Professional Documents
Culture Documents
Common Mental Disorder Among Family Carers of Demented Older People in Brazil
Uploaded by
AndreaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Common Mental Disorder Among Family Carers of Demented Older People in Brazil
Uploaded by
AndreaCopyright:
Available Formats
Dement Neuropsychol 2018 December;12(4):402-407 Original Article
http://dx.doi.org/10.1590/1980-57642018dn12-040010
Common mental disorder among family
carers of demented older people in Brazil
Evelise Saia Rodolpho Duarte1, Liciane Vaz de Arruda Silveira2,
Vanessa de Albuquerque Cítero3, Alessandro Ferrari Jacinto4
ABSTRACT. Objective: Population aging is a global phenomenon associated with a rising prevalence of chronic
degenerative diseases such as dementia. Dementia poses a challenge not only for patients but also their family caregivers
who, in exercising this role, are at higher risk of mental illness. The present study investigated the prevalence of common
mental disorders (CMD) in family caregivers of demented elderly seen at a geriatric outpatient clinic of a Brazilian
teaching hospital. Methods: A cross-sectional study was conducted in which the following assessment instruments
were applied: the Self Reporting Questionnaire, Zarit Burden Interview, Hospital Anxiety and Depression Scale and Mini-
Mental State Examination (caregivers aged ≥65 years) plus a sociodemographic questionnaire. Results: The sample
comprised 90 caregivers; 83 (92.2%) women, 51 (56.7%) married, 60 (66.7%) son/daughter of elder and 62 (68.6%)
holding another job besides caring for the demented elder. Caregivers had a mean age of 57.3 (±11.7) years and mean
education of 9.5 (±4.9) years; 62.2% of caregivers were diagnosed with common mental disorder, 50% exhibited anxiety
symptoms, 52.2% depression symptoms and 66.7% reported burden. Caregivers with common mental disorder had
higher scores on the anxiety, depression and burden scales (p<0.01). Logistic regression showed that caregivers with
anxiety symptoms were 15 times more likely to present common mental disorder (OR: 15.0; 95% CI: 3.5-71.2) and
caregivers with symptoms of depression were 8 times more likely to have CMD (OR: 8.0; 95% CI: 2.1-31.1). Conclusion:
Results revealed a high prevalence of common mental disorder in the population studied.
Key words: mental disorders, carers, aged, dementia.
TRANSTORNO MENTAL COMUM EM FAMILIARES CUIDADORES DE IDOSOS COM DEMÊNCIA NO BRASIL
RESUMO. Objetivo: O envelhecimento populacional é um fenômeno mundial que está associado ao aumento da
prevalência de doenças crônico-degenerativas, como as demências. Demências desafiam não somente os pacientes,
mas também seus familiares cuidadores que, como consequência, estão em maior risco de adoecimento mental. O estudo
verificou a prevalência de transtorno mental comum em familiares cuidadores de idosos com demência acompanhados
em ambulatórios de geriatria de um hospital-escola brasileiro. Métodos: Neste estudo transversal, os instrumentos de
avaliação utilizados foram: Self Reporting Questionnaire, Zarit Burden Interview, Hospital Anxiety and Depression Scale
e Mini-Exame do Estado Mental (cuidadores com 65 anos ou mais) e questionário sócio demográfico. Resultados: A
amostra foi composta por 90 cuidadores; 83 (92,2%) era do sexo feminino, 51 (56,7%) casados, 60 (66,7%) filhos(as)
do idoso e 62 (68,6%) possuíam alguma ocupação além de cuidar do idoso dementado. A média de idade foi 57,3
(±11,7) anos e a média de escolaridade foi de 9,5 (±4,9) anos; 62,2% dos cuidadores apresentaram transtorno mental
comum, 50% apresentaram sintomas de ansiedade, 52,2% apresentaram sintomas de depressão e 66,7% apresentaram
sobrecarga. Cuidadores com transtorno mental comum apresentaram escores maiores nos instrumentos de ansiedade,
depressão e sobrecarga (p<0,01). Regressão logística mostrou que cuidadores com sintomas de ansiedade tiveram 15
vezes mais chances de apresentar TMC (OR: 15,0; IC95%: 3,5-71,2) e cuidadores com sintomas de depressão tiveram
8 vezes mais chances de apresentar TMC (OR: 8,0; IC95%: 2,1-31,1). Conclusão: Resultados encontrados demonstram
que, na população estudada, existe alta prevalência de transtorno mental comum.
Palavras-chave: transtorno mental, cuidadores, idoso, demência.
This study was conducted at the Department of Internal Medicine, São Paulo State University (UNESP), Botucatu Medical School, Botucatu, SP, Brazil.
1
MSc, Department of Internal Medicine, São Paulo State University (UNESP), Botucatu Medical School, Botucatu, SP, Brazil. 2PhD, Institute of Biosciences, São Paulo
State University (UNESP), Botucatu Medical School, Botucatu, SP, Brazil. 3MD, PhD, Department of Psychiatry, Federal University of São Paulo (UNIFESP), Paulista
Medical School, São Paulo, SP, Brazil. 4MD,PhD, Department of Internal Medicine, São Paulo State University (UNESP), Botucatu Medical School, Botucatu, SP, Brazil.
Evelise Saia Rodolpho Duarte. Department of Internal Medicine / São Paulo State University (UNESP) / Botucatu Medical School – Av. Rubião Jr, s/n – 18618-
294 Botucatu SP – Brazil. E-mail: evesrodolpho@gmail.com
Disclosure: The authors report no conflits of interst.
Received July 13, 2018. Accepted in final form October 25, 2018.
402 Mental disorders in family carers of demented patients Duarte et al.
Dement Neuropsychol 2018 December;12(4):402-407
P opulation aging is a global phenomenon.1 Between
2015 and 2050, the proportion of the world popula-
tion aged over 60 years is set to rise from 12% to 22%,
ing CMD among family carers of dementia patients is
scarce.
Therefore, the objective of the present study was to
and by 2050, 80% of older people will reside in develop- determine the prevalence of common mental disorder in
ing countries.2 Also in 2050, there will be an estimated family carers of older people diagnosed with dementia
131.5 million older people with dementia worldwide.3 and to identify the clinical and sociodemographic factors
Dementia is characterized by cognitive and behav- associated with the occurrence of CMD.
ioral changes associated with functional decline and
dependence for activities of daily living.4 The disease METHODS
poses a challenge for patients, family members and car- A cross-sectional study of carers of dementia patients
ers.5 Growth in the elderly population is accompanied by from the Geriatric Outpatient Clinic of the Health
an increase in the number of individuals with dementia Center School of the Faculdade de Medicina de Botucatu
requiring assistance for activities of daily living and self- – UNESP was conducted.
care tasks. Consequently, the number of family mem- Between April 2015 and March 2017, all family carers
bers caring for dementia patients also rises.5,6 of older people diagnosed with dementia identified from
Looking after a relative with dementia is a complex medical records on outpatient service days were invited
multifactorial process associated with burden for fam- to take part in the study. Ninety-six individuals were ini-
ily carers.7 This burden depends on several factors, such tially invited, 6 of whom refused to participate. Thus, a
as the psychological or emotional health of the carer, total of 90 dementia patient carers present in the wait-
presence of physical morbidities, social life, ethnicity ing room for medical visits or nursing care of their family
and income, and not only on the dementia symptoms member were randomly selected for inclusion. The inclu-
of the elderly patient.8 Burden among dementia patient sion criteria were being a carer age ≥18 years and next-
carers is considered a public health problem.9 Thus, car- of-kin of the elder (undergoing treatment at the clinic).
ing for a patient with dementia is associated with a host After inviting the family member to take part in the
of negative consequences for mental health and a high study, they filled out and signed the free and informed
rate of mood disorders can be found in these carers.10,11 consent form and completed the following instruments:
Some carers suffer from distress, which manifests • Mini-Mental State Examination (MMSE) – global
with anxiety, somatic and depressive symptoms, yet do cognition, Portuguese version (Brucki et al.).14
not fulfill the formal criteria for depression and/or anxi- • Self Reporting Questionnaire (SRQ-20): Screens
ety diagnosis according to the DSM-V (Diagnostic and for common mental disorder (non-psychotic) in pri-
Statistical Manual of Mental Disorders – Fifth Edition) mary health care of developing countries;13,15 contains
and ICD-10 (International Classification of Diseases – 20 questions with binary responses (yes/no). The valid-
10th Revision) classifications, and are thus character- ity study of the SRQ-20 for use in Brazil established a
ized as having common mental disorder (CMD).12 cut-off score of ≥7 yielding sensitivity of 83% and speci-
CMD has a functional disability comparable to that ficity of 80%, recommending its use.13,15
of well-established chronic conditions.13 These disor- • Zarit Burden Interview (ZBI): Measures burden in
ders present either alone or together with one or more carers associated with care of patients with functional
physical disorders.12 Various factors were found to be and behavioral disabilities.16,17 The validated Brazilian
associated with common mental disorders, such as version17 (Scazufca, 2002) has 22 items with responses
lower socioeconomic status, psychological illnesses, poor rated on a 5-level Likert scale (0=never, 1=rarely,
reproductive health, gender disadvantage and physical 2=sometimes, 3=quite frequently, 4=nearly always)
ill-health. Furthermore, socio-economic deprivation has yielding a score of 0-88 points, where higher total score
been directly associated with poor reproductive health, indicates greater burden.
substance use disorders (especially tobacco) and chronic • Hospital Anxiety and Depression Scale (HADS):
medical illnesses, which ultimately lead to common Assesses 14 items divided into anxious and depressive
mental disorders.12,13 Usually, CMD patients fail to seek symptom subscales.18 In the Brazilian validity study, for
medical assistance, and when they do so, the nonspe- a cut-off score ≥8, the scale showed 93.7% sensitivity
cific somatic complaints may lead to underdiagnosis and and 72.6% specificity for anxiety, and 84.6% sensitivity
inadequate treatment.13 and 90.3% specificity for depression.18,19
In Brazil, the prevalence of CMD in the general popu- Statistical analyses were performed using the SPSS
lation ranges from 20% to 56%.13 Literature investigat- v.22” and STATA/SE 14 Data Analysis and Statistical
Duarte et al. Mental disorders in family carers of demented patients 403
Dement Neuropsychol 2018 December;12(4):402-407
Software packages, adopting a significance level of 0.05. <0.25 (associations) for inclusion of the variables into
The associations between the categorized variables were the regression model.
determined using the Chi-Square test. The comparison The study was approved by the Research Ethics Com-
of means of continuous variables was performed using mittee of the Botucatu Medical School - UNESP under
the Student´s t-test, given that the data had a normal CAAE permit no. 40558115.3.0000.5411. The study
distribution according to the Shapiro Wilks test. was explained to participants, all of whom filled out and
After the initial descriptive analysis of the distribu- signed the Free and Informed Consent Form.
tion of frequencies and contingency tables of categori-
cal variables and of the distribution of central tendency RESULTS
measures of continuous variables, the distribution of The overall profile of the sample and distribution of
the sample was explored using “presence/absence of the sociodemographic and mental health variables
CMD” as the dependent variable based on categoriza- according to the presence/absence of CMD are given in
tion on the SRQ using the Chi-square test and Student´s Tables 1 and 2.
t-test for continuous variables. The logistic regression According to Table 1, with regard to overall profile,
model was then fitted. The level of statistical signifi- carers were predominantly female (92.3%), married
cance adopted was 0.05. The dependent variable was (56.6%), had a mean age of 57 years (±12 years), and
“presence/absence of CMD”, based on a p-value of mean education of 9.5 years (±4.9 years). The degree of
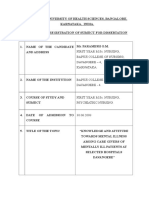
Table 1. Distribution of sociodemographic and mental health variables according to presence/absence of common mental disorder (CMD) in dementia
patient carers, with group comparisons.
Continuous variables Mean (SD)
Age (years) 57.3 (11.7)
Education (years) 9.5 (4.9)
MMSE 27.0 (1.9)
CMD present CMD absent Total
N=56 (%) N=34 (%) N=90 (%) p*
Gender Female 51 (56.6) 32 (35.6) 83 (92.2) 0.6
Male 5 (5.6) 2 (2.2) 7 (7.8)
Marital status Married 31 (34.4) 20 (22.2) 51 (56.6) 0.21
Without companion (single, widowed) 25 (27.8) 14 (15.6) 39 (43.4)
Economically active Yes 38 (42.2) 24 (26.6) 62 (68.8) 0.20
No 18 (20.1) 10 (11.1) 28 (31.2)
Degree of kinship Son/daughter 40 (44.4) 20 (22.2) 60 (66.6)
Spouse 6 (6.6) 5 (5.6) 11 (12.2) 0.74
Other 10 (11.1) 9 (10.1) 19 (21.2)
Anxiety (HADS) Improbable (≤7 points) 16 (17.8) 29 (32.2) 45 (50)
Possible (8-11points) 14 (15.5) 5 (5.6) 19 (21.1) <0.01
Probable (≥12 points) 26 (28.9) 0 26 (28.9)
Depression (HADS) Improbable (≤7 points) 16 (17.8) 27 (30) 43 (47.8)
Possible (8-11 points) 23 (25.6) 7 (7.8) 30 (33.4) <0.01
Probable (≥12 points) 17 (18.8) 0 17 (18.8)
Burden (ZBI) Absence (≤21 points) 8 (11.1) 22 (22.2) 30 (33.3)
Moderate (22-40 points) 34 (37.8) 10 (11.1) 44 (48.9) <0.01
Moderate to Severe (41-60 points) 9 (10) 2 (2.2) 11 (12.2)
Severe (≥61 points) 5 (5.6) 0 5 (5.6)
*Chi-square test. The prevalence of CMD among the carers assessed was 62.2% (N=56).
404 Mental disorders in family carers of demented patients Duarte et al.
Dement Neuropsychol 2018 December;12(4):402-407
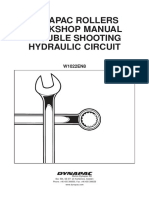
Table 2. Estimates and 95% Confidence Intervals (CI) of odds ratios (OR), obtained by the logistic regression model.
CI95%(OR)
OR Upper limit Lower bound
HADS-Anxiety (possible or probable) 15.0 3.5 71.2
HADS-Depression (possible or probable) 8.0 2.1 31.1
Carer burden 7.2 1.9 27.2
Age (younger) 0.93 0.88 0.99
kinship with the demented elder was predominantly In a Norwegian study, results indicated that having a
son/daughter (66.6%) while most carers were economi- partner with dementia was associated with lower levels
cally active (68.8%). Of the carers assessed, 50% had of life satisfaction and more symptoms of anxiety and
possible or probable anxiety, 52.2% possible or probable depression than those reported by elderly spouses with-
depression and 66.7% reported some degree of burden. out dementia. Having a partner with dementia residing
With regard to the distribution of variables accord- in a nursing home was associated with a markedly lower
ing to presence/absence of CMD among carers, no sta- life satisfaction.22 A national study demonstrated that
tistically significant difference was found for any of the neuropsychiatric symptoms and severity of cognitive
sociodemographic variables (gender, marital status, decline were the major factors associated with burden
economically active and degree of kinship); a statisti- in patients with AD, mostly mild-to-moderate.23
cally significant association (p<0.05) between anxious The prevalence of CMD among family carers of
or depressive symptoms or burden and the presence of dementia patients was 62.2%, proving higher than the
CMD was found among the carers. rate for the general Brazilian population which, accord-
On the multivariate analysis, the dependent variable ing to previous studies ranges from 20% to 56%,24 and
was “presence/absence of CMD”, based on a p-value of also greater than the rate for the global population of
<0.25 (associations) for inclusion of the variables into 29.2% reported by a systematic review.25 In Brazil, a
the regression model. 2014 study in a population of 604 patients of a primary
The logistic regression (Table 2) revealed that carers health care service found a CMD rate of 31.4%,26 whereas
with anxiety symptoms, as measured by the HADS-Anx- another Brazilian study in 2013 of an elderly population
iety scale (possible or probable), had a 15 times greater from Campinas city reported a CMD rate of 29.7%.27
association with CMD (OR: 15.0; 95% CI: 3.5-71.2) and The only national study assessing the presence of
carers with depression symptoms, as measured by the CMD, involving 58 family carers of older people with
HADS-Depression scale (possible or probable), had an dementia, found a prevalence of 46.55%. The presence
8 times greater association with CMD (OR: 8.0; 95% CI: of CMD was associated with the practice of sports, back
2.1-31.1). Carers exhibiting burden according to score pain and duration of daily care.6
on the ZBI had a 7.2 times greater association with The presence of burden was reported by 66.7% of
CMD (OR: 7.2; 95% CI: 1.9-27.2). Younger carers had carers in the present study. A study in India28 showed
a 0.93 lower association with CMD (OR: 0.93; 95% CI: that carer burden was greater depending on the degree
0.88-0.99). of cognitive impairment of the elder. In China, a study
assessing burden of dementia patient carers found that
DISCUSSION 62% of carers reported burden associated with caring
Response: Previous reports have shown that carers are for the demented patient.29 A Brazilian study6 associated
predominantly women,20 a phenomenon also observed the presence of burden with occupation (retired carers
in the present study, whose sample was 92.2% female. had greater burden), sports (carers who engaged in sport
In a psychogeriatric service in São Paulo, 49 elderly reported greater burden), presence of back pain and
people and their caregivers were evaluated. Akin to the duration of daily care (the longer the amount of time
present study, the impact of care was assessed using the dedicated to daily care, the greater the burden).
Zarit Scale and caregivers were predominantly women, A study showed the negative effects of the care situ-
daughters or wives, where a high average burden was ation on the physical and mental health of carers, citing
observed.21 the prevalence of psychiatric disorders, greater incidence
Duarte et al. Mental disorders in family carers of demented patients 405
Dement Neuropsychol 2018 December;12(4):402-407
in the use of psychotropic medications, greater number Response: The present study has several limita-
of somatic diseases, decline in overall clinical health, tions, the first being its cross-sectional design. Selection
social isolation, personal and family stress, feelings of bias may have occurred given the convenience sample
obligation to exercise the role, among others.30 The find- drawn from a specialized outpatient clinic (geriatrics)
ings of two studies showed that the presence of emo- as opposed to a general clinic, where certain carers
tional burnout was associated with a decline in quality might have had a greater likelihood of being selected
of life, behavioral disorders and depressive symptoms.5,31 for the study. In the sociodemographic questionnaire,
Controlling behavioral symptoms of older people with no information was requested on the duration of daily
dementia has been reported as more stressing for carers care, the degree of cognitive impairment of the elder,
than managing cognitive decline.32 the presence of BPSD or whether the patient lived with
Levels of anxiety and depression are higher in car- the carer.
ers than in the general population.33 In the present
study, a statistically significant association was found Author contributions. Evelise Saia Rodolpho Duarte
between individuals diagnosed with CMD and anxious devised the study design, collected data, and wrote
and depressive symptoms. both the protocol and the paper. Liciana Vaz de Arruda
Knowledge of these characteristics is vital for estab- Silveira analyzed the data and reviewed the paper.
lishing more effective measures to support this popula- Vanessa de Albuquerque Citero reviewed the paper.
tion. An example intervention involving carers of older Alessandro Ferrari Jacinto took part in planning the
people is the running of support groups and courses study, was involved in the statistical analyses and the
based on psychoeducation.34,35 In this context, psy- interpretation of the results and wrote the paper.
choeducational interventions contribute significantly
toward improving the well-being of carers, providing an Acknowledgements. We would like to thank the carers
educational component covering the diagnosis, course of the patients who kindly agreed to participate in the
and progression of dementia to improve competencies study.
to cope with the disease.35
REFERENCES
1. Carvalho JAM, Garcia RA. The aging process in the Brazilian population: 12. RISAL A. Common mental disorder. Kathmandu Univ Med J (KUMJ).
a demographic approach. Cad. Saúde Pública, Rio de Janeiro; 2003; 2011;9(35):213-7.
19:725-33. 13. Santos KOB, Araújo TM, Pinho PS, Silva ACC. Evaluation of an instru-
2. World Health Organization & Alzheimer’s Disease International. Mental ment for measuring psychiatric morbity: a validity study of Self-Reporting
health publications. Dementia: A public health priority, 2012. Questionnaire (SRQ-20). Rev Baiana Saúde Pública. 2010; 34:544-
3. ADI – Alzheimer’s Disease International. World Alzheimer Report 2015: 560.
the global impact of dementia – an analysis of prevalence, incidence, 14. Brucki SMD, Nitrini R, Caramelli P, Bertolucci PHF, Okamoto IH. Sugges-
cost and trends. London; 2015. tions for utilization of the mini-mental state examination in Brazil. Arq
4. Frota NAF, Nitrini R, Damasceno BP, Forlenza O, Dias-Tostas E, Silvas Neuropsiquiatr. 2003;61:777-81.
AB, et al. Criteria for the diagnosis of Alzheimer’s disease. Dement 15. Mari JJ, Williams P. A validity study of a psychiatric screening question-
Neurophysicol, 2010;5:5-10. naire (SRQ-20) in primary care in the city of São Paulo. Br J Psychiatry.
5. Takai M, Takahashi M, Iwamitsu Y, Ando N, Okazaki S, Nakajima K, Oishi 1986;148:23-6.
S, Miyaoka H. The experience of burnout among home carers of patients 16. Zarit SH, Zarit JM. The memory and behavior problems checklist 1987R
with dementia: Relations to depression and quality of life. Arch Gerontol and the burden interview (technical report). University Park (PA): Penn-
Geriatr. 2008;49(1):e1-5. sylvania State University; 1987.
6. Silva CF, Passos VMA, Barreto SM. Frequency and impact of the 17. Scazufca M. Brazilian version of the burden interview scale for the
burden on family carers of older people with dementia. Rev Bras Geriatr assessment of burden of care in carers of people with mental illness.
Gerontol. 2012;15:707-731. Ver Bras Psiquiatr. 2002;24:12-17.
7. Arai Y, Kumamoto K, Washio M, Ueda T, Miura H, Kudo K. Factors 18. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale.
related to feelings of burden among carers looking after impaired older Acta Psychiatr Scand. 1983;67:361-370.
people in Japan under the longterm care insurance system. Psychiatry 19. Botega NJ, Bio MR, Zormignani MA, Garcia-Junior C, Pereira WAB.
Clin Neurosci. 2004;58:396-402. Mood disorders among medical in-patients: a validation study of the
8. Covinsky K, Newcomer R, Fox P, Wood J, Sands L, Dane K, Yaffe K. hospital anxiety and depression scale (HAD). Rev Saúde Pública, 1995;
Patient and carer characteristics associated with depression in carers of 29:355-63.
patients with dementia. J Gen Intern Med. 2003;18:1006-1014. 20. Andrén S, Elmstahl S. Relationships between income, subjective
9. Etters L, Goodall D, Harrison BE. Carer burden among dementia patient health and carer burden in carers of people with dementia in group
carers: A review of the literature. J Am Acad Nurse Pract. 2008;20:423-8. living care: A cross-sectional community-based study. Int J Nurs Stud.
10. Pinquart M, Sorensen S. Differences between carers and noncarers 2004;44:435-446.
in psychological health and physical health: a meta-analysis. Psychol 21. Garrido R, Menezes PR. Impact on caregivers of elderly patients with
Aging. 2003;18:250-67. dementia treated at a psychogeriatric service. Rev Saude Publica, 2004;
11. Schulz R, Martire LM. Family caregiving of persons with dementia. Am 38:835-841.
J Geriatr Psychiatry. 2004;12:240–9. 22. Langballe EM, Holmen J, Selbaek G, Saltvedt I, Tambs K. Mental health
406 Mental disorders in family carers of demented patients Duarte et al.
Dement Neuropsychol 2018 December;12(4):402-407
and wellbeing in spouses of persons with dementia: the Nord-Trøndelag 29. Tang B, Harary E, Kurzman R, Mould-Quevedo JF, Pan S, Yang J, Qiao
Health Study. BMC Public Health, 2014;14:413. J. Clinical Characterization and the Carer Burden of Dementia in China.
23. Moscoso MA, Marques RCG, Ribeiz SRI, Dos Santos L, Bezerra DM, Value Health Reg Issues. 2013;2(1):118-126.
Jacob Filho W, et al. Profile of caregivers of Alzheimer’s disease patients 30. Neri AL, Caldeira RB, Batistoni SST, Cachioni M. Variables associated
attended at a reference center for cognitive disorders. Dement Neuro- with the life satisfaction of older people carers of chronically ill and depen-
psychol. 2007;1(4):412-417. dent older people relatives. Rev Bras Geriatr Gerontol. 2017; 20:503-517.
24. Santos EG, Siqueira MM. Prevalence of mental disorders in the Brazilian 31. Gallicchio L, Siddiqi N, Langenberg P. Gender differences in burden and
adult population: a systematic review from 1997 to 2009. J Bras. depression among informal carers of demented elders in the community.
Psiquiatr. (Rio de Janeiro). 2010;59:238-246. Int J Geriatr Psychiatry. 2002;17:154-163.
25. Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, Silove D. 32. Ulstein I, Wyller T, Engedal K. High scores on the Relative Stress Scale,
The global prevalence of common mental disorder: a systematic review a marker of possible psychiatric disorder in family carers of patients with
and meta-analysis 1980-2013. Int J Epidemiol. 2014;43:476-493. dementia. Int J Geriatr Psychiatry. 2007;22:195-202.
26. Lucchese R, Sousa K, Bonfin SP, Vera I, Santana FR. Prevalence of 33. Ampalam P, Gunturu S, Padma V. A comparative study of carer burden
common mental disorder in primary health care. Acta Paul Enferm. 2014; in psychiatric illness and chronic medical illness. Indian J Psychiatry,
27:200-7. 2012; 54:239-243.
27. Borim FSA, Barros MBA, Botega NJ. Common mental disorder among 34. Cerqueira ATAR, Oliveira NIL A. Support Program for Carers: A Thera-
older people individuals: a population-based study in Campinas, São peutic and Preventive Action in the Health Care of the Older people.
Paulo State, Brazil. Cad Saúde Pública. 2013;29:1415-1426. Psicol. USP, São Paulo; 2002;13:133-150.
28. Pattanayak RD, Jena R, Tripathi M, Khandelwal SK. Assessment of 35. Lopes LO, Cachioni M. Psychoeducational intervention for carers of
burden in carers of Alzheimer’s disease from India. Asian J Psychiatry. older people with dementia: a systematic review. J Bras Psiquiatr. 2012;
2010;3:112-116. 61:252-61.
Duarte et al. Mental disorders in family carers of demented patients 407
You might also like
- Inpatient Geriatric Psychiatry: Optimum Care, Emerging Limitations, and Realistic GoalsFrom EverandInpatient Geriatric Psychiatry: Optimum Care, Emerging Limitations, and Realistic GoalsHoward H. FennNo ratings yet
- Psychological Distress in Informal Caregivers of Patients With Dementia in Primary Care: Course and DeterminantsDocument8 pagesPsychological Distress in Informal Caregivers of Patients With Dementia in Primary Care: Course and DeterminantsalvarooNo ratings yet
- Descriptive Epidemiology of Generalized Anxiety Disorder in CanadaDocument6 pagesDescriptive Epidemiology of Generalized Anxiety Disorder in CanadaPin Han NaNo ratings yet
- Assessment of Depression Among Older AdultsDocument9 pagesAssessment of Depression Among Older Adultsrani nauraNo ratings yet
- The Prehensive Differences Between Students Who Are Depressed and Those Who Are Not. A Study of Teenager From Age 15-19 Years Old in Various SchoolDocument6 pagesThe Prehensive Differences Between Students Who Are Depressed and Those Who Are Not. A Study of Teenager From Age 15-19 Years Old in Various SchoolIJAR JOURNALNo ratings yet
- Original Article: ISSN: 0976 3325Document4 pagesOriginal Article: ISSN: 0976 3325Adina OlteanuNo ratings yet
- Ijmrhs 21 41642Document4 pagesIjmrhs 21 41642emiliodiazneuropsicologoNo ratings yet
- Lansia Di Panti Jompo USADocument10 pagesLansia Di Panti Jompo USADWI INDAHNo ratings yet
- Quality of Life in Caregivers of Patients With Schizophrenia A Literature ReviewDocument6 pagesQuality of Life in Caregivers of Patients With Schizophrenia A Literature Reviewgw0q12dxNo ratings yet
- Mood Disorder, Anxiety, and Suicide Risk Among Subjects With Alcohol Abuse And/or Dependence: A Population-Based StudyDocument5 pagesMood Disorder, Anxiety, and Suicide Risk Among Subjects With Alcohol Abuse And/or Dependence: A Population-Based StudyAntônio Neto MachadoNo ratings yet
- The Experience of Psychological Distress in Family CaregiversDocument8 pagesThe Experience of Psychological Distress in Family CaregiversCristina MPNo ratings yet
- Gender Dysphoria and Social AnxietyDocument9 pagesGender Dysphoria and Social AnxietyJellybabyNo ratings yet
- Ajol File Journals - 75 - Articles - 155877 - Submission - Proof - 155877 889 406908 1 10 20170511Document6 pagesAjol File Journals - 75 - Articles - 155877 - Submission - Proof - 155877 889 406908 1 10 20170511Reni Tri AstutiNo ratings yet
- Hirvikoski, Et Al.j. (2015) - Cognitive Behavior Therapy-Based Psychoeducational Groups For Adults With ADHD and Their Significant OthersDocument11 pagesHirvikoski, Et Al.j. (2015) - Cognitive Behavior Therapy-Based Psychoeducational Groups For Adults With ADHD and Their Significant OthersjuanNo ratings yet
- Comoborbilidad Somatica en Niños y Adolescentes ArtDocument9 pagesComoborbilidad Somatica en Niños y Adolescentes Artotrops10% (1)
- Journal of Affective Disorders ReportsDocument10 pagesJournal of Affective Disorders ReportsAnnisa NurainiNo ratings yet
- Autism Spectrum Disorder: Outcomes in Adulthood: ReviewDocument8 pagesAutism Spectrum Disorder: Outcomes in Adulthood: ReviewRosa Indah KusumawardaniNo ratings yet
- Neurology, Psychiatry and Brain Research: B.A. Pramesona, S. TaneepanichskulDocument6 pagesNeurology, Psychiatry and Brain Research: B.A. Pramesona, S. TaneepanichskulMutiara Anak NegeriNo ratings yet
- Older Adults With Schizophrenia and Their Caregivers - An Often Invisible PopulationDocument5 pagesOlder Adults With Schizophrenia and Their Caregivers - An Often Invisible PopulationrahmaliaadewiiNo ratings yet
- Factor Influncing Depression Among AdolescentsDocument5 pagesFactor Influncing Depression Among AdolescentsIJSTENo ratings yet
- Perception About General Awarness of Mental Illness: Group A2Document23 pagesPerception About General Awarness of Mental Illness: Group A2Dilawar JanNo ratings yet
- Artigo - Autismo & SIBDocument10 pagesArtigo - Autismo & SIBFernanda Rodrigues de Araujo Paiva CampeloNo ratings yet
- Abstract:: Background: Objective: MethodologyDocument17 pagesAbstract:: Background: Objective: MethodologyDilawar JanNo ratings yet
- The Overdiagnosis of Depression in Non-Depressed Patients in Primary CareDocument7 pagesThe Overdiagnosis of Depression in Non-Depressed Patients in Primary Careengr.alinaqvi40No ratings yet
- MENTAL HEALTH ACROSS LIFESPANDocument5 pagesMENTAL HEALTH ACROSS LIFESPANCala WritesNo ratings yet
- Mental Health and Cognitive Function in Older Irish AdultsDocument48 pagesMental Health and Cognitive Function in Older Irish AdultsMuhammad AkrimNo ratings yet
- We Therell 2009Document10 pagesWe Therell 2009Oslo SaputraNo ratings yet
- Cognitive Functioning in Adolescents With SelfReported ADHD and Depression Results From A Population-Based StudyDocument14 pagesCognitive Functioning in Adolescents With SelfReported ADHD and Depression Results From A Population-Based StudyJesúsCoyacNo ratings yet
- A Systematic Review and Meta-Analysis of Dyadic Psychological InterventionsDocument22 pagesA Systematic Review and Meta-Analysis of Dyadic Psychological InterventionsCristina MPNo ratings yet
- Written Assignment For HS 4241-01Document6 pagesWritten Assignment For HS 4241-01doreenwNo ratings yet
- The Presence of Behavioural and Psychological Symptoms and Progression To Dementia in The Cognitively Impaired Older PopulationDocument11 pagesThe Presence of Behavioural and Psychological Symptoms and Progression To Dementia in The Cognitively Impaired Older PopulationCeci_SunshineNo ratings yet
- Caregiver BurdenDocument17 pagesCaregiver BurdenAlam Zeb Khattak 70-FSS/PHDPSY/F18No ratings yet
- 5938 20021 3 PBDocument9 pages5938 20021 3 PBbiswaspritha.18No ratings yet
- Prevalence, Persistence, and Sociodemographic Correlates of DSM-IV Disorders in The National Comorbidity Survey Replication Adolescent SupplementDocument18 pagesPrevalence, Persistence, and Sociodemographic Correlates of DSM-IV Disorders in The National Comorbidity Survey Replication Adolescent SupplementGaluh SabikhaNo ratings yet
- Anxiety Disorders Among Adolescents Referred To General Psychiatry For Multiple Causes: Clinical Presentation, Prevalence, and ComorbidityDocument10 pagesAnxiety Disorders Among Adolescents Referred To General Psychiatry For Multiple Causes: Clinical Presentation, Prevalence, and ComorbidityRatu CalistaNo ratings yet
- Dementia Cases Set to Triple by 2050 But Still Largely IgnoredDocument5 pagesDementia Cases Set to Triple by 2050 But Still Largely IgnoredmiibabhiekNo ratings yet
- Who PhsycogeriatriDocument6 pagesWho PhsycogeriatriWilson WilliamNo ratings yet
- 10.1080@09540261.2019.1675283Document6 pages10.1080@09540261.2019.1675283Firda FatimahNo ratings yet
- Introduction-WPS OfficeDocument21 pagesIntroduction-WPS Officemadanfalah11No ratings yet
- Conference 1 Team Prep Sheet RevisedDocument4 pagesConference 1 Team Prep Sheet Revisedapi-610733417No ratings yet
- Depression Research Paper PDFDocument8 pagesDepression Research Paper PDFgz9g97ha100% (1)
- 82264-Article Text-197411-1-10-20121015 PDFDocument6 pages82264-Article Text-197411-1-10-20121015 PDFJamesNo ratings yet
- Depressive Disorder in Mexican Pediatric Patients With Systemic Lupus Erythematosus (SLE)Document6 pagesDepressive Disorder in Mexican Pediatric Patients With Systemic Lupus Erythematosus (SLE)Random PersonNo ratings yet
- Mental HealthDocument6 pagesMental HealthLiza Mae PisiaoNo ratings yet
- First Year M.Sc. Nursing, Bapuji College of Nursing, Davangere - 4, KarnatakaDocument14 pagesFirst Year M.Sc. Nursing, Bapuji College of Nursing, Davangere - 4, KarnatakaAbirajanNo ratings yet
- Literature ReviewDocument7 pagesLiterature Reviewapi-583321795No ratings yet
- 0717 9227 RCHNP 58 04 0314Document10 pages0717 9227 RCHNP 58 04 0314A-Claudio MANo ratings yet
- Depression in Diabetes Patients in MalaysiaDocument12 pagesDepression in Diabetes Patients in Malaysiayeremias setyawanNo ratings yet
- 1 s2.0 S1056499316301274 MainDocument26 pages1 s2.0 S1056499316301274 MainDavidNo ratings yet
- Medical Comorbidities in Children and AdolescentsDocument12 pagesMedical Comorbidities in Children and AdolescentsSalud-psicología-psiquiatria DocenciaNo ratings yet
- 2007Document6 pages2007api-302133133No ratings yet
- World Psychiatry - 2022 - Reynolds - Mental Health Care For Older Adults Recent Advances and New Directions in ClinicalDocument28 pagesWorld Psychiatry - 2022 - Reynolds - Mental Health Care For Older Adults Recent Advances and New Directions in ClinicalpujakpathakNo ratings yet
- 9 8 - 566 569 PDFDocument4 pages9 8 - 566 569 PDFJay DixitNo ratings yet
- FigmentDocument4 pagesFigmentanaella delacruzNo ratings yet
- Journal of Affective Disorders ReportsDocument8 pagesJournal of Affective Disorders ReportsBAISHA BARETENo ratings yet
- Individual Mental Health AssignmentDocument18 pagesIndividual Mental Health AssignmentRebekah Roberts100% (1)
- Case StudyDocument7 pagesCase Studydipak suresh sawarkarNo ratings yet
- Offspring of Mothers With Bipolar Disorder - A Systematic Review Considering Personality FeaturesDocument9 pagesOffspring of Mothers With Bipolar Disorder - A Systematic Review Considering Personality FeaturesGiovanna SouzaNo ratings yet
- Term Paper On Huntingtons DiseaseDocument6 pagesTerm Paper On Huntingtons Diseaseea8r2tyk100% (1)
- 13-SAMSS-003 2017 General Purpose Gear UnitsDocument7 pages13-SAMSS-003 2017 General Purpose Gear UnitsWHWENNo ratings yet
- Mag-Gage The Superior Magnetic Level Gauge: Process Level Technology, Ltd. 281.332.6241Document12 pagesMag-Gage The Superior Magnetic Level Gauge: Process Level Technology, Ltd. 281.332.6241BYRON ENRIQUE AGUILERA CHIMARRONo ratings yet
- Fmea - Failure Mode Effect AnalysisDocument23 pagesFmea - Failure Mode Effect AnalysisAsawari JoshiNo ratings yet
- The Importance of Earth Loop ImpedanceDocument4 pagesThe Importance of Earth Loop ImpedanceKarim Amer100% (1)
- wp2 FinalDocument3 pageswp2 Finalapi-523698524No ratings yet
- Panelboard O&M ManualDocument7 pagesPanelboard O&M Manualchris100% (1)
- Foreign Bodies of Air Passages and Food PassageDocument20 pagesForeign Bodies of Air Passages and Food PassageRamli HassanNo ratings yet
- Algae and Aquatic Biomass For A Sustainable Production of 2nd Generation BiofuelsDocument258 pagesAlgae and Aquatic Biomass For A Sustainable Production of 2nd Generation BiofuelsjcbobedaNo ratings yet
- Leave Policy For EmployeesDocument9 pagesLeave Policy For EmployeesMEGHA PALANDENo ratings yet
- Tie Systems: The Right Solution For All Wall Formwork: Waterproof Gas-Proof Fire Resistant Soundproof Radiation-ProofDocument16 pagesTie Systems: The Right Solution For All Wall Formwork: Waterproof Gas-Proof Fire Resistant Soundproof Radiation-Proofidesawy1982No ratings yet
- Reviewer Ansc 111Document6 pagesReviewer Ansc 111Jeric MadroñoNo ratings yet
- Pinatubo Eruption Case Study: Disaster Readiness and Risk ReductionDocument5 pagesPinatubo Eruption Case Study: Disaster Readiness and Risk ReductionAndrie PaydoenNo ratings yet
- Advanced Vehicle Security System: Key To The Programmable WorldDocument40 pagesAdvanced Vehicle Security System: Key To The Programmable WorldTajinder SinghNo ratings yet
- Hvac Ducting System - BoqDocument6 pagesHvac Ducting System - BoqBeò FhathastNo ratings yet
- 6 Review of Related LiteratureDocument2 pages6 Review of Related Literaturerusty0% (2)
- Intro To Psychology Crash Course Psychology 1Document3 pagesIntro To Psychology Crash Course Psychology 1Hahaha YeahNo ratings yet
- The Logic of Immunity Deciphering An EnigmaDocument204 pagesThe Logic of Immunity Deciphering An EnigmaSatyabrataSahaNo ratings yet
- Hawaiian Hibiscus Facts: Care, Features & Endangered StatusDocument2 pagesHawaiian Hibiscus Facts: Care, Features & Endangered StatusJustine Airra OndoyNo ratings yet
- Human Heredity Principles and Issues 10th Edition Michael Cummings Solutions Manual 1Document10 pagesHuman Heredity Principles and Issues 10th Edition Michael Cummings Solutions Manual 1yvette100% (39)
- Hydraulic Troubleshoot - DynapacDocument37 pagesHydraulic Troubleshoot - DynapacMoazzam Ali0% (1)
- Analysis of A Healthcare Risk Management PlanDocument6 pagesAnalysis of A Healthcare Risk Management PlanGeralds B GeraldNo ratings yet
- Rolling Budget Report by Tanmay RajgadkarDocument4 pagesRolling Budget Report by Tanmay RajgadkarTanmay RajgadkarNo ratings yet
- Why Check Valves SlamDocument2 pagesWhy Check Valves SlamBramJanssen76No ratings yet
- Goodlife Zero Vat Items 14062022Document345 pagesGoodlife Zero Vat Items 14062022kidusNo ratings yet
- Deccan 12Document4 pagesDeccan 12Ehtesam khanNo ratings yet
- Class 8th syllabus overviewDocument1 pageClass 8th syllabus overviewMuhammad Abdullah KhanNo ratings yet
- A Review On The Biosurfactants Properties Types and Its Applications 2090 4541 1000248Document6 pagesA Review On The Biosurfactants Properties Types and Its Applications 2090 4541 1000248Mo NassifNo ratings yet
- Employees' State Insurance Corporation E-Pehchan Card: Insured Person: Insurance No.: Date of RegistrationDocument3 pagesEmployees' State Insurance Corporation E-Pehchan Card: Insured Person: Insurance No.: Date of RegistrationShankar KhuspeNo ratings yet
- Mak 187 BulDocument4 pagesMak 187 BulxephilimNo ratings yet
- Relationship Wide of House VentilationDocument5 pagesRelationship Wide of House VentilationNova RizkenNo ratings yet
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Don't Panic: Taking Control of Anxiety AttacksFrom EverandDon't Panic: Taking Control of Anxiety AttacksRating: 4 out of 5 stars4/5 (12)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (38)
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeFrom EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeRating: 4.5 out of 5 stars4.5/5 (140)
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionFrom EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionNo ratings yet
- Heal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaFrom EverandHeal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaRating: 4.5 out of 5 stars4.5/5 (56)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (1)
- Rapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreFrom EverandRapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreRating: 5 out of 5 stars5/5 (17)
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryFrom EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryRating: 4.5 out of 5 stars4.5/5 (157)
- Feel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveFrom EverandFeel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveRating: 4 out of 5 stars4/5 (249)
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesFrom EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesRating: 5 out of 5 stars5/5 (70)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDFrom EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDRating: 4.5 out of 5 stars4.5/5 (167)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- When Religion Hurts You: Healing from Religious Trauma and the Impact of High-Control ReligionFrom EverandWhen Religion Hurts You: Healing from Religious Trauma and the Impact of High-Control ReligionRating: 4 out of 5 stars4/5 (11)
- Fighting Words Devotional: 100 Days of Speaking Truth into the DarknessFrom EverandFighting Words Devotional: 100 Days of Speaking Truth into the DarknessRating: 5 out of 5 stars5/5 (6)
- Overcoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsFrom EverandOvercoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsRating: 4.5 out of 5 stars4.5/5 (48)
- BORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONFrom EverandBORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONRating: 4.5 out of 5 stars4.5/5 (24)
- Winning the War in Your Mind: Change Your Thinking, Change Your LifeFrom EverandWinning the War in Your Mind: Change Your Thinking, Change Your LifeRating: 5 out of 5 stars5/5 (558)
- Smart Phone Dumb Phone: Free Yourself from Digital AddictionFrom EverandSmart Phone Dumb Phone: Free Yourself from Digital AddictionRating: 5 out of 5 stars5/5 (11)
- Insecure in Love: How Anxious Attachment Can Make You Feel Jealous, Needy, and Worried and What You Can Do About ItFrom EverandInsecure in Love: How Anxious Attachment Can Make You Feel Jealous, Needy, and Worried and What You Can Do About ItRating: 4.5 out of 5 stars4.5/5 (84)
- Call of the Wild: How We Heal Trauma, Awaken Our Own Power, and Use It For GoodFrom EverandCall of the Wild: How We Heal Trauma, Awaken Our Own Power, and Use It For GoodNo ratings yet
- Binaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationFrom EverandBinaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationRating: 5 out of 5 stars5/5 (9)
- The Somatic Psychotherapy Toolbox: A Comprehensive Guide to Healing Trauma and StressFrom EverandThe Somatic Psychotherapy Toolbox: A Comprehensive Guide to Healing Trauma and StressNo ratings yet
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeFrom EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeRating: 4.5 out of 5 stars4.5/5 (49)
- Emotional Detox for Anxiety: 7 Steps to Release Anxiety and Energize JoyFrom EverandEmotional Detox for Anxiety: 7 Steps to Release Anxiety and Energize JoyRating: 5 out of 5 stars5/5 (6)
- The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk: Key Takeaways, Summary & AnalysisFrom EverandThe Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (2)