Professional Documents
Culture Documents
Liver Abscess An Assessment of The Outcome With Various Treatment Modalities
Liver Abscess An Assessment of The Outcome With Various Treatment Modalities
Uploaded by
dianOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Liver Abscess An Assessment of The Outcome With Various Treatment Modalities
Liver Abscess An Assessment of The Outcome With Various Treatment Modalities
Uploaded by
dianCopyright:
Available Formats
edicine & S OPEN ACCESS Freely available online
lM
a
urg
Tropic
Tropical Medicine & Surgery
ery
ISSN: 2329-9088
Research Article
Liver Abscess: An Assessment of the Outcome with Various Treatment
Modalities
Vikas Sankar Kottareddygari*, Suma Surya, Sreeramulu PN, Prakash Dave and Naveed Ahmed Khan
Sri Devaraj Urs Medical College, Kolar, Karnataka, India
ABSTRACT
Aim: To evaluate the clinical presentation and to compare the various treatment modalities for the treatment of
liver abscesses.
Materials and methods: Over a period of 3 years, 24 cases of liver abscesses were studied retrospectively. Complete
clinical details including clinical presentation, etiology, investigative work up and treatment with morbidity and
mortality of all patients were reviewed.
Results: Among the 24 cases, 18 were male and 6 were female, age of the patients ranged from 23-70, mean age of 58
years. 15 patients underwent pigtail catheterisation using Seldinger technique, 5 patients underwent USG guided
aspiration and 4 patients received empirical therapy alone. No major complications were encountered. A patient
on empirical therapy was converted to laparoscopic abscess drainage while another patient treated by USG guided
aspiration had to undergo pig tail catheterisation for recurrence.
Conclusion: In our experience, those cases presenting with abscess and collection of less than 100 cc can be managed
with antibiotics and antiamoebics alone, collection more than 100 cc can be managed most of the times with
ultrasound guided aspiration but requires follow up with imaging to rule out recollection while for collections more
than 200 cc a pig tail catheterization is warranted.
Keywords: Hypereosinophilic syndrome; Empty sella syndrome; S. stercoralis
INTRODUCTION In the last few years we have witnessed a huge change in the
management of liver abscess and further decrease in the morbidity
Pyogenic liver abscesses accounts for 80% of all liver abscesses in the
and mortality to 5%-30% [8]. Advances in interventional radiology
developed world and is always polymicrobial [1,2]. Southeast Asia
has aided in treating these conditions by minimally invasive
and Africa show a prevalence of amoebic and fungal liver abscesses
which are relatively less common in other parts of the world [3]. procedures. In combination with targeted empirical therapy,
Though relatively rare, with a reported incidence of 0.5%-0.8% percutaneous aspiration remains as the main stay of treatment.
in western world and a incidence of 20 per 100000 among the However a small number of patients do not respond to minimally
hospitalized patients, pyogenic liver abscess is potentially lethal [4]. invasive procedures and may require the traditional surgical
Hence there is need to diagnose and treat this condition early. drainage as a definitive treatment.
The etiology of this condition has altered over the years. We reviewed our experience in the management of liver abscesses
Traditionally appendicitis was considered as the major cause of in the past 3 years to explain the etiology, management and further
liver abscess [5], but with advent of surgery and better antibiotic course of the disease & reviewed the literature in this field &
coverage overtime its incidence as a source of abscess has reduced. present a summary on the current practice which may serve as a
In comparison, cholelithiasis and biliary tract diseases having a tool in treating this condition.
potential to cause ascending portal tract sepsis [6], have replaced
appendicitis as leading cause of hepatic abscess formation. Liver METHODS
abscess was regarded as a high morbidity disease requiring surgical
drainage with mortality rates between 9% to 80% [7], if untreated; The demographic and clinical details of all patients admitted to
it would result in death [1]. our institution for liver abscess confirmed by ultrasonography over
Correspondence to: Sri Devaraj Urs Medical College, Kolar, Karnataka, India, Tel: 917760895920; E-mail: kottareddigaryvs@gmail.com
Received: April 08, 2018; Accepted: January 25, 2019; Published: April 25, 2019
Citation: Kottareddygari VS, Surya S, Sreeramulu PN, Dave P, Khan NA (2019) Research Article: Liver Abscess: An Assessment of the Outcome with
Various Treatment Modalities. Trop Med Surg 7:224. doi: 10.35248 /2329-9088.7.2.224.
Copyright: © 2019 Kottareddygari VS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Trop Med Surg, Vol. 7 Iss. 2 No: 224 1
Kottareddygari VS, et al. OPEN ACCESS Freely available online
a period of 3 years (2013 to 2016) were studied retrospectively. Data
regarding clinical findings, etiology, investigations, treatment was
gathered. Patients with chronic alcoholic history and cirrhosis of
liver and patients with history of hepatitis were excluded from the
study.
Patients with abscess less than 100 cc were managed by empirical
therapy alone for 3 weeks. Beyond 100 cc, ultra sound guided
percutaneous aspiration was done. But if the patient’s general
condition deteriorated they were managed by pigtail catheterization.
And beyond 200 cc pig tail catheterisation was done by Seldinger’s
technique (Figures 1-3) under local anaesthesia.
Figure 4: Drainage of purulent collection.
guided aspiration was done if all the above measures failed.
RESULTS
Of the 24 patients studied, most of them were in the age group
46 to 55 years [8] were as only one patient was below 25 years
(Figure 5).
Figure 1: Painting of abdomen.
Figure 2: Draping of the site and local anaesthic injection. Figure 5: Bar diagram showing age distribution of patients in our study
Majority of the patients i.e. 16 were male and only 8 were female
(Figure 6).
Figure 3: Pig tail catheter insertion.
The catheter was left in situ for 7-10 days or until the drain output
was less than 30 cc. Pus was sent for culture and sensitivity analysis
after both aspiration and catheterization. Patients were empirically
given a combination of cephalosporin and metronidazole (empirical
therapy) which was later changed based on response of patient or Figure 6: Pie diagram showing sex distribution of patients in our study.
culture sensitivity if intervention was done. (Figure 4) Laparoscopy Figure 7 shows the abscess was predominantly seen in the 7th
segment of liver (44%).
Trop Med Surg, Vol. 7 Iss. 2 No: 224 2
Kottareddygari VS, et al. OPEN ACCESS Freely available online
evacuation. The data of follow up for a period of 6 months showed
repeat liver function tests and imaging confirmed the resolution of
the abscess cavity in all cases [9].
DISCUSSION
Hepatic abscess was described back from the time of Hippocrates
around 4000 B.C. Ochsner’s review of 47 cases of pyogenic liver
abscess indicated open surgical management as the main stay of
therapy [10]. This series emphasized a uniformly fatal outcome
of the untreated pyogenic liver abscess. Even after the aggressive
management of the liver abscess, mortality remained as high as
Figure 7: Pie diagram showing segmental distribution of liver abscesses. 60%-80% in the mid twentieth century (Figure 9). Advancements
in radiological and microbiology techniques have improved the
The distribution of patients according to the volume of abscess diagnosing as well as revolutionized the management of the liver
cavity is as follows (Figure 8). abscess which to a reduction in mortality rate to <5%-30% [8].
With early diagnosis and management, the peak incidence is shifting
from the young towards sixth and seventh decade of life. Hepatic
abscess are relatively rare in children and adolescents and are usually
associated with trauma or any underlying immunodeficiency
status. Clinical presentation of pyogenic liver abscess can be non-
specific and similar to other infectious conditions or hepatobiliary
inflammations. These include fever with chills and rigors, nausea
and vomiting, right upper quadrant pain, anorexia, weight loss,
weakness and malaise, cough hiccups and referred pain to the right
shoulder due to irritation of the diaphragm. Patients with small
solitary lesions have an insidious course with anorexia, weight loss,
and fatigue anemia of chronic disease while multiple abscess have
an acute presentation.
The laboratory parameters associated with hepatic abscess like
Figure 8: Pie diagram showing patient distribution according to volume the inflammatory markers are sensitive but not specific. In
of abscess cavity. our study patients presented with leucocytosis and normocytic
and normochromic anemia. Ultrasonography and computed
tomography are the gold standard modalities in the diagnosis
of liver abscess [11] and have a therapeutic value for guided
percutaneous aspiration and drainage of the abscess cavity. These
radiological interventions may also reveal the etiology sometimes,
for example hepatobiliary pathologies.
There has not been any change in the incidence of the pyogenic
liver abscess but there has been a definite change in the etiology
of the condition due to advent in surgical and microbiological
practices. Biliary tract diseases are the major cause of bacterial liver
abscess followed by appendicitis. Choledocholitiasis, obstructing
tumors, strictures, and congenital anomalies of the biliary tract
are the major causative conditions. An alternative mechanism
is by direct spread of contiguous infection i.e., embolization of
a septic focus from the intra-abdominal infection. Diverticulitis,
Figure 9: Pie diagram showing patient distribution according to inflammatory bowel disease, perforated hollow viscus and
management received. appendicitis are probable source of the emboli. Systemic bacteremia
due to endocarditis, pyelonephritis may result in abscess formation
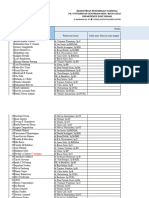
Table 1: Showing the organisms isolated in patients.
due to hematogenous spread. Such cases have been reported in
Sl. No. Organism No. of patients immunocompromised and leukemic patients (Table 1).
1. Escherichia coli 10 The microbial organisms isolated from the pus show a wide
2. Entamoeba histolytica 8 spectrum of infection from polymicrobial to parasitic infestations
3. Klebsiella pneumonia 4 particularly in tropical and subtropical areas. Entamoeba histolytica
and Ascaris lumbricoides are two such parasites associated with liver
4. Polymicrobial 1
abscess. These should be considered particularly in the endemic
5. No growth 1
areas. Liver abscess if left untreated can end up in sepsis and later
There were no mortalities in this study. The mean length of peritonitis secondary to rupture. If the abscess contains less than
hospital stay was 21 days and much longer in the case of surgical 100 cc of pus 3 weeks of systemic broad spectrum antibiotics are
Trop Med Surg, Vol. 7 Iss. 2 No: 224 3
Kottareddygari VS, et al. OPEN ACCESS Freely available online
the main stay of treatment. Yet there are some studies which suggest amoebiasis. All the cases except 1 responded to empirical treatment.
that antibiotics alone are not the best mode of treatment especially Those cases presenting with abscess less than 100 cc of collection
when the size of the abscess is increasing in which case surgical or can be managed with empirical therapy of an antibiotic and
radiology guided drainage of the abscess is the best modality of antiamoebic alone. Those above 100 cc if managed with Ultrasound
treatment. guided aspiration only have to be followed up with imaging to rule
out recurrence. Cases with more than 200 mL of pus in the liver
Various reports suggest that an abscesses above 7 cm need to be
are best treated with pig tail catheter drainage. All the cases require
drained routinely. In addition other criteria for percutaneous
a course of empirical therapy for a period of 3 to 4 weeks and a
drainage are continued pyrexia for 48-72 hours post initiation
follow-up for 6 months to look for complete resolution.
of medical treatment, and clinical and ultrasonographic features
suggestive of impending perforation [12]. Surgical drainage has a REFERENCES
high therapeutic success rate and was the gold standard until the
mid-1970s. 1. Branum GD, Tyson GS, Branum MA, Meyers WC. Hepatic abscess:
Changes in etiology, diagnosis, and management. Ann Surg.
With the advancement of the sonographic imaging, the 1990;212(6):655-662.
percutaneous drainage has emerged as an effective alternative to
the surgical drainage with similar high success rate. The decision 2. Maroun EN, Amrita C, Mary M, Deepti C, Oehler R, Greene, et al.
to leave the catheter in place after aspiration rather than repeated Pyogenic Liver Abscess Due to Fusobacterium Mimicking Metastatic
Liver Malignancy. Infect Dis Clin Pract. 2012;20(5):359-361.
aspiration is also combative. Multiple aspirations appear to be
simple, effective and easy to perform with less post procedural 3. Ghosh S, Sharma S, Gadpayle AK. Clinical Laboratory and
complications and sepsis. However this requires careful follow up Management Profile in Patients of Liver Abscess from Northern India.
with repeated imaging to assess the response to the therapy and J Trop Med. 2014:1-8.
patient compliance tends to be less. Insertion of a drainage catheter
4. Rahimian J, Wilson T, Oram V, Holzman RS. Pyogenic liver
is found to be more effective if the size of the abscess is more than 5
abscess: recent trends in Etiology and Mortality Clin Infect Dis.
cm. The average time to achieve 50% reduction in the size is found
2004;39(11):1654-1659.
to be significantly low with percutaneous drainage than with the
needle aspiration. 5. Huang CJ, Pitt HA, Lipsett PA, Osterman FA, Lillemoe KD, Cameron
JL, et al. Pyogenic hepatic abscess: Changing trends over 42 years. Ann
Despite the high success rate of percutaneous drainage techniques,
Surg. 1996;223(5):600-607.
there is a major role of surgical aspiration in the management of
pyogenic abscess. 6. Helen M, Heneghan, Healy NA, Martin ST, Ryan RS, Nolan N, et
al. Modern management of pyogenic hepatic abscess: a case series and
These conditions include:
review of the literature. BMC Res Notes. 2011;4:80
• No clinical response for 4-7 days in spite of drainage via a
7. Mustafa M, Menon J, Rahman MDS, Parash MTH, Shimmi SC. Acute
catheter placed in the abscess cavity.
Biliary tract infections, Diagnostic criteria and Treatment. Int J Pharm
• Multiple, large or loculated abscesses. Sci Invent. 2014;3(10):58-62.
• Thick walled abscess with viscous pus 8. Farges O, Leese T, Bismuth H. Pyogenic liver abscess: an improvement
in prognosis. 1988;75(9):862-865.
• Concurrent intra-abdominal surgical pathology.
9. Agha RA, Fowler AJ, Rajmohan S, Barai I, Orgill DP, The PROCESS
With the results in our study it can be safely said that the treatment
Group. The PROCESS Statement: Preferred Reporting of Case Series
of liver abscess can be tailored according to the volume of the abscess
in Surgery. Int J Surg. 2016;36:319-323.
cavity and response of the patient to empirical therapy (Figure 8).
Small abscesses can be treated with empirical therapy alone based 10. Ochsner A, DeBakey M, Murray S. Pyogenic Abscess of the Liver II. An
on the local antibiotic and antiamoebic policy, medium abscesses Analysis of Forty-Seven Cases with Review of the Literature. Am J Surg.
can be treated with aspiration and follow up while catheterisation 1938;40(1):292-319.
is preferable in large abscesses. 11. Kochel JQ, Koehler PR, Lee TG, Welch DM. Diagnosis of abdominal
abscesses with computed tomography, ultrasound, and 111-In
CONCLUSION leuckocyte scan. Radiology. 1980;137(2):425-432.
In our experience of managing liver abscess at a tertiary care 12. Krige JE, Beckingham IJ. ABC of diseases of liver, pancreas, and biliary
rural hospital we conclude that it occurs secondary to intestinal system. BMJ. 2001;322(7285):537-540.
Trop Med Surg, Vol. 7 Iss. 2 No: 224 4
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Update IlmiahDocument6 pagesUpdate IlmiahdianNo ratings yet
- Jadwal Divisi DM April 2022Document25 pagesJadwal Divisi DM April 2022dianNo ratings yet
- BHP Bedah AnakDocument4 pagesBHP Bedah AnakdianNo ratings yet
- Morbiditas Dari Divided Stoma Dibandingkan Loop ColostomyMorbiditas Dari Divided Stoma Dibandingkan Loop Colostomy Pada Pasien Dengan Malformasi Anorektal-3Document4 pagesMorbiditas Dari Divided Stoma Dibandingkan Loop ColostomyMorbiditas Dari Divided Stoma Dibandingkan Loop Colostomy Pada Pasien Dengan Malformasi Anorektal-3dianNo ratings yet
- Usulan Kegiatan Tour Di Bali 2020Document3 pagesUsulan Kegiatan Tour Di Bali 2020dianNo ratings yet
- Degloving InjuryDocument27 pagesDegloving InjurydianNo ratings yet
- Soal + Jawaban Ujian TulisDocument18 pagesSoal + Jawaban Ujian TulisdianNo ratings yet
- Ventral Hernia PDFDocument8 pagesVentral Hernia PDFdianNo ratings yet
- DR - Ainun Aschorijanto Spu Sub Divisi Urologi, Lab/Smf Ilmu Bedah FK Unsrat - Rsu Prof R.D Kandou ManadoDocument20 pagesDR - Ainun Aschorijanto Spu Sub Divisi Urologi, Lab/Smf Ilmu Bedah FK Unsrat - Rsu Prof R.D Kandou ManadodianNo ratings yet
- Referat TrueDocument32 pagesReferat TruedianNo ratings yet
- Balans Cairan & Elektrolit RSTDocument59 pagesBalans Cairan & Elektrolit RSTdianNo ratings yet
- Trauma WajahDocument37 pagesTrauma WajahdianNo ratings yet
- Avm (Indo)Document21 pagesAvm (Indo)dianNo ratings yet