients With Non Alcoholic Steatohepatitis Related Cirrhosis A Randomised Placebo Controlled Phase 2 TrialAntonio SalemeNo ratings yet
- The Impact of NicotineDocument1 pageThe Impact of NicotineSanwana MoosaNo ratings yet
- MultivitaminDocument1 pageMultivitaminKatie McPeek88% (8)
- Orphan Drugs Doctoral SeminarDocument21 pagesOrphan Drugs Doctoral SeminarDr RC Mishra100% (1)
- National Tuberculosis and Lung Disease Conference 2024Document5 pagesNational Tuberculosis and Lung Disease Conference 2024Noor Shazana MustaffaNo ratings yet
- Vaccine CDCDocument40 pagesVaccine CDCnasibdinNo ratings yet
- Contraception Brochure Sample#1Document2 pagesContraception Brochure Sample#1Kelsey NuñezNo ratings yet
- Dosage AdjustmentDocument10 pagesDosage AdjustmentNido MalghaniNo ratings yet