Professional Documents
Culture Documents
Antibiotics For The Prevention of Infection Related Preterm Birth
Uploaded by
Awal SafarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antibiotics For The Prevention of Infection Related Preterm Birth
Uploaded by
Awal SafarCopyright:
Available Formats
BMJ 2016;355:i5805 doi: 10.1136/bmj.
i5805 (Published 2 November 2016) Page 1 of 1
Letters
LETTERS
REDUCING THE RISK OF PRETERM BIRTH
Antibiotics for the prevention of infection related
preterm birth
Ronald F Lamont professor of obstetrics and gynaecology
Department of Obstetrics and Gynaecology, Odense University Hospital, University of Southern Denmark, 5000 Odense C, Denmark
Stock and Ismail discuss reducing the risk of preterm birth, Stock and Ismail also fail to take into account the finding that
which is an important cause of neonatal mortality and screening at 10-16 weeks’ gestation and treating vulvovaginal
morbidity.1 But they omit the use of antibiotics to prevent candidiasis, trichomoniasis, or bacterial vaginosis reduced the
infection related preterm birth. The aetiology of preterm birth rate of preterm birth and low birth weight from 22.3% and 20%
is multifactorial, but overwhelming evidence implicates infection in controls to 9.7% and 8.4% (P=0.001), respectively, in those
or inflammation in up to 40% of cases—more so at early screened and treated.6
gestations.
Bacterial vaginosis detected at 13-16 weeks’ gestation was Competing interests: None declared.
associated with a five to sevenfold higher risk of preterm birth
before 34 weeks and late miscarriage (the aetiology of which 1 Stock SJ, Ismail KMK. Which intervention reduces the risk of preterm birth in women with
risk factors?BMJ 2016;355:i5206. doi:10.1136/bmj.i5206 pmid:27707727.
is on a continuum with early preterm birth).2 3 Individual 2 Hay PE, Lamont RF, Taylor-Robinson D, Morgan DJ, Ison C, Pearson J. Abnormal
prophylaxis studies have found benefits of antibiotics for the bacterial colonisation of the genital tract and subsequent preterm delivery and late
miscarriage. BMJ 1994;308:295-8. doi:10.1136/bmj.308.6924.295 pmid:8124116.
prevention of preterm birth, but meta-analyses have not, owing 3 Kurki T, Sivonen A, Renkonen OV, Savia E, Ylikorkala O. Bacterial vaginosis in early
to the inclusion of large methodologically flawed studies with pregnancy and pregnancy outcome. Obstet Gynecol 1992;80:173-7.pmid:1635726.
4 Lamont RF. Advances in the prevention of infection-related preterm birth. Front Immunol
negative results that failed to tackle the optimal antibiotic (in 2015;6:566. doi:10.3389/fimmu.2015.00566 pmid:26635788.
my view, clindamycin), in the optimal patient (women with 5 Lamont RF, Nhan-Chang CL, Sobel JD, Workowski K, Conde-Agudelo A, Romero R.
Treatment of abnormal vaginal flora in early pregnancy with clindamycin for the prevention
objective evidence of bacterial vaginosis), at the optimal time of spontaneous preterm birth: a systematic review and meta analysis. Am J Obstet Gynecol
in pregnancy (earlier than 22 weeks’ gestation, before 2011;205:177-90. doi:10.1016/j.ajog.2011.03.047 pmid:22071048.
inflammatory damage can occur).4 In a more focused systematic 6 Farr A, Kiss H, Hagmann M, Marschalek J, Husslein P, Petricevic L. Routine use of an
antenatal infection screen-and-treat program to prevent preterm birth: long-term experience
review and meta-analysis clindamycin given to women with at a tertiary referral center. Birth 2015;42:173-80. doi:10.1111/birt.12154 pmid:25677078.
bacterial vaginosis before 22 weeks’ gestation significantly Published by the BMJ Publishing Group Limited. For permission to use (where not already
reduced the rate of preterm birth by 40% and late miscarriage granted under a licence) please go to http://group.bmj.com/group/rights-licensing/
by 80%.5 permissions
rlamont@health.sdu.dk
For personal use only: See rights and reprints http://www.bmj.com/permissions Subscribe: http://www.bmj.com/subscribe
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Safe Motherhood ProgramDocument17 pagesSafe Motherhood ProgramNiel A.No ratings yet
- Daftar Pustaka: and Problem Pregnancies. 5Document2 pagesDaftar Pustaka: and Problem Pregnancies. 5Iqbal HambaliNo ratings yet
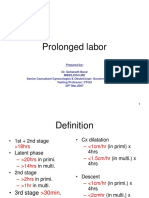
- Lecture-15 Prolonged LaborDocument8 pagesLecture-15 Prolonged LaborMadhu Sudhan PandeyaNo ratings yet
- (Continuity of Care Midwifery) Di Wilayah KerjaDocument7 pages(Continuity of Care Midwifery) Di Wilayah KerjaNafisha HaifaNo ratings yet
- WW.04.05 Contraction Stress Test (Oxytocin Challenge Test) PDFDocument3 pagesWW.04.05 Contraction Stress Test (Oxytocin Challenge Test) PDFDiah Kurniawati100% (1)
- PQCNC 2024 Kickoff PQCNC 2024 20240110Document28 pagesPQCNC 2024 Kickoff PQCNC 2024 20240110kcochranNo ratings yet
- Enhanced IncomeShield Brochure - WebsiteDocument18 pagesEnhanced IncomeShield Brochure - WebsiteAntony VijayNo ratings yet
- 200 New Procedures For 12 Districts Other Than West GodavariDocument18 pages200 New Procedures For 12 Districts Other Than West GodavariKrishna Bharadwaj ReddyNo ratings yet
- Resume - Parand GheshlaghiDocument3 pagesResume - Parand Gheshlaghimohammadrezahajian12191No ratings yet
- Who Preterm Birth 2018Document5 pagesWho Preterm Birth 2018Santi Ayu LestariNo ratings yet
- Mary Frances Gardner Honored As An America's Registry of Outstanding Professionals Lifetime VIP and Professional of The YearDocument2 pagesMary Frances Gardner Honored As An America's Registry of Outstanding Professionals Lifetime VIP and Professional of The YearPR.comNo ratings yet
- Preterm Rupture of MembranesDocument26 pagesPreterm Rupture of MembranesHebara AhmedNo ratings yet
- Placenta Praevia and Placenta Accreta: Diagnosis and ManagementDocument48 pagesPlacenta Praevia and Placenta Accreta: Diagnosis and ManagementMirza FinandarNo ratings yet
- Q&A 3ednDocument15 pagesQ&A 3ednrohitNo ratings yet
- Abdominal Palpation 4.0Document9 pagesAbdominal Palpation 4.0dm pamNo ratings yet
- NCM 107Document3 pagesNCM 107Sunshine BocoNo ratings yet
- M1 Post Task - Caparas-Bsn2a-A2Document2 pagesM1 Post Task - Caparas-Bsn2a-A2Gretta CaparasNo ratings yet
- Obstretic Evidnece Based PDFDocument25 pagesObstretic Evidnece Based PDFnamrata humaneNo ratings yet
- Rendam Kaki Dengan Rebusan Jahe Merah Dapat Mencegah Terjadinya EklamsiaDocument8 pagesRendam Kaki Dengan Rebusan Jahe Merah Dapat Mencegah Terjadinya EklamsiaMellwandariskNo ratings yet
- Postnatal Care PDF 66142082148037Document64 pagesPostnatal Care PDF 66142082148037veronia widayantiNo ratings yet
- 209 Handouts High RiskDocument26 pages209 Handouts High RiskxiumethemoneyNo ratings yet
- Practice: Preterm Labour: Summary of NICE GuidanceDocument4 pagesPractice: Preterm Labour: Summary of NICE GuidanceStaporn KasemsripitakNo ratings yet
- Gynae CompilationDocument787 pagesGynae CompilationMajgsjqNo ratings yet
- Consentimiento Informado RCOG 2015Document13 pagesConsentimiento Informado RCOG 2015Paola RoigNo ratings yet
- Salinan Terjemahan 2 - 511-518 - LR - Peran Suplemen Magnesium Terhadap Hipertensi Dalam Kehamilan Dan PreeklDocument8 pagesSalinan Terjemahan 2 - 511-518 - LR - Peran Suplemen Magnesium Terhadap Hipertensi Dalam Kehamilan Dan PreeklyulyafathankenzieNo ratings yet
- ObgynDocument6 pagesObgynGeraldine MaresNo ratings yet
- 12 Best IVF Doctors in Bangalore With High Success RatesDocument8 pages12 Best IVF Doctors in Bangalore With High Success RatesPrabha SharmaNo ratings yet
- BMC Ultrasound ReportDocument3 pagesBMC Ultrasound ReportBrandy PorciunculaNo ratings yet
- Bahan MirrorDocument2 pagesBahan MirrorAnonymous jbLwTMNo ratings yet